Abstract
Background
People with stroke have reduced walking activity. It is not known whether this deficit is due to a reduction in all aspects of walking activity or only in specific areas. Understanding specific walking activity deficits is necessary for the development of interventions that maximize improvements in activity after stroke.
Objective
The purpose of this study was to examine walking activity in people poststroke compared with older adults without disability.
Design
A cross-sectional study was conducted.
Methods
Fifty-four participants poststroke and 18 older adults without disability wore a step activity monitor for 3 days. The descriptors of walking activity calculated included steps per day (SPD), bouts per day (BPD), steps per bout (SPB), total time walking per day (TTW), percentage of time walking per day (PTW), and frequency of short, medium, and long walking bouts.
Results
Individuals classified as household and limited community ambulators (n=29) did not differ on any measure and were grouped (HHA-LCA group) for comparison with unlimited community ambulators (UCA group) (n=22) and with older adults without disability (n=14). The SPD, TTW, PTW, and BPD measurements were greatest in older adults and lowest in the HHA-LCA group. Seventy-two percent to 74% of all walking bouts were short, and this finding did not differ across groups. Walking in all categories (short, medium, and long) was lowest in the HHA-LCA group, greater in the UCA group, and greatest in older adults without disability.
Limitations
Three days of walking activity were captured.
Conclusions
The specific descriptors of walking activity presented provide insight into walking deficits after stroke that cannot be ascertained by looking at steps per day alone. The deficits that were revealed could be addressed through appropriate exercise prescription, underscoring the need to analyze the structure of walking activity.
Stroke is the leading cause of disability in the United States.1 Approximately 80% of the 5.5 million people living with stroke have some level of disability.2 This disability is a consequence of, and a risk factor for, physical inactivity.3,4 Lack of physical activity has serious health and functional consequences for people poststroke, including an increased risk of a second stroke5 and an increased risk of mortality.1 Inactivity exacerbates the normal decline in aerobic fitness, putting the cardiovascular capacity of most people poststroke below the level needed for activities of daily living.6,7 Therefore, a thorough understanding of inactivity after stroke is necessary to develop optimal interventions to improve activity.
Activity after stroke is most commonly examined using self-report measures or accelerometer-based devices that can provide accurate and reliable information about daily step activity.7–9 Results from a variety of studies using step monitoring devices demonstrate that daily walking activity in people with chronic (>6 months) stroke is extremely low,7,10,11 well below the activity level of even the most sedentary adults (<5,000 steps/day).12 However, daily step activity differs depending on walking speed after stroke. Using Perry's classification of ambulation status, which is based on walking speed, Bowden and colleagues10 found that the number of steps per day are lowest in those who are limited to household ambulation and greatest in those who are unlimited community ambulators. Although daily step counts provide a global representation of physical activity, they provide little understanding of the structure of daily walking activity. By examining walking activity, including how often a person engages in walking, the length of each walking bout, and how often bouts of varying lengths occur, important information is obtained regarding specific walking activity deficits outside a clinical setting.13,14 This information can provide a foundation for the future development of more focused therapeutic interventions that address the specific walking activity deficits observed.
The purpose of this study was to examine walking activity in people poststroke with a wide variety of functional walking ability, as measured by gait speed, and compare them with older adults without disability. We hypothesized that analyzing walking activity would reveal differences between groups that are not revealed by counting steps per day alone. This information is currently not available, yet it is critical for the design of optimal interventions that target the primary deficits that lead to restriction of walking activity after stroke.
Method
Participants
All people poststroke living in the community and older adults without disability who were retired or semiretired were invited to participate in this 16-month project. This sample of convenience was recruited from local physical therapy clinics and stroke support groups and through advertisements in the local newspaper. Individuals poststroke were included if they were older than 18 years, had experienced a stroke, were able to walk without assistance of another person (orthotic and assistive devices were allowed), and were able to follow instructions and communicate with the investigators. Individuals poststroke were excluded if they had additional neurologic diagnoses. All individuals poststroke received medical clearance to participate in the research study. Older adults without disability were included if they were retired or semiretired and did not have any deficits that would affect walking. All included individuals signed informed consent approved by the Human Subjects Review Board at University of Delaware prior to participation.
Procedure
A StepWatch Activity Monitor (SAM) (Orthocare Innovations, Seattle, Washington) was placed above the ankle on the nonparetic lower extremity for individuals poststroke and the leg that corresponded with the dominant hand for older adults without disability. The SAM was calibrated to each participant's height and walking characteristics per manufacturer's instructions. Calibration was checked by having participants walk 30 strides at their self-selected speed and 10 strides at a slightly faster pace. Recalibration was performed if the number of manually counted strides differed from the SAM-counted strides by ≥2. The number of strides was counted in each consecutive 5-second interval (changed from the SAM default interval of 60 seconds) to ensure the most accurate representation of continuous stepping in individuals across a wide range of walking speeds.
Participants were asked to wear the SAM for 3 consecutive days during all waking hours except during bathing and swimming activities. An information packet given to all participants included instructions for wearing the SAM and a physical activity diary for documenting the time the device was donned and doffed each day.
Data Analysis
The SAM data were processed using a custom-designed MATLAB program (The MathWorks Inc, Natick, Massachusetts) to obtain the walking pattern variables of interest. To determine the beginning and end of a walking bout, we developed an algorithm based on a previous study.14 First, we operationally defined the start of a walking bout as 3 strides within a 15-second interval and the end of a walking bout as a 10-second interval in which no strides occurred. This algorithm prevented leg movements during resting or standing from being counted as strides during walking. Once data were grouped into walking bouts, the stride count was doubled to provide the number of steps per day (SPD). Additional calculations provided the number of walking bouts per day (BPD), median steps per bout (SPB), total time walking per day (TTW), and percentage of time walking per day (PTW) (defined as the ratio of total time walking to total time wearing the SAM each day).
To analyze walking in the context of real-world community mobility, further data reduction was performed based on the study by Andrews et al.15 They found that going to a physician's office, post office, or bank required walking a minimum of 25.1 m and a maximum of 149.4 m. We consider these medium distances. Activities such as shopping in a grocery store, department store, or superstore required individuals to walk a minimum of 206.3 m,15 which we considered long distances. We divided those distances by the average adult step length (when walking at speeds matched to those poststroke) of 0.5 m16 and operationally defined a medium-distance bout as containing 41 to 300 steps and a long-distance bout as containing 300 or more steps. We operationally defined a short-distance bout as containing <40 steps based on a study of employed people without disability that demonstrated 75% of walking occurs in short bouts of <40 steps in a row.14 Using these operational definitions, we calculated the frequency of short, medium, and long bouts walked by each participant over the 3 days.
Finally, the participants with stroke were divided into 3 groups based on the speed-based walking classification system developed by Perry et al.17 Based on this system, individuals who ambulated less than 0.4 m/s were classified as household ambulators (HHA group), those who ambulated between 0.4 and 0.8 m/s were classified as limited community ambulators (LCA group), and those who ambulated faster than 0.8 m/s were classified as unlimited community ambulators (UCA group).17
Statistical Analysis
The descriptors of step activity were calculated for each day, and the average values across days were used in analysis of group differences for SPD, BPD, SPB, TTW, and PTW. The numbers of short-, medium-, and long-distance bouts were calculated over all 3 days. The data were not normally distributed, so nonparametric statistics were used. Independent-samples Kruskal-Wallis one-way analysis of variance by ranks was utilized to identify group differences. When group differences were found, Mann-Whitney U tests were used for post hoc tests. We hypothesized that individuals without disability would have significantly more SPD, BPD, TTW, PTW, and quantity of small, medium, and long walking bouts than those poststroke.
Results
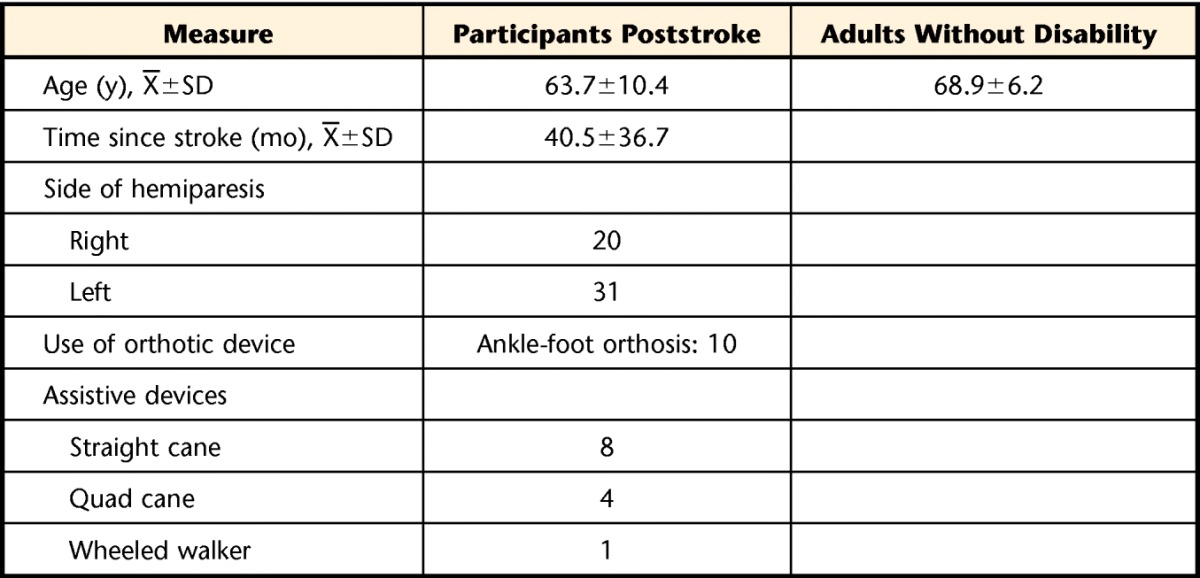
Eighty-five participants poststroke were screened for participation. Twenty-two participants poststroke were referred by health care practitioners, 38 responded to newspaper advertisements, and 18 were recruited through participation in stroke support groups. Seven participants poststroke and 18 older adults without disability were part of our research database of previous study participants who had given permission to be contacted for appropriate future studies. Following the screening procedures, 21 participants were unable to meet the inclusion criteria, and 10 participants did not return the necessary paperwork for participation. The remaining 54 participants poststroke and 18 older adults without disability underwent evaluation and participated in this research project. However, 7 participants (3 participants poststroke) did not return the SAM with a minimum of 3 days of ambulation activity and, therefore, were excluded, leaving 51 participants poststroke and 14 older adults without disability who underwent data analysis. Participant demographic information is presented in the Table. Of the 51 participants with stroke, 12 were classified as belonging to the HHA group (average gait speed=0.31 m/s, SD=0.07), 17 were classified as belonging to the LCA group (average gait speed=0.62 m/s, SD=0.10), and 22 were classified as belonging to the UCA group (average gait speed=1.01 m/s, SD=0.12).
Table.
Participant Demographics
Individuals in the HHA group were not statistically different from those in the LCA group on any of the dependent variables (P>.05). Therefore, these individuals were grouped together (HHA-LCA group) for subsequent comparison with those in the UCA group and with older adults without disability.
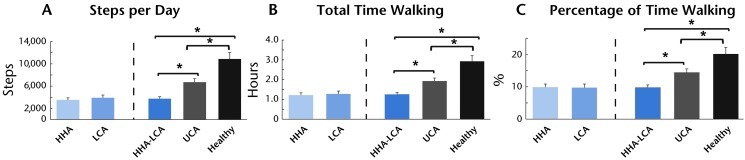
Step Activity
The number of steps per day, total time walking, and percentage of time spent walking per day differed between all groups of individuals poststroke and older adults without disability (Fig. 1; P<.000). Steps per day for the participants in the HHA-LCA group differed from those in the UCA group and older adults without disability and between the UCA group and older adults without disability (Fig. 1; all P<.01). The same differences also were noted in total time spent walking (Fig. 1; all P<.01) and percentage of time spent walking (Fig. 1; all P<.02), with older adults without disability engaging in the greatest amount of step activity.
Figure 1.
Steps per day (A), total time walking (B), and percentage of time walking (C) were not significantly different between participants in the household ambulator (HHA) and limited community ambulator (LCA) groups (left of dashed line). Participants in these groups were combined to form the HHA-LCA group. To the right of the dashed lines, older adults without disability (healthy) were significantly different from all participants poststroke. Individuals poststroke in the HHA-LCA group were significantly different from participants in the unlimited community ambulator (UCA) group. Error bars represent ±1 standard error. Asterisk indicates P<.05 between indicated groups.
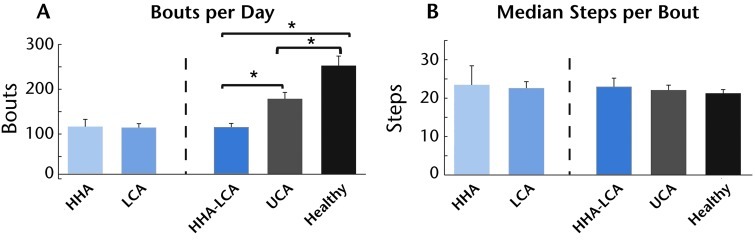
Description of Step Activity
The number of bouts per day differed between all groups of people poststroke and older adults without disability (Fig. 2A; P<.01). Bouts per day for the participants in the HHA-LCA group differed from those in the UCA group and the older adults without disability and between the UCA group and older adults without disability (Fig. 2A; all P<.01). Across all groups, the median number of steps per bout was approximately 22 and no group differences were observed (Fig. 2B; P>.05).
Figure 2.
(A) Bouts per day were not significantly different between participants in the household ambulator (HHA) and limited community ambulator (LCA) groups (left of dashed line). Participants in these groups were combined to form the HHA-LCA group. To the right of the dashed lines, older adults without disability (healthy) were significantly different from all participants poststroke. Individuals poststroke in the HHA-LCA group were significantly different from participants in the unlimited community ambulator (UCA) group. (B) Median steps per bout did not differ across groups. Error bars represent ±1 standard error. Asterisk indicates P<.05 between indicated groups.
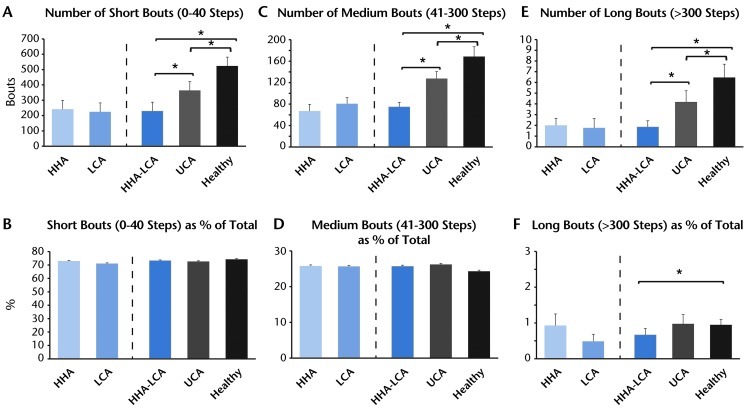
In all participants, the most frequently walked bouts were 40 steps or less (short bouts) (Fig. 3A and 3B), with the lowest number in the HHA-LCA group, greater in the UCA group, and greatest in older adults without disability (Fig. 3A; P<.001). However, when the number of short-distance bouts was expressed as a percentage of the total number of bouts, 72% and 74% of all bouts were in the short-distance range, and this finding did not differ across groups (Fig. 3B; P>.05).
Figure 3.
The frequency of bouts in the (A) short-distance, (C) medium-distance, and (E) long-distance categories for each group and percentage of the total represented by (B) short-distance, (D) medium-distance, and (F) long-distance bouts. To the left of the dashed line in each figure are the results for the household ambulator (HHA) and limited community ambulator (LCA) groups shown separately. To the right of the dashed lines, the bars represent, from left to right, the results for the combined HHA-LCA group, for the unlimited community ambulator (UCA) group, and for older adults without disability (healthy). Error bars represent ±1 standard error. Asterisk indicates P<.05 between indicated groups.
Medium-distance walking bouts were far less common in all groups (Figs. 3C and 3D) and similar to the short-distance walking bouts. The number of medium-distance bouts was lowest in the HHA-LCA group, greater in the UCA group, and highest in older adults without disability (Fig. 3C; P=.001). The participants in the HHA-LCA and UCA groups produced fewer medium-distance walking bouts than older adults without disability (Fig. 2C; P=.001 and P<.05, respectively). Participants in the HHA-LCA group also produced fewer medium-distance walking bouts than those in the UCA group (Fig. 3C; P<.05). When the number of medium-distance bouts was expressed as a percentage of the total number of bouts walked, less than 25% of all walking bouts were in the medium-distance category, and this finding did not differ across groups (Fig. 3D).
The lowest number of bouts walked was in the long-distance range across all of the groups. As was the case for short and medium bouts, the number of long bouts was lowest in the HHA-LCA group, greater in the UCA group, and greatest in older adults without disability (Fig. 3E; P<.001). All participants with stroke had fewer long walking bouts than the participants without disability (Fig. 3E; all P<.01). Those in the HHA-LCA group had fewer long walking bouts than those in the UCA group (Fig. 3E; P<.05). Less than 1% of all walking bouts were long and this percentage differed between the HHA-LCA group and the group without disability (Fig. 3F; P<.05).
Discussion
The results of this study demonstrated, for the first time, that the structure of walking activity was different in people poststroke compared with older adults without disability and that it varied based on functional walking ability as measured by gait speed. The results provide valuable insight into reduced walking activity that would not have been revealed by measuring total steps per day alone. The deficits that were revealed appear to those that could be addressed through appropriate exercise prescription, underscoring the need to analyze specific walking activity behaviors.
The fewer walking bouts per day found in the individuals poststroke who participated in this study agree with findings of Cavanaugh et al,13 who studied walking patterns in older adults and found that older adults without disability used fewer walking bouts per day than younger adults. Despite these overall differences, in both the individuals poststroke and older adults without disability, short bouts of walking made up approximately 75% of all walking bouts. This finding is not entirely unexpected because similar findings have been demonstrated in employed adults without disability.14 It does suggest, however, that steps per bout was not the limiting factor in the amount of step activity performed each day by the individuals poststroke. Rather, it appears that fewer bouts of walking was the primary contributor to fewer overall steps per day.
Long walking bouts also were reduced in all individuals poststroke compared with older adults without disability. Fewer than half of all participants in the HHA-LCA group had even 1 long-distance walking bout during the 3 days. Carvalho et al18 found that individuals poststroke who walked at speeds below 0.8 m/s (as in our HHA and LCA groups) walked an average of 175 m (SD=67) during the Six-Minute Walk Test, which is considerably shorter than the distances required for completing many community-based activities such as grocery shopping.15 It appears, therefore, that participants in the HHA-LCA group may have lacked the physical capacity to walk long distances, which may explain the small number of long bouts observed in this group. In contrast, for individuals with chronic stroke and walking speeds greater than 0.8 m/s (as in our UCA group), the average Six-Minute Walk Test distance was 463 m (SD=84),18 well over that required for long-distance bouts. This finding suggests that individuals whose gait speed indicates they can ambulate in the community without limitation likely retain the basic physical capacity needed for long-distance walking. It is possible, therefore, that issues such as lack of social support or transportation19 played a larger role in the lack of long-distance walking in the UCA group.
This is the first study to report the time spent walking in individuals poststroke compared with older adults without disability. Individuals poststroke spent 10% to 15% of their waking hours performing walking activities, which is less than half of the time spent by older adults. Cavanaugh et al13 reported similar findings in that older adults with functional limitations also spent less time walking than younger adults. The small amount of time spent in ambulatory activities is a serious concern, considering the vicious cycle of disability ↔ inactivity that occurs after stroke4 and its relationship to the development of comorbidities and risk of a second stroke.1
Our conclusions should be considered in light of several limitations of this study. The included participants comprised a sample of convenience for both the adults poststroke and those without disability and as such may have been more motivated than those who did not volunteer to participate. In addition, the participants wore the SAM for 3 consecutive days, and although this amount of time has been shown to produce high reliability,8 it is possible that results would differ if participants wore the SAM for a greater number of days. Finally, although our sample of individuals poststroke included people with rather disparate levels of mobility, there was a larger number of participants whose walking speed indicated they were higher functioning and could ambulate in the community without limitation.
Implications
Analyzing the structure of walking activity provided insight into walking deficits after stroke that would be undetected if only total steps per day were analyzed. The results demonstrate that the fewer number of steps per day after stroke is due to fewer bouts of walking per day. Individuals poststroke not only have a reduced number of long walking bouts, as might be predicted, but they also perform fewer short walking bouts throughout the day. A reduced number of walking bouts at the distances needed to access the community suggests that even those individuals categorized as being unlimited during community ambulation had limitations that could have real implications for their community participation.
The Bottom Line
What do we already know about this topic?
People living with chronic stroke have low levels of daily walking activity.
What new information does this study offer?
This study found that reduced daily walking activity after stroke occurs because of fewer bouts of walking throughout the day. The reduced number of bouts of walking occurred in all walking categories, including short bouts (consistent with walking around the house) and longer bouts (consistent with walking in the community).
If you're a patient, what might these findings mean to you?
Walking activity after stroke can be increased simply by increasing the number of walking bouts both in and around your house each day as well as in your community.
Footnotes
All authors provided concept/idea/research design, writing, and data analysis. Dr Roos provided data collection. Dr Reisman provided project management, fund procurement, and facilities/equipment.
This study was approved by the Human Subjects Review Board at University of Delaware.
A portion of the manuscript was presented at the Combined Sections Meeting of the American Physical Therapy Association; February 9–12, 2011; New Orleans, Louisiana.
This research was supported by National Institutes of Health grant number NR010786.
References
- 1. Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181 [DOI] [PubMed] [Google Scholar]
- 2. Lees KR, Zivin JA, Ashwood T, et al. NXY-059 for acute ischemic stroke. N Engl J Med. 2006;354:588–600 [DOI] [PubMed] [Google Scholar]
- 3. Mayo NE, Wood-Dauphinée S, Cote R, et al. Activity, participation, and quality of life 6 months poststroke. Arch Phys Med Rehabil. 2002;83:1035–1042 [DOI] [PubMed] [Google Scholar]
- 4. Rimmer JH, Wang E. Aerobic exercise training in stroke survivors. Top Stroke Rehabil. 2005;12:17–30 [DOI] [PubMed] [Google Scholar]
- 5. Hornnes N, Larsen K, Boysen G. Little change of modifiable risk factors 1 year after stroke: a pilot study. Int J Stroke. 2010;5:157–162 [DOI] [PubMed] [Google Scholar]
- 6. Macko RF, Ivey FM, Forrester LW, et al. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke: a randomized, controlled trial. Stroke. 2005;36:2206–2211 [DOI] [PubMed] [Google Scholar]
- 7. Michael KM, Allen JK, Macko RF. Reduced ambulatory activity after stroke: the role of balance, gait, and cardiovascular fitness. Arch Phys Med Rehabil. 2005;86:1552–1556 [DOI] [PubMed] [Google Scholar]
- 8. Mudge S, Stott NS. Test-retest reliability of the StepWatch Activity Monitor outputs in individuals with chronic stroke. Clin Rehabil. 2008;22:871–877 [DOI] [PubMed] [Google Scholar]
- 9. Rand D, Eng JJ, Tang PF, et al. Daily physical activity and its contribution to the health-related quality of life of ambulatory individuals with chronic stroke. Health Qual Life Outcomes. 2010;8:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bowden MG, Balasubramanian CK, Behrman AL, Kautz SA. Validation of a speed-based classification system using quantitative measures of walking performance poststroke. Neurorehabil Neural Repair. 2008;22:672–675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Michael KM, Macko RF. Ambulatory activity intensity profiles, fitness, and fatigue in chronic stroke. Top Stroke Rehabil. 2007;14:5–12 [DOI] [PubMed] [Google Scholar]
- 12. Tudor-Locke C, Bassett DR., Jr How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004;34:1–8 [DOI] [PubMed] [Google Scholar]
- 13. Cavanaugh JT, Coleman KL, Gaines JM, et al. Using step activity monitoring to characterize ambulatory activity in community-dwelling older adults. J Am Geriatr Soc. 2007;55:120–124 [DOI] [PubMed] [Google Scholar]
- 14. Orendurff MS, Schoen JA, Bernatz GC, et al. How humans walk: bout duration, steps per bout, and rest duration. J Rehabil Res Dev. 2008;45:1077–1089 [DOI] [PubMed] [Google Scholar]
- 15. Andrews AW, Chinworth SA, Bourassa M, et al. Update on distance and velocity requirements for community ambulation. J Geriatr Phys Ther. 2010;33:128–134 [PubMed] [Google Scholar]
- 16. Chen G, Patten C, Kothari DH, Zajac FE. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture. 2005;22:51–56 [DOI] [PubMed] [Google Scholar]
- 17. Perry J, Garrett M, Gronley JK, Mulroy SJ. Classification of walking handicap in the stroke population. Stroke. 1995;26:982–989 [DOI] [PubMed] [Google Scholar]
- 18. Carvalho C, Sunnerhagen KS, Willen C. Walking speed and distance in different environments of subjects in the later stage post-stroke. Physiother Theory Pract. 2010;26:519–527 [DOI] [PubMed] [Google Scholar]
- 19. Rimmer JH, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. J Rehabil Res Dev. 2008;45:315–322 [DOI] [PubMed] [Google Scholar]