Abstract
Background
A major challenge following successful weight loss is continuing the behaviors required for long-term weight maintenance. This challenge may be exacerbated in rural areas with limited local support resources.
Objective
This study describes and compares program costs and cost-effectiveness for 12-month extended care lifestyle maintenance programs following an initial 6-month weight loss program.
Design
A 1-year prospective controlled randomized clinical trial.
Participants/Setting
The study included 215 female participants age 50 or older from rural areas who completed an initial 6-month lifestyle program for weight loss. The study was conducted from June 1, 2003, to May 31, 2007.
Intervention
The intervention was delivered through local Cooperative Extension Service offices in rural Florida. Participants were randomly-assigned to a 12-month extended care program using either individual telephone counseling (n=67), group face-to-face counseling (n=74), or a mail/control group (n=74).
Main Outcome Measures
Program delivery costs, weight loss, and self-reported health status were directly assessed through questionnaires and program activity logs. Costs were estimated across a range of enrollment sizes to allow inferences beyond the study sample.
Statistical Analyses Performed
Non-parametric and parametric tests of differences across groups for program outcomes were combined with direct program cost estimates and expected value calculations to determine which scales of operation favored alternative formats for lifestyle maintenance.
Results
Median weight regain during the intervention year was 1.7 kg for participants in the face-to-face format, 2.1 kg for the telephone format, and 3.1 kg for the mail/control format. For a typical group size of 13 participants, the face-to-face format had higher fixed costs, which translated into higher overall program costs ($420 per participant) when compared to individual telephone counseling ($268 per participant) and control ($226 per participant) programs. While the net weight lost after the 12-month maintenance program was higher for the face-to-face and telephone programs compared to the control group, the average cost per expected kilogram of weight lost was higher for the face-to-face program ($47/kg) compared to the other two programs (approximately $33/kg for telephone and control).
Conclusions
Both the scale of operations and local demand for programs are important considerations in selecting a delivery format for lifestyle maintenance. In this study, the telephone format had a lower cost, but similar outcomes compared to the face-to-face format.
Keywords: Obesity, cost-effectiveness, randomized trial, rural health
INTRODUCTION
Despite equal or higher prevalence of obesity (1-3), sedentary lifestyle (3-5), and associated chronic diseases in rural counties in the United States (U.S.) (3-8), rural residents face many challenges in accessing health care services. Positive lifestyle behaviors that contribute to achieving a healthy weight may prevent or delay onset of certain chronic diseases including diabetes, and are therefore important considerations for rural residents (9). Other clinical research has indicated the efficacy of lifestyle interventions to improve diet, increase exercise, and achieve weight reduction, (10-13) but also have indicated that participants commonly re-gain much of the lost weight within a year of treatment (10,13-15). Distance to center-based care can present a barrier to ongoing participation in programs to improve weight maintenance in rural communities (1,6). Therefore, it is critical to examine alternative delivery methods for lifestyle maintenance programs to serve rural residents. This area has been studied previously with respect to outcomes and cost for individual versus group telephone counseling programs, with an emphasis on total costs for participants and program delivery combined (16,17). However, from a programmatic perspective, the economies of scale* that may be possible in urban settings might not exist in rural areas and can limit program offerings. This paper addresses this knowledge gap by focusing on program delivery costs of alternative formats for lifestyle maintenance programs.
Programmatic decision making in cost-effectiveness studies requires two basic questions: 1. Is the outcome of a program superior (or inferior) to others? and 2. Is the cost of a program lower (or higher) compared to others? Earlier work used randomized trial data to address the first question in finding that both the telephone and face-to-face formats were superior to an education/control group in limiting post-reduction weight regain at 12 months (p<0.05), but the two experimental program formats had weight regain outcomes that were statistically equivalent (16). An exploratory cost description was conducted in conjunction with the published clinical trial results, but the initial assessment of costs included both program and participant costs, was limited to a single program scale of operations, and was not provided at a level of detail that would be helpful in assisting local decision making for rural programs that may choose among program formats. Thus, the present study hypothesized that: (1) the telephone format would cost less to deliver than the face-to-face program, but more to deliver than the education/control program, and (2) the average cost-effectiveness ratio of the telephone format would be similar or better than the face-to-face format and better than the education/control program. The control group was anticipated to have lower average costs across most scales of operation due to the limited program resources needed. And, due to limited support offered to the control group, effectiveness was also anticipated to be lower compared to the two active lifestyle maintenance programs. In addition to examining these central economic hypotheses, this research aimed to offer information regarding program cost characteristics across a range of operating scales to inform local program decisions.
METHODS
Study Process and Recruitment
This research expanded the economic analysis for a previously-published prospective randomized clinical trial. Recruitment of participants and protection of subjects procedures were reviewed and approved by the full Institutional Review Board committee at the University of Florida. Full details regarding the main randomized trial and results, including participant recruitment, screening, and randomization procedures have been described in detail elsewhere, but are briefly summarized here as they pertain to the economic analysis (16).
Cooperative Extension Service (CES) offices in rural communities were the venues for the clinical trial. Participants included rural women ages 50 to 75. This demographic was chosen because of World Health Organization (WHO) publications emphasizing interventions that target weight loss and physical activity for women ages 50 and older and due to higher prevalence of obesity in rural versus urban and suburban areas (18,19) . Other study criteria required that participants: (1) resided in rural counties designated as Health Professional Shortage Areas (HPSA’s) in Florida (20), (2) had a body mass index (BMI) greater than 30, (3) weighed less than 159.1 kg, (4) did not have uncontrolled hypertension or diabetes mellitus and (5) did not have a diagnosis within the prior 12 months of cardiovascular, cerebrovascular, renal, or hepatic disease. Systematic clinical criteria for exclusion were: substance abuse disorders, significant psychopathology, musculoskeletal problems that prevented walking, and recent use of medications to promote weight loss. Study brochures were mailed to approximately 15,000 households in the six rural counties where the program was offered. The mailing list, purchased from a private agency, included households with women in the designated age range based on U.S. Census data. Potential subjects who responded to the announcement (N=559) were invited to attend an orientation session and, if interested, consented to participate. Once consented, an initial health screening visit was conducted and reviewed by the study physician, who determined the medical eligibility of each screened participant.
Participants first completed an initial 6-month lifestyle modification program to promote lifestyle behavior changes and weight loss. The program was delivered to groups of 10 to 14 participants at local Cooperative Extension Service (CES) offices by trained group leaders. Group leaders for both the initial program and subsequent intervention were CES family and consumer sciences agents or individuals with degrees in nutrition, exercise science, or psychology who were hired for the study for their expertise in behavioral science, dietetics, nutrition, and consumer education. Additional training with content-specific information based on the Diabetes Prevention Program was provided to group leaders via initial and ongoing training sessions (2,21,22). The initial 6-month program was offered at no charge to study participants and included a low-calorie eating plan (at least 1200 kcal/day), cooking demonstrations, strategies to increase physical activity, and training in behavior modification strategies such as goal setting and self-monitoring of daily food intake (13,15).
Interventions and Program Costs
Participants who completed the initial 6-month lifestyle modification program were randomly assigned to one of three 12-month extended care programs: 26 bi-weekly face-to-face group counseling sessions in a group setting, 26 bi-weekly one-on-one telephone counseling sessions, or 26 bi-weekly mailed newsletters without counseling (the education/control group). All participants, regardless of study assignment, received handouts describing how to use problem-solving strategies to handle obstacles to maintaining their weight loss and were encouraged to continue using behavioral weight control strategies, self-monitoring logs of food intake and physical activity.
Participants assigned to the control group were sent bi-weekly newsletters via regular postal delivery during the follow-up phase and were assessed for body weight and other outcomes 12 months after the initial weight loss program concluded. Program costs for the control group included staff time preparing and printing the newsletter, mailing costs, pre-paid postage for participants to provide their self-monitoring logs, and time spent reviewing the tracking logs provided by participants.
Participants assigned to the telephone counseling program received one-on-one contact with a group leader every other week and were provided with pre-paid postage to provide self-monitoring logs for review by program staff. The calls were scheduled in advance by the group leader and typically lasted 15-20 minutes. Conversations addressed barriers to maintaining eating and exercise behaviors required for sustaining lost weight. The program used a well-developed problem solving model developed by Perri and colleagues to help guide the discussions with each participant (23-25), with an expectation that each participant would complete at least 21 of the possible 26 calls. Program costs included group leader time for the phone calls, which included set-up, call sessions, call re-scheduling when needed, program training for the group leader, and telephone service to conduct the calls.
Participants in the face-to-face format attended bi-weekly meetings conducted as 1-hour group sessions staffed by a group leader and program assistant. Content was similar to the telephone-based program, but included group discussions and problem-solving. Program costs included program leader and assistant time for program training, time conducting the group meeting sessions (3 hours per meeting, which included session set-up, the main sessions, make-up sessions, and clean-up), travel time and mileage for the group leader and program assistant to attend the meetings, and the fair market value of space rental.*
Cost Measures
Study personnel collected outcome and cost data at three time points: baseline/enrollment, at the conclusion of the initial lifestyle modification program (month 6), and after the 12-month extended care phase (month 18). These measures included participants’ weight, and self-reported health status along with a variety of socio-demographic characteristics. During both the initial program and the extended care phase, participants were asked to keep periodic logs that monitored food intake, exercise, and other activities related to lifestyle maintenance. These logs were routinely collected and reviewed by program staff. Program staff, including group leaders and assistant group leaders, recorded time spent in various program activities including: counseling sessions, reviewing participant logs, administrative tasks, and training. Mileage for the program team to travel to rural sites for in-person sessions was based on the most direct route for a round-trip from the main study site, with the group leader and assistant sharing a ride. Other measures of staff time were obtained via treatment progress notes and self-reported recall of program staff activities for each of the delivery formats. From these sources, typical staff time costs were calculated for each delivery format. Payroll information was used to assess hourly wage rates for program staff; a standard rate for fringe benefits, 30%, was added to the hourly wage rate. Validity of the time and cost estimates was captured through verification of final estimates with multiple project staff, consistency in reporting across program staff, and subsequent verification of “typical, best-case, and worst-case” estimates by program leaders, assistants, the primary project manager, and the study’s principal investigator. Where any systematic discrepancies in estimates were noted, project logs and other source documents were re-reviewed with the principal investigator to determine the most appropriate estimate.
Other Outcome Measures
Measures of participants’ weight were obtained Detecto® 402KL Physicians Beam Scales at baseline, 6-months, and 18-months by a nurse or medical technician who was masked to participants’ randomized assignment. For each assessment, participants were asked to step on the scale two times to confirm their weight to the nearest 0.1 kilogram. While the overall clinical trial was designed and powered to detect actual changes in kilograms of weight as the primary outcome, the economic analysis presented here also used standardized weight change criteria established by the Institute of Medicine (IOM) regarding successful weight loss maintenance (26). Specifically, outcomes were classified into two categories: at least 5% weight loss maintained for 12 months, or 5% weight reduction not achieved and/or not maintained for 12 months. Self-rated health status (SRHS) measures relied on a standard visual analog scale, similar to a thermometer, on which individual participants rated their own health state on a scale from 0 (lowest) to 100 (highest). While this measure has the advantages of minimal respondent burden and being commonly used in economic evaluation studies, it is subjective. The multiple measures of outcomes were used to determine if there were dimensions of outcomes for which one of the two experimental programs was superior based on statistical analysis.
Analysis
The perspective for this analysis was that of the payer since the decision for a local county or other community entity to offer a similar program would depend largely on the program delivery costs rather than the costs of time and travel borne by individual program participants. Analysis of costs and outcomes relied on multiple methods and two primary software programs: Microsoft® Excel® 2010 and Stata™ version 10.1 (27,28). First, statistical and economic analysis methods were used to describe costs and outcomes. Program costs for each study arm were modeled according to fixed versus variable costs. Then, total and average (per-participant) program costs were calculated for a typical group size observed in the study (13 participants). Because program costs can vary with the scale of program operations, extrapolation methods were used to estimate total and average program costs for a range of group sizes. Thus, even though the fixed costs associated with the face-to-face program were relatively high compared to the telephone format, these costs were divided among more participants at larger scales of operation. In contrast, the variable (per-participant) costs for the telephone program increased along with program size. Next, overall expected values of program costs and participant outcomes were calculated for each program format, with an initial assumption of 13 participants per group (29). Costs per participant across a variety of program sizes were examined to determine whether optimal program format was sensitive to possible economies of scale.
To model outcomes, a simple decision tree was developed to include the randomly-assigned maintenance program along with the median initial weight reduction for each program and change in weight during the 12-month lifestyle maintenance phase. From this model, expected values for net kilograms of weight lost and expected change in SRHS were calculated for each lifestyle maintenance program and overall using the observed weight and SRHS from the study participants. The calculation of expected change in kilograms following the 12-month program, for example, was the weighted average for each participant observed in the program: where “i” represents an individual’s probability of the outcome and Δkg is the outcome (change in weight, measured in kilograms). Although participant characteristics were largely independent of program costs, random assignment of participants to program formats alleviated the potential for participant characteristics to differentially impact other program outcomes across treatment arms (16).
RESULTS
Of the 559 women screened for study participation, 298 initiated the 6-month lifestyle modification program, and 234 completed the program and were randomly assigned to the one of the three follow-up maintenance programs. Participants for whom final weight, SRHS, and participant cost data were missing were excluded from the analysis (n=19). The final analytic sample for the present cost analysis included the 215 participants assigned to the face-to-face (n=74), telephone (n=67), or education/control (n=74) format. Analysis of baseline characteristics such as weight, age, income, education levels, and health measures indicated that the three programs were well-balanced. The only statistically-significant difference among the three groups was related to racial/ethnic composition; a larger proportion of African-American women were assigned by chance to the telephone format.
The initial 6-month weight loss program showed statistically significant success in promoting weight loss and improving measures of clinical health. The average starting weight (assessed at baseline) was 97 kg. Most participants (83%) lost at least 5% of their baseline weight during the initial 6-month weight loss program, with an average reduction of 10 kg, or approximately 10% of bodyweight. There were no statistical differences in initial program weight loss success according to randomized group for the subsequent weight maintenance program.
The main randomized clinical trial results indicated that most rural participants were successful in losing a significant amount of weight during the initial 6-month program and participants assigned to the telephone and face-to-face 12-month maintenance programs regained significantly less weight than those in the mail/control group (16). Table 1 describes mean and median weight maintenance and self-reported health status outcomes following the 12-month lifestyle maintenance program. Non-normality of the distributions of data indicated use of non-parametric tests to assess statistical differences across the three programs along with a Bonferroni adjustment for multiple comparisons. These adjusted tests indicated no statistically significant differences across program formats using a p-value of 0.05. However, the sample sizes were inadequate to detect small differences between groups.
Table 1. Weight loss and Self-Reported Health Status (SRHS) Outcomes at Month 18 by Extended Care Program.
| Outcome | Telephone (n=67) |
Face-to-Face (n=74) |
Control (n=74) |
|---|---|---|---|
| Percent weight lost, months 0-18 | |||
| mean ± sd | 8.4 ± 8.5 | 9.2 ± 8.8 | 7.3 ± 8.3 |
| median (IQR)a | 6.6 (2.1-12.9) | 8.3 (3.1-14.6) | 6.0 (0.5-13.1) |
|
| |||
| Kilograms regained, months 6-18 | |||
| mean ± sd | 1.3 ± 5.5 | 1.1 ± 6.0 | 3.4 ± 6.0 |
| median (IQR) | 2.1 (-2.6-5.9) | 1.7 (-1.3-5.5) | 3.1 (-0.2-7.2) |
| Kilograms lost since baseline, months 0-18 | |||
| mean ± sd | 8.2 ± 8.4 | 9.0 ± 8.8 | 6.9 ± 7.8 |
| median (IQR) | 5.6 (1.8-13.3) | 8.0 (2.7-15.1) | 5.7 (0.5-11.3) |
| Maintained initial loss of ≥5% weight | |||
| Number of participants (%) | 36 (54) | 44 (60) | 39 (53) |
|
| |||
| SRHS, 0-100 scale | |||
| mean (month 18) ± sdc | 85.3 ± 11.0 | 84.9 ± 12.1 | 85 ± 13 |
| median (IQR) | 90 (80-95) | 90 (80-90) | 90 (80-90) |
|
| |||
| Change in SRHS since Baseline | |||
| mean ± sd | 6.4 ± 15 | 8.8 ± 15 | 5.3 ± 14 |
| median (IQR) | 5 (-2-16) | 6.5 (0-15) | 5 (0-15) |
|
| |||
| SRHS increased since baseline | |||
| Number of participants (%) | 38 (57) | 52 (70) | 45 (61) |
Sample includes study participants who completed all assessments
IQR = Inter-quartile Range
Baseline mean SRHS measures were: 78.8 ± 12.6 (telephone), and 76.1 ± 15.1 (face-to-face). Whereas the face-to-face group started with a lower average measure, both formats had similar average and median measures for SRHS at month 18.
Note: Due to non-normality of the distributions of the variables, non-parametric statistical tests (Wilcoxon rank-sum tests with a correction for multiple comparisons) were conducted. Results indicated no statistically significant difference across program formats using an alpha of 0.05. Weight regain from months 6-18 was significantly higher for the mail/control group without adjusting for multiple comparisons, but was only marginally significant once this adjustment was included (p=0.67).
Program costs were categorized as fixed costs that did not vary according to the number of participants and variable costs that were incurred on a per-participant basis. As such, fixed costs would be considered to be similar regardless of the number of participants. Variable costs (rounded to the nearest half-dollar) were calculated as $46 per participant for the face-to-face program, $84.50 for the control group, and $155.50 for the telephone group. Most staff time was fixed for the face-to-face format; group leaders and program assistants participated in each of the face-to-face sessions regardless of the number of attendees. The fair-market value (opportunity cost) for local facility rental and staff time to conduct meetings represented core fixed costs for the face-to-face program. However, there were minimal variable costs, such as postage and mailings, related to individual participants. Variable costs primarily entailed printing costs for handouts and staff time reviewing self-monitoring logs. In contrast, staff time was primarily variable for participants in the telephone format since the group leader’s time was dependent on the number of phone calls needed for program completion. The primary costs for the control group were related to newsletter preparation (a fixed cost) and review of participants’ logs (a variable cost), both of which were managed by a staff program assistant.
Table 2 presents program cost calculations for a program size of 13 participants, corresponding to the typical group size observed in the study. At this scale of operations, total and average costs for the face-to-face program were highest, particularly when staff travel costs were included.* Excluding travel costs, the per-participant estimate of total costs was $420 for the 12-month face-to-face program. Costs for the telephone and control group format were lower at $268 and $226, respectively.
Table 2. Program Delivery Costs by Maintenance Program, Example with 13 participants per programa.
| Costsa | Telephone | Face-to-Face | Control |
|---|---|---|---|
| Fixed Costs ($) | |||
| Staff Time for Sessionsb | - | 2411 | |
| Telephone Service or Facility Rentalc | 360 | 1000 | - |
| Staff Training and Administrative Timed | 1099 | 1457 | 1838 |
| Staff Travel to/from Sessionse | 1966 | ||
|
| |||
| Subtotal: Fixed Costs (Excluding Travel) | 1459 | 6834 (4868) | 1819 |
|
| |||
| Variable Costs ($) | |||
| Staff time for Sessionsf | 1270 | - | - |
| Postage, Handouts, and printing | 195 | 39 | 349 |
| Subtotal: Variable Costs | 2020 | 595 | 1099 |
|
| |||
|
Total Program Costs (And Costs Excluding
Travel) |
$3479 | $7429 ($5463) | $2938 |
|
| |||
| Average Cost per Participant (excluding travel) | $268 | $571 ($420) | $226 |
Cost estimates are presented for the delivery of a 12-month maintenance program. These estimates exclude indirect operating costs that would not differ by program such as office space for program staff, computer and other technical resources, administrative overhead, and utilities other than telephone.
Each face-to-face group session required approximately 3 hours for both the group leader and program assistant, including time for make-up sessions, setting up the room, and post-session clean-up. We assumed each leader and assistant attended 24 of 26 bi-weekly sessions, which was typical for the study. Staff time values relied on wage rate information. For group leaders, an annual salary of $30,000 per year was assumed, which corresponded to an hourly wage rate of $14.31 (=$30,000/2096 hours) plus fringe benefits (30%) for an effective hourly wage rate of $18.60. For program assistants, the hourly wage rate was calculated using an annual salary of $24,000 per year, which corresponded to $11.45 per hour plus fringe benefits, or $14.89 per hour.
Facility space for bi-weekly meetings was donated by the CES offices for the study. However, if a similar program were to be offered outside of the research environment, fair-market value of similar facilities (e.g., CES offices, community churches with kitchen/meeting space) was estimated to be $1000 per year.
Required leader training was 2 hours per month for the telephone and face-to-face program formats. Administrative time for documentation and miscellaneous activities was estimated from staff time logs. Total (fixed) leader training and administrative time was estimated to be 43.5 hours over 12 months for both the telephone and face-to-face formats. Assistants prepared the 26 bi-weekly mailings for the control group, which required 4 hours of time for each mailing (26*4=104 total hours). Assistants were required to complete the 2-hour monthly training sessions for the face-to-face program and spent approximately 1.5 hours per participant over the 12 months conducting miscellaneous program-related activities. Total time for these activities was estimated to be 147.5 hours over 12 months for each program.
Staff travel from the main study site included the time and distance for a team (program leader and assistant) to travel round-trip for 26 program meetings, using a mileage rate of $0.50 per mile and roundtrip distance of 101.2 miles (average across study sites). Average roundtrip travel time was estimated as 2.2 hours per person (group leader and assistant). In practice, programs offered in rural locations may be able to recruit qualified local staff who would not incur or be reimbursed for these costs. As such, estimates without travel costs are also included in this table and were used in subsequent results.
Each completed call was estimated to require 15 minutes of program leader time, including call-backs. For this illustration, we assumed the group leader was able to complete 21 calls per participant (21 calls × 13 participants × 15 minutes per call × $14.31 per hour).
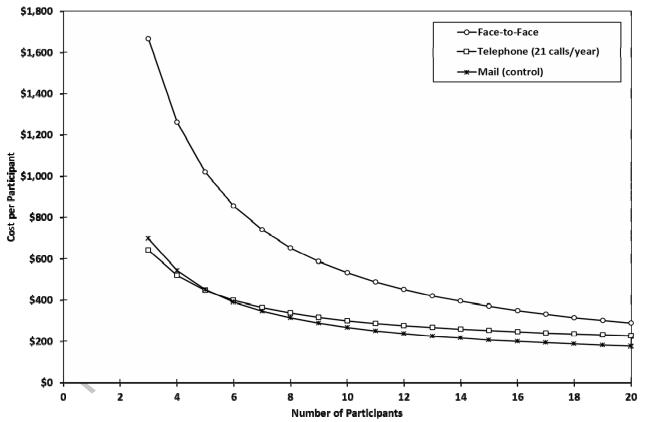
Figure 1 expands the information provided in Table 2 with a summary of the total expected program costs per participant for group sizes ranging from three to 20 participants. If the program is offered to fewer than five participants, the telephone program was least costly; average costs were even lower than those associated with the mail/control group. However, because the primary cost for the control group was related to the fixed costs of newsletter preparation, average costs for this format are lower for increasing scales of operation. Higher fixed costs for the face-to-face format lead to higher overall costs at the scales of operation studied here.
Figure 1.
Program Cost per Participant by Scale of Operations and Program Type
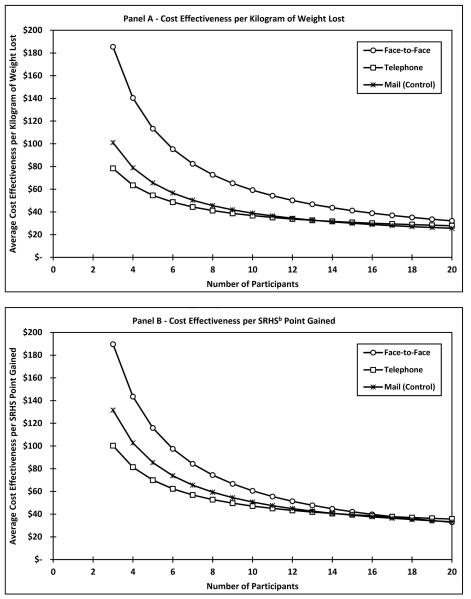
Tables 1 and 2 along with Figure 1 provide a description of the program outcomes and costs. However, the descriptive findings do not offer strong evidence regarding which program option rural communities should adopt based on cost-outcome criteria. Thus, a description of average cost-to-expected outcome ratios was needed because a rural community would likely offer a single program format rather than multiple formats. And, because the outcomes of interest to decision-makers may be multi-faceted to include both weight loss and other salient health outcomes, both net kilograms of weight lost and change in SRHS were used as outcomes in Table 3 and Figure 2.
Table 3. Average Cost-Effectiveness ratios for Programs with 13 participants.
| Group | (1) Expected Cost Per Participanta |
(2) Expected Point Gain in SRHS per participant (0-100 scale)b |
(3) Expected Cost per Point Gain in SRHSc |
(4) Expected weight loss(Kg) |
(5) Expected Cost per Kg weight lossd |
|---|---|---|---|---|---|
| Telephone Counseling |
$268 | 6.4 | $ 41.88 | 8.2 | $32.68 |
| Face-to-Face Counseling |
$420 | 8.8 | $ 47.73 | 9.0 | $46.67 |
| Control | $226 | 5.3 | $42.64 | 6.9 | $32.75 |
Notes: Outcomes of SRHS and Weight are changes from Baseline to Program completion (18 months)
Estimated with an assumption of 13 participants per group for a 12-month lifestyle maintenance program. Travel costs were excluded for the Face-to-Face program, since these costs may be unique to the study’s program delivery parameters. See Table 2 for calculation details.
Expected point gain in SRHS was calculated using data collected from the trial with a decision tree model in TreeAge®, where the probability of each outcome was multiplied by the expected SRHS value associated with the outcome. The probability of successful maintenance of 5% weight loss multiplied by the SRHS gain associated with success was added to the probability of unsuccessful maintenance of 5% weight reduction multiplied by the associated SRHS change, which can be stated as: EV(program X)= [prob(success)*SRHS change(success)] + [(1-p(success))*SRHS change(no success)]. For the telephone counseling program, the numeric values were as follows: prob(success)=36/67 or 0.54, SRHS change(success)=11.33, 1-prob(success)=.46, SRHS change(no success)=0.67. Thus, the expected value for SRHS change for the telephone counseling program is: (0.54*11.33) +(0.46*0.67)=6.4.
Expected cost per point gain in SRHS is the expected program cost divided by the expected point gain in SRHS from baseline to final assessment following the 6-month weight loss program and 12-month follow-up program (e.g., month 18). For the telephone counseling group, it is $268/6.4=$41.88
Expected cost per kg weight lost is the expected program cost per participant divided by the expected net weight loss from baseline to month 18 (see Table 1). For the face-to-face counseling group, it is $420/9.0= $46.67
Figure 2. Average Cost-Effectiveness Ratios by Number of Program Participantsa.
a Average Cost-effectiveness ratios were calculated using the methods described in Table 3. However, for each program size presented in this table, average program costs were estimated as the sum of fixed and variable costs per participant and divided by the expected value for participant outcomes for each program format.
b SRHS represents self-reported health status
Assuming 13 participants per group (Table 3), the three programs had similar average costs per expected point increase in SRHS ($42 to $48 per point gain from baseline to program completion 18 months later), with the telephone program having the lowest cost per SRHS point gain. The average cost per kilogram lost indicates a similar pattern, with the highest ratio associated with the face-to-face counseling group (around $47) and lower ratios for the education/control and telephone formats (both around $32.75). Figure 2 extends the information presented in Table 3 across a range of potential program sizes for rural communities to provide information that supports local program decision-making. Based solely on this information, rural communities with limited resources that opt for one of the “active” programs for lifestyle maintenance would be expected to choose the telephone-based program to ensure a lower average cost per participant (Figure 1). With 17 or fewer participants, the telephone program has lower average cost per point gain in SRHS (Figure 2, panel B) compared to the face-to-face program. However, the actual difference in both these average cost-effectiveness ratios was modest for programs with at least ten participants.
Discussion
Programs that result in successful initial weight loss and subsequent lifestyle maintenance are complex and require tools and support methods that meet the unique needs of participants. Learning which methods and modalities are effective is critical given the epidemic rates of obesity and associated increased rates of morbidity and mortality. In the present study, both the face-to-face and telephone forms of treatment delivery (interactive) were more effective at helping participants maintain lost weight compared to the control group. And, while both interactive formats were successful, telephone delivery was generally less expensive to deliver and demonstrated a more favorable average cost-effectiveness ratio for both kilograms lost and self-reported health status gains compared to the face-to-face option for group sizes typical in rural areas. This result is directly related to the higher fixed costs associated with the face-to-face program format, including space rental and staff time, which were invariant to the number of participants. The telephone counseling program required fewer fixed resources related to space and staffing, which could make it a more attractive format for programs with limited resources.
The results of this study both complement and extend findings from other recent studies. For example, a long-term follow-up clinical trial conducted by Wing and colleagues compared face-to-face and internet-based weight loss maintenance programs with a newsletter control (29-30) . Overall, they reported that newsletters were less effective in weight loss maintenance compared to the two interventions; however, cost-effectiveness was not a component of the Wing et al. study. And, although it is not possible to directly compare all the results presented in Table 3 and figure 2 to other studies, the expected cost per kilogram of weight lost is similar to results reported by a variety of commercial weight loss programs and the average weight loss maintained for at least a year was better than the typical results of many commercial weight loss programs (31). The descriptive analysis of program costs for the individual telephone program is consistent with results recently reported for other trials indicating that remote counseling can support successful weight loss and lifestyle maintenance as well as in-person programs (17,32). Results presented in this paper indicate that the costs of remote individual telephone counseling are lower and may be preferable to other delivery formats when effectiveness is equivalent.
One factor in interpreting these results is that costs per participant and average cost-effectiveness depend, in part, on available local resources to offer programs. The total program costs of a 12-month lifestyle maintenance program delivered to a group of 13 participants ranged from under $3000 for a program with bi-weekly newsletter mailings and self-monitoring logs to almost $7500 for biweekly face-to-face group sessions requiring travel for the program staff (Table 2). The average program cost per participant to offer the 12-month maintenance program for 13 participants ranged from $226 to $571 per participant, which is comparable to the monthly costs for participants to join commercial weight loss and lifestyle programs such as Weight Watchers©. A challenge in determining relative cost effectiveness based on program size is that it is rare for lifestyle programs to be offered for more than 20 participants per group, with a most common group size of 10-15 participants per group (13). The face-to-face program had the best expected outcomes, but also the highest average cost among the three program types for groups with 20 or fewer participants. While the face-to-face program may offer economies of scale for larger scales of operation, the scale needed may exceed the program demand and capacity for many rural communities. Three of the six counties included in this study had a local venue capacity that would allow forty or more participants or classes, and three did not. Larger group sizes may also limit the opportunity for individual attention to participants, which is a key component of the behavioral lifestyle program concept. Though current understanding of the dynamics of group size and attention with respect to effectiveness is limited, having such information could influence optimal program choices.
Another factor to consider in determining which type of program to deliver is what modality may be most accessible and well received by participants. Demand for lifestyle programs may vary over time and across diverse rural areas. As such, frequency of program offerings and resources available in unique local areas may need consideration in determining the most cost-efficient program format. Telephone delivery to a few individual participants in several smaller groups that are staggered to begin over time may require less content re-training for program staff over 12-months than a single, yet larger, face-to-face or telephone program that is offered for enrollment once each year. Larger classes may be an option for areas that have ample venue space and can capture the needed economies of scale. Participant convenience, a variable not considered in this analysis, may be a key consideration for rural communities. For example, rural residents who do not own a car are dependent on others or limited rural public transportation systems services (33); this may limit rural residents’ ability to attend regularly scheduled face-to-face classes. For these situations, a telephone program may be a more viable option.
There are several possible limitations to this research. First, the results presented in this paper are descriptive and reflect a sample of participants who met the eligibility criteria for a randomized clinical trial. Next, the analysis excluded participants who did not fully participate in baseline and follow-up data collection efforts. Although imputation methods were feasible in the initial study that used weight regain from months 6 to 18 as the primary outcome (16), there were not sufficient insights on how participants with missing outcome data would differ to place “bounds” on these assumptions, which were needed for the economic analysis. It is likely that across the program formats participants who completed the study were more enthusiastic and motivated than those who did not. Third, the analysis included several assumptions based on a detailed understanding of the programs offered and participants who enrolled in the study. Readers should be cautious in generalizing these assumptions to other study populations or programs. Additional studies with larger populations and criteria to include men and a wider range of ages and group sizes would be necessary to determine whether the results from the clinical trial sample would apply to other rural populations. Finally, a consideration in designing the prospective measures for this study was whether self-reported health status was a reasonable indicator of the lifestyle program outcome. Given the multi-faceted goals of lifestyle maintenance, the simple visual-analog measure over time was included to capture participants’ perception of their own overall health status. Assessment of changes in quality-adjusted life years (QALYs) was beyond the scope of the desired respondent time for survey data collection, but would be indicated for future studies. Despite these limitations, this study offers several insights to improve understanding of program costs and outcomes for post-weight reduction lifestyle maintenance that can aid in decision-making regarding weight maintenance program format for rural communities. The results highlight the important distinction between fixed and variable costs in selecting optimal formats for community health programs. Such information can assist diverse rural communities in careful planning and selection of programs to promote healthy eating habits and lifestyle choices for local residents.
Conclusions
With obesity rates at an all-time high, it is critical for researchers to develop effective treatment programs that promote weight loss and maintenance in ideal medical settings. But, it is also important to develop these interventions for translation to the real-world that can be implemented in any setting, including rural areas. In the present study, three lifestyle maintenance program formats were compared for salient outcomes of weight change, health status, and cost at one-year in six rural counties in the Southeast that was delivered through Cooperative Extension Offices. While both the face-to-face and telephone programs were most effective at minimizing weight regain, the telephone treatment modality had the most favorable average cost effectiveness of the two. The scale of operations, availability of resources, and local demand for programs are all important considerations in selecting a delivery format for lifestyle maintenance in rural settings. However, this study suggests that effective weight loss and maintenance programs can be economically delivered in multiple modalities using an evidence-based problem-solving treatment approach. While more research is needed, these results contribute to understanding how effective long-term management of obesity can be delivered in a cost-effective manner in real-world rural settings.
Footnotes
In economics, “economies of scale” typically refers to a specific relationship between average costs and production levels in which costs decrease with increasing output. Here, it specifically refers to decreasing average costs as the number of participants served per program increases.
While the CES offices donated the meeting space used in this study, there were two reasons to include this as a consideration in the analysis. First, there is an opportunity cost associated with providing the space to this program versus others. Second, it is unclear whether meeting space would be donated in other situations.
For this study, staff traveled from the main study site to the rural locations where the bi-weekly meetings were held. Because this expense may not be relevant in most situations for program planning, calculations without travel costs were included for all other results presented in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tiffany A. Radcliff, Department of Family Medicine, University of Colorado Denver, Mail Stop F413, P.O. Box 6508, Aurora, CO 80045-0508 (during study and present); Department of Health Policy and Management, Texas A&M Health Science Center, School of Rural Public Health, MS 1266, College Station, TX 77843-1266. (present) Tiffany.Radcliff@ucdenver.edu, tel. 979-862-7821, fax: 979-458-0656.
Linda B. Bobroff, Department of Food and Nutrition, IFAS, University of Florida, 3026-B McCarty Hall D PO BOX 110310, Gainesville, FL 32611-0310 bobroff@ufl.edu, tel. 352-273-3521 fax: 352-392-8196.
Lesley D. Lutes, Department of Psychology, East Carolina University, 104 Rawl Building, Greenville, NC 27858-4353 lutesl@ecu.edu, tel. 252-328-6283.
Patricia E. Durning, Department of Clinical and Health Psychology, College of Public Health and Health Professions, University of Florida, P.O. Box 10065, Gainesvillve, FL 32610 pdurning@phhp.ufl.edu, tel. 352-273-6037, fax: 352-273-6199.
Michael J. Daniels, Department of Statistics, 102 Griffin-Floyd Hall, P.O. Box 118545 Gainesville, FL 32611-8545, mdaniels@stat.ufl.edu, tel. 352-273-1845, fax: 352-392-5175.
Marian C. Limacher, Division of Cardiiovascular Medicine, School of Medicine, University of Florida, PO Box 100277, Room M-409 Gainesville, FL 32611-0277, limacmc@medicine.ufl.edu, tel.: 352-846-1228, fax: 352-846-1217.
David M. Janicke, Department of Clinical and Health Psychology, College of Public Health and Health Professions, University of Florida, P.O. Box 10065, Gainesvillve, FL 32610 djanicke@phhp.ufl.edu, tel. 352-273-6046, fax: (352) 273-6156.
A. Daniel Martin, Department of Physical Therapy, College of Public Health and Health Professions, University of Florida, P.O. Box 100154, Gainesville, FL 32610 dmartin@phhp.ufl.edu, tel. 352-273-6105, fax: 352-273-6109.
Michael G. Perri, University of Florida, College of Public Health and Health Professions, 101 S. Newell Drive, Suite 4101, Gainesvillve, FL 32610 mperri@phhp.ufl.edu, tel. 352-273-6214, fax: 352-273-6199.
References
- 1.Eberhardt MS, Ingram DD, Makuc DM, et al. Urban and rural health chartbook: Health United States, 2001. National Center for Health Statistics; Hyattsville, MD: 2001. [Google Scholar]
- 2.Jackson JE, Doescher MP, Jerant AF, Hart LG. A national study of obesity prevalence and trends by type of rural county. J Rural Health. 2005;21(2):140–148. doi: 10.1111/j.1748-0361.2005.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 3.Lutfiyya MN, Lipsky MS, Wisdom-Behounek J, Inpanbutr-Martinkus M. Is rural residency a risk factor for overweight and obesity for US children? Obesity. 2007;15(9):2348–2356. doi: 10.1038/oby.2007.278. Silver Spring. [DOI] [PubMed] [Google Scholar]
- 4.Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health. 2004;20(2):151–159. doi: 10.1111/j.1748-0361.2004.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 5.Call KT, Casey MM, Radcliff T. Rural beneficiaries with chronic conditions: Does prevalence pose a risk to medicare managed care? Managed Care Quarterly. 2000;8(3):48–57. [PubMed] [Google Scholar]
- 6.Barnett E, Halverson J. Disparities in premature coronary heart disease mortality by region and urbanicity among black and white adults ages 35-64, 1985-1995. Public Health Rep. 2000;115(1):52–64. [PMC free article] [PubMed] [Google Scholar]
- 7.Dobalian A, Tsao JC, Radcliff TA. Diagnoes mental and physical health conditions in the united states nursing home population: Differences between urban and rural facilities. J Rural Health. 2003;19(4):477–483. doi: 10.1111/j.1748-0361.2003.tb00585.x. [DOI] [PubMed] [Google Scholar]
- 8.Phillips CD, McLeroy KR. Health in rural America: Remembering the importance of place. Am J Public Health. 2004;94(10):1661–1663. doi: 10.2105/ajph.94.10.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wylie-Rossett J, Herman WH, Goldberg RB. Lifestyle intervention to prevent diabetes: Intensive and cost effective. Curr Opin Lipidol. 2006;17(1):37–44. doi: 10.1097/01.mol.0000203890.27267.eb. [DOI] [PubMed] [Google Scholar]
- 10.National Institutes of Health, National Heart, Lung and Blood Institute Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obes Res. 1998;6(suppl 2):51S–219S. [PubMed] [Google Scholar]
- 11.Knowler WC, Barett-Connor E, Fowler SE, et al. Reduction in incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Look AHEAD Research Group. Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: One-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. 2007;132(6):2226–2238. doi: 10.1053/j.gastro.2007.03.051. [DOI] [PubMed] [Google Scholar]
- 14.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 15.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: The weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 16.Perri MG, Limacher MC, Durning PE, et al. Extended-care programs for weight management in rural communities: The treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med. 2008;168(21):2347–2354. doi: 10.1001/archinte.168.21.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Befort CA, Donnelly JE, Sullivan DK, Ellerbeck EF, Perri MG. Group versus individual phone-based obesity treatment for rural women. Eat Behav. 2010;11(1):11–17. doi: 10.1016/j.eatbeh.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization, editor. Obesity: Preventing and managing the global epidemic. World Health Organization; Geneva, Switzerland: 1998. No. WHO/NUT/NCD/98.1. [PubMed] [Google Scholar]
- 19.Sobal J, Troiano R, Frongillo E. Rural-urban differences in obesity. Rural Sociology. 1996;61(2):289–305. [Google Scholar]
- 20.US Department of Health and Human Services . List of designated primary medical care, mental health, and dental health professional shortage areas. [Accessed 10/21, 2007]. http://bhpr.hrsa.gov/shortage. [Google Scholar]
- 21.Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29(9):2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seidel MC, Powell RO, Zgibor JC, Siminerio LM, Piatt GA. Translating the diabetes prevention program into an urban medically underserved community: A non-randomized prospective intervention study. Diabetes Care. 2008;31(4):684–689. doi: 10.2337/dc07-1869. [DOI] [PubMed] [Google Scholar]
- 23.Perri MG, Corsica JA. Improving the maintenance of weight lost in behavioral treatment of obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity. 3rd Edition Guilford Press; Hoboken, NJ: 2002. pp. 357–379. [Google Scholar]
- 24.Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. J Consult Clin Psychol. 2001;69(4):722–726. [PubMed] [Google Scholar]
- 25.Perri MG, Nezu AM, Viegner BJ. Improving the long-term management of obesity: theory, research, and clinical guidelines. John Wiley & Sons; New York, NY: 1992. [Google Scholar]
- 26.Institute of Medicine, editor. Weighing the options: Criteria for evaluating weight management programs. Government Printing Office; Washington, D.C.: 1995. [Google Scholar]
- 27.Stata statistical software . version 10.1. StataCorp. College Station; TX: 2010. [Google Scholar]
- 28.Microsoft Excel 2010. Microsoft Corporation; Redmond, WA: 2010. [Google Scholar]
- 29.Veney JE, Kaluzny AD. Evaluation and decision making for health services. 3rd ed. Health Administration Press; Ann Arbor, MI: 1998. Cost benefit and cost effectiveness. [Google Scholar]
- 30.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355(15):1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 31.Tsai AG, Wadden TA. Systematic review: An evaluation of major commercial weight loss programs in the united states. Ann Intern Med. 2005;142(1):56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 32.Appel LJ, Clark JM, Yeh H, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rural transportation at a glance . Agriculture Information Bulletin Number 795. Economic Research Service; [Accessed November 07, 2011]. 2005. U. S. Department of Agriculture Web site. Available at http://www.ers.usda.gov/publications/aib795/aib795_lowres.pdf. [Google Scholar]