Abstract
Laugier-Hunziker syndrome is a rare acquired disorder characterized by macular hyperpigmentation of the oral and occasionally genital mucosa as well as longitudinal melanonychia. It is considered a benign condition without systemic manifestation or malignant potential. We report on a woman who concomitantly developed Laugier-Hunziker syndrome and a carcinoma of the pancreas.
Key Words: Laugier-Hunziker syndrome, Paraneoplastic disease, Hyperpigmentation, Oral mucosa
Introduction
Laugier-Hunziker syndrome is a rare acquired disorder characterized by macular hyperpigmentation of the oral mucosa and sometimes genital mucosa as well as longitudinal melanonychia. It is considered a benign condition with no systemic manifestation or malignant potential. We report on a woman who concomitantly developed Laugier-Hunziker syndrome and a carcinoma of the pancreas.
Case Report
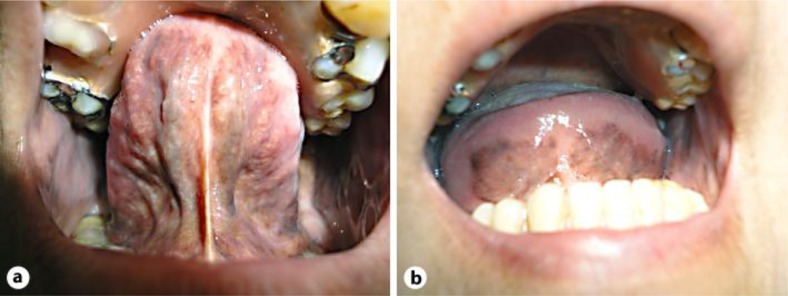
A 61-year-old Caucasian woman presented with a 3-month history of asymptomatic oral and vulvar hyperpigmentation. There was no family history of abnormal pigmentation of the skin or mucosa. Pigmented confluent macules were noted on the buccal mucosa and ventral aspect of the tongue; the lips were not involved (fig. 1a, b). Similar lesions were seen on the vulvar mucosa. Physical examination was otherwise unremarkable.
Fig. 1.
a, b Sharply demarcated macular hyperpigmentation of the tongue.
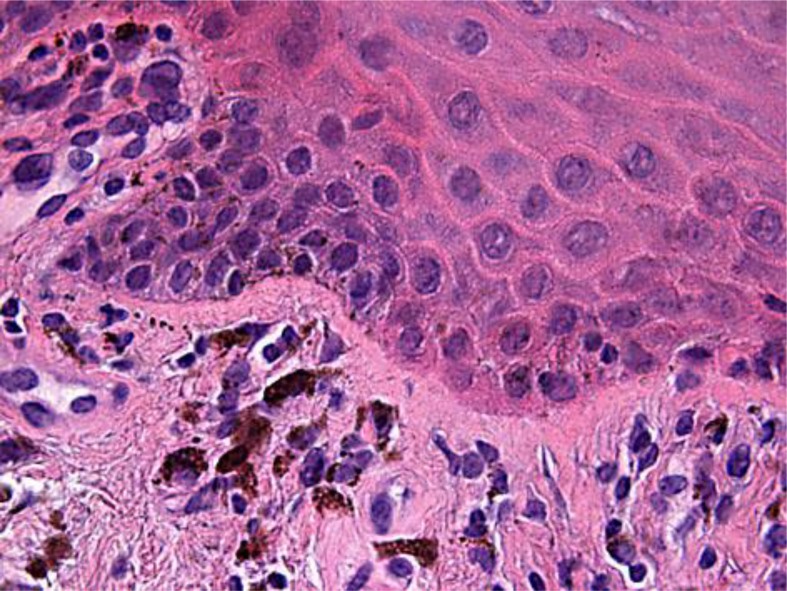
Histologic examination showed increased basal layer pigmentation with a normal number and morphology of melanocytes and numerous melanophages in the papillary dermis (fig. 2). Thus, the diagnosis of Laugier-Hunziker syndrome was established.
Fig. 2.
Hyperpigmentation of the basal cell layer and macrophages in the dermis. HE, ×630.
The patient also mentioned unintended weight loss and nausea since a few months. Recently performed gastroscopy and colonoscopy were unremarkable. A CT scan of the abdomen revealed a carcinoma of the pancreas 2.5 cm in size, infiltrating the gastric wall. Surgical removal was not possible and the patient died 5 months later, after having received chemotherapy.
Discussion
Laugier-Hunziker syndrome was first described in 1970 [1]. It is a rare benign pigmentary disorder characterized by adult-onset oral pigmentation and sometimes similar genital lesions. The pigmentation consists of slate to dark brown, lenticular or linear macules. They can be solitary or confluent, with well-defined or indistinct margins. In addition, the nails can be involved in up to 50% of all patients, usually leading to longitudinal melanonychia (‘Laugier-Hunziker-Baran syndrome’) [2]. Fingernails are more frequently involved than toenails. In the so-called ‘extended’ Laugier-Hunziker syndrome, more widespread areas of pigmentation are seen, for example the fingers and anal mucosa [3]. The most important clinical differential diagnoses are melanoma of the oral mucosa and Peutz-Jeghers syndrome [4]. In this inherited autosomal dominant disease, the pigmentation generally occurs at birth, in infancy or early childhood. The mucosa of the lips is typically also involved and shows small hyperpigmented macules. Additionally, hamartomatous polyps of the bowel with malignant potential are found.
In Laugier-Hunziker syndrome, no systemic manifestations have been described so far. Laugier-Hunziker syndrome was described in a patient with ovarian cancer during polychemotherapy, but this occurrence was considered to be incidental [5]. There is no evidence of genetic transmission or spontaneous resolution. To the best of our knowledge, this is the first case associated with a carcinoma of the pancreas. This association may be fortuitous. However, the onset of the mucosal lesion and the first symptoms of carcinoma, i.e. weight loss and nausea, were contemporaneous. We therefore believe that in Laugier-Hunziker syndrome, the possibility of an underlying malignancy should be considered.
Disclosure Statement
The authors declare that there are no conflicts of interest.
References
- 1.Griffiths WA. Pityriasis rubra pilaris. Clin Exp Dermatol. 1980;5:105–112. doi: 10.1111/j.1365-2230.1980.tb01676.x. [DOI] [PubMed] [Google Scholar]
- 2.Lowell AG, Howard PB. Pityriasis Rubra Pilaris. Fitzpatrick's DERMATOLOGY. :442–444. [Google Scholar]
- 3.Logan WS. Vitamin A and keratinization. Arch Dermatol. 1972;105:748–753. [PubMed] [Google Scholar]
- 4.van Voorst Vader PC. van Oostveen F. Houthoff HJ. Marrink J. Pityriasis rubra pilaris, vitamin A and retinol-binding protein: a case study. Acta Derm Venereol. 1984;64:430–432. [PubMed] [Google Scholar]
- 5.Kellum RE. Possible significance of aqueous emulsified vitamin A in effective therapy for pityriasis rubra pilaris. J Am Acad Dermatol. 1989;20:126–128. doi: 10.1016/s0190-9622(89)80007-6. [DOI] [PubMed] [Google Scholar]