Abstract
Background
Understanding the determinants of major depression in sub-Saharan Africa is important for planning effective intervention strategies.
Objective
To investigate the social and life-event determinants of major depressive disorder in the African socio-cultural context of rural Uganda.
Methods
A cross-section survey was carried out in 14 districts in Uganda from 1st June 2003-30th October 2004. 4660 randomly selected respondents (15 years and above) were interviewed. The primary outcome was the presence of major depressive disorder as assessed by the Hopkins Symptom Checklist (HSCL-25).
Results
The prevalence of major depressive disorder was 29.3% (95% confidence interval, 28.0%-30.6%). Factors independently associated with depression in both genders included: the ecological factor, district; age (increase with each age category after 35 years); indices of poverty and deprivation (no formal education, having no employment, broken family, and socio-economic classes III-V). Only a few adverse life events, notably those suggestive of a disrupted family background (death of a father in females and death of a mother in males) were associated with increased risk. Conclusion: Socioeconomic factors operating at both ecological and the individual level are the strongest independent determinants of depression. Adverse life events were less strongly associated with depression in this sample.
Keywords: major depressive disorder, Africa, risk factors, poverty, ecological factors
INTRODUCTION
A major finding of multinational studies of major depressive disorder is the very wide variation in prevalence rates between countries [8]. Rates of psychiatric disorders in Africa have been observed to be up to two times those seen in the West even when similar assessment tools have been used [30,40]. How much of the geographical variation in major depressive disorder can be attributed to ecological factors and how much to individual risk factors is not known. The association between psychiatric pathology on the one hand and lower socioeconomic status (poverty) and stressful life events on the other has been consistently documented both from the West and in some developing countries [4,13,14,17,20,24,39]. Evidence from the West on the role of ecological or contextual explanations has remained inconclusive [7, 11, 36].
This paper will investigate the contribution of ecology, socioeconomic factors, and adverse life events to major depressive disorder in the socio-cultural context of rural Uganda.
METHODOLOGY
A community-based survey was conducted in 14 rural districts of Uganda of which 11 were disadvantaged (relatively poor, experiencing on-going conflict or recently affected by conflict, and having poor health facilities) while 3 districts from Southern and Central Uganda were relatively prosperous, not recently affected by conflict and had better health services.
This study was commissioned by the Support to the Health Sector Strategic Plan Project (SHSSP Project) of the Ministry of Health of Uganda to generate district level health indices including those of mental health.
Sampling procedure
A multistage sampling procedure was used to draw up the sample for this study. During the first stage 10 enumeration areas (EA; derived from the listings of the 2002 Uganda Population and Housing Census sampling frame) were randomly selected from each of the study districts employing a probability proportional to size sampling technique. The second stage of sampling involved the random selection of 25 households from each of the selected EAs. From each of the selected households all respondents 15 years and above were enrolled into this study (it was anticipated each household would have between 1−3 household members who fit in this age bracket). EAs that were host to internally displaced persons (IDPs) camps were excluded as it was felt that the situation of internal displacement was unnatural and temporary and a potential factor for exaggerating the prevalence figures for mental illness. When a selected EA fell within an area of the district with an IDP camp, it was replaced by another EA using simple random sampling.
Preparation and calibration of data collection tools
A generic data collection tool which was translated into the five languages spoken in the study areas was pre-tested, adjusted and then used in this study. Non-medical interviewers who had previously participated in demographic surveillance data collection exercises with the Uganda Bureau of Statistics were recruited as research assistants.
Measures
Major depressive disorder
The 15-item depression scale of the Hopkins Symptom Checklist (HSCL-25) was calibrated and used to diagnose major depressive disorder in this study [9]. This instrument has previously been used in similar socio-cultural contexts in Uganda and Rwanda with good results [2,3]. The Hopkins Symptom Checklist (HSCL-25; test scale) was calibrated against Structured Clinical Interview for DSM IV (SCID) [37] (the gold standard) to determine the ideal cut-off points corresponding to a diagnosis of major depressive disorder in this socio-cultural environment. This was by an exercise that involved administering translated versions of both these instruments to 150 randomly selected respondents from two villages in the neighbourhood of the national psychiatric hospital at Butabika. The optimal cut-off scores were determined by generating a ROC curve. The uppermost and most lateral point on the ROC curve corresponded to a specificity of 90% and a sensitivity of 76% which translated into a cut-off point on the Hopkins Depression Scale of 31. In this study the Hopkins Symptom Checklist for depression instrument had a Cronbach α of 0.86, which is comparable to Mollica and colleagues’ (2001) finding, among Bosnian refugees, of Cronbach α of 0.89.
Ecological factors
The effect of ecological factors was assessed using district as a proxy measure for this factor. Various district level indices were used as socio-economic indicators, viz: whether experiencing on-going war conflict or not at the time of the study (measure of civil conflict); percentage of mothers delivered by trained health workers (proxy for state of health services); literacy rates (proxy for degree of socio-economic development); distance to nearest government health facility (also proxy for the state of health services in the district); and percentage of households whose main material used to construct the walls were burnt bricks bound together by cement mortar (proxy measure for the socioeconomic development of the district)-derived from the non-mental health chapters of the SHSSP report [12].
Individual socioeconomic status
The individual socioeconomic status assessment was done based on Hollingshead’s 1958 classification which was modified by Minde (1975) for his study in Uganda and more recently used by Kinyanda and colleagues (2004) where: Class I were professionals with university degree/ senior civil servants; Class II were owners of large businesses with no university education; Class III were junior civil servants, primary teachers, policemen, clerks and soldiers; Class IV were craftsmen, farmers owning more than 3 acres of land, and mechanics; and Class V farmers of small plots of land and unskilled labourers [21, 25]. Socioeconomic status was also assessed by assessing employment status and level of education.
Adverse life events and history inventories
Items derived from the Life Events and History module of the European Parasuicide Study Interview Schedule I (EPSIS I) which had previously been modified and used in Uganda by Kinyanda and colleagues (2005) were used to collect data on adverse life events of the study subjects [18,22]. The items considered the significant lifetime experiences of social relationships of the respondent with parents, partners, and significant others; an additional question elicited exposure to war trauma experiences [19, 28].
Socio-demographics
The data collection tool also gathered information on status in the household, gender, age group and marital status.
Ethical Issues
The study sought and obtained Ethical clearance from the Uganda National Council of Science and Technology. Informed consent was sought from study participants after adequate explanation of the study objectives and expected benefits for the health services in the country. Those found to have significant scores on the various mental health assessment scales were offered a referral to the nearest health facility.
Analysis
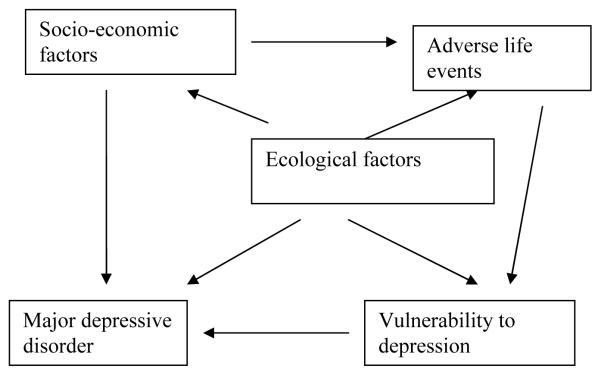
Logistic regression was used for all analyses with major depressive disorder coded as a binary outcome (present or absent). Major depressive disorder was defined as a score of 31 or above on the 15-item depression scale of the Hopkins Symptom Checklist -25 [9]. To take into consideration the hierarchical ordering of the determinants of the study outcome, a conceptual framework (Figure 1) based on the stress-vulnerability model for depression was specified a priori to guide the multivariate analyses [27].
Figure 1.
Conceptual framework based on the stress-diathesis model for depression
Since overall 250 households were selected per district, a household in a smaller district had a larger probability of being chosen than one from the bigger districts. To control for this effect and the effect of clustering at district level, sampling weights for each district were generated based on the formula: Number of households per district/ 250. The resultant weights for each district we then normalized by dividing each by the mean of all the district weights to produce the sample weights which were then used at analysis to produce a more robust version of logistic regression with the Wald test used as the test statistic.
Firstly, the district level rates of major depressive disorder (representing ecological factors) were determined and arranged in ascending order. Secondly, various district level indices (proxy indicators of ecological characteristics of the district) were tabulated against district rates of major depressive disorder. Thirdly, univariate logistic regression analyses were performed for the socioeconomic factors stratified by gender; all those factors with a P<0.1 were then included in a multivariate model. The factors independently associated with the outcome (P<0.1) in the multivariate model were retained for subsequent analyses. Fourthly, the associations of adverse life events with major depressive disorder were estimated for each gender adjusting for significant socioeconomic factors. Two final multivariate models, one for each gender were then constituted, made up of all the ecological, socioeconomic and adverse life event factors that were independently associated with major depressive disorder. We report odds ratios (ORs) unadjusted and adjusted (for the adverse life events) and 95% confidence intervals (CIs) for associations.
RESULTS
Of 4984 selected respondents, 4660 (93.5%) eventually completed the interview; the reasons for failure to complete the interview included: repeatedly not at home 174 (3.5%), refusal to be interviewed 25 (0.5%), incomplete questionnaires 70 (1.4%), physical and mental incapacity 5 (0.1%) and other specified reasons 30 (0.6%). Those who did not complete the interview did not differ significantly from the completers in terms of age and gender.
Prevalence of Major depressive disorder & association with ecological factors
The prevalence of major depressive disorder at the time of study interview was 29.3% (n=1366, 95% CI, 28.0%−30.6%). The variable of district was significantly associated with major depressive disorder, with rates of major depressive disorder in the districts varying between 7.7% in Bushenyi district and 49.6% in Moyo (P<0.001) (Table 1). Also shown in Table 1 is the variation of district rates of major depressive disorder with various district level indices. It was only the district literacy rates which showed a reciprocal relationship with the district rates of major depressive disorder.
Table 1.
Prevalence of Major Depressive disorder (MDD) in 14 districts of Uganda and it's association by gender
| Prevalence of MDD | Male | Female | |
|---|---|---|---|
| Total N=4660 (%) | Univariate OR (95% CI)* |
Univariate OR (95%
CI)* |
|
| Adjumani | 68 (15.6) | 1.0 | 1.0 |
| Mebende | 72 (24.8) | 2.0 (0.9-4.7) | 1.9 (1.1-3.4) |
| Bugiri | 158 (44.4) | 4.5 (2.1-9.8) | 4.9 (3.3-7.1) |
| Kapchorwa | 22 (8.4) | 0.4 (0.2-1.0) | 0.8 (0.4-1.6) |
| Katakwi | 133 (40.3) | 2.3 (0.9-5.5) | 5.8 (3.9-8.6) |
| Soroti | 104 (44.4) | 4.3 (1.8-10.3) | 5.4 (3.0-9.8) |
| Kaberamaido | 179 (48.0) | 4.2 (1.9-9.3) | 7.3 (4.9-10.8) |
| Apac | 43 (10.5) | 0.7 (0.2-1.8) | 0.7 (0.3-1.4) |
| Arua | 130 (31.6) | 2.7 (1.3-5.7) | 2.7 (1.7-4.2) |
| Lira | 40 (12.6) | 1.0 (0.4-2.3) | 0.7 (0.4-1.3) |
| Moyo | 191 (49.6) | 5.3 (2.4-11.5) | 6.1 (3.9-9.4) |
| Nebbi | 116 (34.0) | 2.9 (1.3-6.1) | 3.2 (2.2-4.6) |
| Yumbe | 88 (38.9) | 2.8 (1.2-6.7) | 4.9 (3.0-7.8) |
| Bushenyi | 22 (7.7) | 0.3 (0.1-0.9) | 0.6 (0.3-1.1) |
| All districts | 1366 (29.3) |
Wald test P-value significant at <0.001
Association of major depressive disorder with socioeconomic factors
Female gender was independently associated with increased risk of major depressive disorder with a rate of major depressive disorder of 34.7% among females compared with 24.2% among males (OR, 1.7; 95% CI, 1.5−1.9). Table 2 presents the univariate ORs for the associations of socio-economic factors with major depressive disorder, stratified by gender.
Table 2.
Prevalence of major depressive disorder (MDD) and ecological factors by district
| Prevalence of MDD∫ |
% HH using bricks & mortar walls¶ |
War affected at time of the study |
% mothers delivered by HW¶ |
Literacy rates§ |
Dist. to health facility (Km)¶ |
HH. expend. medical care (Ushs.)¶ |
|
|---|---|---|---|---|---|---|---|
| Districts | |||||||
| Bushenyi | 7.7 | 3.0 | No | 8.0 | 55 | 5 | 23,870 |
| Kapchorwa | 8.4 | 1.1 | No | 12.0 | 54 | 4 | 28,243 |
| Apac | 10.5 | 2.6 | Yes | 9.6 | 53 | 5 | 18,635 |
| Lira | 12.6 | 4.2 | Yes | 10.8 | 50 | 5 | 21,873 |
| Adjumani | 15.6 | 0.3 | No | 4.9 | 46 | 3 | 14,412 |
| Mebende | 24.8 | 2.9 | No | 10.7 | 58 | 6 | 29,186 |
| Arua | 31.6 | 1.1 | No | 8.8 | 46 | 4 | 11,570 |
| Nebbi | 34.0 | 1.9 | No | 4.4 | 47 | 4 | 16,756 |
| Yumbe | 38.9 | 0.8 | No | 8.8 | 47 | 6 | 14,840 |
| Katakwi | 40.3 | 1.4 | Yes | 14.0 | 47 | 6 | 22,070 |
| Bugiri | 44.4 | 5.7 | No | 16.0 | 47 | 4 | 22,036 |
| Soroti | 44.4 | 2.6 | Yes | 12.0 | 47 | 5 | 22,275 |
| Kaberamaido | 48.0 | 1.3 | Yes | 12.0 | 47 | 6 | 28,670 |
| Moyo | 49.6 | 1.5 | No | 11.7 | 45 | 3 | 12,701 |
Derived from other chapters of the IDEAS consortium Baseline SHSSP Report 200427
Derived from the 1991 Population and Housing Census, Statistics Department, Ministry of Finance & Economic Planning
Prevalence of major depressive disorder by district is reported in ascending order
In both genders, socioeconomic factors associated with increased risk of major depressive disorder were related to deprivation (no formal education, having no employment, broken family) and poverty (low socioeconomic status).
Association of major depressive disorder with adverse life events by gender
Table 3 presents both the unadjusted and adjusted ORs for the association of adverse life events with the risk for major depressive disorder stratified by gender.
Table 3.
Association of Socio-economic factors with Major depressive disorder (MDD) by gender in a community sample from Uganda (N= 4660)
| Characteristics | Prevalence of MDD |
Males Univariate OR(95% CI) |
Wald test P- value |
Prevalence of MDD |
Females Univariate OR(95% CI) |
Wald test P- value |
|---|---|---|---|---|---|---|
| Status in household | ||||||
| Head | 509 (26.7) | 1.0 | 428 (38.5) | 1.0 | ||
| Offspring | 27 (13.2) | 0.5 (0.3-0.7) | < 0.001* | 38 (23.0) | 0.5 (0.30.7) | < 0.001* |
| Others | 43 (15.3) | 0.5 (0.4-0.8) | 321 (32.3) | 0.8 (0.6-0.9) | ||
| Age Group | ||||||
| 15-18 yrs | 32 (16.2) | 1.0 | 94 (21.5) | 1.0 | ||
| 19-24 yrs | 53 (16.5) | 1.0 (0.6-1.9) | 107 (26.4) | 1.3 (0.9-1.9) | ||
| 25-35 yrs | 155 (20.4) | 1.3 (0.8-2.1) | <0.001* | 235 (33.7) | 1.8 (1.3-2.6) | <0.001* |
| 36-50yrs | 167 (28.0) | 2.0 (1.2-3.2) | 185 (43.0) | 2.9 (2.0-4.0) | ||
| 51-60yrs | 88 (42.3) | 3.7 (2.2-6.4) | 80 (51.9) | 4.0 (2.5-6.2) | ||
| 61+ yrs | 83 (45.6) | 4.0 (2.1-7.3) | 83 (68.6) | 8.0 (4.9-12.8) | ||
| Educational Status | ||||||
| Attained formal education | 113 (33.4) | 1.0 | 328 (49.2) | 1.0 | ||
| No formal education | 451 (24.1) | 1.6 (1.2-2.1) | 0.001* | 395 (30.2) | 2.2 (1.8-2.7) | <0.001* |
| Marital Status | ||||||
| Married | 411 (25.2) | 1.0 | 481 (31.4) | 1.0 | ||
| Separated/widowed | 83 (42.6) | 2.2 (1.6-3.1) | 231 (57.3) | 3.0 (2.4-3.9) | ||
| Single parent | 10 (31.3) | 1.3 (0.5-2.9) | <0.001* | 23 (43.4) | 1.7 (0.9-3.0) | <0.001* |
| Never married | 71 (13.9) | 0.9 (0.2-3.6) | 2 (11.1) | 0.3 (0.1-1.3) | ||
| Others | 4 (18.2) | 0.5 (0.4-0.7) | 50 (19.0) | 0.5 (0.4-0.7) | ||
| Employment Status | ||||||
| Not employed | 482 (24.3) | 1.0 | 542 (31.2) | 1.0 | ||
| Employed/Student | 93 (34.6) | 0.6 (0.4-0.8) | 0.001* | 236 (47.0) | 0.5 (0.4-0.6) | <0.001* |
|
Socio-economic
Status | ||||||
| Class I | 14 (10.4) | 0.2 (0.1-0.5) | 10 (9.8) | 0.1(0.1-0.3) | ||
| Class II | 22 (18.3) | 0.5 (0.3-0.8) | 21 (20.8) | 0.4 (0.2-0.7) | ||
| Class III | 45 (24.6) | 0.7 (0.5-1.1) | <0.001* | 49 (35.5) | 0.7 (0.5-1.1) | <0.001* |
| Class IV | 154 (21.3) | 0.6 (0.4-0.7) | 198 (30.0) | 0.6 (0.5-0.8) | ||
| Class V | 342 (31.1) | 1.0 | 504 (40.4) | 1.0 | ||
Statistically significant association
In males, factors suggestive of a disrupted family environment (either maternal or and paternal death, parental divorce, parent(s) addicted to alcohol) and abuse and neglect (often felt neglected and lonely, ever forced to have sexual intercourse, ever suffered psychological mistreatment) and exposure to war trauma (ever experienced war related torture such as being beaten, rape, gunshot injuries, military detention, staying in the bush) were significantly associated with major depressive disorder.
In females, factors suggestive of a disrupted family (both paternal and maternal death, and parent divorce), abuse and neglect (ever forced to have sexual intercourse, psychological mistreatment, often felt neglected and lonely, and ever been seriously beaten up) and exposure to war trauma (ever experienced war related torture such as being beaten, rape, gunshot injuries, military detention, staying in the bush) were significantly associated with major depressive disorder.
None of the partner related adverse life events was significantly associated with major depressive disorder for either gender.
Association with ecological, socioeconomic and adverse life event risk factors
The final multivariate models, computed separately for each gender (Table 4) show that 3 domains of risk factors were independently associated with major depressive disorder, namely; ecological factors (represented by district), socioeconomic factors and adverse life events. Among males, the risk factors independently associated with major depressive disorder were: ecological factors (district); older age –age categories above 35 years; socioeconomic factors (being separated/ divorced, poorer socioeconomic status) and life events related to parental relationships (mother died and parent(s) addicted to alcohol). Among females, the risk factors independently associated with major depressive disorder were: ecological factors (district; with the rates for females showing an overall pattern similar to that for males); older age –age categories above 35 years; socioeconomic factors (no formal education, being separated/ divorced, being a single parent, no employment and poorer socioeconomic status) and the life event of paternal death.
Table 4.
Association of Adverse life events with Major depression in a community sample from Uganda
| Risk Factor | Males | Females | ||
|---|---|---|---|---|
| Unadjusted OR (95% CI) |
¶Adjusted OR (95% CI) |
OR (95% CI) (95% CI) |
¶Adjusted OR (95% CI) |
|
| Father died | 1.7 (1.3-2.2)*** | 1.2 (0.9-1.5) | 1.8 (1.5-2.3)*** | 1.3 (1.0-1.8)* |
| Mother died | 2.2 (1.7-2.9)*** | 1.6 (1.2-2.1)*** | 1.9 (1.5-2.4)*** | 1.3 (1.0-1.8)* |
| Parents divorced | 1.6 (1.2-2.1)*** | 1.4 (1.1-1.8)* | 1.5 (1.1-1.9)** | 1.0 (0.8-1.4) |
| Ever forced to have sexual intercourse | 1.7 (1.4-2.2)*** | 1.3 (1.0-1.8)* | 1.5 (1.2-1.9)*** | 1.3 (0.9-1.7) |
| Often felt neglected and left alone |
2.2 (1.8-2.7)*** | 1.6 (1.3-2.1)*** | 1.9 (1.5-2.3)*** | 1.3 (1.0-1.7)* |
| Parent(s) addicted to alcohol |
1.7(1.3-2.1)*** | 1.5 (1.1-1.9)** | 1.2 (0.9-1.4) | 1.1 (0.9-1.4) |
| Ever been seriously beaten |
1.7 (1.4-2.1)*** | 1.2 (0.9-1.5) | 1.6 (1.3-1.9)*** | 1.2 (0.9-1.6) |
| Ever been psychologically mistreated |
1.6 (1.3-1.9)*** | 1.1 (0.9-1.4) | 1.4 (1.2-1.7)*** | 1.3 (1.0-1.6) |
| Ever experienced war related torture (e.g. gunshot injuries, rape etc) |
1.4(1.07-1.85)* | 1.0 (0.7-1.3) | 1.6(1.2-2.1)*** | 1.4 (0.9-2.0) |
|
Partner related life events in later life¶ (included married, separated/widowed; n=3761) |
||||
| Had frequent rows or arguments with partner(s) |
0.9 (0.7-1.2) | 0.7 (0.5-1.0) | 1.2 (0.9-1.5) | 1.1 (0.8-1.6) |
| Partner(s) addicted to alcohol, rugs or medicines for one year or longer |
1.1 (0.8-1.4) | 0.8 (0.6-1.1) | 0.9 (0.7-1.2) | 0.8 (0.6-1.2) |
| Ever had serious relationship problems with partner(s) |
1.2 (0.9-1.5) | 0.9 (0.6-1.2) | 1.2 (0.9-1.6) | 1.0 (0.7-1.4) |
| Ever been beaten or physically mistreated by partner(s) |
1.0 (0.7-1.3) | 0.8 (0.6-1.2) | 1.1 (0.8-1.5) | 0.8 (0.6-1.1) |
| Ever been psychologically mistreated by partner(s) |
0.8 (0.6-1.1) | 0.7 (0.5-1.0) | 1.3 (1.0 -1.7) | 1.0 (0.7-1.4) |
| Partner ever attempted suicide (without fatal outcome) |
1.0 (0.8-1.4) | 0.8 (0.6-1.1) | 1.3 (0.9-1.7) | 1.2(0.8-1.7) |
| Partner(s) ever died | 1.1 (0.8-1.5) | 0.9 (0.6-1.3) | 1.2 (0.9-1.7) | 1.1 (0.7-1.6) |
P≤0.05
P≤ 0.01
P≤0.001
Adjusted for district, age group, having obtained formal education, marital status, being employed, & socio-economic status
DISCUSSION
This is the largest epidemiological study on mental illness that has ever been undertaken in Uganda. Unlike previous epidemiological studies which were only carried out in one region, this study covered all the 4 regions of the country and 14 districts. The paper sought to investigate the relationship between ecological, socioeconomic and adverse life events with major depressive disorder depression in this African country. The principal finding of this study is that socioeconomic factors operating at both ecological and the individual level are the strongest independent determinants of depression. Adverse life events which could be considered as proximal determinants of depression in this study were much less strongly associated with depression after adjusting for distal socioeconomic determinants.
Prevalence of major depressive disorder and ecological variation
The 29.3% overall prevalence of major depressive disorder obtained in this study is similar to the figures reported in previous studies for this country [3, 30]. Orley and Wing (1979) obtained a rate of 25.3% in a study in two villages in South-Central Uganda while Bolton and colleagues (2004) a quarter a century later obtained a rate of 24.4% in a study carried out in South-Western Uganda. These rates are much higher than those reported in the World Mental Health (WMH) survey initiative where the 12-month prevalence rates for a mood disorder varied between 0.8% to 9.1% [38].
The average prevalence figure given for this study masks large variations in rates at the level of districts: we observed a seven fold variation in the prevalence of major depressive disorder. Although the low rate of major depressive disorder for Bushenyi could be explained by the fact that this district is one of the most prosperous in the country and has not suffered from conflict recently, the high rate of major depressive disorder in the comparison district of Bugiri (44.4%) is not easy to explain. Bugiri district is also relatively prosperous, has not experienced war directly and has relatively good health infrastructure. Vinck and colleagues (2007) in their study of 4 war affected districts in Northern Uganda also observed a wide variation in the prevalence of major depressive disorder with district (varied between 30.9% and 62.6%) in their study. This was despite the fact that the districts in the Vinck et al (2007) study were more homogenous than those in this study (neighbouring each other, from the same Luo ethnic group, equally affected by the Northern civil war, relatively very poor and with poor health infrastructure). The results from Vinck et al (2007)’s study and of this study seem to suggest that other, yet undetermined, contextual factors may be responsible for the large ecological differences in district rates of major depressive disorder.
An attempt in this study to explore the contextual factors that may be operating at district level yielded only the factor of literacy rates which was reciprocally related to the district rates of major depressive disorder. However, since we excluded sub-counties with IDP camps we may have excluded the worst affected areas in those districts affected by ongoing conflict and hence failed to observe the effect of this factor. That in this study, ecological factors were strongly associated with major depressive disorder independently of individual factors is contrary to has been observed in the West [7,11,36], but similar to what has been observed in South Africa where less favourable clustering of social and economic circumstances had a protective effect on suicide [6]. These results therefore call for further studies to delineate the specific contextual factors that may be underlying major depressive disorder in the African socio-cultural context. Such wide variations in rates for mental disorder have been observed in multinational studies, such as the World Mental Health (WMH) survey initiative [38].
Socioeconomic risk factors
Female gender as compared to male gender conferred almost twice (1.7) the risk for depression in this study. Kaharuza and colleagues (2006) in a community sample of HIV/AIDS patients in Eastern Uganda observed a 1.6 fold increase in the risk for depression among females as compared to males. Patel and colleagues (2006 a,b) in India have suggested that that the association between common mental disorder and female gender is due to gender disadvantage experienced by women in that country. Indeed in this study some of the SES factors independently associated with depression are more frequently experienced by, or have more negative impact for women, namely; being separated/widowed, single parenthood, having no formal education and having no employment. These disproportional experiences for women are largely the product of socially constructed gender disadvantage. An increased risk of depression with age was observed in this study both among males and females being most pronounced after the age of 35 years. Both Bolton et al (2004) in a rural community sample in south-western Uganda and Kaharuza et al (2006) in a community sample of HIV positive persons in eastern Uganda observed an increase in the risk of depression with increasing age.
In this study, indices of poverty and deprivation were independently associated with major depressive disorder. In both genders, being separated/widowed and being in the poorer socioeconomic classes of III-V conferred an increased risk for major depressive disorder while being a single parent, lack of formal education, and not being employed conferred increased risk for major depression among females. Kaharuza et al (2006) in a community sample of HIV/AIDS patients observed a significant association between depression and having no income. Patel and colleagues (2006a) in India have also reported a strong association between common mental disorders and the deprivation and poverty indices of low education, low household income, lack of access to running water, having experienced hunger and difficulties in making ends meet.
Adverse Life Events
In this study, as in previous studies from sub-Saharan Africa, adverse life events were significantly associated with depression [1,5,31]. In both genders factors suggestive of disrupted family backgrounds i.e. death of a mother in males and death of a father in females were independently associated with depression. Previous authors both from the West and in Africa have also reported the association of major depression with dysfunctional parenting, low maternal care and orphanhood [1,31,32,35]. Previous findings from developed countries which demonstrated a gender specific effect of specific adverse life events on the risk of depression was also observed in this study [15,16].
However, we did not find any significant association between adverse life events related to the marital relationship and depression. Possible explanations for this lack of association between partner related adverse life events and depression in this study include the fact that the type of life events assessed in this study may not have the same threat/distressing potential in the Ugandan socio-cultural environment as in they have in the West where the assessment tool (the Life Events Inventory of the EPSIS I) was developed.
Indeed from previous studies from Africa, life events in the marital relationship that are associated with loss of face, shame and humiliation generate the most distress including precipitating suicide, domains which were not picked up by the Western designed Life Events Inventory of the EPSIS I [10,23,29].
Limitations
As our study is based on a cross sectional survey design, the causal direction between the various investigated factors and major depression cannot be demonstrated but at best inferred. Secondly, because of resource constraints, the depression assessment tool could only be calibrated within one language grouping and then generalized to the entire study districts. This may have introduced bias due to cultural differences between the different tribes in Uganda and due to inter-rater bias between the different interview teams, but this was thought to be minimal due to the marked similarities in the various language groupings and the shared cultural views about mental health.
Implications
Firstly, to address the burden of major depressive disorder in developing country settings such as in sub-Saharan Africa, there is need for a multifaceted approach that only provides clinical services, but also provides social interventions aimed at addressing poverty and economic disadvantage, family dysfunction and abuse and that addresses the inequalities still faced by women.
Secondly, there is need to investigate the underpinning of ecological or contextual factors in major depressive disorder in this environment.
Supplementary Material
Table 5.
Final multivariate Model of risk factors for MDD in males in a community sample from Uganda
| Risk Factor | Odds ratio (95% Confidence Interval) |
Adjusted Wald test P- Value |
|---|---|---|
| Adverse Life events | ||
| Mother died | 1.5 (1.2-2.0) | 0.002* |
| Parent(s) addicted to alcohol | 1.4 (1.1-1.9) | 0.01* |
| Socio-economic factors | ||
| Age Group | ||
| 15-18 yrs | 1.0 | |
| 19-24 yrs | 0.9 (0.5-1.7) | |
| 25-35 yrs | 1.0 (0.5-1.8) | <0.001* |
| 36-50yrs | 1.7 (0.9-3.1) | |
| 51-60yrs | 3.0 (1.5-6.1) | |
| 61+ yrs | 3.8 (1.8-7.8) | |
| Marital Status | ||
| Married | 1.0 | |
| Separated/widowed | 2.1 (1.5-3.0) | |
| Single parent | 1.3 (0.5-3.2) | <0.001* |
| Never married | 2.1 (0.7-6.8) | |
| Others | 0.9 (0.6-1.3) | |
| Socio-economic Status | ||
| Class I | 0.3 (0.1-0.5) | |
| Class II | 0.5 (0.3-0.8) | <0.001* |
| Class III | 0.7 (0.4-1.1) | |
| Class IV | 0.6 (0.5-0.8) | |
| Class V | 1.0 | |
| Ecological factors | ||
| Districts | ||
| Adjumani | 1.0 | |
| Mebende | 1.8 (0.8-4.3) | |
| Bugiri | 6.5 (2.8-15.3) | |
| Kapchorwa | 0.7 (0.2-1.9) | |
| Katakwi | 2.7 (1.1-7.0) | |
| Soroti | 4.9 (2.1-11.9) | |
| Kaberamaido | 5.2 (2.3-11.9) | |
| Apac | 0.9 (0.3-2.7) | <0.001* |
| Arua | 3.7 (1.7-8.0) | |
| Lira | 1.2 (0.5-3.0) | |
| Moyo | 6.1 (2.7-13.6) | |
| Nebbi | 3.1 (1.4-6.8) | |
| Yumbe | 4.5 (1.9-10.9) | |
| Bushenyi | 0.3 (0.1-0.8) | |
Statistically significant association
Table 6.
Final multivariate Model of risk factors for MDD in females among a community sample from Uganda
| Risk Factor | Odds ratio (95% Confidence Interval) |
Adjusted Wald test P- Value |
|---|---|---|
| Adverse Life events | ||
| Father died | 1.4 (1.1-1.8) | 0.02* |
| Ever been seriously beaten up |
0.07 | |
| Socio-economic factors | ||
| Age Group | ||
| 15-18 yrs | 1.0 | |
| 19-24 yrs | 0.9 (0.6-1.5) | |
| 25-35 yrs | 1.2 (0.8-2.0) | <0.001* |
| 36-50yrs | 1.9 (1.2-3.2) | |
| 51-60yrs | 1.9 (1.0-3.6) | |
| 61+ yrs | 3.2 (1.5-6.5) | |
|
Highest level of Education attained |
1.0 | |
| No formal education | 1.4 (1.1-1.8) | 0.02* |
| Marital Status | ||
| Married | 1.0 | |
| Separated/widowed | 2.5 (1.8-3.5) | |
| Single parent | 2.0 (1.1-3.8) | <0.001* |
| Never married | 0.8 (0.2-3.4) | |
| Others | 0.8 (0.5-1.1) | |
| Employment Status | ||
| Not employed | 1.0 | |
| In some employment/Students |
0.7 (0.5-0.9) | 0.02* |
| Socio-economic Status | ||
| Class I | 0.1 (0.1-0.2) | |
| Class II | 0.4 (0.2-0.7) | |
| Class III | 0.5 (0.3-0.8) | <0.001* |
| Class IV | 0.6 (0.4-0.9) | |
| Class V | 1.0 | |
| Ecological factors | ||
| Districts | ||
| Adjumani | 1.0 | |
| Mebende | 2.7 (1.4-5.4) | |
| Bugiri | 9.2 (5.3-16.2) | |
| Kapchorwa | 0.9 (0.3-2.6) | |
| Katakwi | 11.2 (6.1-20.3) | |
| Soroti | 8.1 (4.0 -16.4) | |
| Kaberamaido | 11.3 (6.5 -19.6) | <0.001* |
| Apac | 1.6 (0.6-4.2) | |
| Arua | 5.2 (2.7-10.0) | |
| Lira | 1.0 (0.5-2.0) | |
| Moyo | 10.1 (5.5-18.5) | |
| Nebbi | 5.2 (3.0-9.1) | |
| Yumbe | 10.3 (5.2-20.2) | |
| Bushenyi | 0.8 (0.4-1.8) |
Note: Statistically significant association
Acknowledgement
This project was funded by the Government of Uganda through a loan from the African Development Bank. Would like to acknowledge the advice provided by both Professor Richard Mollica, Director Harvard Program in Refugee Trauma and Dr Jonathan Levin of the MRC/UVRI Unit on AIDS in Uganda. Vikram Patel is supported by a Wellcome Trust Senior Clinical Research Fellowship in Tropical Medicine.
Contributor Information
Eugene Kinyanda, Medical Research Council/Uganda Virus Research Institute, Entebbe, Uganda P. O. Box 49, Entebbe, Ugand, Tel: 256 0414 320042/320272, Fax: 256 0414 321137, Eugene.Kinyanda@mrcuganda.org.
Patrick Woodburn, Medical Research Council/Uganda Virus Research Institute, Entebbe, Uganda.
Joshua Tugumisirize, Department of Psychiatry, Makerere University, Kampala, Uganda.
Johnson Kagugube, Uganda Bureau of Statistics, Kampala, Uganda.
Sheila Ndyanabangi, Mental Health Division, Ministry of Health, Kampala, Uganda.
Vikram Patel, London School of Hygiene & Tropical Medicine, London, United Kingdom.
REFERENCES
- 1.Atwine B, Cantor-Graae E, Bajunirwe F. Psychological distress among AIDS orphans in rural Uganda. Soc Sci Med. 2005;61:555–564. doi: 10.1016/j.socscimed.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 2.Bolton P, Neugebauer R, Ndogoni L. Prevalence of depression in rural Rwanda based on symptom and functional criteria. J Nerv Ment Dis. 2002;190:631–637. doi: 10.1097/00005053-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Bolton P, Wilk CM, Ndogoni L. Assessment of depression prevalence in rural Uganda using symptom and function criteria. Soc Psychiatry Psychiatr Epidemiol. 2004;39:442–447. doi: 10.1007/s00127-004-0763-3. [DOI] [PubMed] [Google Scholar]
- 4.Broadhead JC, Abas M. Life events, difficulties and depression among women in an urban setting in Zimbabwe. Psychol Med. 1998;28:29–38. doi: 10.1017/s0033291797005618. [DOI] [PubMed] [Google Scholar]
- 5.Broadhead J, Abas M, Sakutukwa GK, Chigwanda M, Garura E. Social support and life events as risk factors for depression amongst women in an urban setting in Zimbabwe. Soc Psychiatry Psychiatr Epidemiol. 2001;36:115–122. doi: 10.1007/s001270050299. [DOI] [PubMed] [Google Scholar]
- 6.Burrows S, Laflamme L. Living circumstances of suicide mortality in a South African city; an ecological study of differences across race groups and sexes. Suicide Life Threat Behav. 2005;35(5):592–603. doi: 10.1521/suli.2005.35.5.592. [DOI] [PubMed] [Google Scholar]
- 7.Cutrona CE, Russell DW, Brown PA. Neighborhood context, personality and stressful life events as predictors of depression among African American women. J Abnorm Psychol. 2005;1:3–15. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 9.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins symptom checklist (HSCL): a self report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 10.Fallers LA, Fallers MC. Homicide and Suicide in Busoga. In: Bohannan P, editor. African Homicide and Suicide. Princeton University Press; Princeton: 1960. pp. 65–93. [Google Scholar]
- 11.Fone D, Dunstan F, Williams G, Lloyd K, Palmer S. Places, people and mental health: A multilevel analysis of economic inactivity. Soc Sci Med. 2007;64:633–645. doi: 10.1016/j.socscimed.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 12.Information Discovery and Solutions Limited, editor. The Support to the Health Sector Strategic Plan Project, Results of the baseline survey report to provide basic data for the development of the National Communication Strategy, for the promotion of the National Minimum Health Care Package (NMHCP) Ministry of Health; Uganda: 2004. [Google Scholar]
- 13.Kaharuza FM, Bunnell R, Moss S, Purcell DW, Bikaako-Kajura W, Wamai N, Downing R, Solberg P, Coutinho A, Mermin J. Depression and CD4 cell count among persons with HIV infection in Uganda. AIDS Behav. 2006;10:S105–S111. doi: 10.1007/s10461-006-9142-2. [DOI] [PubMed] [Google Scholar]
- 14.Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- 15.Kendler K, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry. 2001;158:587–593. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- 16.Kendler K, Gardner CO, Prescott CA. Towards a comprehensive model for major depression in men. Am J Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC. The effects of stressful life events on depression. Ann Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- 18.Kerkhof AJFM, Bernasco W, Bille-Brahe U, Platt S, Schmidtke A. A WHO/EURO Multicentre study on parasuicide. In: Schiødt H, Aagaard B, editors. European Parasuicide study interview schedule EPSIS I version 6. Department and clinical and Health Psychology; University of Leiden: 1989. [Google Scholar]
- 19.Kinyanda E, Musisi S. War traumatisation and its psychological consequences on women of Gulu District. Review of Women’s Studies. 2001;11(1-2):102–132. [Google Scholar]
- 20.Kinyanda E. Mental Health chapter. In: Information Discovery and Solutions Limited, editor. The Support to the Health Sector Strategic Plan Project, Results of the baseline survey report to provide basic data for the development of the National Communication Strategy, for the promotion of the National Minimum Health Care Package (NMHCP) Ministry of Health; Uganda: 2004. pp. 108–132. [Google Scholar]
- 21.Kinyanda E, Hjelmeland H, Musisi S. Deliberate self-harm as seen Kampala, Uganda: A case-control study. Soc Psychiatry Psychiatr Epidemiol. 2004;39:318–325. doi: 10.1007/s00127-004-0748-2. [DOI] [PubMed] [Google Scholar]
- 22.Kinyanda E, Hjelmeland H, Musisi S. Negative life events associated with deliberate self-harm in an African population in Uganda. Crisis. 2005;26(1):4–11. doi: 10.1027/0227-5910.26.1.4. [DOI] [PubMed] [Google Scholar]
- 23.Kinyanda E, Hjelmeland H, Musisi S, Kigozi F, Walugembe J. Repetition of deliberate self-harm as seen in Uganda. Archives of Suicide Research. 2005;9(4):333–344. doi: 10.1080/13811110500182208. [DOI] [PubMed] [Google Scholar]
- 24.McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. J Health Soc Behav. 1990;31(2):162–172. [PubMed] [Google Scholar]
- 25.Minde KK. Psychological problems in Ugandan school children: A controlled evaluation. J Child Psychol Psychiatry. 1975;16:49–59. doi: 10.1111/j.1469-7610.1975.tb01871.x. [DOI] [PubMed] [Google Scholar]
- 26.Mollica RF, Sarajlic N, Chernoff M, Lavelle J, Vukovic IS, Massagli MP. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA. 2001;286(5):546–54. doi: 10.1001/jama.286.5.546. [DOI] [PubMed] [Google Scholar]
- 27.Monroe SM, Simon AD. Diathesis -stress theories in the context of life stress research: implications for the depressive disorders. Psychol Bull. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- 28.Musisi S, Kinyanda E, Leibling H, Mayengo K. Posttraumatic torture disorders in Uganda-A three year retrospective study of patient records as seen at a specialized torture treatment center in Kampala, Uganda. Torture. 2000;10(3):81–87. [Google Scholar]
- 29.Mzezewa S, Jonsson K, Åberg M, Salemark L. A prospective study of suicidal burns admitted to Harare burns unit. Burns. 2000;26:460–464. doi: 10.1016/s0305-4179(00)00019-x. [DOI] [PubMed] [Google Scholar]
- 30.Orley JH, Wing JK. Psychiatric disorders in two African villages. Arch Gen Psychiatry. 1979;36:513–521. doi: 10.1001/archpsyc.1979.01780050023001. [DOI] [PubMed] [Google Scholar]
- 31.Olley BO, Seedat S, Nei DG, Stein DJ. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS Patient Care STDS. 2004;18(8):481–487. doi: 10.1089/1087291041703700. [DOI] [PubMed] [Google Scholar]
- 32.Parker G. Parental ‘affectionless control’ as an antecedent to adult depression. A risk factor delineated. Arch Gen Psychiatry. 1983;40:956–960. doi: 10.1001/archpsyc.1983.01790080038005. [DOI] [PubMed] [Google Scholar]
- 33.Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Why women suffer common mental disorders. Population-based longitudinal study. Br J Psychiatry. 2006a;189:547–555. doi: 10.1192/bjp.bp.106.022558. [DOI] [PubMed] [Google Scholar]
- 34.Patel V, Kirkwood BR, Pednekar S, Pereira B, Barros P, Fernandes J, Datta J, Pai R, Weiss H, Mabey D. Gender disadvantage and reproductive health risk factors for common mental disorders in women. A community survey in India. Arch Gen Psychiatry. 2006b;63:404–413. doi: 10.1001/archpsyc.63.4.404. [DOI] [PubMed] [Google Scholar]
- 35.Sato T, Sakado K, Uehara T, Narita T, Hirano S, Nishioka K, Kashara Y. Dysfunctional parenting as a risk factor to lifetime depression in a sample of employed Japanese adults; evidence for the ‘affectionless control’ hypothesis. Psychol Med. 1998;28:737–742. doi: 10.1017/s0033291797006430. [DOI] [PubMed] [Google Scholar]
- 36.Skapinakis P, Lewis G, Araya R, Jones K, Williams G. Mental health inequalities in Wales, UK: multi-level investigation of the effect of area deprivation. Br J Psychiatry. 2005;186:417–422. doi: 10.1192/bjp.186.5.417. [DOI] [PubMed] [Google Scholar]
- 37.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM III R (SCID) I: history, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 38.The WHO World Mental Survey Consortium Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization World Mental Surveys. JAMA. 2008;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 39.Vadher A, Ndetei DM. Life events and depression in a Kenyan setting. Br J Psychiatry. 1981;139:134–137. doi: 10.1192/bjp.139.2.134. [DOI] [PubMed] [Google Scholar]
- 40.Vinck P, Pham PN, Stover E, Weinstein HM. Exposure to war crimes and implications for peace building in northern Uganda. JAMA. 2007;298(5):543–554. doi: 10.1001/jama.298.5.543. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.