Abstract
Background
A Heat-Health Watch system has been established in England and Wales since 2004 as part of the national heatwave plan following the 2003 European-wide heatwave. One important element of this plan has been the development of a timely mortality surveillance system. This article reports the findings and timeliness of a daily mortality model used to ‘nowcast’ excess mortality (utilising incomplete surveillance data to estimate the number of deaths in near-real time) during a heatwave alert issued by the Met Office for regions in South and East England on 24 June 2011.
Methods
Daily death registrations were corrected for reporting delays with historical data supplied by the General Registry Office. These corrected counts were compared with expected counts from an age-specific linear regression model to ascertain if any excess had occurred during the heatwave.
Results
Excess mortality of 367 deaths was detected across England and Wales in ≥85-year-olds on 26 and 27 June 2011, coinciding with the period of elevated temperature. This excess was localised to the east of England and London. It was detected 3 days after the heatwave.
Conclusion
A daily mortality model was sensitive and timely enough to rapidly detect a small excess, both, at national and regional levels. This tool will be useful when future events of public health significance occur.
Keywords: Heatwave, excess mortality, nowcasting, influenza, mortality, epidemiology
Introduction
The 2003 European-wide heatwave and the resulting substantial excess mortality highlighted the significant impact these sudden events can have upon the general population.1–3 This notable climatic event is predicted to become annual by the 2080s4 due to changes in climate; indeed, the UK has experienced some notably warm summers since 2003, which have been associated with excess morbidity and mortality.5 In response, a Heat-Health Watch system6 was established in 2004 in England and Wales as part of the heatwave plan which operates from 1 June to 15 September each year. Region-specific thresholds have been set for maximum daytime and minimum nighttime temperatures, above which heat could have a significant effect on health (table 1). A threshold breach alerts social and healthcare services which can then work to reduce the potential health impact by targeting specific actions to high-risk groups. In recent seasons, the development of a real-time age group and region-specific excess mortality surveillance system by the Health Protection Agency (HPA) became possible with the creation of the online death registration system by the General Registry Office (GRO) in 2009. Daily death data from this surveillance system has enabled rapid estimation of the mortality impact of public health events such as pandemic influenza and extreme temperature.5 This timely analysis can then be used to help guide and prioritise public health measures and identify vulnerable individuals. Reporting delays between the date of death and date of registration are inherent in the civil death registration process in England and Wales. Therefore, the process of nowcasting, predicting the number of deaths that occurred on a given day by adjusting available data for reporting delays, together with development of a daily surveillance system have been important to provide timely information on the health impact of an event, particularly if it is persisting.7 8
Table 1.
Maximum daily temperature (°C) recorded in the regions of England and Wales during the heatwave alert in June 2011*
| Region | Heat-Health Watch regional heatwave daytime threshold values (°C) | Maximum daily temperature (°C) | |
| 26 June 2011 | 27 June 2011 | ||
| East of England | 30 | 29.0 | 31.9 |
| East Midlands | 30 | 28.1 | 29.8 |
| London | 32 | 28.7 | 31.4 |
| Northeast England | 28 | 23.9 | 22.1 |
| Northwest England | 30 | 25.1 | 27.0 |
| Southeast England | 31 | 28.5 | 31.2 |
| Southwest England | 30 | 27.6 | 24.8 |
| West Midlands | 30 | 27.6 | 28.5 |
| Yorkshire & Humber | 29 | 27.8 | 29.6 |
| Wales | 30 | 26.8 | 23.4 |
The station for each region was chosen to be as representative as possible for each region as a whole. Bold values indicate exceedance of Heat-Health Watch regional threshold temperatures.
Data provided by the Met Office National Climate Information Centre. Please note, this data is provisional and is still subject to quality control measures.
When a risk ≥60% of regional temperatures approaching the predefined Heat Watch thresholds was reached in London, southeast England, the east of England and the East Midlands on 24 June 2011, an alert was issued by the Met Office to inform social and healthcare services.6 This remained until the morning of 28 June 2011. This alert triggered the provision of daily GRO data to the HPA to enable daily estimation of excess mortality. This article outlines the key findings of this new daily mortality surveillance system, detailing if an excess was detected during this time, and how the system performed in near-real time.
Methods
Following the trigger of the heatwave alert on 24 June 2011, a historical dataset of all daily death data in England and Wales back to 17 May 2011 was provided by the GRO to the HPA. To nowcast excess all-cause deaths (defined as observed deaths minus expected deaths), reporting delays between death and registration were accounted for by correcting the number of observed deaths each day. This was particularly important for younger age groups where registration delays can be long.9 Historical daily death data was supplied to the HPA by the Office for National Statistics (ONS) for the summers of 2010 and 2011 to develop an age- and region-specific delay correction factor. The observed delay factor was dependent upon the day of the week of death, age of the deceased and region where the death was reported. The method for how it was calculated is described elsewhere.5
After correcting historical data for delays, the data was used to establish a baseline by fitting an age-specific linear regression model within each region to determine the expected number of deaths, excluding the days on which a heatwave alert was active from the baseline model. Daily data for deaths registered the previous day was further supplied after 24 June 2011 from Monday to Friday for 2 weeks and corrected for delays. Excess deaths during the heatwave period were estimated as observed delay-corrected deaths minus baseline deaths. Estimates of excess for England and Wales, overall, and by region were calculated. 95% CIs were calculated based on the variability in deaths during the non-heatwave period. To determine whether any excess was significant, an upper 3SD limit was added to the baseline. 3SD was used to allow for multiple testing when assessing many age groups, regions and different days. The 2SD upper limit was also calculated to see if excess mortality was close to significance (above 2SD but <3SD). The assessment of excess deaths was repeated daily for each new dataset supplied, with estimates given for deaths occurring up to two working days prior to the date of the dataset provision. Estimates given in this report are those as determined on 7 July 2011 when the final dataset was provided.
Mean and maximum Central England Temperatures (CET)10 were monitored for the duration of the heatwave. Provisional region-specific temperatures were provided by the Met Office National Climate Information Centre post-heatwave.
Results
Temperatures were high on 26 and 27 June 2011, with mean CETs of 20.3°C and 22.0°C and maximum CETs of 26.7°C and 28.0°C, respectively. Regionally, heatwave thresholds were exceeded on Monday 27 June in the east of England, southeast England, and Yorkshire & Humber. No regional thresholds were exceeded on Sunday 26 June (table 1).
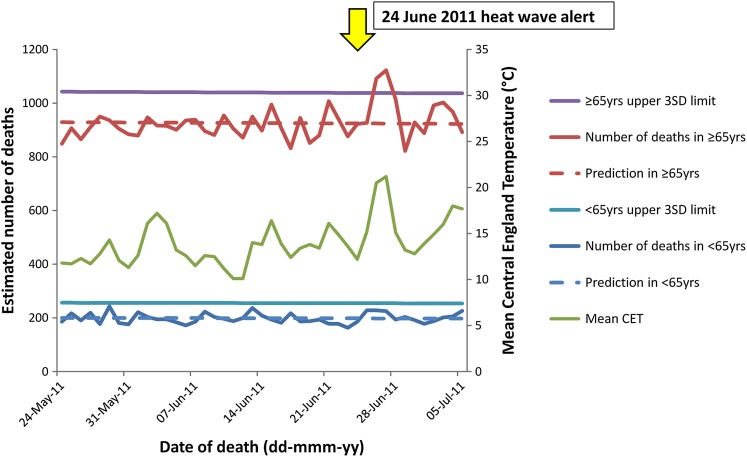
For the period when daily mortality data was available (17 May–5 July 2011), and after correcting the number of observed deaths each day for reporting delays, significant excess mortality (above the 3SD limit) was observed in ≥65-year-olds across England and Wales on 26 and 27 June 2011, coinciding with the peak in mean CET (figure 1). This excess was detected by the daily model on 30 June (3 days later) when the model was run for the first time, once data was available and a baseline had been established. An estimated 367 excess deaths were calculated over this 2-day period. This equates to 16.6% (367/2215) (95% CI 9.7 to 23.4) of deaths in ≥65-year-olds over these 2 days (figure 1). This compares with 299 of 3197 deaths (9.4%, 95% CI 4.5 to 14.2) detected between 30 June and 2 July 2009 during the 2009 heatwave.5
Figure 1.
Delay-corrected observed and predicted number of all-cause deaths in <65-yr-olds and ≥65-yr-olds in England and Wales, and mean Central England Temperature from 24 May to 5 July 2011. The yellow arrow indicates when the heatwave alert was issued by the Met Office. Excess mortality (number of deaths greater than the prediction) is deemed significant if greater than the upper 3SD limit.
When age-group-specific excess was explored in more detail (data not shown), the excess was only significant in ≥85-year-olds over the same time period. Two hundred and twenty-two of 1036 deaths (21.4%, 95% CI 10.4 to 32.4) in this age group were classified as excess.
When region-specific excess mortality was assessed, it was only significant in two regions in ≥65-year-olds: the east of England on 27 June with 32 of 79 deaths excess (40.5%, 95% CI 17.7 to 63.3), and London on 28 June with 39 of 139 (28.1%, 95% CI 10.1 to 46.0). Although a significant excess was not seen in other regions, excess mortality during the heatwave was above a 2SD upper limit in four of the eight remaining regions (northwest England, southwest England, West Midlands and Yorkshire & Humber). No significant excess was detected in any region in <65-year-olds.
Discussion
The UK experienced a heatwave alert in June 2011 which triggered various public health responses. Daily excess mortality reporting was switched on to enable nearreal-time monitoring of the population impact. Despite the alert lasting only four days, and temperature values increasing slightly above thresholds, the surveillance system was sensitive and timely enough to detect significant excess all-cause mortality within a short period (3 days) of the event. The observed excess was not detected in the weekly models run at the HPA over the same time period using the well-established Serfling model and the recently piloted EuroMOMO algorithm (data not shown).11 12
Furthermore, the new daily mortality surveillance system was able to describe which age groups and regions were affected. The observed excess in ≥65-year-olds was primarily attributed to ≥85-year-olds. The elderly are a key risk group susceptible to the effects of heatwaves and so it is not surprising they were affected.1 13 The geographical distribution of observed excess in the east of England and London was consistent with the high regional temperatures observed, and also with heatwave-associated community morbidity indicators at this time determined through the routine monitoring using HPA syndromic surveillance systems.14 Temperatures were notably high in the east of England, and rose above the 30°C regional threshold (maximum temperature of 31.9°C recorded), with 27 June 2011 recorded as the hottest day in the region for 5 years.15 A small delayed excess was seen in London one day after the heatwave, despite temperatures not increasing above the regional threshold of 32°C. While temperature thresholds were breached in southeast England and Yorkshire & Humber, no significant excess was detected in these regions, although excess mortality was above a 2SD upper limit in Yorkshire & Humber, and so, close to significance.
The findings are consistent with the well-described epidemiology of heatwaves.5 Excess mortality detected by the daily model coincided with the period over which an alert was issued, confirming appropriate temperature thresholds set by the national heatwave plan. The provision of daily data by GRO and nowcasting through this system will be useful when future events of public health significance occur and prompt analysis is required, such as heatwaves, pandemic influenza and mass gatherings such as the 2012 London Olympics.
These findings add to the evidence of the rapid effect of short periods of high temperature on sectors of the population. With an increasing elderly population and future climate changes predicted, the importance of timely heatwave public health intervention measures and an associated robust real-time mortality surveillance system is highlighted.
What is already known on this subject.
Heatwaves can have considerable implications on vulnerable sections of the population, and mortality usually rises within 24–48 h of temperature increases.
A timely mortality surveillance system is key to rapidly detect and monitor the impact of heatwaves, which are predicted to increase in frequency with changes in climate.
What this study adds.
Excess deaths were detected during a heatwave alert in England and Wales in June 2011 when temperatures were elevated for a short period, enabling a rapid evaluation of the population health impact.
Despite temperature values increasing only slightly above Heat Watch thresholds, a daily mortality model was sensitive and timely enough to nowcast small levels of excess mortality both in the elderly and in specific regions of England.
Acknowledgments
We are grateful to the Office for National Statistics for supplying historical death data, and the General Registry Office for providing us with the daily mortality data and enabling us to carry out this analysis. We are also grateful to the Met Office National Climate Information Centre for providing us with region-specific temperature data. We would like to thank our colleagues from the Real-time Syndromic Surveillance Team within the HPA for sharing relevant information from their systems, and in particular, to Alex Elliot and Gillian Smith for their review of the manuscript. Additionally, we would like to thank our colleagues, Pia Hardelid for previous model development work, and Virginia Murray, Katie Carmichael and John Watson for their review of the manuscript.
Footnotes
Contributors: RP and NA initiated the study as part of the national heatwave plan in England and Wales. NA and HKG designed the model. HKG collated the data. HKG and NA analysed the data. HKG, NA and RP interpreted the data. HKG, NA and RP drafted the article. HKG, NA, GB and RP revised the article. The guarantor of the article is RP.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Johnson H, Kovats S, McGregor G, et al. The impact of the 2003 heat wave on daily mortality in England and Wales and the use of rapid weekly mortality estimates. Euro Surveill 2005;10:558 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=558 [PubMed] [Google Scholar]
- 2.Robine JM, Cheung SLK, Le Roy S, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biologies 2008;331:171–8 http://www.sciencedirect.com/science/article/pii/S1631069107003770 [DOI] [PubMed] [Google Scholar]
- 3.D'Ippoliti D, Michelozzi P, Marino C, et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health 2010;16:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Health Heatwave Plan For England. 2011. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_127235.pdf (accessed Jul 2011). [Google Scholar]
- 5.Health Protection Agency Chemical Hazards and Poisons report: Rapid estimation of excess mortality in England and Wales during the heatwave of June 30th to July 2nd 2009. 2010. http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1274091561553 (accessed July 2011). [Google Scholar]
- 6.Met Office Heat-Health Watch. http://www.metoffice.gov.uk/weather/uk/heathealth/ (accessed Jul 2011).
- 7.Nicoll A, Ammon A, Amato Gauci A, et al. Experience and lessons from surveillance and studies of the 2009 pandemic in Europe. Public Health 2010;124:14–23 [DOI] [PubMed] [Google Scholar]
- 8.Donker T, van Boven M, van Ballegooijen WM, et al. Nowcasting pandemic influenza A/H1N1 2009 hospitalisations in the Netherlands. Eur J Epidemiol 2011;26:195–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devis T, Rooney C. The time taken to register a death. Popul Trends 1997;88:48–55 [PubMed] [Google Scholar]
- 10.Met Office Hadley Centre Central England Temperature (HadCET) Dataset. http://www.metoffice.gov.uk/hadobs/hadcet/index.html (accessed Jul 2011).
- 11.Serfling RE. Methods for current statistical analysis of excess pneumonia-influenza deaths. Public Health Rep 1963;78:494–506 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1915276/pdf/pubhealthreporig00078-0040.pdf [PMC free article] [PubMed] [Google Scholar]
- 12.EuroMOMO European Monitoring Of Excess Mortality For Public Health Action. http://www.euromomo.eu/ (accessed Jul 2011).
- 13.Rooney C, McMichael AJ, Kovats RS, et al. Excess mortality in England and Wales, and in greater London, during the 1995 heat wave. J Epidemiol Community Health 1988;52:482–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Health Protection Agency Real-Time Syndromic Surveillance. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/RealtimeSyndromicSurveillance/ (accessed Oct 2011).
- 15.BBC Weather UK Review—June 2011. 2011. http://news.bbc.co.uk/weather/hi/uk_reviews/newsid_9531000/9531298.stm (accessed Jul 2011). [Google Scholar]