Abstract
Objective
The Zwolle Outpatient Diabetes project Integrating Available Care (ZODIAC) study was initiated in 1998 to investigate the effects of shared care for patients with type 2 diabetes mellitus (T2DM) in the Netherlands, and to reduce the number of diabetes-related complications. Benchmarking the performance of diabetes care was and is an important aspect of this study. We aimed to investigate trends in diabetes care, within the ZODIAC study for a wide variety of quality indicators during a long follow-up period (1998–2008), with special interest for different age groups.
Design
Prospective observational cohort study.
Setting
Primary care, Zwolle, The Netherlands.
Participants
Patients with T2DM.
Methods
A dataset of quality measures was collected annually during the patient's visit to the practice nurse or general practitioner. Linear time trends from 1998 to 2008 were estimated using linear mixed models in which we adjusted for age and gender. Age was included in the model as a categorical variable: for each follow-up year all participants were categorised into the categories <60, 60–75 and >75 years. Differences in trends between the age categories were investigated by adding an interaction term to the model.
Results
The number of patients who were reported to participate increased in the period 1998–2008 from 1622 to 27 438. All quality indicators improved in this study, except for body mass index. The prevalence albuminuria decreased in an 11-year-period from 42% to 21%. No relevant differences between the trends for the three age categories were observed. During all years of follow-up, mean blood pressure and body mass index were the lowest and highest, respectively, in the group of patients <60 years (data not shown).
Conclusions
Quality of diabetes care within the Dutch ZODIAC study, a shared care project, has considerably improved in the period 1998–2008. There were no relevant differences between trends across various age categories.
Article summary.
Article focus
Shared care, defined as care for patients with a chronic condition provided in cooperation between primary and secondary healthcare, has been promoted and developed in order to reduce the number of diabetes-related complications.
There are limited data whether improvements in diabetes care in the past few decades are comparable across different age categories.
We aimed to investigate trends in diabetes care, within a shared care project, during a long follow-up period (1998–2008), with a special focus on different age groups.
Key messages
Quality of diabetes care within the Dutch ZODIAC study, a shared care project, has considerably improved in the period 1998–2008.
Large improvements were observed for all quality indicators studied in this study, except for body mass index.
No relevant differences between the trends for different age categories were observed.
Strengths and limitations of this study
Strengths of our study are the long follow-up period and the high number of participants.
A causal relationship between shared care and the observed improvements cannot be proved due to the observational design of our study.
Introduction
Ever since it was established that type 2 diabetes mellitus (T2DM) leads to significant morbidity and mortality,1 2 prevention and (early) treatment of both microvascular and macrovascular complications of T2DM have become important goals in diabetes care. Efforts to improve the quality of diabetes care are necessary in order to reduce morbidity and mortality associated with T2DM.3 4 Since adequate treatment of patients with T2DM often needs the involvement of more than one caregiver, shared care, defined as care for patients with a chronic condition provided in co-operation between primary and secondary healthcare, has been promoted and developed.5
The Zwolle Outpatient Diabetes project Integrating Available Care (ZODIAC) study was initiated in 1998 to investigate the effects of shared care for patients with T2DM in the Netherlands.6 Benchmarking the performance of diabetes care was and is an important aspect of this initiative. Previous reports from the ZODIAC study showed that structured shared care with task delegation to nurses leads to improvements in quality of diabetes care and life expectancy.6–8 However, effectiveness of shared care in general was not demonstrated in a 2007 Cochrane review.5 Inadequate length of follow-up was mentioned by the authors as a possible explanation for the lack of evidence.
Although diabetes care has improved considerably during the past few decades in patients with diabetes, there are limited data regarding whether these improvements are comparable across different age categories.9 10 A cross-sectional study from France showed that quality of care had considerably improved for patients ≥65 years with T2DM in the period 2001–2007.11 Unfortunately, trends for patients >75 years were not described separately in this study. Although the number of patients with T2DM >75 years is increasing, the evidence for cardiovascular risk interventions in this age category is low.12 Data from observational studies show that classic cardiovascular risk factors may even have different consequences in elderly patients.13–17
In the present study, we aimed to investigate trends in diabetes care, within a shared care project, for a wide variety of quality indicators during a long follow-up period (1998–2008). Because of limited evidence for cardiovascular risk interventions in old age, we had specific interest whether the same trends were observed for different age groups (<60, 60–75 and >75 years).
Methods and patients
Study population and ZODIAC
The ZODIAC study started in 1998 as a prospective observational study for patients with T2DM.6 Participating practices were allocated to one of the two intervention groups or to the standard care group. The interventions involved extensive or limited task delegation from general practitioners to practice nurses and/or diabetes specialist nurses. Moreover, it included a diabetes register, structured recall, facilitated generalist–specialist communication, audit and feedback, patient-specific reminders and it emphasised patients’ education.6 The patients participating in the ZODIAC study are known with T2DM and exclusively treated in primary care. Patients who were already treated in secondary care for their diabetes, patients with a very short life expectancy (including patients with active cancer) and patients with insufficient cognitive abilities were excluded from participation. In the first few years of ZODIAC, only patients in the surrounding area of the city of Zwolle participated in the study. Because of the improvements in the quality of diabetes care in the two intervention groups, the shared care project has expanded gradually in the past decade. First, the shared care project became the standard for diabetes care in the entire Zwolle region (2002–2003), and in 2005–2006 the project expanded to the northeast region of the Netherlands. Patients who were received standard care in the beginning of the project, switched to shared care in 2002–2003 when the shared care project became the standard for the entire Zwolle region. These patients were included in the current analyses from the moment they switched to shared care. The number of participating general practitioners (GPs) has increased from 53 in 1998 to 459 in 2008. Patient numbers increased from 1622 to 27 438 in this time frame, and nowadays even more than 60 000 patients are participating. A benchmark of annually gathered quality measures of this cohort, based on the guidelines of the Dutch College of General Practitioners and the Dutch Diabetes Federation, has been developed.18
Data collection
The dataset of quality measures is collected annually during the patient's visit to the practice nurse and/or GP. These quality measures are collected in the GPs’ patient information systems and each year the relevant data are uploaded and sent to our diabetes centre for benchmarking and research purposes. At baseline, additional data were collected including a full medical history. The dataset contains many quality measures, including data on cardiovascular risk control, treatment and complications. Distinction is made between process and outcome measures. Process measures indicate whether tests or assessments have been performed, for example, the number of patients whose HbA1c level has been determined. Outcome measures reflect the results of the assessments, such as the mean systolic blood pressure or the proportion of patients with a systolic blood pressure <140 mm Hg. Table 1 shows an overview of the measures we investigated in this study for each year of follow-up.
Table 1.
Overview of the process and outcome measures studied
| Parameter | Process measure | Outcome measure |
|---|---|---|
| HbA1c | Percentage of patients measured | Mean HbA1c (%) |
| Percentage HbA1c<7% | ||
| Percentage HbA1c≥8.5% | ||
| Glucose-lowering treatment | NA | Percentage diet only |
| Percentage oral medication only | ||
| Percentage insulin with or without oral medication | ||
| Blood pressure | Percentage of patients measured | Mean SBP (mm Hg) |
| Percentage SBP<140 mm Hg | ||
| Antihypertensive treatment | NA | Percentage patients using antihypertensive drugs |
| Cholesterol–HDL ratio | Percentage of patients measured | Mean total cholesterol–HDL ratio |
| Percentage total cholesterol–HDL ratio<4 | ||
| Lipid-lowering drugs | NA | Percentage patients using lipid-lowering drugs |
| Renal function | Percentage of patients with creatinine measurements | Mean creatinine (μmol/l) |
| Percentage of patients with ACR measurements | Percentage microalbuminuria | |
| Percentage macroalbuminuria | ||
| BMI | Percentage of patients measured | Mean BMI (kg/m2) |
| Percentage BMI<25 kg/m2 |
Abbreviations: ACR, albumin–creatinine ratio; BMI, body mass index; HDL, high-density lipoprotein; NA, not applicable; SBP, systolic blood pressure.
Participating practices were instructed to perform blood pressure measurements in supine position after at least 5 min of rest, and to calculate the mean blood pressure of two recording for each visit. Laboratory data (HbA1c, serum creatinine and lipid profile) were determined using standard hospital procedures. Until 2005, all procedures were performed in the clinical chemistry laboratory of the Isala Clinics (Zwolle region). Because of the expansion of the project in 2005–2006 to the northeast region of the Netherlands, laboratories of other regions started participating. HbA1c was measured using affinity chromatography high-performance liquid chromatography (Ultra 2, Trinity Biotech, Kansas City, Missouri, USA) in the Zwolle region (coefficient of variation approximately 1.5%).19 There are differences in the methods used in the various laboratories in the northeast region of the Netherlands. Generally speaking, the variation coefficient has decreased in the study period due to the worldwide standardisation of HbA1c measurements and improved techniques. Because of the high number of patients in the last years of the project, it is not likely that differences in the coefficient of variation coefficient have influenced the results.
Statistical analyses
Continuous variables are represented as means and 95% CI for the normally distributed values. Normality was evaluated using Q–Q plots and histograms. Nominal variables are represented as the proportion of patients together with 95% CIs. The database contained 37 320 unique patients and data of 92 340 unique yearly diabetic check-ups. For 9279 patients, we only had data of one diabetic check-up. The descriptive statistics were strictly cross-sectional and included observations of all visits (n=92 340). Since cross-sectional outcomes are influenced by changes in population (inmigration and outmigration), besides changes in quality of care, cross-sectional outcomes tend to overestimate time trends when compared to longitudinal analyses.20 Therefore, we estimated linear time trends from 1998 to 2008 using a linear mixed model for continuous variables (SAS PROC MIXED) and a generalised linear mixed model for binary variables (PROC GLIMMIX, using the logit link function) in which we adjusted for age and gender. In all analyses, time, age and sex were modelled as fixed effects. Since the estimated linear time trends are based on individual changes over time, data of at least two visits were necessary. As a consequence, these longitudinal analyses were based on 83 061 visits of 28 041 patients. Age was included in the model as a categorical variable: for each follow-up year all participants were categorised into the categories <60, 60–75 and >75 years. All time trends were visually inspected and a quadratic time trend was only introduced when such a trend was likely based on the plot. Differences in trends between men and women and the age categories were investigated by adding interaction terms for age and time and sex and time to the model. A significant interaction for age and time means that differences exist between the time trends for the three age categories. The same applies for the interaction between sex and time. All analyses were performed with SPSS V.18.0.0 software (SPSS Inc, Chicago, Illinois, USA) and with SAS V.9.2 software (SAS Institute Inc, Cary, North Carilina, USA).
The manuscript was written based on the ‘Strengthening the reporting of observational studies in epidemiology’ statement.21
Ethics statement
The ZODIAC study and the informed consent procedure were approved by the local medical ethics committee of the Isala Clinics, Zwolle, the Netherlands. In the first years of ZODIAC, verbal informed consent was obtained from all patients and the consent was documented in the patient's records. According to Dutch law, written informed consent was not necessary for this type of study in 1998. Nowadays, written informed consent is obtained. All data were analysed anonymously.
Results
The number of patients who were reported to participate in this shared care project increased in the period 1998–2008 from 1622 to 27 438. Mean age decreased with time from 68.9 to 67.4 years (p for trend <0.0001). A gradual increase was observed for the proportion of male patients participating in the project. Median diabetes duration remained rather constant at 5 years throughout the study period. The proportion of patients aged older than 75 years was 31% in 1998 and declined to 26.3% in 2008. The number of patients who did not participate in the study due to short life expectancy of insufficient cognitive abilities is unknown after 1999. The results for all process and outcome measures of each year for the overall study group are presented in table 2.
Table 2.
Characteristics of all participants in the Zwolle Outpatient Diabetes project Integrating Available Care study for the period 1998–2008
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n=1622 | n=1767 | n=1462 | n=1615 | n=1761 | n=4029 | n=4729 | n=4508 | n=18469 | n=24940 | n=27438 | p value for trend* | |
| Age | 68.9 (68.4 to 69.5) | 68.9 (68.3 to 69.4) | 67.8 (67.2 to 68.4) | 67.8 (67.2 to 68.3) | 67 (66.5 to 67.6) | 67.6 (67.2 to 67.9) | 67.5 (67.2 to 67.9) | 67.5 (67.2 to 67.8) | 67.4 (67.2 to 67.6) | 67 (66.9 to 67.2) | 67.4 (67.2 to 67.5) | <0.0001 |
| Sex (female) | 58 (55.6 to 60.4) | 58.2 (55.9 to 60.5) | 56.2 (53.7 to 58.8) | 56.9 (54.5 to 59.3) | 55.4 (53.1 to 57.7) | 54.7 (53.2 to 56.2) | 53.8 (52.4 to 55.2) | 53.5 (52.1 to 55.0) | 52.6 (51.9 to 53.3) | 52.6 (51.9 to 53.2) | 51.9 (51.3 to 52.5) | <0.0001 |
| DM duration | 5.2 (2.5 to 9.8) | 5.7 (3 to 10.5) | 5.6 (2.8 to 10.4) | 5 (2.1 to 9.9) | 4.5 (2.1 to 9) | 4.5 (2.3 to 8.5) | 4.9 (2.3 to 8.5) | 5 (2.6 to 8.7) | 4.7 (2.4 to 8.1) | 4.8 (2.4 to 8.1) | 5.3 (2.9 to 8.8) | <0.0001 |
| HbA1c | ||||||||||||
| Process | 88.6 (87 to 90.1) | 86.4 (84.8 to 88) | 97.4 (96.6 to 98.2) | 91.1 (89.7 to 92.5) | 91.6 (90.3 to 92.9) | 83.6 (82.5 to 84.8) | 85.9 (84.9 to 86.8) | 96.1 (95.5 to 96.6) | 87.8 (87.3 to 88.3) | 85.8 (85.4 to 86.2) | 95.5 (95.3 to 95.8) | <0.0001 |
| Mean | 7.5 (7.4 to 7.5) | 7.5 (7.4 to 7.5) | 7.3 (7.2 to 7.3) | 7 (7 to 7.1) | 7.1 (7 to 7.1) | 7 (6.9 to 7) | 7 (7 to 7) | 6.8 (6.8 to 6.9) | 6.7 (6.7 to 6.8) | 6.7 (6.7 to 6.7) | 6.7 (6.7 to 6.7) | <0.0001 |
| % <7 | 40.4 (37.9 to 43.0) | 40.6 (38.1 to 43.1) | 46.6 (44 to 49.2) | 56.7 (54.2 to 59.2) | 53.3 (50.9 to 55.8) | 57.2 (55.5 to 58.8) | 57 (55.5 to 58.5) | 61.9 (60.5 to 63.4) | 67.5 (66.8 to 68.2) | 69.8 (69.2 to 70.5) | 70.1 (69.6 to 70.7) | <0.0001 |
| % ≥8.5 | 13.2 (11.5 to 15) | 12.9 (11.2 to 14.6) | 9.7 (8.2 to 11.2) | 7.8 (6.5 to 9.2) | 7.4 (6.2 to 8.7) | 5.7 (4.9 to 6.5) | 5.6 (4.9 to 6.3) | 3.4 (2.8 to 3.9) | 3 (2.8 to 3.3) | 2.6 (2.4 to 2.8) | 2.3 (2.1 to 2.5) | <0.0001 |
| DM treatment | ||||||||||||
| Diet only | 16.6 (14.9 to 18.5) | 18.5 (16.8 to 20.4) | 18.5 (16.6 to 20.6) | 18.2 (16.4 to 20.2) | 23.1 (21.2 to 25.1) | 21.9 (20.7 to 23.2) | 21.3 (20.1 to 22.5) | 20.1 (18.9 to 21.3) | 24.1 (23.5 to 24.7) | 24.9 (24.3 to 25.4) | 23.8 (23.3 to 24.3) | <0.0001 |
| Percentage of OBLD only | 67.9 (65.6 to 70.2) | 65.9 (63.6 to 68) | 65.7 (63.3 to 68.1) | 65 (62.6 to 67.2) | 61.5 (59.2 to 63.8) | 64.5 (63 to 66) | 62.1 (60.7 to 63.5) | 63.0 (61.6 to 64.4) | 63.8 (63.1 to 64.4) | 62.8 (62.2 to 63.4) | 63.4 (62.9 to 64) | <0.0001 |
| Percentage of Insulin | 15.5 (13.8 to 17.3) | 15.6 (14 to 17.4) | 15.7 (14 to 17.7) | 16.8 (15.1 to 18.7) | 15.4 (13.8 to 17.2) | 13.6 (12.5 to 14.6) | 16.6 (15.6 to 17.7) | 16.9 (15.9 to 18.1) | 12.2 (11.7 to 12.6) | 12.3 (11.9 to 12.7) | 12.8 (12.4 to 13.2) | <0.0001 |
| SBP | ||||||||||||
| Process | 88.7 (87.2 to 90.3) | 88.5 (87 to 90) | 97.3 (96.4 to 98.1) | 97 (96.1 to 97.8) | 96.4 (95.5 to 97.2) | 77.2 (75.9 to 78.5) | 92.8 (92.1 to 93.5) | 95.7 (95.1 to 96.3) | 93.4 (93 to 93.8) | 96.7 (96.5 to 96.9) | 98.5 (98.4 to 98.7) | <0.0001 |
| Mean | 154.5 (153.3 to 155.8) | 150.3 (149.1 to 151.4) | 149.4 (148.2 to 150.6) | 145.9 (144.9 to 146.9) | 144.4 (143.4 to 145.4) | 146.7 (146.0 to 147.4) | 145.9 (145.3 to 146.5) | 144.6 (144 to 145.2) | 141.9 (141.7 to 142.2) | 141.2 (140.9 to 141.4) | 140 (139.8 to 140.2) | <0.0001 |
| Percentage <140 | 22 (19.9–24.2) | 26.4 (24.2 to 28.6) | 29.4 (27 to 31.8) | 33 (30.7 to 35.3) | 34.6 (32.4 to 36.9) | 33.2 (31.5 to 34.8) | 37.9 (36.4 to 39.3) | 40.8 (39.3 to 42.2) | 43 (42.2 to 43.7) | 44.6 (43.9 to 45.2) | 47.7 (47.1 to 48.3) | 0.0003 |
| SBP treatment | ||||||||||||
| Percentage of drugs | 41.1 (38.8 to 43.5) | 49.6 (47.3 to 52) | 55 (52.4 to 57.5) | 61.1 (58.7 to 63.5) | 65.7 (63.4 to 67.9) | 46.7 (45.1 to 48.2) | 69.7 (68.4 to 71.0) | 72.7 (71.4 to 74) | 73.5 (72.8 to 74.1) | 73.7 (73.2 to 74.3) | 74.6 (74.1 to 75.1) | <0.0001 |
| Cholesterol–HDL ratio | ||||||||||||
| Process | 73.3 (71.2 to 75.5) | 74.9 (72.9 to 77) | 96.4 (95.4 to 97.3) | 91.9 (90.6 to 93.2) | 92.3 (91 to 93.5) | 77.2 (75.9 to 78.5) | 79.5 (78.4 to 80.7) | 87.8 (86.9 to 88.8) | 83.1 (82.6 to 83.7) | 84.2 (83.7 to 84.6) | 94.2 (94 to 94.5) | <0.0001 |
| Mean | 5.2 (5.1 to 5.3) | 4.8 (4.7 to 4.9) | 4.5 (4.5 to 4.6) | 4.4 (4.3 to 4.5) | 4.1 (4 to 4.1) | 4 (3.9 to 4) | 3.8 (3.8 to 3.9) | 3.8 (3.7 to 3.8) | 3.6 (3.6 to 3.7) | 3.7 (3.7 to 3.7) | 3.8 (3.8 to 3.8) | <0.0001 |
| Percentage <4 | 23 (20.7 to 25.4) | 30.7 (28.2 to 33.1) | 35.6 (33.1 to 38.1) | 42.3 (39.8 to 44.8) | 49.8 (47.4 to 52.3) | 55 (53.2 to 56.7) | 59.2 (57.7 to 60.8) | 61.7 (60.2 to 63.2) | 67.1 (66.3 to 67.8) | 64.5 (63.8 to 65.1) | 61.1 (60.5 to 61.7) | <0.0001 |
| LLD | ||||||||||||
| % drugs | 10.2 (8.9 to 11.8) | 13.5 (12 to 15.2) | 20.8 (18.8 to 23) | 26.2 (24.1 to 28.4) | 29.9 (27.8 to 32.1) | 21.7 (20.4 to 23) | 35.8 (34.5 to 37.2) | 40.1 (38.7 to 41.5) | 54.3 (53.6 to 55.1) | 59.7 (59.1 to 60.4) | 62.8 (62.2 to 63.3) | <0.0001 |
| Creatinine | ||||||||||||
| Process | 89.1 (87.6 to 90.7) | 87.3 (85.8 to 88.9) | 97.5 (96.7 to 98.3) | 91.9 (90.6 to 93.2) | 91.8 (90.5 to 93.1) | 84.7 (83.6 to 85.8) | 85.7 (84.7 to 86.7) | 93.1 (92.4 to 93.9) | 87.8 (87.3 to 88.3) | 85.5 (85.1 to 86) | 95.4 (95.1 to 95.6) | <0.0001 |
| Mean | 96.5 (51.7 to 141.2) | 95 (48.9 to 141.1) | 93.8 (50.2 to 137.4) | 96.8 (52.9 to 140.7) | 98.2 (54.4 to 142) | 95.4 (52.9 to 137.8) | 96.5 (53.9 to 139.1) | 97.7 (55.6 to 139.7) | 92.9 (47 to 138.7) | 98.9 (52.9 to 144.8) | 98.7 (51.9 to 145.5) | <0.0001 |
| ACR | ||||||||||||
| Process | 65.8 (63.5 to 68.2) | 68 (65.9 to 70.2) | 93.5 (92.2 to 94.8) | 85.4 (83.7 to 87.1) | 84.8 (83.2 to 86.5) | 57.4 (55.9 to 58.9) | 62 (60.6 to 63.4) | 69.9 (68.5 to 71.2) | 59 (58.3 to 59.7) | 66.8 (66.2 to 67.4) | 82.3 (81.9 to 82.8) | <0.0001 |
| Percentage micro | 33.6 (30.8 to 36.4) | 32.6 (30 to 35.3) | 31.4 (28.9 to 33.8) | 29.4 (27 to 31.8) | 25.1 (22.9 to 27.3) | 22.1 (20.4 to 23.8) | 24.4 (22.9 to 26) | 23.2 (21.8 to 24.7) | 19.2 (18.5 to 20) | 19.8 (19.2 to 20.4) | 18.5 (18 to 19) | <0.0001 |
| Percentage macro | 8.3 (6.7 to 10) | 7.7 (6.2 to 9.2) | 6.7 (5.3 to 8) | 4.7 (3.6 to 5.8) | 4.8 (3.7 to 5.9) | 3.7 (2.9 to 4.4) | 3.9 (3.2 to 4.6) | 4.2 (3.5 to 4.9) | 2.9 (2.6 to 3.2) | 2.5 (2.2 to 2.7) | 2.4 (2.2 to 2.6) | <0.0001 |
| BMI | ||||||||||||
| Process | 69 (66.7 to 71.2) | 69.5 (67.3 to 71.6) | 96.9 (96 to 97.7) | 96.7 (95.8 to 97.5) | 95.7 (94.8 to 96.7) | 62.3 (60.8 to 63.8) | 83 (82 to 84.1) | 88.4 (87.5 to 89.4) | 78.1 (77.5 to 78.7) | 88.1 (87.7 to 88.5) | 93.1 (92.8 to 93.4) | <0.0001 |
| Mean | 29 (28.7 to 29.2) | 28.9 (28.6 to 29.1) | 29.3 (29 to 29.5) | 29.4 (29.2 to 29.7) | 29.5 (29.3 to 29.7) | 29.6 (29.4 to 29.7) | 29.6 (29.5 to 29.8) | 29.5 (29.4 to 29.7) | 29.5 (29.5 to 29.6) | 29.5 (29.5 to 29.6) | 29.5 (29.5 to 29.6) | 0.1399 |
| Percentage <25 | 20.4 (18 to 22.7) | 20.4 (18.1 to 22.6) | 17.4 (15.5 to 19.4) | 16.7 (14.8 to 18.5) | 15.8 (14 to 17.5) | 16.2 (14.8 to 17.7) | 16.1 (14.9 to 17.2) | 16.3 (15.1 to 17.4) | 16.8 (16.2 to 17.4) | 17.1 (16.6 to 17.6) | 17.1 (16.6 to 17.6) | 0.6638 |
All data are mean values or proportions together with their 95% CIs, or median values together with the interquartile range.
*p For trend is based on age- and gender-adjusted analyses.
ACR, albumin–creatinine ratio; BMI, body mass index; DM, diabetes mellitus;HDL, high-density lipoprotein; LLD, lipid-lowering drugs; OBLD, oral blood glucose-lowering drugs; SBP, systolic blood pressure.
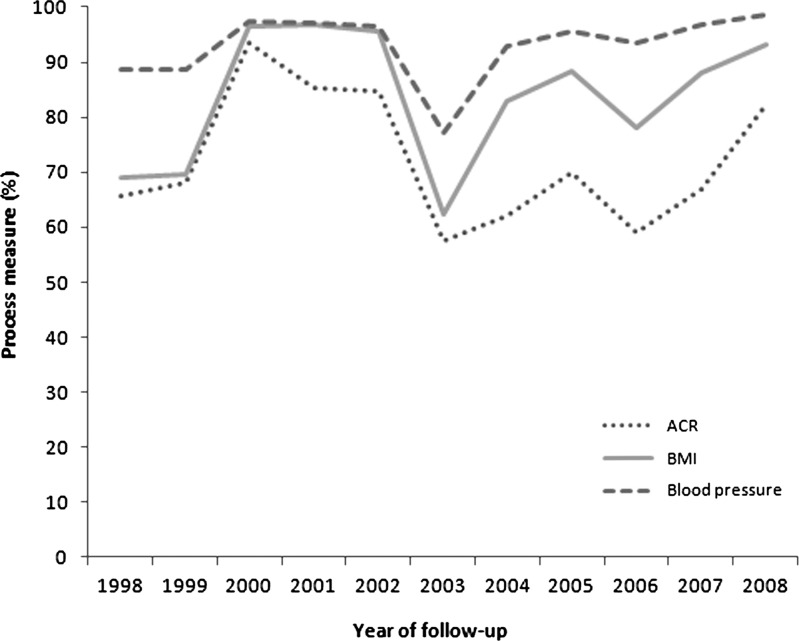
Process measures
All process measures show a similar trend (table 2): a gradual increase in the first years of the project followed by a decrease in the years 2002 and 2003, an increase in the upcoming 2 years, followed by a decrease in 2006 again and a rising trend in the process measures in the last 2 years. Body mass index (BMI), the lipid profile and the albumin–-creatinine ratio (ACR) were less often measured in patients aged >75 years compared to the younger patients (p for interaction with age for all variables <0.0001). Figure 1 illustrates the trends for the process measure of ACR, BMI and blood pressure in the total study population.
Figure 1.
Process measures for albumin-creatinine ratio (ACR), body mass index (BMI) and blood pressure.
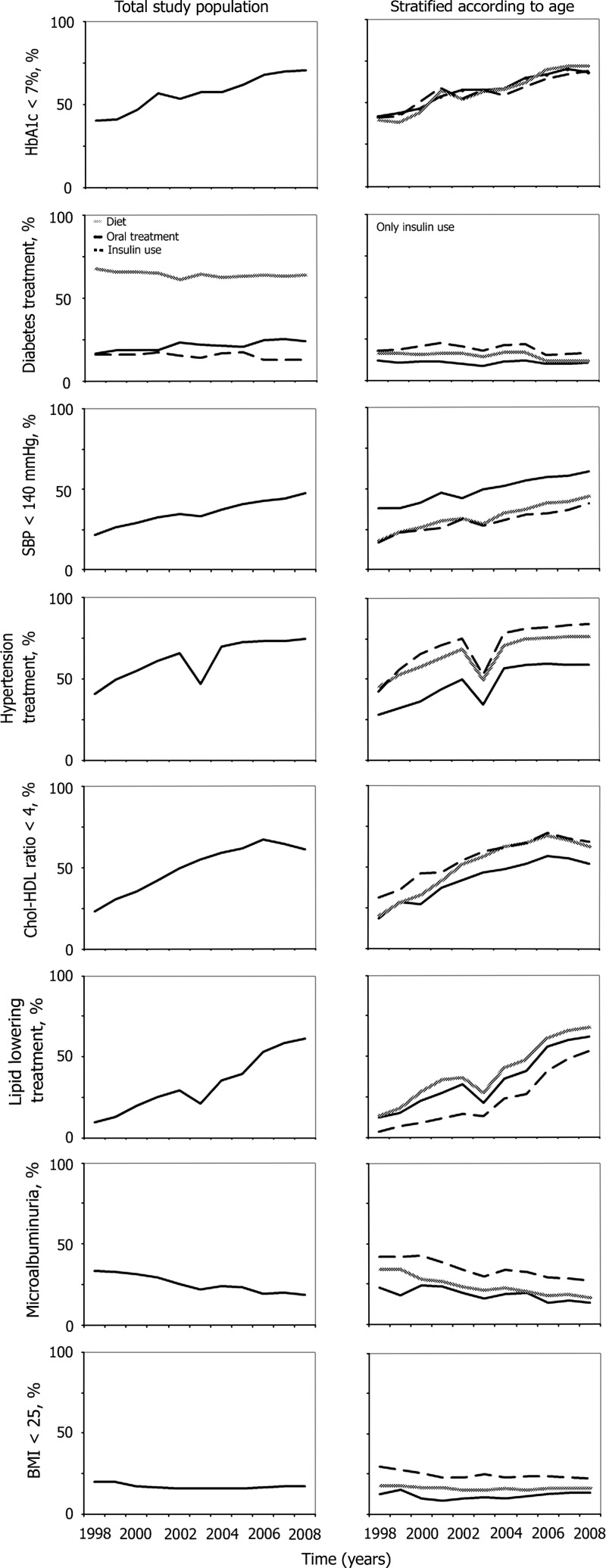
Outcome measures
Figure 2 presents the trends for outcome measures over time for the overall study group and also stratified according to the three age categories.
Figure 2.
Outcome measures for the total study population and stratified according to age (<60 (black line), 60–75 (grey line) and >75 (black dashed line) years).
Glycemic control and diabetes treatment
The decline in mean HbA1c over time is reflected in the proportion of patients achieving the target value of <7%; 35.8% in 1998 compared to 67% in 2008. The differences between the three age categories seem to be small, although the proportion of patients with an HbA1c≥8.5% tended to be the highest for patients aged <60 years in all years (p for interaction with age 0.0773). The proportion of patients treated with only a diet increased over time from 16.6% to 23.8%. A total of 15.5% used insulin in 1998 and this proportion declined to 12.8% in 2008.
Blood pressure and treatment
Mean blood pressure has decreased over time in all age groups, with the lowest values in the youngest patient category (p for interaction with age <0.0001). In 1998 about one-fifth (22%) had a systolic blood pressure <140 mm Hg, compared to 47.7% in 2008. The number of patients with antihypertensive medication increased in all age groups. With advancing age, the number of patients using these agents also increased (p for interaction with age <0.0001). A remarkable decrease in 2003 was directly followed by a large increase in 2004.
Lipids and treatment
Mean total cholesterol–high-density lipoprotein (HDL) ratio has decreased in the period 1998–2006, followed by a small increase in the last 2 years (p for quadratic trend <0.0001). Patients aged <60 years performed worse with regard to the mean cholesterol-HDL ratio compared to the older patients categories (p for interaction with age <0.0001). Approximately one-quarter (23%) of the patients participating in 1998 had a ratio <4. This proportion increased to 61.1% in 2008, which is also reflected in the number of patients receiving lipid-lowering drugs: 10.2% in 1998 and 62.8% in 2008. As was the case with the number of patients using antihypertensives, a remarkable decrease was also observed for the number of patients using lipid-lowering drugs in 2003.
Renal function
Mean values of serum creatinine have remained rather constant throughout the study period. The prevalence of microalbuminuria and macroalbuminuria in 1998 was 33.6% and 8.3%, respectively. These proportions declined over time to 18.5% and 2.4%, respectively. The highest prevalence of microalbuminuria was observed for the group >75 years (p for interaction with age <0.0001).
Body mass index
After an increase in the first 5 years, mean BMI remained rather constant afterwards. In the highest age category, the highest proportion of patients with a BMI<25 kg/m2 was observed and vice versa (p for interaction with age <0.0001).
Discussion
Quality of diabetes care within the Dutch ZODIAC study, a shared care project, has considerably improved in the period 1998–2008. Large improvements were observed for all quality indicators studied in this study, except for BMI. Each time that large groups of general practices joined the shared care initiative (2002 and 2006), there was a short relapse in the process measures, which was mostly redressed within 1 year. No relevant differences between the trends for the three age categories were observed. During all years of follow-up, mean blood pressure and BMI were the lowest and highest, respectively, in the group of patients <60 years. Patients in this age category also had the highest cholesterol–HDL ratio values and the lowest albumin–ACR values throughout the study period.
Striking changes were the increase in the use of blood pressure and lipid-lowering drugs. This increased use was also reflected in the improvements in blood pressure and lipid levels. Remarkably, the decrease in HbA1c was not accompanied by an increase in the proportional use of oral blood glucose-lowering drugs or insulin. Instead, an increase in the proportion of patients on a diet was observed for all age categories. One could hypothesise that more patients with early diagnosed T2DM were included in the last few years of the study. However, median diabetes duration did not relevantly change throughout the study. Patient education and better adherence to lifestyle advices could be other possible explanations.
The results of our study confirm previous reports that also observed improvements in risk factor control during the past few decades.9–11 22 However, this is the first study presenting the results of a large shared care project with a follow-up period of more than 10 years. Although this study demonstrates the impressive results that have been achieved in a shared care setting, it should be emphasised that causality cannot be proved by our study. The two decreases in the process measures, which were observed after the expansion of the ZODIAC project in 2002 and 2006, and the quick rebound afterwards, suggest positive effects of participating in the project (figure 1). However, there are many other factors that may also explain the improvements in quality of care. First, national and international guidelines advocating stricter treatment in patients with T2DM have been published in the period 1998–2008. For example, in 1999 and in 2006 revisions of the guideline T2DM of the Royal Dutch College of General Practitioners were published.18 23 It could be that adherence to these guidelines, irrespective of participating in shared care projects, is the most important factor explaining the general tendency to improved diabetes care. Second, financial incentives from health insurance companies for general practitioners that provide care of a high quality have been introduced in the past decade. Although a recent Cochrane review concluded that there is insufficient evidence to support the use of such financial incentives, positive effects on quality of care can also not be excluded.24
To our knowledge, our study is the first study that also specifically investigated the trends in diabetes care for patients aged older than 75 years. This population is of special interest for two reasons. First, more than one-quarter of the type 2 diabetic population in primary care in the Netherlands is >75 years. Second, clinical trials in old age investigating cardiovascular risk interventions, such as hypertension treatment, are either lacking or subject to selection bias.25–27 Since the evidence for strict cardiovascular risk control in old age is low, old age is characterised by a high prevalence of complications and comorbidities, and elderly patients are at increased risk for possible adverse events, less strict treatment targets for elderly patients with T2DM have been advocated in the literature.28–30 Generally speaking, individualising target values is being increasingly advocated in the literature nowadays.30 Take for example, hypertension treatment in old age. Whereas a systolic blood pressure target value of 140 mm Hg should be used for patients >75 years without many comorbidities who are not using insulin, it is unknown as to whether this target value is also appropriate for the overall elderly population.27 In conclusion, although the current study observed the same improvements in the various quality measures across all age categories, it remains uncertain as to whether these improvements will have the same beneficial effects on cardiovascular comorbidity and mortality in the oldest elderly as in younger patients with T2DM.
Our study has several important limitations that need to be addressed. First, it is important to realise that the cross-sectional data presented in table 2 and figure 2 are influenced by changes in population (inmigration and outmigration), besides possible changes in quality of care. Since the estimated linear time trends were based on individual changes over time, it is possible to conclude that there is an improvement over time. However, these improvements are probably smaller than the cross-sectional data suggest, since cross-sectional outcomes on HbA1c overestimate improvements over time when compared with longitudinal outcomes.20 Second, because of its observational design a causal relationship between shared care and the observed improvements cannot be proven. Unfortunately, we were not able to include a control group of patients with diabetes receiving standard care. Third, the data in our study have been provided by practice nurses and GPs as part of the yearly benchmark. As a consequence, the quality and reliability of the data are dependent on the accuracy of the data providers. For example, the number of patients using lipid-lowering treatment in 2003 is an extreme outlier compared to the other years and is probably not representative for the actual number of patients. This difference suggests a fault in providing or collecting the data. When a patient is registered as not using a statin, this could either mean that he or she is actually not using a statin or that it is incorrectly registered. However, with respect to the process parameters this may have led at the most to an underestimation of the actual measures. Also, our study only comprises patients whom data have been reported by the GPs. It is not unlikely that GPs have opted not to provide data of patients who never show up at their diabetes check-ups. Furthermore, the number of patients who did not participate in the study due to short life expectancy of insufficient cognitive abilities is unknown after 1999.
Strengths of our study are the long follow-up period and the high number of participants, especially in the last years of the ZODIAC study. Because of the size of our database, it is important to realise that small differences may easily lead to statistical significant differences while some can hardly be called relevant. For example, the mean serum creatinine level fluctuates around 95 μmol/l throughout the whole study period, but there is a slight positive (ie, upward) linear trend for males above 75 years, while for women there is a slight negative linear trend for all age categories while the overall linear (very slightly positive) trend is nevertheless highly significant (p<0.0001).
In conclusion, our study shows that quality of diabetes care within the Dutch ZODIAC study has improved in the period 1998–2008, irrespective of age. Future studies are needed to elucidate whether there is a causal relationship between shared care and the improvements. Whether the large improvements observed in old age will lead to reductions in morbidity and mortality also remains to be determined.
Supplementary Material
Footnotes
Contributors: KJJH (guarantor), ID, NK and HJGB designed the study; KJJH and HJGB acquired the data used in this study; KJJH and KHG analysed the data; KJJH and KHG performed the statistical analyses; and all authors participated in interpretation of the data. All authors had full access to all of the data. KJJH drafted the manuscript and all authors participated in revision of the manuscript. NK, STH, KM and HJGB supervised the study.
Competing interests: None.
Ethics approval: Medical Ethics Committee of the Isala Clinics.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Turner RC, Millns H, Neil HA, et al. United Kingdom Prospective Diabetes Study Group. UK prospective diabetes study 23: risk factors for coronary artery disease in non-insulin dependent diabetes. BMJ 1998;316:823–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stamler J, Vaccaro O, Neaton JD, et al. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993;16:434–44 [DOI] [PubMed] [Google Scholar]
- 3.Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011;378:31–40 [DOI] [PubMed] [Google Scholar]
- 4.Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabetes Med 1997;14(Suppl 5):S1–85 [PubMed] [Google Scholar]
- 5.Smith SM, Allwright S, O'Dowd T. Effectiveness of shared care across the interface between primary and specialty care in chronic disease management. Cochrane Database Syst Rev 2007;3:CD004910. [DOI] [PubMed] [Google Scholar]
- 6.Ubink-Veltmaat LJ, Bilo HJ, Groenier KH, et al. Shared care with task delegation to nurses for type 2 diabetes: prospective observational study. Neth J Med 2005;63:103–10 [PubMed] [Google Scholar]
- 7.Greving JP, Denig P, de Zeeuw D, et al. Trends in hyperlipidemia and hypertension management in type 2 diabetes patients from 1998–2004: a longitudinal observational study. Cardiovasc Diabetol 2007;6:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lutgers HL, Gerrits EG, Sluiter WJ, et al. Life expectancy in a large cohort of type 2 diabetes patients treated in primary care (ZODIAC-10). PLoS One 2009;4:e6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gudbjörnsdottir S, Cederholm J, Nilsson PM, et al. The National Diabetes Register in Sweden: an implementation of the St. Vincent declaration for quality improvement in diabetes care . Diabetes Care 2003;26:1270–6 [DOI] [PubMed] [Google Scholar]
- 10.Nilsson PM. ACCORD and risk-factor control in type 2 diabetes. N Engl J Med 2010;362:1628–30 [DOI] [PubMed] [Google Scholar]
- 11.Pornet C, Bourdel-Marchasson I, Lecomte P, et al. Trends in the quality of care for elderly people with type 2 diabetes: the need for improvements in safety and quality (the 2001 and 2007 ENTRED Surveys). Diabetes Metab 2011;37:152–61 [DOI] [PubMed] [Google Scholar]
- 12.European Diabetes Working Party for Older People Clinical guidelines for type 2 diabetes mellitus 2004. http//www.instituteofdiabetes.org (Accessed 1 September 2011) [DOI] [PubMed] [Google Scholar]
- 13.De Ruijter W, Westendorp RGJ, Assendelft WJJ, et al. Use of Framingham risk score and new biomarkers to predict cardiovascular mortality in older people: population based observational cohort study. BMJ 2009;338:a3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rönnback M, Isomaa B, Fagerudd J, et al. Botnia study group. Complex relationship between blood pressure and mortality in type 2 diabetic patients: a follow-up of the Botnia study . Hypertension 2006;47:168–73 [DOI] [PubMed] [Google Scholar]
- 15.Van Hateren KJ, Landman GW, Kleefstra N, et al. The lipid profile and mortality risk in elderly type 2 diabetic patients: a ten-year follow-up study (ZODIAC-13). PLoS One 2009;4: e8464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Hateren KJ, Landman GW, Kleefstra N, et al. Lower blood pressure associated with higher mortality in elderly diabetic patients (ZODIAC-12). Age Ageing 2010;39:603–9 [DOI] [PubMed] [Google Scholar]
- 17.Van Hateren KJ, Landman GW, Kleefstra N, et al. Glycemic control and the risk of mortality in elderly type 2 diabetic patients (ZODIAC-20). Int J Clin Pract 2011;65:415–19 [DOI] [PubMed] [Google Scholar]
- 18.Rutten GEHM, Grauw WJC de, Nijpels G, et al. NHG practice guideline diabetes meliltus type 2 (second revision). Huisarts Wet 2006;49:137–52 [Google Scholar]
- 19.Lenters-Westra E, Slingerland RJ. Hemoglobin A1c determination in the A1c-derived average glucose (ADAG)-study. Clin Chem Lab Med 2008;46:1617–23 [DOI] [PubMed] [Google Scholar]
- 20.Miller DR, Pogach L. Longitudinal approaches to evaluate health care quality and outcomes: the veterans health administration diabetes epidemiology cohorts. J Diabetes Sci Technol 2008;2:24–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schunk M, Schweikert B, Gapp O, et al. Time trends in type 2 diabetes patients’ disease management and outcomes: evidence from two KORA surverys in Germany. Exp Clin Endocrinol Diabetes 2009;117:88–94 [DOI] [PubMed] [Google Scholar]
- 23.Rutten GEHM, Verhoeven S, Heine RJ, et al. NHG practice guideline diabetes mellitus type 2 (first revision). Huisarts Wet 1999;42:67–84 [Google Scholar]
- 24.Scott A, Sivey P, Ait Ouakrim D, et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database Syst Rev 2011;9:CD008451. [DOI] [PubMed] [Google Scholar]
- 25.Cherubini A, Oristrell J, Pla X, et al. The persistent exclusion of older patients from ongoing clinical trials regarding heart failure. Arch Intern Med 2011;171:550–6 [DOI] [PubMed] [Google Scholar]
- 26.Gurwith JH, Goldberg RJ. Age-based exclusions from cardiovascular clinical trials. Arch Intern Med 2011;171:557–8 [DOI] [PubMed] [Google Scholar]
- 27.Van Hateren KJ, Landman GW, Kleefstra N, et al. Time for considering new blood pressure target values in elderly patients with type 2 diabetes? IJCP 2012;66:125–7 [DOI] [PubMed] [Google Scholar]
- 28.Brown AF. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc 2003;51:S265–80 [DOI] [PubMed] [Google Scholar]
- 29.Gregg E, Beckles G, Williamson D, et al. Diabetes and physical disability among older U.S. adults . Diabetes Care 2000;23:1272–7 [DOI] [PubMed] [Google Scholar]
- 30.American Diabetes Association Standard of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl 1):S11–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.