Abstract
Context
Hospice patients are at risk for falls and hip fracture with little clinical information to guide clinical decision making.
Objectives
To examine whether surgery is done and survival of hip fracture surgery among persons receiving hospice services.
Methods
This was an observational cohort study from 1999 to 2007 of Medicare Hospice beneficiaries aged 75 years and older with incident hip fracture. We studied outcomes among hospice beneficiaries who did and did not have surgical fracture repair. Main outcomes included the trends in the proportion of those undergoing surgery, the site of death, and six-month survival.
Results
Between 1999 and 2007, approximately one percent (n=14,400) of patients 75 and older admitted with a diagnosis of their first hip fracture were receiving hospice services in the 30 days prior to that admission and 83.4% underwent surgery. Among patients on hospice at the time of the hip fracture, 8.8% died during the initial hospitalization and an additional two-thirds died within the first six months on hospice. The median survival from hospital admission was 25.9 days for those forgoing surgery compared to 117 days for those who had surgery. adjusted for age, race, and other covariates (P <0.001).
Conclusion
Despite being on hospice services, the majority underwent surgery with improved survival. Sixty-six percent of all individuals on hospice at the time of the fracture died in the first six months, with the majority returning to hospice services.
Keywords: Hip fracture, hospice use, survival
Introduction
Hospice is a philosophy of care focusing on holistic care of persons with terminal illness. In the U.S., the election of the Medicare Hospice benefit requires persons to agree to treatment focusing on palliation not curative treatment of the terminal illness. Hospice services can be received in the individual’s home (e.g., private residence, assisted living facility), nursing home, or hospital. Receipt of hospice differs from palliative care services in that the individual has received a diagnosis of a terminal illness from a physician certifying the individual has less than six months to live and has chosen comfort care instead of curative treatment for the terminal illness. By contrast, receipt of palliative care in the U.S. is available for patients regardless of the stage of their disease, does not stipulate that the individual has a terminal diagnosis with a life expectancy of less than six months, and does not require that the individual waive curative treatments. An important clinical question is whether hospice patients who suffer a hip fracture should undergo surgery. Surgical intervention followed by rehabilitation is the principle medical treatment for individuals admitted to the hospital with a hip fracture.1,2 Previous research has estimated 6.2% to 8.0% of first hip fracture hospital admissions did not undergo surgical intervention.7–9 Non-operative treatment has been associated with advanced age, black race, multiple comorbidities, and medical instability.2,6–8 These studies did not address the outcomes of people enrolled in hospice. To our knowledge, there has only been one study of 15 hospice patients in the U.S. that examined survival.
Clinicians caring for hospice patients are often faced with a patient who has a terminal disease and then suffers an acute fracture. The decision then has to be made as to whether proceeding with surgery makes sense in the context of patient preferences, overall life expectancy, and the patient’s quality of life. There is little data on the outcomes of surgery on which to make an informed decision.
This study’s objective was to use a national cohort of fee-for service Medicare Hospice beneficiaries who had their first hip fracture between 1999 and 2007 to describe whether surgery was performed and the outcomes in surgical versus non-surgical treatment. Five research questions guided this study: 1) what was the number of Medicare hospice patients admitted to the hospital in the U.S. for a hip fracture? 2) What proportion of Medicare patients on hospice admitted to the hospital with a diagnosis of a hip fracture underwent a surgical intervention? 3) Does survival differ among Medicare hospice patients based on treatment after hip fracture (i.e., surgical or non-surgical intervention)? 4) Among those who died in the first six months after fracture, what proportion was on hospice at the time of death? and 5) Has the use of surgical intervention for older adults on hospice changed over time?
Methods
Data Source
Patient information was obtained for 100% Medicare Provider Analysis and Review (MEDPAR) inpatient files, hospice files, the nursing home residential assessment minimum data set (MDS), and denominator files from January 1, 1999 to December 30, 2007. Information on site of death and the type of services used was based on the Residential History File (RHF) methodology.10 The RHF integrates Medicare administrative files including the denominator file and Medicare claims with the MDS to create an individualized historical record of service utilization and site of care including sequence of care sites, length of stay at each service location, and date and location at time of death.10
Cohort Development
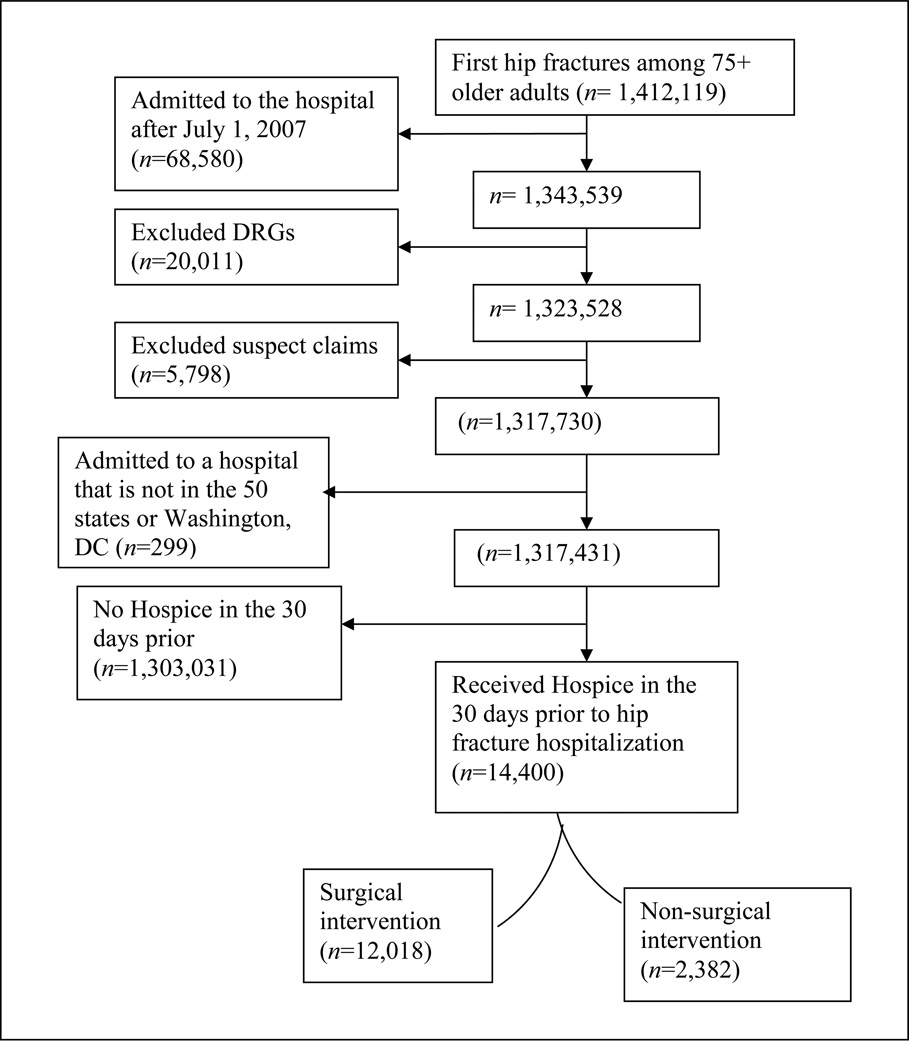
Beneficiaries were eligible if they were 75 years of age or older at the time of the admission for their first hip fracture, were enrolled in Medicare part A and part B, and were not enrolled in a managed care health plan (n=1,412,119). We excluded individuals admitted for their first hip fracture after June 30, 2007 to allow for a six-month observation period (n=68,580);, refer to Fig. 1 for cohort inclusion criteria.
Fig. 1.
Hospice Cohort Inclusion and Exclusion Criteria
DRG= Diagnosis Resource Groups.
Incident hip fractures were identified using the primary International Classification of Diseases, 9th revision (ICD-9) diagnosis codes on the hospital admission (see Appendix). A five-year look-back period was used to exclude any beneficiaries with prior hip fracture. Suspect claims occurring after the date of death (n=5,798), hospitalization outside the U.S. (n= 299), and those with surgery codes indicating a revision of a previous hip fracture, bilateral hip surgery, or multiple trauma (n= 20,011) also were excluded.
Among those identified as having their first hip fracture, enrollment in hospice at the time of the fracture was identified. Hospice use was defined as any submitted claim for hospice in the 30 days prior to the hip fracture hospitalization. Individuals not receiving hospice in the 30 days prior to the hip fracture hospitalization were excluded (n=1,303,031). The final cohort consisted of 14,400 individuals receiving hospice who were hospitalized for their first hip fracture between January 1, 1999–June 30, 2007. If a second fracture occurred during the observation period, it was not included in the analysis.
Main Explanatory Variable
Surgical or non-operative treatment was determined based on ICD-9 procedure codes and/or a diagnosis related group (DRG) that indicated surgery (see Appendix). To ensure that the cohort was not biased by excluding those individuals who were not medically stable to have surgery during the initial hospital stay or those individuals who were transferred to another hospital for surgery, individuals having a hip fracture procedure within thirty days also were included in the surgical cohort.7 Medicare beneficiaries hospitalized with an ICD-9 diagnosis code for hip fracture (820.XX) and having either an ICD-9 procedure code or DRG code consistent with a hip fracture repair within 30 days of index hip fracture hospitalization were defined as the hip fracture surgical cohort.
Although pathologic fracture should not be coded with the 820.XX ICD-9 diagnosis code, the final cohort was reviewed to determine if any of the index event hip fractures were diagnosed as pathological fractures (ICD-9 diagnosis code 733.10); none were found.
Outcome Variables
Survival from hip fracture hospital admission (in days) to death was the outcome of interest. For those individuals alive at six months and those dying within the first six months, the type of service being used at six months or the time of death was identified: nursing home, skilled nursing facility, inpatient rehabilitation facility, home with home care, home with self-care, home on hospice, nursing home with hospice, death during initial hip fracture hospitalization, hospitalization (i.e., acute care hospital stay, emergency room visit, or observation), or other site of care (psychiatric hospital, long-term care hospital, outpatient services).
Covariates
Sociodemographic characteristics used to describe the hospice cohort included: age, race (White, Black, and Hispanic), and gender. In order to describe what type of hospice services were being used at the time of the fracture, indicators of the location where hospice services were being received was included (nursing home or community). Hospital admission records were used to identify the type of hip fracture (femoral neck fracture, petrochanteric fracture), the occurrence of an intensive care unit (ICU) stay, length of hospitalization (days), comorbid diagnoses (cancer, cardiovascular disease, dementia, degenerative disease of the central nervous system, chronic obstructive pulmonary disease (COPD), acute myocardial infarction, and renal disease), year of the hip fracture, and the Elixhauser comorbidity measure.8
Statistical Analysis
The means and distributions of patient characteristics and time trends are presented in Table 1. Using STATA 10.0 (StataCorp, LP, College Station, TX), six-month survival was calculated using Kaplan-Meier survival curves. A Cox proportional hazard model was estimated to test the effect of surgery on survival, adjusting for covariates and clustering within hospitals using the Huber-White correction.
Table 1.
Characteristics of Hospice Patients Experiencing a Hip Fracture
| Hospice Cohort (n=14,400) | |||
|---|---|---|---|
| Cohort (n=14,400) |
Surgery (n=12,018) |
No Surgery (n=2,382) |
|
| Age, mean(SD) | 85.6(6.1) | 85.5(6.1) | 85.8(6.2) |
| Female (%) | 72.5 | 72.7 | 71.5 |
| Race (%) | |||
| White | 95.0 | 95.1 | 94.5 |
| Black | 3.1 | 3.0 | 3.6 |
| Hispanic | 0.7 | 0.7 | 0.7 |
| Other race | 1.3 | 1.3 | 1.2 |
| Location of Hospice prior fracture (%) | |||
| Hospice at home | 93.8 | 94.3 | 91.6 |
| Hospice in a nursing home | 6.2 | 5.7 | 8.4 |
| Hip fracture type (%) | |||
| Petrochanteric Fracture | 51.6 | 52.3 | 47.7 |
| Femoral neck Fracture | 48.4 | 47.7 | 52.3 |
| Intensive Care Unit stay | 17.0 | 19.0 | 7.4 |
| Comorbidities (%) | |||
| Cancer | 24.6 | 23.9 | 28.2 |
| Cardiovascular disease | 4.8 | 4.8 | 4.3 |
| Dementia | 4.6 | 4.5 | 4.9 |
| Degeneration of central nervous system | 23.3 | 24.2 | 18.8 |
| Chronic obstructive pulmonary disease | 31.5 | 31.2 | 33.1 |
| Acute myocardial infarction | 1.3 | 1.3 | 1.6 |
| Elixhauser comorbidity measure, mean(SD) | 2.8(1.4) | 2.8(1.4) | 2.7(1.4) |
| Hospital length of stay, mean(SD) | 5.6(3.4) | 6.0(3.3) | 3.4(3.1) |
| Hospital deaths, (%) | 8.8 | 6.2 | 21.8 |
| Year of the hip fracture, (%) | |||
| 1999 | n=765 | 82.5 | 17.5 |
| 2000 | n=960 | 84.3 | 15.7 |
| 2001 | n=1,176 | 82.5 | 17.5 |
| 2002 | n=1,416 | 81.6 | 18.4 |
| 2003 | n=1,711 | 82.7 | 17.3 |
| 2004 | n=2,066 | 84.1 | 15.9 |
| 2005 | n=2,376 | 83.8 | 16.2 |
| 2006 | n=2,552 | 84.7 | 15.3 |
| 2007 | n=1,378 | 83.4 | 16.6 |
Note: Hip fractures prior July 1, 2007.
SD= standard deviation.
Results
Cohort Description
Between 1999 and June 30, 2007, 1,317,431 persons were admitted to the hospital with their first hip fracture; one percent (n=14,400) of first time hip fracture hospitalizations were patients receiving hospice services in the 30 days prior to that admission. Table 1 presents the unadjusted proportions, means, and standard deviations of the hospice cohort, stratified by treatment. The majority of individuals were female (72.4%), White (95.6%), and receiving hospice services in the community (93.8%) at the time of the fracture.
Surgical Treatment Rates
Within this hospice cohort, 83.5% underwent surgery (n= 12,018). Individuals not undergoing surgery were slightly older and had a higher proportion of admissions from a nursing home on hospice (8.4% vs. 5.7%). Having an ICU stay (19.0% vs. 7.4%) was more common among the surgery cohort. Over this eight-year period, the proportion of individuals on hospice undergoing surgical intervention for a hip fracture remained stable at around 84%.
Survival
Among those patients undergoing surgery, 6.2% died in the hospital. Of those who died in the hospital and underwent surgical intervention, 7.2% died on the day of surgery (n=736) and the unadjusted mean survival was 5.1 days from surgery to death.
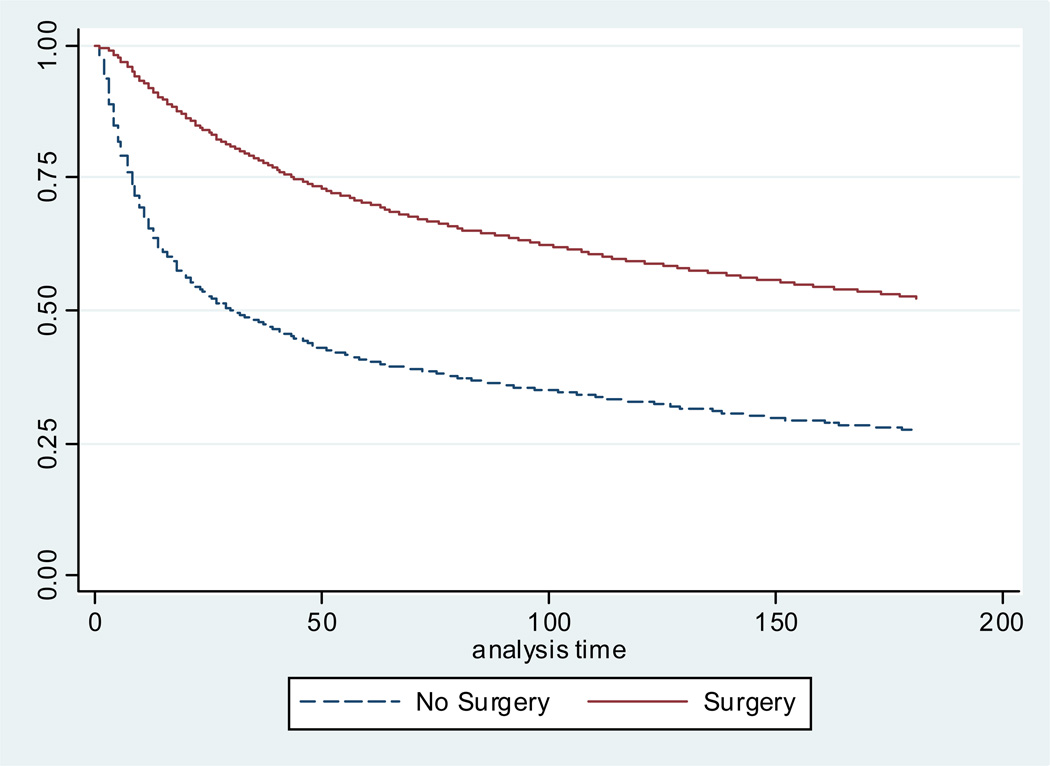
Figure 2 presents the Kaplan-Meir survival curve examining six-month survival for hospice patients who underwent surgery and those who did not have surgery. The adjusted median survival was 117 days for those undergoing surgery compared with 25.9 days for the non-surgical group (Fig. 2). Table 2 presents the Cox proportional hazard model for six-month survival. Survival was better for those undergoing surgical intervention for the hip fracture (hazard ratio [HR] 0.36, 95% confidence interval [CI] 0.34–0.38) compared with those on hospice who did not undergo surgical intervention for their first hip fracture.
Figure 2.
Adjusted Six-Month Mortality
Note: Kaplan-Meier survival curve is adjusted for: age, sex, race, location of hospice prior, ICU stay, length of hospitalization, Elixhauser comorbidity measure, fracture type, cancer, chronic obstructive pulmonary disease, dementia, cardiovascular disease, disease of the central nervous system, acute myocardial infarction, year of the fracture.
Table 2.
Cox Proportional Hazard Model: Six-Month Mortality
| Hazard Ratio | 95% CI | ||
|---|---|---|---|
| No Surgical intervention for hip fracture | (Reference) | ||
| Had surgery for hip fracture | 0.36 | 0.34 | 0.38 |
| Age at the time of the fracture | |||
| Age 75–80 | (Reference) | ||
| Age 81–85 | 1.09 | 1.03 | 1.15 |
| Age 86–89 | 1.11 | 1.04 | 1.18 |
| Age 90+ | 1.21 | 1.14 | 1.29 |
| Female | 0.71 | 0.68 | 0.74 |
| Race | |||
| White | (Reference) | ||
| Black | 0.73 | 0.66 | 0.82 |
| Hispanic | 0.94 | 0.72 | 1.22 |
| Other race | 0.88 | 0.71 | 1.10 |
| Hospice in the community prior to fracture | (Reference) | ||
| Hospice in a nursing home prior to fracture | 0.97 | 0.88 | 1.07 |
| Petrotrochanteric fracture | 1.03 | 0.99 | 1.08 |
| Elixhauser co-morbidity measure | 1.04 | 1.02 | 1.06 |
Note: Adjusting for ICU stay, hospital length of stay, and comorbid diagnoses analysis was clustered at the hospital.
Type of Service Use at the End of Life
Six-month survival was poor for both groups; of those not having surgery, 12.3% were alive at six months compared with 37.2% of those who underwent surgery. Twenty-five percent of the non-surgical hospice cohort that died in the first six months died during the initial hip fracture hospitalization and 62.7% died on hospice. Among those having surgery who died in the first six months, 62.0% died on hospice and 15.9% died while in a skilled nursing facility without hospice (Table 3).
Table 3.
Six-Month Outcomes for Hospice Beneficiaries with a Non-Pathological Hip Fracture
| Hospice Cohort (n=14,400) | |||
|---|---|---|---|
| Cohort (n=14,400) |
Surgery (n=12,018) |
No Surgery (n=2,382) |
|
| Alive at 6 months (n=4,759) | 33.1 | 37.2 | 12.3 |
| Type of service received at 6 months (%) | |||
| Home on hospice | 38.8 | 38.9 | 37.4 |
| Hospice in a nursing home | 24.8 | 24.3 | 32.7 |
| Skilled nursing facility | 2.6 | 2.6 | 2.0 |
| Nursing home | 16.9 | 17.1 | 14.3 |
| Inpatient rehabilitation facility | 0.02 | 0.02 | 0 |
| Home to self care | 12.4 | 12.5 | 10.9 |
| Home health | 3.5 | 3.6 | 2.0 |
| Hospital | 0.6 | 0.6 | 0 |
| Other | 0.4 | 0.4 | 0.7 |
| Deceased by 6 Months (n=9,641) | 66.9 | 62.8 | 87.7 |
| Place of Death in first 6 months (%) | |||
| Death during index event | 13.0 | 9.8 | 24.8 |
| Home on hospice | 40.0 | 39.9 | 40.4 |
| Hospice in a nursing home | 22.0 | 22.1 | 22.3 |
| Skilled nursing facility | 14.0 | 15.9 | 6.9 |
| Nursing home | 3.0 | 2.9 | 1.6 |
| Inpatient rehabilitation facility | 0.001 | 0.2 | 0.0 |
| Home to self care | 0.03 | 3.0 | 2.1 |
| Home health | 0.003 | 0.4 | 0.1 |
| Hospital | 0.04 | 5.3 | 1.7 |
| Other | 0.01 | 0.6 | 0.2 |
Note: Numbers may not add to 100% because of rounding.
Hospital= acute care hospital admission, emergency room visit, or hospital observation; Other= psychiatric hospital, long-term care hospital, outpatient services.
Discussion
Approximately one percent of all hip fracture admissions were on hospice services at the time of hip fracture, with a similar proportion of individuals undergoing surgery (ranging from 81.6 to 84.7%) over the eight-year period. The majority of hospice patients with a hip fracture referred to an acute care hospital did undergo surgery, with improved median survival, but still experienced poor six-month survival, with two-thirds of the cohort dead in the first 180 days. Among those hospice patients undergoing surgery who died in the first six months, 38% were not receiving hospice services at the time of death.
To our knowledge, there is only one small study that has looked at survival among hospice patients experiencing a hip fracture in the U.S..1 This small study (n=15) found no differences in survival based on surgical versus non-surgical intervention (17 vs. 20 days) of elderly hospice patients. Using a large national cohort of Medicare patients on hospice, the study presented here demonstrates that there is a difference in survival for those undergoing surgical hip fracture repair among patients with terminal illness.
It should be emphasized that survival is only one factor to consider in the decision to have or not have surgery. Consideration must be given for recovery time after surgery, time spent in rehabilitation, and the patients’ quality of life. Previous studies examining functional recovery after a hip fracture among community-living older adults found that significant functional disability persists after one year.12–14 Alternatively, little is known about the quality of life of those receiving hospice at the time of hip fracture and their trajectory after a hip fracture. There is no evidence documenting rehabilitation utilization, functional outcomes, or measures of quality of life among individuals receiving hospice prior to their hip fracture and who undergo surgical repair. Further work is needed in these areas in order to better understand the impact of surgery on the quality of life for these individuals acutely injured while on hospice.
Limitations
There are limitations that need to be considered in the interpretation of these findings. Our cohort was limited to those individuals on hospice presenting to the hospital after a hip fracture; those individuals on hospice electing not to go to the hospital after a hip fracture are not included in the cohort. Secondly, this study used claims data that may not fully capture the severity of illness, which could lead to residual confounding. Third, this analysis is descriptive and does not adjust for the selection bias regarding which patients were healthy enough to undergo surgery. Fourth, the use of claims data does not provide insight into the beliefs and desires for care held by the patient and family after the hip fracture event. It also should be acknowledged that our cohort was limited to those 75 years of age or older. Therefore, not including those younger Medicare beneficiaries on hospice with a hip fracture may have biased our survival results.
Conclusion
The majority of patients on hospice presenting to the hospital with a hip fracture undergo surgical treatment. Hip fracture surgical trends among individuals on hospice have remained fairly stable over time. The surgical patients survive longer but most die by six months; many died without returning to hospice. The decision whether or not to operate on a patient receiving hospice presenting to the hospital with a hip fracture must weigh better survival and quality of life.
Acknowledgments
This research was made possible in part by the Shaping Long-Term Care in America Project funded by the National Institute on Aging (1P01AG027296). Dr. Natalie Leland was being funded through the Agency for Healthcare Research and Quality (AHRQ) National Research Services Awards (NRSA) Post- Doctoral Fellowship Training Grant (5T32HS000011-24) during this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors have no conflicts of interest. Drs. Leland, Teno Gozalo, and Mor are affiliated with the Warren Alpert Medical School of Medicine at Brown University and Dr. Bynum is affiliated with the Dartmouth Medical School and the Dartmouth Institute for Health Policy and Clinical Practice. None of these relationships pose a conflict of interest or potential conflict of interest.
References
- 1.Fortier D, Gruzman T. Management of hip fractures in the terminally ill. J Am Geriatr Soc. 2003;51:1046–1047. doi: 10.1046/j.1365-2389.2003.51329.x. [DOI] [PubMed] [Google Scholar]
- 2.Hossain M, Neelapala V, Andrew JG. Results of non-operative treatment following hip fracture compared to surgical intervention. Injury Int J Care Injured. 2009;40:418–421. doi: 10.1016/j.injury.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Goldacre MJ, Roberts SE, Yeates D. Mortality after admission to hospital with fractured neck of femur: database study. BMJ. 2002;325:868–869. doi: 10.1136/bmj.325.7369.868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magaziner J, Simonsick EM, Kashner TM, et al. Survival experience of aged hip fracture patients. Am J Public Health. 1989;79:274–278. doi: 10.2105/ajph.79.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractures neck of femur in an English population, 1968–98: database study. BMJ. 2003;327:771–775. doi: 10.1136/bmj.327.7418.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McNamara P, Sharma K. Surgery or palliation for hip fractures in patients with advanced malignancy. Age Aging. 1997;26:471–474. doi: 10.1093/ageing/26.6.471. [DOI] [PubMed] [Google Scholar]
- 7.Neuman MD, Fleisher LA, Even-Shoshan O, Silber JH. Non-operative care for hip fracture in the elderly: the influence of race, income, and comorbidities. Med Care. 2010;48:314–320. doi: 10.1097/mlr.0b013e3181ca4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ooi LH, Wang TH, Toh CL, Wong HP. Hip fractures in nonagenarians—a study on operative and non-operative management. Injury Int J Care Injured. 2005;36:142–147. doi: 10.1016/j.injury.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 9.Lu-Yao GL, Baron JA, Barrett JA, Fisher ES. Treatment and survival among elderly Americans with hip fractures: a population based study. Am J Public Health. 1994;84:1287–1291. doi: 10.2105/ajph.84.8.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Intrator O, Hiris J, Berg K, Miller S, Mor V. The residential history file: studying nursing home residents long-term care histories. Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use of administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol Med Sci. 2000;55A:M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 13.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community dwelling aged. Am J Epidemiol. 2003;157:1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 14.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol Med Sci. 1990;45:M101–M107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]