Abstract
Background
Standard behavioral obesity treatment produces poor long-term results. Focusing on healthy eating behaviors, rather than caloric intake, may be an alternative strategy. Furthermore, important behaviors might differ for short- vs. long-term weight control.
Objective
To describe and compare associations between changes in eating behaviors and weight after 6 and 48 months
Design
Secondary analysis of data collected during a randomized weight loss intervention trial with 48-month follow-up
Participants
465 overweight and obese postmenopausal women enrolled in the Women on the Move through Activity and Nutrition (WOMAN) Study
Main outcome measures
Changes in weight from baseline to 6 and 48 months.
Statistical analyses performed
Linear regression models examined the associations between 6- and 48-month changes in eating habits assessed by the Conner Diet Habit Survey and changes in weight. Analyses were conducted in the combined study population and stratified by randomization group.
Results
At 6 months in the combined population, weight loss was independently associated with decreased desserts (p<0.001), restaurant eating (p=0.042), sugar-sweetened beverages (p=0.009), and fried foods (p<0.001), and increased fish consumption (p=0.003). Results were similar in intervention participants; only reduced desserts and fried foods associated with weight loss in controls. At 48 months in the combined population, weight loss was again associated with decreased desserts (p=0.003) and sugar-sweetened beverages (p=0.011), but also decreased meats/cheeses (p=0.024) and increased fruits/vegetables (p<0.001). Decreased meats/cheeses predicted weight loss in intervention participants; desserts, sugar-sweetened beverages, and fruits/vegetables were independently associated in controls.
Conclusions
Changes in eating behaviors were associated with weight change, though important behaviors differed for short- and long-term weight change and by randomization group. Future studies should determine whether interventions targeting these behaviors could improve long-term obesity treatment outcomes.
Keywords: diet, lifestyle intervention, weight maintenance, weight loss, obesity
INTRODUCTION
More than one third of Americans are obese,1 a condition which increases the risk of cardiovascular disease, type 2 diabetes, and some cancers,2 and has been associated with a yearly excess of 111,909 deaths in the U.S.3 The prevalence of obesity has increased over the past 50 years,1, 4 and public health initiatives for reducing the obesity epidemic have not yet substantially moved the needle on obesity rates.5 Obesity treatment through behavioral lifestyle change has been widely researched in a clinical setting with limited long-term success. Intensive behavioral clinical weight loss trials usually result in about a 10% reduction of initial body after 6 months6; however, these changes are generally not sustained long-term – even when coupled with weight maintenance interventions.7, 8
Traditional behavioral treatment for obesity has emphasized rigorous self-monitoring of daily caloric intake to achieve negative energy balance and weight loss. Indeed, evidence from the National Weight Control Registry suggests that tracking daily food intake is a common habit among successful weight loss maintainers and other studies have found that increased self-monitoring was associated with weight loss success.9–11 However, reported time and effort spent on weight control and dietary goal attainment as well as degree of satisfaction for a given effort have been reported to decrease even during the first 6 months of a weight loss program.12 This observation, coupled with the discouraging long-term weight loss maintenance outcomes using standard treatment methods, has encouraged research in the area of changing dietary patterns or specific eating behaviors for weight loss or weight control.
The 2010 USDA Dietary Guidelines advocate movement toward a `more healthful eating pattern' with specific recommendations to decrease the intake of calorically dense foods (e.g. sweets, protein sources high in saturated fats) and increase the intake of fruits, vegetables, and whole grains.13 Some studies have found long-term weight loss or maintenance to be inversely associated with eating behaviors (e.g. eating at restaurants or snacking between meals) and specific types of foods (e.g. fried foods, desserts, sweetened beverages, meats, high fat dairy products).14–20 Fruit and vegetable intake has been directly associated with long-term weight loss and maintenance.14, 16 Moreover, emerging evidence suggests that eating strategies associated with short-term weight loss may be distinct from those associated with long-term weight loss.14, 21 However, it is yet unclear which of these eating behavioral strategies are most important for weight loss in a clinical population seeking obesity treatment. Understanding which eating behaviors are important for short-term and/or long-term weight loss could be useful for designing interventions that target changes in eating behaviors as well as broader recommendations for obesity treatment and long-term weight loss at the population level.
The purpose of the current investigation was to determine if changes in eating behaviors and selected foods were associated with 6- and 48-month weight change in the WOMAN (Women on the Move through Activity and Nutrition) Study.22, 23 We hypothesized that limiting eating at restaurants and reduced consumption of desserts, sugar-sweetened beverages, fried foods, meats and cheeses as well as increased consumption of fish, fruits and vegetables would be associated with 6-month weight loss outcomes, but that only some of these eating behaviors would be associated with long-term (48-month) weight changes. We further hypothesized that eating behavior changes that predict short- and long- term weight change may differ by randomized treatment group, where targeted eating behavior changes of the lifestyle intervention would predict weight change in intervention participants but not necessarily participants in the control group.
SUBJECTS and METHODS
Study Population and Design
The WOMAN Study was conducted at the University of Pittsburgh from April 2002 to June 2008 in post-menopausal women to investigate whether a diet and physical activity lifestyle intervention with a 10% weight loss goal could impact low-density lipoprotein particles, triglycerides, and subclinical cardiovascular disease.22, 23 The study population has been previously described in detail.23 In brief, the study recruited women via direct mailings from selected zip codes in Allegheny County, Pennsylvania starting in 2002. Key eligibility criteria included: aged 52–62 years and post-menopausal, body mass index from 25–39.9 kg/m2, waist circumference >80 cm, blood pressure <140/95 mmHg, LDL cholesterol from 100–160 mg/dL, no use of lipid lowering drugs, no history of cardiovascular disease or diabetes, and no physical limitations that would preclude physical activity. A total of 508 women met eligibility criteria and were randomized to either a Lifestyle Change group (intervention) or a Health Education group (control) using block randomization. Participants were followed for 48 months. All study participants provided informed consent and the study was approved by the University of Pittsburgh institutional review board (#000356).
As previously described,23 the Lifestyle Change intervention was group-based and facilitated by nutritionists, exercise physiologists, and psychologists. Intervention groups met weekly during the first six months, bi-weekly for the next six months, and monthly for the remainder of the study. The specific intervention targets for the dietary intervention included: 1) reducing total, saturated, and trans fat along with cholesterol from meat, dairy, fats, oils, baked goods, and snacks; 2) reducing caloric intake; 3) increasing foods high in soluble fiber; 4) promotion of fruits, vegetables, and whole grains; and 5) promotion of sources of stanols/sterols and n-3 fatty acids. The physical activity component was introduced slowly during the first 6 months of the study and utilized a stepped care approach with the minimum goal of 150 minutes per week of moderate- intensity physical activity (e.g. brisk walking), which is reflective of public health recommendations for physical activity.24 If the participant was willing, the physical activity goal was increased to up to 240 minutes of moderate intensity physical activity per week. Strength training was included as an adjunct to aerobic training.
The Health Education (control) group was offered six seminars during the first year of participation and two to four yearly seminars during years two through four of the study. Seminars were lead by an experienced health professional and focused on general women's health (e.g. smoking cessation, health benefits of physical activity), but not specifically weight loss.
Study Assessments
The current investigation uses body weight assessed at baseline, 6 months, and 48 months as the primary outcomes. Eating behaviors were assessed the Connor Diet Habit Survey at the same follow-up intervals, which was slightly modified to include regional foods.25 This questionnaire was developed for the Family Health Study and includes 32 items assessing regular eating behaviors in the past month, including frequency of desserts, fried foods, sugar-sweetened beverages, fruits, vegetables, meats and cheeses along with the frequency of eating meals (breakfast, lunch, and dinner separately) at restaurants. Questionnaire answers were converted into frequencies based on the question (e.g., times per month) and scores were averaged when more than one answer was selected by the participant. Associations were similar for fruits and vegetables taken separately as well as eating at restaurants for specific meals, and so these variables were combined into fruits + vegetables and all restaurant eating, respectively. Ten-day test-retest reliability as well as validity against 24 hour recall and with changes in plasma lipids over time for this instrument have been previously shown to be comparable with other dietary assessment instruments.25, 26
Leisure-time physical activity was assessed at baseline and 48 months using the Modifiable Activity Questionnaire (MAQ), an interviewer-administered questionnaire that assesses past-year leisure-time and occupational physical activity.27 Due to the limited reported occupational activity in the WOMAN Study population,28 only the leisure-time estimate is reported. Physical activity levels were calculated as the product of the duration and frequency of 39 common leisure activities (hr·wk−1), weighted by a standardized estimate of the metabolic equivalent (MET) of each activity,29 and then summed for all activities performed. Leisure-time physical activity was expressed as metabolic equivalent hours per week (MET·hr·wk−1). The MAQ is a reliable and valid estimate of self-reported physical activity.30
Statistical Analyses
This secondary data analysis included WOMAN Study subjects with complete body weight and eating habits data at baseline and at least one of the 6 or 48 month follow-up assessments. Baseline participant characteristics are summarized overall and by randomized group assignment. Continuous variables are reported as either mean ± standard deviation or median (interquartile rage). Categorical variables are presented as proportions.
Pearson's correlations were calculated between 6-month changes in weight and 6-month changes in eating behaviors overall and by randomized group, adjusted for baseline values of weight and eating behavior. This was repeated for 48-month changes. Participants were then categorized into one of four weight loss categories based on amount of weight lost from baseline to 6 and 48 months: weight gain defined as a weight increase ≥2.5 kg; weight stable defined as a weight change in either direction of < 2.5 kg31; moderate weight loss defined as a weight loss from 2.5 to 10 kg; and significant weight loss defined as a >10 kg weight loss. Eating behaviors at baseline and follow-up were plotted for each weight change category overall and by randomization group. Absolute changes in eating behaviors were compared across increasing weight loss categories at 6 and 48 months using a parametric test for trend adjusted for randomized group (overall results only), baseline weight, and baseline eating behavior.
Linear regression models were used to examine associations between changes in weight (kgs) and changes in eating behaviors in separate models at 6 and 48 months. Change in weight was used as the dependent variable, controlling for baseline weight and group. All change variables were assessed for normality and models were evaluated for points of influence. Single behavior models used change in one eating behavior as the primary independent variable and adjusted for the baseline value of that behavior. Fully adjusted model included all covariates listed above and each change in behavior and baseline behavior value. Beta (β) coefficients were standardized so that the coefficient can be interpreted as the change in weight associated with a change of one standard deviation in each eating behavior and compared across behaviors. Models are reported in all participants and after stratification by randomized group assignment. Lastly, change in leisure-time physical activity from baseline to 48 months (not assessed at 6 months) was added to the 48 month models to determine the influence on associations between changes in eating habits and weight.
All analyses were conducted using Stata version 10 (StataCorp, College Station, TX).
RESULTS
Of the 508 women enrolled in the study, n=465 (92%) women had complete data for 6-months and n=419 (82%) women had complete data for 48 months. Table 1 presents baseline characteristics for women with complete data at either follow-up (n=481). Groups were balanced with the exception of greater dessert consumption among controls. Subsequent analyses adjust for baseline values and do not investigate the effect of the intervention.
Table 1.
Baseline Characteristics of WOMAN Study Participants
| Overall (n=481) | Intervention (n=241) | Control (n=240) | p-valuea | |
|---|---|---|---|---|
| Age, years | 57.0 ± 2.9 | 56.8 ± 2.9 | 57.2 ± 2.9 | 0.237 |
| % Caucasian | 88 | 90 | 87 | 0.249 |
| Body Mass Index, kg/m2 | 30.8 ± 3.8 | 30.6 ± 3.8 | 30.9 ± 3.8 | 0.412 |
| Weight, kg | 81.7 ± 11.5 | 81.4 ± 11.3 | 82.0 ± 11.7 | 0.542 |
| Desserts, servings per month | 13.3 ± 9.5 | 12.3 ± 9.0 | 14.4 ± 9.9 | 0.019 |
| Eating at Restaurants, times per month | 13.9 ± 9.6 | 14.1 ± 9.8 | 13.7 ± 9.3 | 0.696 |
| Sugar-sweetened Beverages, 12 ounce servings per dayb | 0 [0, 1] | 0 [0, 1] | 0 [0, 1] | 0.714 |
| Fried Foods, servings per monthb | 7 [2, 12] | 7 [2, 12] | 7 [2, 12] | 0.792 |
| Fish, servings per month | 4.1 ± 3.3 | 4.2 ± 3.4 | 3.9 ± 3.1 | 0.292 |
| Meat and Cheese, ounces per day | 6.3 ± 2.4 | 6.3 ± 2.6 | 6.2 ± 2.3 | 0.568 |
| Fruits and Vegetables, servings per day | 4.1 ± 1.9 | 4.2 ± 1.8 | 4.2 ± 1.9 | 0.405 |
| Leisure time physical activity, MET-hours/weekb | 11.1 [5.3, 20.3] | 10.7 [5.9, 19.9] | 11.5 [4.9, 21.5] | 0.533 |
Data presented as mean ± standard deviation unless otherwise specified
Comparison across intervention groups by t test, Wilcoxon rank-sum test, or the chi-square test as appropriate
Median [interquartile range]
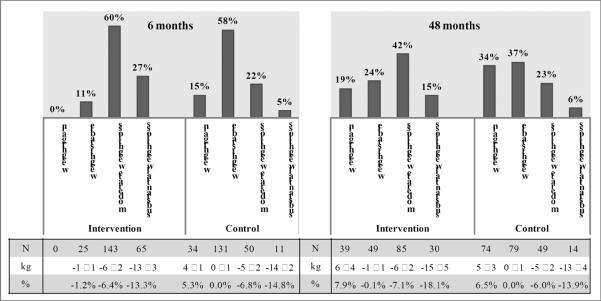
Average weight change in intervention vs. control participants was −7.8 ± 4.5 kg vs. −1.3 ± 4.3 kg at 6 months (p<0.001) and −3.6 ± 7.3 kg vs. −0.2 ± 5.6 kg (p<0.001) at 48 months. When separated into categories of weight gain, weight stable, moderate and substantial weight loss, the distribution of participants across weight change categories differed by randomized group with intervention participants more frequently in the weight loss categories at 6 (p<0.001) and 48 months (p<0.001) (Figure 1).
Figure 1. Weight Change Category at 6-months and 48-months by Intervention Group.
Weight Gain (>2.5kg); Weight Stable (±2.5kg); Moderate Weight Loss (2.5–10kg); Substantial Weight Loss (>10kg)
Table displays number, mean weight loss ± standard deviation, and percent weight change by intervention group and weight loss category.
At 6 months, changes in weight were significantly correlated with changes in each eating behavior in the expected direction in the combined study population (Table 2). Correlations were consistent across randomized groups for consuming desserts and fried foods, but significant correlations were only observed in the intervention group for eating at restaurants, consuming fish, and eating meats and cheeses. Weight change was significantly correlated with consuming sugar-sweetened beverages and fruits and vegetables in the control group only. At 48 months, again most changes in eating behaviors were correlated with changes in weight, with the exception of frequency of eating at restaurants (r = 0.06, p=0.218). Change in leisure-time physical activity was inversely correlated with weight change at 48 months (r = −0.21, p<0.001). When stratified by randomized group, consuming fish and meats and cheeses were only significantly correlated with weight change in intervention participants. Consumption of sugar-sweetened beverages was also significant in intervention participants and not controls, though the magnitude of association was quite comparable.
Table 2.
Pearson's Correlations (r)a of Changes in Eating Behaviorsb and Change in Weight at 6 and 48 Months in WOMAN Study Participants
| Change in Eating Behavior | 0–6 months | 0–48 months | ||||
|---|---|---|---|---|---|---|
| Overall (n=465) | Intervention (n=238) | Control (n=227) | Overall (n=419) | Intervention (n=203) | Control (n=216) | |
| Desserts | 0.43*** | 0.32*** | 0.29*** | 0.20*** | 0.17* | 0.23** |
| Eating at Restaurants | 0.19*** | 0.19** | 0.12 | 0.06 | 0.10 | 0.04 |
| Sugar-Sweetened Beverages | 0.21*** | 0.12 | 0.21** | 0.14** | 0.13 | 0.15* |
| Fried Foods | 0.39*** | 0.28*** | 0.25*** | 0.14** | 0.13 | 0.10 |
| Fish | −0.24*** | −0.24*** | −0.09 | −0.12* | −0.18* | −0.02 |
| Meat and Cheese | 0.22*** | 0.14* | −0.04 | 0.18*** | 0.24** | −0.01 |
| Fruits and Vegetables | −0.22*** | −0.08 | −0.17** | −0.24*** | −0.20** | −0.29*** |
| Physical Activity (MET-hr/week)c | −0.21*** | −0.28*** | −0.14* | |||
Adjusted for baseline weight and eating behavior
Eating behaviors measured by the Connor Diet Habit Survey assessing usual behavior in the past month
Physical activity assessed by the Modifiable Activity Questionnaire, not assessed at 6 months
p<0.05,
p<0.01
p<0.001
In the combined study population, progressive changes from baseline to 6 months in each behavior were observed across weight change categories in the expected direction (Figure 2), with the exception of a nonsignificant trend for change in frequency of eating at restaurants (p=0.051) and no association with change in consumption of meats and cheese (p=0.616). Analyses stratified by randomized group were similar with the exception of significant associations for eating at restaurants and fish among intervention participants only, while significant associations with sugar-sweetened beverages and fruits and vegetables were only observed in controls (Appendix Figures 1 and 2).
Figure 2. Change in Eating Behaviors by 6-month and 48-month Weight Loss Categories.
Weight Gain (>2.5kg); Weight Stable (±2.5); Moderate Weight Loss (2.5–10kg); Substantial Weight Loss (>10kg) p for trend tests changes in each behavior across increasing weight loss categories adjusted for baseline weight, baseline eating behavior, and randomized group.
At 48 months in the combined study population, a progressive trend across weight change categories was observed for all behaviors except for frequency of eating at restaurants (p=0.573) (Figure 2). Within randomized groups, associations were heterogeneous across randomized groups. Among intervention participants, increasing weight loss category was associated with decreased consumption of meat and cheeses and sugar-sweetened beverages, and increased consumption of fruits and vegetables. Among controls, increasing weight loss category was associated with decreased consumption of desserts and fried foods, and with increased consumption of fruits and vegetables (Appendix Figures 1 and 2).
Using linear regression models including all eating behaviors, frequency of desserts, eating at restaurants, sugar-sweetened beverages, fried foods, and fish were independently associated with 6-month weight change in all WOMAN Study participants (bottom of Table 3). Similar relationships were observed when the analysis was repeated among only intervention participants. In controls, only changes in the frequency of eating desserts and fried foods were associated with changes in weight at 6 months.
Table 3.
Association of Changes in Eating Behaviorsa and Change in Weight at 6 Months
| All Subjects (n=465) | Intervention (n=238) | Control (n=227) | ||||
|---|---|---|---|---|---|---|
| Single Eating Behavior Modelb | Std β | p-value | Std β | p-value | Std β | p-value |
| Change in Desserts | 1.59 | <0.001 | 2.11 | <0.001 | 1.40 | <0.001 |
| Change in Eating at Restaurants | 0.79 | 0.001 | 1.01 | 0.003 | 0.56 | 0.082 |
| Change in Sugar-Sweetened Beverages | 1.05 | <0.001 | 0.86 | 0.071 | 1.05 | 0.001 |
| Change in Fried Foods | 1.93 | <0.001 | 2.63 | <0.001 | 1.77 | <0.001 |
| Change in Fish | −0.82 | <0.001 | −1.14 | <0.001 | −0.40 | 0.189 |
| Change in Meat and Cheese | 0.29 | 0.221 | 0.71 | 0.034 | −0.18 | 0.578 |
| Change in Fruits and Vegetables | −0.59 | 0.013 | −0.36 | 0.267 | −0.88 | 0.009 |
| All Eating Behaviors Modelc | std β | p-value | Std β | p-value | Std β | p-value |
| Change in Desserts | 0.95 | <0.001 | 1.41 | 0.001 | 0.83 | 0.020 |
| Change in Eating at Restaurants | 0.46 | 0.042 | 0.68 | 0.037 | 0.28 | 0.365 |
| Change in Sugar-Sweetened Beverages | 0.74 | 0.009 | 0.91 | 0.040 | 0.57 | 0.120 |
| Change in Fried Foods | 1.32 | <0.001 | 1.48 | 0.031 | 1.49 | <0.001 |
| Change in Fish | −0.61 | 0.003 | −0.87 | 0.003 | −0.33 | 0.249 |
| Change in Meat and Cheese | 0.10 | 0.668 | 0.36 | 0.267 | −0.24 | 0.424 |
| Change in Fruits and Vegetables | −0.37 | 0.102 | −0.15 | 0.627 | −0.58 | 0.079 |
Eating behaviors measured by the Connor Diet Habit Survey assessing usual behavior in the past month
This model uses change in weight in kilograms as the dependent variable adjusted for group, baseline weight, and baseline eating behavior value but not the other eating behavioral variables listed in the table
This model includes all eating behavior variables adjusted for group, baseline weight, and all baseline eating behavior values
At 48 months (bottom of Table 4), weight change was independently associated with frequency of consuming desserts, sugar-sweetened beverages, meats/cheeses, and fruits/vegetables when including all eating behaviors. Within the intervention group in the fully adjusted model, weight change was only significantly associated with frequency of meats and cheeses. Among controls, frequency of desserts, sugar-sweetened beverages, and fruits and vegetables were independent predictors of weight change in the fully adjusted model.
Table 4.
Association of Changes in Eating Behaviorsa and Change in Weight (kg) at 48 Months
| All Subjects (n=419) | Intervention (n=203) | Control (n=216) | ||||
|---|---|---|---|---|---|---|
| Single Eating Behavior Modelb | Std β | p-value | Std β | p-value | Std β | p-value |
| Change in Desserts | 1.61 | <0.001 | 1.60 | 0.015 | 1.61 | 0.001 |
| Change in Eating at Restaurants | 0.48 | 0.225 | 0.34 | 0.599 | 0.68 | 0.143 |
| Change in Sugar-Sweetened Beverages | 1.42 | 0.005 | 1.57 | 0.064 | 1.27 | 0.029 |
| Change in Fried Foods | 1.04 | 0.019 | 1.04 | 0.173 | 1.01 | 0.052 |
| Change in Fish | −0.73 | 0.030 | −1.40 | 0.012 | −0.12 | 0.768 |
| Change in Meat and Cheese | 1.03 | 0.005 | 2.02 | 0.001 | −0.09 | 0.834 |
| Change in Fruits and Vegetables | −1.73 | <0.001 | −1.79 | 0.006 | −1.76 | <0.001 |
| All Eating Behaviors Modelc | Std β | p-value | Std β | p-value | Std β | p-value |
| Change in Desserts | 1.20 | 0.003 | 0.74 | 0.282 | 1.59 | 0.001 |
| Change in Eating at Restaurants | 0.13 | 0.735 | −0.10 | 0.871 | 0.27 | 0.546 |
| Change in Sugar-Sweetened Beverages | 1.25 | 0.011 | 1.53 | 0.072 | 1.28 | 0.023 |
| Change in Fried Foods | 0.46 | 0.304 | 0.72 | 0.358 | 0.34 | 0.505 |
| Change in Fish | −0.30 | 0.372 | −0.92 | 0.099 | 0.19 | 0.640 |
| Change in Meat and Cheese | 0.82 | 0.024 | 2.07 | <0.001 | −0.51 | 0.261 |
| Change in Fruits and Vegetables | −1.48 | <0.001 | −1.13 | 0.090 | −1.76 | <0.001 |
Eating behaviors measured by the Connor Diet Habit Survey assessing usual behavior in the past month
This model uses change in weight in kilograms as the dependent variable adjusted for group, baseline weight, and baseline eating behavior value but not the other eating behavioral variables listed in the table
This model includes all eating behavior variables adjusted for group, baseline weight, and all baseline eatins behavior values
Change in leisure time physical activity was associated with 48 month weight change (standardized β = −1.29 kg per MET-hour/week, p<0.001), but the addition of physical activity to the model did not change associations observed between eating habits and weight change at 48 months (data not shown).
DISCUSSION
The WOMAN Study is one of the few long term weight reduction studies and, similar to other studies,6 documents the difficulties of maintaining substantial weight loss over time for most of the participants. As hypothesized, most of the eating habits predicted weight change at 6 months when considered individually, and results in the intervention group mirrored the analysis including all WOMAN Study participants. Interestingly, most of these eating behaviors were independently associated with weight change in the fully adjusted model, suggesting a role for each eating behavior change in the context of short-term weight loss or control. Decreased consumption of fried foods and desserts had the largest standardized coefficients when including all WOMAN participants and within the intervention group, and these were the only significant predictors in fully adjusted analysis within the control group, highlighting these two specific targets for short-term weight change. At 48 months, frequency of eating at restaurants was consistently not associated with weight change, though the other eating behaviors continued to have associations when considered in isolation. In the fully adjusted model, only changes in meat and cheese intake were associated with weight change in the intervention group while desserts, sugar-sweetened beverages, and fruits and vegetables were independent predictors in the control group. These behavior changes could represent changes in eating behaviors that both influence weight change and are sustainable long-term.
A surprising finding was that frequency of eating at restaurants was not related to weight change outcomes at 48 months. Reported restaurant eating decreased whether subjects decreased weight or not (see Figure 2), consistent with the lack of association observed even in the single behavior analyses. Specific measurement of the frequency of dining at fast food restaurants, which has been shown to predict weight change in other studies,32, 33 was not available but may have been more strongly associated with weight change.
The associations observed at 6 months and 48 months were all consistent with a diet that decreases energy density. Lower energy density has been associated with greater weight loss or decreased weight gain in cohort studies,34, 35 secondary analyses within clinical weight loss trials,36–38 and in randomized trials.39, 40 Further, successful weight loss maintainers report a diet with lower energy density compared to normal weight or obese controls,16 indicating that decreasing energy density may be a particularly useful strategy for maintaining a weight-reduced state. At the same time, many of the behaviors that predicted weight change were specific targets of the intervention. Thus, results within the intervention group in particular may also reflect that weight loss or maintenance is more common among participants that follow dietary prescriptions more closely.
The differences in the magnitude of the associations between the intervention and control groups in this secondary analysis should be interpreted with caution. The intervention group received active treatment, especially during the first year, which resulted in a distribution of weight change in this group that was shifted toward weight loss with 85% of participants maintaining or losing weight at 48 months (Figure 1). In contrast among controls, the distribution of weight change was more centered around weight maintenance, with about a third of controls achieving weight loss (29%), maintenance (37%), and weight gain (34%) at 48 months (Figure 1). With this in mind, results from the intervention group may be more applicable to short- and long-term weight loss in a clinical setting; whereas, findings in the control group may be more applicable to women interested in weight loss who have not received an evidence-based intervention in a clinical setting.
Strengths of this study include a large sample size, long duration, and excellent retention in a lifestyle intervention study. Though the average weight loss at 48 months in the intervention group was <5%, a sizable subset of women had lost more than a 10 kgs at 48 months, providing variability in the outcome measure. With these strengths and the measurement of eating habits at relevant time points, this study was able to tease out which eating habits were independently related to short-term and long-term weight change in post-menopausal women.
On the other hand, several limitations deserve discussion. First, eating behaviors and physical activity were self-reported and thus vulnerable to the known biases involved with self-report, such as underreporting of undesirable habits (e.g. eating desserts). Further, seasonality may have affected certain eating habits between the baseline and 6 month assessments, e.g. fruits and vegetables, and this could explain why changes in fruits and vegetables were not independently associated with weight change at 6 months. Change in leisure-time physical activity over the first 6 months of the intervention was not included in regression models because the physical activity component of the intervention was slowly introduced during the first 6 months. However, the 48-month results reassuringly showed associations between eating behaviors and weight change to be independent of physical activity. Also, certain eating behaviors are collinear as evidenced by the attenuated associations when moving from single eating behavior models to all eating behaviors models, for example eating of fried foods and eating at restaurants. However, these eating behaviors had independent associations with weight change at 6 months and each single behavior model is reported to inform this issue. Also, information on frequency of snacking between meals, which may be another eating behavior associated with weight change, was not collected. Lastly, this secondary analysis identifies associations between changes in eating behaviors and changes in weight, but the study was not specifically designed to evaluate whether targeting changes in these behaviors would result in greater weight loss.
In summary, these results suggest that decreased consumption of desserts and sugar-sweetened beverages consistently associate with short- and long-term weight loss or maintenance, but increased fruits/vegetables in controls as well as decreased meats/cheeses in an intervention are additional factors that may help for long-term, but not necessarily short-term, weight loss or control. If the goal is to decrease the burden of obesity, the focus must be on long-term strategies because changes in eating behaviors only associated with short-term weight loss are likely ineffective and/or not sustainable. Future studies should examine whether interventions focused on changing these specific eating behaviors associated with long-term weight change could improve obesity treatment outcomes.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010 Jan 20;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Kopelman P. Health risks associated with overweight and obesity. Obes Rev. 2007 Mar;8(Suppl 1):13–17. doi: 10.1111/j.1467-789X.2007.00311.x. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005 Apr 20;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998 Jan;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 5.Sondik EJ, Huang DT, Klein RJ, Satcher D. Progress toward the healthy people 2010 goals and objectives. Annu Rev Public Health. 2010 Apr 21;31:271–281. doi: 10.1146/annurev.publhealth.012809.103613. 274 p folliwng 281. [DOI] [PubMed] [Google Scholar]
- 6.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007 Oct;107(10):1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008 Mar 12;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 8.Garcia Ulen C, Huizinga MM, Beech B, Elasy T. Weight Regain Prevention. Clinical Diabetes. 2008;26(3):100–113. [Google Scholar]
- 9.Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring) 2007 Dec;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- 10.Bartfield JK, Stevens VJ, Jerome GJ, et al. Behavioral Transitions and Weight Change Patterns Within the PREMIER Trial. Obesity (Silver Spring) 2011 Aug;19(8):1609–1615. doi: 10.1038/oby.2011.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. STOP regain: are there negative effects of daily weighing? J Consult Clin Psychol. 2007 Aug;75(4):652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- 12.Jeffery RW, Kelly KM, Rothman AJ, Sherwood NE, Boutelle KN. The weight loss experience: a descriptive analysis. Ann Behav Med. 2004 Apr;27(2):100–106. doi: 10.1207/s15324796abm2702_4. [DOI] [PubMed] [Google Scholar]
- 13.2010 Dietary Guidelines Updated recommendations put focus on obesity. Mayo Clin Womens Healthsource. 2010 Dec;14(12):1–2. [PubMed] [Google Scholar]
- 14.Kruger J, Blanck HM, Gillespie C. Dietary practices, dining out behavior, and physical activity correlates of weight loss maintenance. Prev Chronic Dis. 2008 Jan;5(1):A11. [PMC free article] [PubMed] [Google Scholar]
- 15.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005 Feb;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 16.Raynor HA, Van Walleghen EL, Bachman JL, Looney SM, Phelan S, Wing RR. Dietary energy density and successful weight loss maintenance. Eat Behav. 2011 Apr;12(2):119–125. doi: 10.1016/j.eatbeh.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.French SA, Jeffery RW, Forster JL, McGovern PG, Kelder SH, Baxter JE. Predictors of weight change over two years among a population of working adults: the Healthy Worker Project. Int J Obes Relat Metab Disord. 1994 Mar;18(3):145–154. [PubMed] [Google Scholar]
- 18.Holden JH, Darga LL, Olson SM, Stettner DC, Ardito EA, Lucas CP. Long-term follow-up of patients attending a combination very-low calorie diet and behaviour therapy weight loss programme. Int J Obes Relat Metab Disord. 1992 Aug;16(8):605–613. [PubMed] [Google Scholar]
- 19.Boggs DA, Palmer JR, Spiegelman D, Stampfer MJ, Adams-Campbell LL, Rosenberg L. Dietary patterns and 14-y weight gain in African American women. Am J Clin Nutr. 2011 Jul;94(1):86–94. doi: 10.3945/ajcn.111.013482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phelan S, Liu T, Gorin A, et al. What distinguishes weight-loss maintainers from the treatment-seeking obese? Analysis of environmental, behavioral, and psychosocial variables in diverse populations. Ann Behav Med. 2009 Oct;38(2):94–104. doi: 10.1007/s12160-009-9135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sciamanna CN, Kiernan M, Rolls BJ, et al. Practices associated with weight loss versus weight-loss maintenance results of a national survey. Am J Prev Med. 2011 Aug;41(2):159–166. doi: 10.1016/j.amepre.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Kuller LH, Pettee Gabriel KK, Kinzel LS, et al. The Women on the Move Through Activity and Nutrition (WOMAN) Study: Final 48-Month Results. Obesity (Silver Spring) 2011 Apr 14; doi: 10.1038/oby.2011.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuller LH, Kriska AM, Kinzel LS, et al. The clinical trial of Women On the Move through Activity and Nutrition (WOMAN) study. Contemp Clin Trials. 2007 Jul;28(4):370–381. doi: 10.1016/j.cct.2006.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United States. Public Health Service. Office of the Surgeon General. National Center for Chronic Disease Prevention and Health Promotion (U.S.) President's Council on Physical Fitness and Sports (U.S.) Physical activity and health : a report of the Surgeon General. U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention President's Council on Physical Fitness and Sports; Atlanta, Ga. Washington, D.C. Pittsburgh, PA: 1996. For sale by the Supt. of Docs. [Google Scholar]
- 25.Connor SL, Gustafson JR, Sexton G, Becker N, Artaud-Wild S, Connor WE. The Diet Habit Survey: a new method of dietary assessment that relates to plasma cholesterol changes. J Am Diet Assoc. 1992 Jan;92(1):41–47. [PubMed] [Google Scholar]
- 26.Hollis JF, Carmody TP, Connor SL, Fey SG, Matarazzo JD. The Nutrition Attitude Survey: associations with dietary habits, psychological and physical well-being, and coronary risk factors. Health Psychol. 1986;5(4):359–374. doi: 10.1037//0278-6133.5.4.359. [DOI] [PubMed] [Google Scholar]
- 27.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997 Jun;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
- 28.Pettee KK, Kriska AM, Conroy MB, et al. Discontinuing hormone replacement therapy: attenuating the effect on CVD risk with lifestyle changes. Am J Prev Med. 2007 Jun;32(6):483–489. doi: 10.1016/j.amepre.2007.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000 Sep;32(9 Suppl):S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 30.Kriska AM, Knowler WC, LaPorte RE, et al. Development of questionnaire to examine relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990 Apr;13(4):401–411. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 31.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes (Lond) 2006 Mar;30(3):391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 32.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005 Jan 1–7;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 33.French SA, Harnack L, Jeffery RW. Fast food restaurant use among women in the Pound of Prevention study: dietary, behavioral and demographic correlates. Int J Obes Relat Metab Disord. 2000 Oct;24(10):1353–1359. doi: 10.1038/sj.ijo.0801429. [DOI] [PubMed] [Google Scholar]
- 34.Savage JS, Marini M, Birch LL. Dietary energy density predicts women's weight change over 6 y. Am J Clin Nutr. 2008 Sep;88(3):677–684. doi: 10.1093/ajcn/88.3.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bes-Rastrollo M, van Dam RM, Martinez-Gonzalez MA, Li TY, Sampson LL, Hu FB. Prospective study of dietary energy density and weight gain in women. Am J Clin Nutr. 2008 Sep;88(3):769–777. doi: 10.1093/ajcn/88.3.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flood A, Mitchell N, Jaeb M, et al. Energy density and weight change in a long-term weight-loss trial. Int J Behav Nutr Phys Act. 2009;6:57. doi: 10.1186/1479-5868-6-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ledikwe JH, Rolls BJ, Smiciklas-Wright H, et al. Reductions in dietary energy density are associated with weight loss in overweight and obese participants in the PREMIER trial. Am J Clin Nutr. 2007 May;85(5):1212–1221. doi: 10.1093/ajcn/85.5.1212. [DOI] [PubMed] [Google Scholar]
- 38.de Oliveira MC, Sichieri R, Venturim Mozzer R. A low-energy-dense diet adding fruit reduces weight and energy intake in women. Appetite. 2008 Sep;51(2):291–295. doi: 10.1016/j.appet.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 39.Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr. 2007 Jun;85(6):1465–1477. doi: 10.1093/ajcn/85.6.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rolls BJ, Roe LS, Beach AM, Kris-Etherton PM. Provision of foods differing in energy density affects long-term weight loss. Obes Res. 2005 Jun;13(6):1052–1060. doi: 10.1038/oby.2005.123. [DOI] [PubMed] [Google Scholar]