Abstract
Background
Dental care is the most common unmet health care need for children with chronic conditions. However, anecdotal evidence suggests that not all children with chronic conditions encounter difficulties accessing dental care. The goals of this study are to evaluate dental care use for Medicaid-enrolled children with chronic conditions and to identify the subgroups of children with chronic conditions that are the least likely to use dental care services.
Methods
This study focused on children with chronic conditions ages 3-14 enrolled in the Iowa Medicaid Program in 2005 and 2006. The independent variables were whether a child had each of the following 10 body system-based chronic conditions (no/yes): hematologic; cardiovascular; craniofacial; diabetes; endocrine; digestive; ear/nose/throat; respiratory; catastrophic neurological; or musculoskeletal. The primary outcome measure was use of any dental care in 2006. Secondary outcomes, also measured in 2006, were use of diagnostic dental care, preventive dental care, routine restorative dental care, and complex restorative dental care. We used Poisson regression models to estimate the relative risk (RR) associated with each of the five outcome measures across the 10 chronic conditions.
Results
Across the 10 chronic condition subgroups, unadjusted dental utilization rates ranged from 44.3% (children with catastrophic neurological conditions) to 60.2% (children with musculoskeletal conditions). After adjusting for model covariates, children with catastrophic neurological conditions were significantly less likely to use most types of dental care (RR: 0.48 to 0.73). When there were differences, children with endocrine or craniofacial conditions were less likely to use dental care whereas children with hematologic or digestive conditions were more likely to use dental care. Children with respiratory, musculoskeletal, or ear/nose/throat conditions were more likely to use most types of dental care compared to other children with chronic conditions but without these specific conditions (RR: 1.03 to 1.13; 1.0 to 1.08; 1.02 to 1.12; respectively). There was no difference in use across all types of dental care for children with diabetes or cardiovascular conditions compared to other children with chronic conditions who did not have these particular conditions.
Conclusions
Dental utilization is not homogeneous across chronic condition subgroups. Nearly 42% of children in our study did not use any dental care in 2006. These findings support the development of multilevel clinical interventions that target subgroups of Medicaid-enrolled children with chronic conditions that are most likely to have problems accessing dental care.
Background
The 2011 Institute of Medicine Report Improving Access to Oral Health Care for Vulnerable and Underserved Populations highlights the problems children with chronic conditions have in accessing dental care [1]. Over 20% of children in the U.S. have chronic conditions [2,3]. Based on the definition of children with special health care needs developed by the Maternal and Child Health Bureau, chronic conditions are behavioral, intellectual, developmental, or physical ailments expected to last ≥12 months in ≥75% of patients identified with the condition [4]. Examples of common chronic conditions include uncontrolled asthma, attention deficit and hyperactivity disorder, and cerebral palsy.
Dental caries is the most common disease among all children, including those with chronic conditions [2,5]. As a group, children with chronic conditions are believed to be at increased risk for caries for the following reasons: (1) use of sugar-containing, acidic, or xerostomic medications; (2) frequent exposure to carbohydrates because of dietary needs or oromuscular problems; (3) behavioral co-morbidities that make it difficult for caregivers to brush the child’s teeth regularly with fluoridated toothpaste; and (4) dentists’ unwillingness to treat children with chronic conditions. A comprehensive strategy to ensure optimal oral health for children with chronic conditions includes regular visits to a dentist for preventive care (e.g., examinations; cleanings; topical fluoride; sealants) as well as restorative care (e.g., fillings; stainless steel crowns; extractions) when needed. However, dental care is the most common unmet health care need among children with chronic conditions [2], which has renewed interests in developing strategies aimed at improving dental utilization for medically vulnerable children.
Medicaid is the largest public source of dental care funding for children with chronic conditions in the U.S. [6]. State Medicaid programs are required by the federal Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Program to provide all child enrollees with comprehensive dental care [7]. While Medicaid-enrolled children are more likely to visit a dentist than uninsured children [8,9], studies have documented disparities in dental care use among subgroups of Medicaid-enrolled children [10,11]. A recent publication reported that Medicaid-enrolled children with chronic conditions are slightly more likely to use dental care than Medicaid-enrolled children without chronic conditions [12]. Compared to Medicaid-enrolled children with less complex chronic conditions, those with more complex chronic conditions were less likely to use any dental care [12]. In another study, Medicaid-enrolled children with an intellectual or developmental disability (defined as children with a non-acquired cognitive impairment) were equally as likely to use preventive dental care as Medicaid-enrolled children without an intellectual or developmental disability [13]. Collectively, these studies suggest heterogeneity in dental care use across subgroups of Medicaid-enrolled children with chronic conditions. While this is consistent with anecdotal evidence, there are no empirical studies to support this statement. The lack of data demonstrating heterogeneity in dental use may be one reason why current interventions fail to target children with chronic condition at greatest risk for disparities in dental use. Population-based interventions that target all children with chronic conditions are inefficient and may misallocate scare resources, which can lead to suboptimal outcomes.
In this study, we used 3M Clinical Risk Grouping (CRG) Software, a validated risk adjustment tool [14], to identify Medicaid-enrolled children with chronic conditions. Our goal was to assess dental use across 10 body system-based chronic condition subgroups. This approach is consistent with the specialty-focused medical care system into which most children with chronic conditions are integrated. Based on previous findings that children with chronic conditions have higher levels of unmet dental needs than those without [2], we compared dental care use for children with chronic conditions across each of the following chronic condition subgroups: hematologic; cardiovascular; craniofacial; diabetes; endocrine; digestive; ear/nose/throat; respiratory; catastrophic neurological; and musculoskeletal. The knowledge generated from this study will help us to identify the subgroups of children with chronic conditions who are at greatest risk for disparities in dental care use and to develop future interventions aimed at ensuring that these children have optimal access to dental care.
Methods
Study design
This was a retrospective study based on enrollment and claims data from the Iowa Medicaid Program (2003-2006). We received approvals from the University of Washington and the University of Iowa Institutional Review Boards.
Conceptual model
The study was based on a sociocultural oral health disparities model presented by Patrick and colleagues [15]. Model covariates were organized into five domains:
· Ascribed factors (immutable individual-level determinants);
· Proximal factors (modifiable individual-level health behaviors);
· Immediate factors (household-level mediators between proximal and intermediate factors);
· Intermediate factors (community-level factors); and
· Distal factors (system-level factors).
Study subjects
We focused on children with chronic conditions ages 3-14 years who were enrolled in the Iowa Medicaid Program for ≥11 months in 2005 and in 2006. Children under age 3 were excluded because chronic conditions are typically not diagnosed until the child’s third birthday [16]. We also excluded children ≥15 years of age because the determinants of dental use for older adolescents are different from younger children [17].
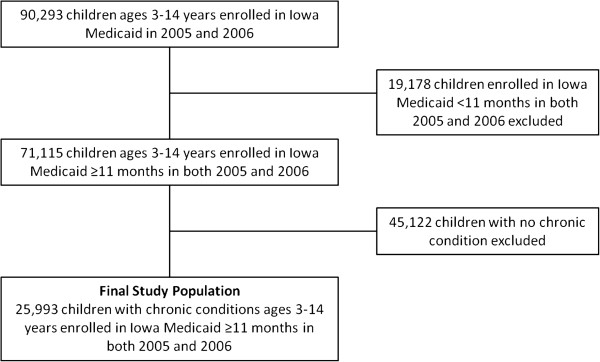
Children with chronic conditions were identified by applying the 3M Clinical Risk Grouping (CRG) Software to each child’s medical claims data from 2003-2005 (Wallingford, CT) [18]. The CRG algorithm uses diagnostic codes (International Classification of Disease–Version Nine–Clinical Modification [ICD-9-CM]) and health service utilization codes (Current Procedural Terminology [CPT]) to classify each child into one of nine mutually exclusive Core Health Status Groups (CHSGs) [4]. We excluded children in CHSGs 1 (healthy children) or 2 (children with an acute condition) and focused on children in CHSGs 3 (minor chronic condition) through 9 (catastrophic chronic condition). The final study population consisted of 25,993 Iowa Medicaid-enrolled children with chronic conditions ages 3-14 years (Figure 1).
Figure 1.
Flowchart on how final study population was derived.
Main exposure variables
The CRG Software also uses ICD-9-CM codes to classify each child into non-mutually exclusive body system-based Medical Diagnostic Categories (MDC). The diagnoses under each MDC correspond to a single organ system and are aligned with the delivery of specialty pediatric medical care [19]. We selected 10 MDCs most relevant for oral health: hematologic (MDC-161); cardiovascular (MDC-51); craniofacial (MDC-32); diabetes (MDC-101); digestive (MDC-61); endocrine (MDC-102); ear/nose/throat (MDC-31); respiratory (MDC-41); catastrophic neurological (MDC-12); and musculoskeletal (MDC-81). Each child with a chronic condition was classified as “no” or “yes” to indicate whether they were classified into each of the 10 MDCs.
Outcome measure
The primary outcome measure was use of any dental care in 2006 (no/yes) [20]. Dental services were identified from encounter files using Current Dental Terminology (CDT) codes, which are five-digit alphanumeric codes used for billing. Secondary outcome measures included use of diagnostic care (e.g., examinations; D0110-D0330), preventive care (e.g., cleanings; topical fluoride treatment; sealants; D1110-D1351; D4355), routine restorative care (e.g., fillings; D2110-D2394), or complex restorative care (e.g., pulp therapy; stainless steel crowns; extraction; D1510-D1550; D2930-4342; D7110-D7140; D9420).
Model covariates
Based on Patrick’s model [15], we considered the following 10 variables (organized into five domains) for inclusion in our models, measured in 2005.
Ascribed factors: age (three categories based on the child’s dentition: 3-7 [primary and early mixed dentition]; 8-12 [mixed dentition]; 13-14 [early permanent dentition] years); sex (male/female); race/ethnicity (White, Black, other, missing/unknown); and chronic condition severity (using previously validated methods [14], the seven CHSGs were reorganized into a four-category hierarchical, mutually exclusive variable referred to as modified CHSGs: episodic chronic condition; life-long chronic condition; malignancy; or catastrophic chronic condition).
Proximal factors: use of preventive medical care in 2005 (no/yes); previous use of any dental care in 2005 (no/yes).
Immediate factors: whether the child had any Medicaid-enrolled siblings (no/yes) or adults in the household (no/yes).
Intermediate factor: rurality (a four-category variable [13] based on the 2003 USDA Rural-Urban Continuum Codes and the child’s county of residence: metropolitan; urban adjacent to metropolitan; urban non-adjacent to metropolitan; rural).
Distal factor: whether the child lived in a dental Health Professional Shortage Area based on the child’s residential zip code (no/yes).
Statistical analyses
After generating descriptive statistics, we used the Pearson chi-square test (α = 0.05) to test the bivariate relationships between model covariates and (1) the 10 chronic condition subgroups and (2) the five outcome measures. Next, we assessed for collinearity between the rurality and dental HPSA variables. There was no evidence of collinearity and both variables were included in the models. Then we constructed five Poisson regression models (use of any dental care, diagnostic care, preventive care, routine restorative care, and complex restorative care) for each of the 10 chronic condition subgroups. We reported covariate-adjusted relative risk ratios and estimated 95% confidence intervals using robust general estimating equation estimators of variance [21]. We tested for a statistical interaction between the two immediate factors (whether the child had a Medicaid-enrolled sibling or adult in the household) and included the interaction term in the regression model only if it was statistically significant. To address the problem of high correlation between use of any dental care in 2005 and the outcome measures, we dropped this variable from the final regression models. We analyzed the data using SPSS Version 19.0 for Windows.
Results
Descriptive statistics
The mean age for children in the study was 8.9 ± 3.4 years (data not shown). About 40% of children were female (Table 1). Over 70% were White; 9.1% were Black; 7.5% were another race or ethnicity; and 13.2% had missing/unknown race or ethnicity data. In regards to chronic condition severity 69.3% had episodic chronic conditions; 28.2% had life-long chronic conditions; 0.3% had a malignancy; and 2.2% had catastrophic chronic conditions. Nearly 90% of children utilized preventive medical care in 2005. About 67.1% had a Medicaid-enrolled sibling and 55.5% had an adult in their household enrolled in Medicaid. Most children lived in a metropolitan area (55.2%) and 65.8% lived in a dental HPSA.
Table 1.
Medicaid-enrolled children (N = 25,993) by chronic condition subgroup
|
All children with a chronic condition N = 25,993 |
Respiratory condition subgroup | Ear/nose/throat condition subgroup | Digestive condition subgroup | Musculoskeletal condition subgroup | Endocrine condition subgroup | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| |
|
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
| |
|
n = 4,415 |
n = 21,578 |
n = 6,965 |
n = 19,028 |
n = 14,759 |
n = 11,234 |
n = 14,757 |
n = 11,236 |
n = 20,429 |
n = 5,564 |
| |
|
(17.0) |
(83.0) |
(26.8) |
(73.2) |
(56.8) |
(43.2) |
(56.8) |
(43.2) |
(78.6) |
(21.4) |
| Ascribed factors |
|
|
|
|
|
|
|
|
|
|
|
| Age (years) |
|
|
|
|
|
|
|
|
|
|
|
| 3-7 |
9,644 (37.1) |
732 (16.6) |
8,912 (41.3)* |
413 (5.9) |
9,231 (48.5)* |
4,655 (31.5) |
4,989 (44.4)* |
6,060 (41.1) |
3,584 (31.9)* |
7,075 (34.6) |
2,569 (46.2)* |
| 8-12 |
11,321 (43.6) |
2,452 (55.5) |
8,869 (41.1) |
4,305 (61.8) |
7,016 (36.9) |
6,982 (47.2) |
4,339 (38.6) |
6,542 (44.3) |
4,779 (42.5) |
9.248 (45.3) |
2,073 (37.3) |
| 13-14 |
5,028 (19.3) |
1,231 (27.9) |
3,797 (17.6) |
2,247 (32.3) |
2,781 (14.6) |
3,122 (21.2) |
1,906 (17.0) |
2,155 (14.6) |
2,873 (25.6) |
4,106 (20.1) |
922 (16.6) |
| Sex |
|
|
|
|
|
|
|
|
|
|
|
| Female |
10,434 (40.1) |
1,461 (33.1) |
8,973 (41.6)* |
2,502 (35.9) |
7,932 (41.7)* |
5,604 (38.0) |
4,830 (43.0)* |
5,627 (38.1) |
4,807 (42.8)* |
8,102 (39.7) |
2,332 (41.9) † |
| Race/ethnicity |
|
|
|
|
|
|
|
|
|
|
|
| White |
18,255 (70.2) |
2,998 (67.9) |
15,257 (70.7)* |
4,892 (70.2) |
13,363 (70.2)* |
10,278 (69.6) |
7,977 (71.0)* |
9,916 (67.2) |
8,336 (74.2)* |
14,373 (70.4) |
3,882 (69.8)* |
| Black |
2,372 (9.1) |
428 (9.7) |
1,944 (9.0) |
769 (11.0) |
1,603 (8.4) |
1,438 (9.7) |
934 (8.3) |
1,543 (10.5) |
829 (7.4) |
1,944 (9.5) |
428 (7.7) |
| Other |
1,944 (7.5) |
263 (6.0) |
1,681 (7.8) |
411 (5.9) |
1,533 (8.1) |
1,058 (7.2) |
886 (7.9) |
1,203 (8.2) |
741 (6.6) |
1,529 (7.5) |
415 (7.5) |
| Missing/Unknown |
3,422 (13.2) |
726 (16.4) |
2,696 (12.5) |
893 (12.8) |
2,529 (13.3) |
1,985 (13.4) |
1,437 (12.8) |
2,092 (14.2) |
1,330 (11.8) |
2,583 (12.6) |
839 (15.1) |
| Chronic condition severity |
|
|
|
|
|
|
|
|
|
|
|
| Episodic |
18,025 (69.3) |
2,936 (66.5) |
15,089 (69.9)* |
4,784 (68.7) |
13,241 (69.6) |
10,891 (73.8) |
7,134 (63.5)* |
10,706 (72.5) |
7,319 (65.1)* |
15,231 (74.6) |
2,794 (50.2)* |
| Life-Long |
7,324 (28.2) |
1,352 (30.6) |
5,972 (27.7) |
2,020 (29.0) |
5,304 (27.9) |
3,672 (24.9) |
3,652 (32.5) |
3,881 (26.3) |
3,443 (30.6) |
4,896 (24.0) |
2,428 (43.6) |
| Malignancy |
85 (0.3) |
18 (0.4) |
67 (0.3) |
16 (0.2) |
69 (0.4) |
27 (0.2) |
58 (0.5) |
41 (0.3) |
44 (0.4) |
36 (0.2) |
49 (0.9) |
| Catastrophic |
559 (2.2) |
109 (2.5) |
450 (2.1) |
145 (2.1) |
414 (2.2) |
169 (1.1) |
390 (3.5) |
129 (0.9) |
430 (3.8) |
266 (1.3) |
293 (5.3) |
| Proximal factors |
|
|
|
|
|
|
|
|
|
|
|
| Child used preventive medical care in 2005 |
23,080 (88.8) |
3,317 (75.1) |
19,763 (91.6)* |
5,562 (79.9) |
17,518 (92.1)* |
12,583 (85.3) |
10,497 (93.4)* |
12,722 (86.2) |
10,358 (92.2)* |
17,875 (87.5) |
5,205 (93.5)* |
| Child used any dental care in 2005 |
15,398 (59.2) |
2,456 (55.6) |
12,942 (60.0)* |
4,039 (58.0) |
11,359 (59.7) ‡ |
8,605 (58.3) |
6,793 (60.5)* |
8,449 (57.3) |
6,949 (61.8)* |
12,217 (59.8) |
3,181 (57.2)* |
| Immediate factors |
|
|
|
|
|
|
|
|
|
|
|
| Child had at least one Medicaid- enrolled sibling |
17,449 (67.1) |
2,799 (63.4) |
14,650 (67.9)* |
4,625 (66.4) |
12,824 (67.4) |
10,287 (69.7) |
7,162 (63.8)* |
10,077 (68.3) |
7,372 (65.6)* |
14,286 (69.9) |
3,163 (56.8)* |
| Child had at least one Medicaid- enrolled adult |
14,436 (55.5) |
1,841 (41.7) |
12,595 (58.4)* |
3,377 (48.5) |
11,059 (58.1)* |
7,879 (53.4) |
6,557 (58.4)* |
7,999 (54.2) |
6,437 (57.3)* |
11,604 (56.8) |
2,832 (50.9)* |
| Immediate factor |
|
|
|
|
|
|
|
|
|
|
|
| Rurality |
|
|
|
|
|
|
|
|
|
|
|
| Metropolitan |
14,353 (55.2) |
2,653 (60.1) |
11,700 (54.2)* |
4,071 (58.4) |
10,282 (54.0)* |
8,261 (56.0) |
6,092 (54.2) ‡ |
8,391 (56.9) |
5,962 (53.1)* |
11,327 (55.4) |
3,026 (54.4) |
| Urban adjacent to metropolitan |
4,978 (19.2) |
812 (18.4) |
4,166 (19.3) |
1,304 (18.7) |
3,674 (19.3) |
2,765 (18.7) |
2,213 (19.7) |
2,716 (18.4) |
2,262 (20.1) |
3,883 (19.0) |
1,095 (19.7) |
| Urban non-adjacent to metropolitan |
5,237 (20.1) |
730 (16.5) |
4,507 (20.9) |
1,239 (17.8) |
3,998 (21.0) |
2,917 (19.8) |
2,320 (20.7) |
2,870 (19.4) |
2,367 (21.1) |
4,091 (20.0) |
1,146 (20.6) |
| Rural |
1,425 (5.5) |
220 (5.0) |
1,205 (5.6) |
351 (5.0) |
1,074 (5.6) |
816 (5.5) |
609 (5.4) |
780 (5.3) |
645 (5.7) |
1,128 (5.5) |
297 (5.3) |
| Distal factor |
|
|
|
|
|
|
|
|
|
|
|
| Child lived in a dental Health Professional Shortage Area | 17,110 (65.8) | 2,876 (65.1) | 14,234 (66.0) | 4,616 (66.3) | 12,494 (65.7) | 9,753 (66.1) | 7,357 (65.5) | 9,798 (66.4) | 7,312 (65.1) ‡ | 13,555 (66.4) | 3,555 (63.9) † |
Pearson Chi Square test to evaluate bivariate relationship between model covariates and each chronic condition.
* p < .0001.
† p < .01.
‡ p < .05.
The proportions of children in the non-mutually exclusive chronic condition subgroups, in descending order, are as follows: respiratory (83.0%); ear/nose/throat (73.2%); digestive (43.2%); musculoskeletal (43.2%); endocrine (21.4%); cardiovascular (10.2%); hematologic (6.4%); catastrophic neurological (2.5%); craniofacial (1.8%); and diabetes (1.4%) (Tables 1 and 2).
Table 2.
Medicaid-enrolled children (N = 25,993) by chronic condition subgroup
| Cardiovascular condition subgroup | Hematologic condition subgroup | Catastrophic neurological condition subgroup | Craniofacial condition subgroup | Diabetes subgroup | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
| |
n = 23,340 |
n = 2,653 |
n = 24,325 |
n = 1,668 |
n = 25,356 |
n = 637 |
n = 25,517 |
n = 476 |
n = 25,642 |
n = 351 |
| |
(89.8) |
(10.2) |
(93.6) |
(6.4) |
(97.5) |
(2.5) |
(98.2) |
(1.8) |
(98.6) |
(1.4) |
| Ascribed factors |
|
|
|
|
|
|
|
|
|
|
| Age (years) |
|
|
|
|
|
|
|
|
|
|
| 3-7 |
8,651 (37.1) |
993 (37.4)* |
8,719 (35.8) |
925 (55.5)* |
9,388 (37.0) |
256 (40.2) |
9,383 (36.8) |
261 (54.8)* |
9.545 (37.2) |
99 (28.2)* |
| 8-12 |
10,262 (44.0) |
1,059 (39.9) |
10,829 (44.5) |
492 (29.5) |
11,069 (43.7) |
252 (39.6) |
11,172 (43.8) |
149 (31.3) |
11,174 (43.6) |
147 (41.9) |
| 13-14 |
4,427 (19.0) |
601 (22.7) |
4,777 (19.6) |
251 (15.0) |
4,899 (19.3) |
129 (20.3) |
4,962 (19.4) |
66 (13.9) |
4,923 (19.2) |
105 (29.9) |
| Sex |
|
|
|
|
|
|
|
|
|
|
| Female |
9,353 (40.1) |
1,081 (40.7) |
9,757 (40.1) |
677 (40.6) |
10,158 (40.1) |
276 (43.3) |
10,250 (40.2) |
184 (38.7) |
10,264 (40.0) |
170 (48.4)‡ |
| Race/ethnicity |
|
|
|
|
|
|
|
|
|
|
| White |
16,393 (70.2) |
1,862 (70.2) |
17,191 (70.7) |
1,064 (63.8)* |
17,790 (70.2) |
465 (73.0)* |
17,928 (70.3) |
327 (68.7)* |
18,002 (70.2) |
253 (72.1) |
| Black |
2,133 (9.1) |
239 (9.0) |
2,181 (9.0) |
191 (11.5) |
2,356 (9.3) |
16 (2.5) |
2,347 (9.2) |
25 (5.3) |
2,338 (9.1) |
34 (9.7) |
| Other |
1,724 (7.4) |
220 (8.3) |
1,783 (7.3) |
161 (9.7) |
1,913 (7.5) |
31 (4.9) |
1,913 (7.5) |
31 (6.5) |
1,924 (7.5) |
20 (5.7) |
| Missing/Unknown |
3,090 (13.2) |
332 (12.5) |
3,170 (13.0) |
252 (15.1) |
3,297 (13.0) |
125 (19.6) |
3,329 (13.0) |
93 (19.5) |
3,378 (13.2) |
44 (12.5) |
| Chronic condition severity |
|
|
|
|
|
|
|
|
|
|
| Episodic |
16,720 (71.6) |
1,305 (49.2)* |
17,052 (70.1) |
973 (58.3)* |
17,981 (70.9) |
44 (6.9)* |
17,810 (69.8) |
215 (45.2)* |
17,957 (70.0) |
68 (19.4)* |
| Life-Long |
6,124 (26.2) |
1,200 (45.2) |
6,728 (27.7) |
596 (35.7) |
7,180 (28.3) |
144 (22.6) |
7,082 (27.8) |
242 (50.8) |
7,066 (27.6) |
258 (73.5) |
| Malignancy |
58 (0.2) |
27 (1.0) |
48 (0.2) |
37 (2.2) |
84 (0.3) |
1 (0.2) |
85 (0.3) |
0 (0.0) |
83 (0.3) |
2 (0.6) |
| Catastrophic |
438 (1.9) |
121 (4.6) |
497 (2.0) |
62 (3.7) |
111 (0.4) |
448 (70.3) |
540 (2.1) |
19 (4.0) |
536 (2.1) |
23 (6.6) |
| Proximal factors |
|
|
|
|
|
|
|
|
|
|
| Child used preventive medical care in 2005 |
20,602 (88.3) |
2,478 (93.4)* |
21,480 (88.3) |
1,600 (95.9)* |
22,471 (88.6) |
609 (95.6)* |
22,631 (88.7) |
449 (94.3)* |
22,751 (88.7) |
329 (93.7)‡ |
| Immediate factors |
|
|
|
|
|
|
|
|
|
|
| Child had at least one Medicaid-enrolled sibling |
15,857 (67.9) |
1,592 (60.0)* |
16,401 (67.4) |
1,048 (62.8)* |
17,326 (68.3) |
123 (19.3)* |
17,200 (67.4) |
249 (52.3)* |
17,214 (67.1) |
235 (67.0) |
| Child had at least one Medicaid-enrolled adult |
13,016 (55.8) |
1,420 (53.5) ‡ |
13,457 (55.3) |
979 (58.7)† |
14,330 (56.5) |
106 (16.6)* |
14,228 (55.8) |
208 (43.7)* |
14,235 (55.5) |
201 (57.3) |
| Immediate factor |
|
|
|
|
|
|
|
|
|
|
| Rurality |
|
|
|
|
|
|
|
|
|
|
| Metropolitan |
12,871 (55.1) |
1,482 (55.9) |
13,431 (55.2) |
922 (55.3) |
13,962 (55.1) |
391 (61.4)‡ |
14,095 (55.2) |
258 (54.2) |
14,170 (55.3) |
183 (52.1) |
| Urban adjacent to metropolitan |
4,486 (19.2) |
492 (18.5) |
4,673 (19.2) |
305 (18.3) |
4,873 (19.2) |
105 (16.5) |
4,891 (19.2) |
87 (18.3) |
4,898 (19.1) |
80 (22.8) |
| Urban non-adjacent to metropolitan |
4,707 (20.2) |
530 (20.0) |
4,901 (20.1) |
336 (20.1) |
5,122 (20.2) |
115 (18.1) |
5,134 (20.1) |
103 (21.6) |
5,171 (20.2) |
66 (18.8) |
| Rural |
1,276 (5.5) |
149 (5.6) |
1,320 (5.4) |
105 (6.3) |
1,399 (5.5) |
26 (4.1) |
1,397 (5.5) |
28 (5.9) |
1,403 (5.5) |
22 (6.3) |
| Distal factor |
|
|
|
|
|
|
|
|
|
|
| Child lived in a dental Health Professional Shortage Area | 15,351 (65.8) | 1,759 (66.3) | 16,023 (65.9) | 1,087 (65.2) | 16,768 (66.1) | 342 (53.7)* | 16,809 (65.9) | 301 (63.2) | 16,879 (65.8) | 231 (65.8) |
Pearson Chi Square test to evaluate bivariate relationship between model covariates and each chronic condition.
* p < .0001.
† p < .01.
‡ p < .05.
Bivariate statistics
The bivariate relationships between model covariates and exposure variables (each of the 10 chronic condition subgroups) are summarized in Tables 1 and 2. Even though most children were male, when there were statistically significant differences, larger proportions of children across the chronic condition subgroups were female. Across every subgroup, significantly larger proportions of children with the chronic condition utilized preventive medical care in 2005 than children without the specific chronic condition. There were no other consistent findings.
The bivariate relationships between model covariates and the primary outcome variable (any dental care use in 2006) as well as the secondary outcome measures (use of diagnostic, preventive, routine restorative, or complex restorative dental care) are summarized in Table 3. Significantly larger proportions of children who utilized each type of dental care were White. In addition, significantly larger proportions of children who utilized preventive medical care in 2005 subsequently utilized all types of dental care in 2006.
Table 3.
Relationships between covariates and dental utilization outcome measures
| Any dental care use in 2006 | Diagnostic dental care use in 2006 | Preventive dental care use in 2006 | Routine restorative dental care use in 2006 | Complex restorative dental care use in 2006 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
No |
Yes |
| |
n = 10,846 (41.7) |
n = 15,147 (58.3) |
n = 11,772 (45.3) |
n = 14,221 (54.7) |
n = 13,119 (50.5) |
n = 12,874 (49.5) |
n = 21,116 (81.2) |
n = 4,877 (18.8) |
n = 23,637 (90.9) |
n = 2,356 (9.1) |
| Main predictor variables (chronic condition subgroups) |
|
|
|
|
|
|
|
|
|
|
| Respiratory condition |
|
|
|
|
|
|
|
|
|
|
| No |
2,017 (18.6) |
2,398 (15.8)* |
2,227 (18.9) |
2,188 (15.4)* |
2,427 (18.5) |
1,988 (15.4)* |
3,656 (17.3) |
759 (15.6)† |
4,078 (17.3) |
337 (14.3)* |
| Yes |
8,829 (81.4) |
12,749 (84.2) |
9,545 (81.1) |
12,033 (84.6) |
10,692 (81.5) |
10,886 (84.6) |
17,460 (82.7) |
4,118 (84.4) |
19,559 (82.7) |
2,019 (85.7) |
| Ear/nose/throat chronic condition |
|
|
|
|
|
|
|
|
|
|
| No |
3,025 (27.9) |
3,940 (26.0)‡ |
3,336 (28.3) |
3,629 (25.5)* |
3,751 (28.6) |
3,214 (25.0)* |
5,650 (26.8) |
1,315 (27.0) |
6,433 (27.2) |
532 (22.6)* |
| Yes |
7,821 (72.1) |
11,207 (74.0) |
8,436 (71.7) |
10,592 (74.5) |
9,368 (71.4) |
9,660 (75.0) |
15,466 (73.2) |
3,562 (73.0) |
17,204 (72.8) |
1,824 (77.4) |
| Digestive condition |
|
|
|
|
|
|
|
|
|
|
| No |
6,286 (58.0) |
8,473 (55.9)† |
6,842 (58.1) |
7,917 (55.7)* |
7,555 (57.6) |
7,204 (56.0)‡ |
11,937 (56.5) |
2,822 (57.9) |
13,469 (57.0) |
1,290 (54.8)‡ |
| Yes |
4,560 (42.0) |
6,674 (44.1) |
4,930 (41.9) |
6,304 (44.3) |
5,564 (42.4) |
5,670 (44.0) |
9,179 (43.5) |
2,055 (42.1) |
10,168 (43.0) |
1,066 (45.2) |
| Musculoskeletal condition |
|
|
|
|
|
|
|
|
|
|
| No |
6,373 (58.8) |
8,384 (55.4)* |
6,891 (58.5) |
7,866 (55.3)* |
7,532 (57.4) |
7,225 (56.1)‡ |
12,102 (57.3) |
2,655 (54.4)* |
13,438 (56.9) |
1,319 (56.0) |
| Yes |
4,473 (41.2) |
6,763 (44.6) |
4,881 (41.5) |
6,355 (44.7) |
5,587 (42.6) |
5,649 (43.9) |
9,014 (42.7) |
2,222 (45.6) |
10,199 (43.1) |
1,037 (44.0) |
| Endocrine condition |
|
|
|
|
|
|
|
|
|
|
| No |
8,508 (78.4) |
11,921 (78.7) |
9,249 (78.6) |
11,180 (78.6) |
10,272 (78.3) |
10,157 (78.9) |
16,408 (77.7) |
4,021 (82.4)* |
18,559 (78.5) |
1,870 (79.4) |
| Yes |
2,338 (21.6) |
3,226 (21.3) |
2,523 (21.4) |
3,041 (21.4) |
2,847 (21.7) |
2,717 (21.1) |
4,708 (22.3) |
856 (17.6) |
5,078 (21.5) |
486 (20.6) |
| Cardiovascular condition |
|
|
|
|
|
|
|
|
|
|
| No |
9,743 (89.8) |
13,597 (89.8) |
10,586 (89.9) |
12,754 (89.7) |
11,747 (89.5) |
11,593 (90.0) |
18,938 (89.7) |
4,402 (90.3) |
21,242 (89.9) |
2,098 (89.0) |
| Yes |
1,103 (10.2) |
1,550 (10.2) |
1,186 (10.1) |
1,467 (10.3) |
1,372 (10.5) |
1,281 (10.0) |
2,178 (10.3) |
475 (9.7) |
2,395 (10.1) |
258 (11.0) |
| Hematologic condition |
|
|
|
|
|
|
|
|
|
|
| No |
10,182 (93.9) |
14,143 (93.4) |
11,047 (93.8) |
13,278 (93.4) |
12,307 (93.8) |
12,018 (93.4) |
19,746 (93.5) |
4,579 (93.9) |
22,101 (93.5) |
2,224 (94.4) |
| Yes |
664 (6.1) |
1,004 (6.6) |
725 (6.2) |
943 (6.6) |
812 (6.2) |
856 (6.6) |
1,370 (6.5) |
298 (6.1) |
1,536 (6.5) |
132 (5.6) |
| Catastrophic neurological condition |
|
|
|
|
|
|
|
|
|
|
| No |
10,491 (96.7) |
14,865 (98.1)* |
11,386 (96.7) |
13,970 (98.2)* |
12,721 (97.0) |
12,635 (98.1)* |
20,527 (97.2) |
4,829 (99.0)* |
23,054 (97.5) |
2,302 (97.7) |
| Yes |
355 (3.3) |
282 (1.9) |
386 (3.3) |
251 (1.8) |
398 (3.0) |
239 (1.9) |
589 (2.8) |
48 (1.0) |
583 (2.5) |
54 (2.3) |
| Craniofacial condition |
|
|
|
|
|
|
|
|
|
|
| No |
10,648 (98.2) |
14, 865 (98.1)* |
11,386 (96.7) |
13,964 (98.2) |
12,864 (98.1) |
12,653 (98.3) |
20,703 (98.0) |
4,814 (98.7)‡ |
23,198 (98.1) |
2,319 (98.4) |
| Yes |
198 (1.8) |
282 (1.9) |
386 (3.3) |
257 (1.8) |
255 (1.9) |
221 (1.7) |
413 (2.0) |
63 (1.3) |
439 (1.9) |
37 (1.6) |
| Diabetes |
|
|
|
|
|
|
|
|
|
|
| No |
10,690 (98.6) |
14,952 (98.7) |
11,603 (98.6) |
14,039 (98.7) |
12,933 (98.6) |
12,709 (98.7) |
20,822 (98.6) |
4,820 (98.8) |
23,207 (98.6) |
2,335 (99.1)‡ |
| Yes |
156 (1.4) |
195 (1.3) |
169 (1.4) |
182 (1.3) |
186 (1.4) |
165 (1.3) |
294 (1.4) |
57 (1.2) |
330 (1.4) |
21 (0.9) |
| Ascribed factors |
|
|
|
|
|
|
|
|
|
|
| Age (years) |
|
|
|
|
|
|
|
|
|
|
| 3–7 |
4,023 (37.1) |
5,621 (37.1) |
4,287 (36.4) |
5,357 (37.7)* |
4,588 (35.0) |
5,056 (39.3)* |
7,969 (37.7) |
1,675 (34.3)* |
8,659 (36.6) |
985 (41.8)* |
| 8–12 |
4,60 2(42.4) |
6,719 (44.4) |
5,042 (42.8) |
6,279 (44.2) |
5,424 (41.3) |
5,897 (45.8) |
9,208 (43.8) |
2,113 (43.3) |
10,218 (43.2) |
1.103(46.8) |
| 13–14 |
2,221 (20.5) |
2,807(18.5) |
2,443 (20.8) |
2,585 (18.12) |
3,107 (23.7) |
1,921 (14.9) |
3,939 (18.7) |
1,089 (22.3) |
4,760 (20.1) |
268 (11.4) |
| Sex |
|
|
|
|
|
|
|
|
|
|
| Female |
4,178 (38.5) |
6,256 (41.3)* |
4,544 (38.6) |
5,890 (41.4)* |
5,147 (39.2) |
5,287(41.1)^ |
8,436 (40.0) |
1,998 (41.0) |
9,483 (40 1) |
951 (40.4) |
| Race/ethnicity |
|
|
|
|
|
|
|
|
|
|
| White |
7,400(68.2) |
10.855 (71.7)* |
8,069 (68.5) |
10,186 (71.6)* |
9,099 (69.4) |
9,156 (71.1) |
14,696(69.8) |
3,559 (73.0)* |
16,539 (70.0) |
1.716 (72.8)* |
| Black |
1,140 (10.5) |
1,232 (8.1) |
1,193 (10.1) |
1,179 (8.3) |
1,303 (9.9) |
1,069 (8.3) |
1,992 (9.4) |
380 (7.8) |
2,220 (9.4) |
152 (6.5) |
| Other |
817 (7.5) |
1,127 (7.4) |
883 (7.5) |
1,061 (7.5)* |
948(72) |
996 (7.7) |
1,562(7.4) |
382 (7.8) |
1,751 (7.4) |
193 (8.2) |
| Missing Unknown |
1,489 (13.7) |
1,933 (12.8) |
1,627 (13.8) |
1,795 (12.6) |
1,653 (13.5) |
1,653 (12.8) |
2,866 (13.6) |
556 (11.4) |
3,127 (13.2) |
295 (12.5) |
| Chronic condition severity |
|
|
|
|
|
|
|
|
|
|
| Episodic |
7,504 (69.2) |
10,521 (69.5)* |
8,139 (69.1) |
9,886 (69.5)* |
9,037 (68.9) |
8,988 (69.8)* |
14,488 (68.8) |
3,537 (72.5) |
16,396 (69.4) |
1,629 (69.1) |
| Life-Long |
3,019 (27.8) |
4,305 (28.4) |
3,279 (27.9) |
4,045 (28.4) |
3,705 (28.2) |
3,619 (28.1) |
1,992 (9.4) |
1,269 (26.0) |
6,654 (28.2) |
670 (28.4) |
| Malignancy |
33 (0.3) |
52 (0.3) |
37 (0.3) |
48 (0.3) |
43 (0.3) |
42 (0.3) |
1,562 (7.4) |
20 (0.4) |
72 (0.3) |
13 (0.6) |
| Catastrophic |
290 (2.7) |
269 (1.8) |
317 (2.7) |
242 (1.7) |
334 (2.5) |
225 (1.7) |
2,866 (13.6) |
51 (1.0) |
515 (2.2) |
44 (1.9) |
| Proximal factors |
|
|
|
|
|
|
|
|
|
|
| Child used preventive medical care in 2005 |
9,391 (86.6) |
13,689 (90.4)* |
10,205 (86.7) |
12,875 (90.5)* |
11,437 (87.2) |
11,643 (90.4)* |
18,691 (88.5) |
4,389 (90.0)† |
20,969 (88.7) |
2,111 (89.6) |
| Immediate factors |
|
|
|
|
|
|
|
|
|
|
| Child had at least one Medicaid- enrolled sibling |
7,200 (66.4) |
10,249 (67.7)‡ |
7,816 (66.4) |
9,633 (67.7)‡ |
8,677 (66.1) |
8,772 (68.1)† |
13,971 (66.2) |
3,478 (71.3)* |
15,806 (66.9) |
1,643 (69.7)† |
| Child had at least one Medicaid- enrolled adult |
6,097 (56.2) |
8,339 (55.1) |
6,528 (55.5) |
7,908 (55.6) |
7,334 (55.9) |
7,102 (55.2) |
11,595 (54.9) |
2,841 (58.3)* |
13,036 (55.2) |
1,400 (59.4)* |
| Immediate factor |
|
|
|
|
|
|
|
|
|
|
| Rurality |
|
|
|
|
|
|
|
|
|
|
| Metropolitan |
5,854 (54.0) |
8,499 (56.1)† |
6,363 (54.1) |
7,990 (56.2)† |
6,958 (53.0) |
7,395 (57.4)* |
11,631 (55.1) |
2,722 (55.8) |
13,007 (55.0) |
1,346 (57.1) |
| Urban adjacent to metropolitan |
2,123 (19.6) |
2,855 (18.8) |
2,308 (19.6) |
2,670 (18.8) |
2,607 (19.9) |
2,371 (18.4) |
4,088 (19.4) |
890 (18.2) |
4,545 (19.2) |
433 (18.4) |
| Urban non-adjacent to metropolitan |
2,275 (21.0) |
2,962 (19.6) |
2,456 (20.9) |
2,781 (19.6) |
2,802 (21.4) |
2,435 (18.9) |
4,264 (20.2) |
973 (20.0) |
4,783 (20.2) |
454 (19.3) |
| Rural |
594 (5.5) |
831 (5.5) |
645 (5.5) |
780 (5.5) |
752 (5.7) |
673 (5.2) |
1,133 (5.4) |
292 (6.0) |
1,302 (5.5) |
123 (5.2) |
| Distal factor |
|
|
|
|
|
|
|
|
|
|
| Child lived in a dental Health Professional Shortage Area | 7,260 (66.9) | 9,850 (65.0)† | 7,821 (66.4) | 9,289 (65.3) | 8,718 (66.5) | 8,392 (65.2)‡ | 13,898 (65.8) | 3,215 (65.9) | 15,566 (65.9) | 1,544 (65.5) |
Pearson Chi Square test to evaluate bivariate relationship between model covariates and each outcome measure.
* p < .0001.
† p < .01.
‡ p < .05.
Unadjusted dental utilization in 2006
About 58.3% of Medicaid-enrolled children with chronic conditions used any dental care in 2006; 54.7% used diagnostic care; 49.5% used preventive care; 18.8% used routine restorative care; and 9.1% used complex restorative care (Table 4).
Table 4.
Dental utilization rates by chronic condition subgroups and across covariates
|
All children with a chronic condition | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
N = 25,993 | ||||||||||
| Utilized any dental care in 2006 | Utilized any diagnostic dental care in 2006 | Utilized any preventive dental care in 2006 | Utilized any routine restorative dental care in 2006 | Utilized any complex restorative dental care in 2006 | ||||||
| |
n = 15,147 (58.3) |
n = 14,221 (54.7) |
n = 12,874 (49.6) |
n = 4,877 (18.8) |
n = 2,356 (9.1) |
|||||
| |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
| Main predictor variables (chronic condition subgroups) |
|
|
|
|
|
|
|
|
|
|
| Respiratory condition |
|
|
|
|
|
|
|
|
|
|
| No |
2,398 |
54.3* |
2,188 |
49.6* |
1,988 |
45.0* |
759 |
17.2‡ |
337 |
7.6* |
| Yes |
12,749 |
59.1 |
12,033 |
55.8 |
10,886 |
50.4 |
4,118 |
19.1 |
2,019 |
9.4 |
| Ear/nose/throat chronic condition |
|
|
|
|
|
|
|
|
|
|
| No |
3,940 |
56.6‡ |
3,629 |
52.1* |
3,214 |
46.1* |
1,315 |
18.9 |
532 |
7.6* |
| Yes |
11,207 |
58.9 |
10,592 |
55.7 |
9,660 |
50.8 |
3,562 |
18.7 |
1,824 |
9.6 |
| Digestive condition |
|
|
|
|
|
|
|
|
|
|
| No |
8,473 |
57.4‡ |
7,917 |
53.6* |
7,204 |
48.8‡ |
2,822 |
19.1 |
1,290 |
8.7‡ |
| Yes |
6,674 |
59.4 |
6,304 |
56.1 |
5,670 |
50.5 |
2,055 |
18.3 |
1,066 |
9.5 |
| Musculoskeletal condition |
|
|
|
|
|
|
|
|
|
|
| No |
8,384 |
56.8* |
7,866 |
53.3* |
7,225 |
49.0‡ |
2,655 |
18.0* |
1,319 |
8.9 |
| Yes |
6,763 |
60.2 |
6,355 |
56.6 |
5,649 |
50.3 |
2,222 |
19.8 |
1,037 |
9.2 |
| Endocrine condition |
|
|
|
|
|
|
|
|
|
|
| No |
11,921 |
58.4 |
11,180 |
54.7 |
10,157 |
49.7 |
4,021 |
19.7* |
1,870 |
9.2 |
| Yes |
3,226 |
58.0 |
3,041 |
54.7 |
2,717 |
48.8 |
856 |
15.4 |
486 |
8.7 |
| Cardiovascular condition |
|
|
|
|
|
|
|
|
|
|
| No |
13,597 |
58.3 |
12,754 |
54.6 |
11,593 |
49.7 |
4,402 |
18.9 |
2,098 |
9.0 |
| Yes |
1,550 |
58.4 |
1,467 |
55.3 |
1,281 |
48.3 |
475 |
17.9 |
258 |
9.7 |
| Hematologic condition |
|
|
|
|
|
|
|
|
|
|
| No |
14,143 |
58.1 |
13,278 |
54.6 |
12,018 |
49.4 |
4,579 |
18.8 |
2,224 |
9.1 |
| Yes |
1,004 |
60.1 |
943 |
56.5 |
856 |
51.3 |
298 |
17.9 |
132 |
7.9 |
| Catastrophic neurological condition |
|
|
|
|
|
|
|
|
|
|
| No |
14,865 |
58.6* |
13,970 |
55.1* |
12,635 |
49.8* |
4,829 |
19.0* |
2,303 |
9.1 |
| Yes |
282 |
44.3 |
251 |
39.4 |
239 |
37.5 |
48 |
7.5 |
54 |
8.5 |
| Cranofacial condition |
|
|
|
|
|
|
|
|
|
|
| No |
14,869 |
58.3 |
13,964 |
54.7 |
12,635 |
49.6 |
4,814 |
18.9‡ |
2,319 |
9.1 |
| Yes |
278 |
58.4 |
257 |
54.0 |
239 |
46.4 |
63 |
13.2 |
37 |
7.8 |
| Diabetes |
|
|
|
|
|
|
|
|
|
|
| No |
14,952 |
58.3 |
14,039 |
54.8 |
12,709 |
49.6 |
4,820 |
18.8 |
2,335 |
9.1‡ |
| Yes |
195 |
55.6 |
182 |
51.9 |
165 |
47.0 |
57 |
16.2 |
21 |
|
| Ascribed factors |
|
|
|
|
|
|
|
|
|
|
| Age (years) |
|
|
|
|
|
|
|
|
|
|
| 3–7 |
5,621 |
58.3* |
5,357 |
55.5* |
5,056 |
52.4* |
1,675 |
17.4* |
985 |
10.2* |
| 8–12 |
6,719 |
59.3 |
6,279 |
55.5 |
5,897 |
52.1 |
2,113 |
18.7 |
1,103 |
9.7 |
| 13–14 |
2,807 |
55.8 |
2,585 |
51.4 |
1,921 |
38.2 |
1,089 |
21 |
268 |
5.3 |
| Sex |
|
|
|
|
|
|
|
|
|
|
| Female |
6,256 |
60.0* |
5,890 |
56.5* |
5,287 |
50.7‡ |
1,998 |
19.1 |
951 |
9.1 |
| Male |
8,891 |
57.1 |
8,331 |
53.5 |
7,587 |
48.8 |
2,879 |
18.5 |
1,405 |
9.0 |
| Race/ethnicity |
|
|
|
|
|
|
|
|
|
|
| White |
10,855 |
59.5* |
10,186 |
55.8* |
9,156 |
50.2* |
3,559 |
19.5* |
1,716 |
9.4* |
| Black |
1,232 |
51.9 |
1,179 |
49.7 |
1,069 |
45.1 |
380 |
16.0 |
152 |
6.4 |
| Other |
1,127 |
58.0 |
1,061 |
54.6 |
996 |
51.2 |
382 |
19.7 |
193 |
9.9 |
| Missing/Unknown |
1,933 |
56.5 |
1,795 |
52.5 |
1,653 |
48.3 |
556 |
16.2 |
295 |
8.6 |
| Chronic condition severity |
|
|
|
|
|
|
|
|
|
|
| Episodic |
10,521 |
58.4* |
9,886 |
54.8* |
8,988 |
49.9* |
3,537 |
19.6* |
1,629 |
9.0 |
| Life-Long |
4,305 |
58.8 |
4,045 |
55.2 |
3,619 |
49.4 |
1,269 |
17.3 |
670 |
9.1 |
| Malignancy |
52 |
61.2 |
48 |
56.5 |
42 |
49.4 |
20 |
23.5 |
13 |
15.3 |
| Catastrophic |
269 |
48.1 |
242 |
43.3 |
225 |
40.3 |
51 |
9.1 |
44 |
7.9 |
| Proximal factors |
|
|
|
|
|
|
|
|
|
|
| Child used preventive medical care in 2005 |
|
|
|
|
|
|
|
|
|
|
| No |
1,458 |
50.1* |
1,346 |
46.2* |
1,231 |
43.3* |
488 |
16.8† |
245 |
8.4 |
| Yes |
13,689 |
59.3 |
12,875 |
55.8 |
11,643 |
50.4 |
4,389 |
19.0 |
2,111 |
9.1 |
| Immediate factors |
|
|
|
|
|
|
|
|
|
|
| Child had at least one Medicaid-enrolled sibling |
|
|
|
|
|
|
|
|
|
|
| No |
4,898 |
57.3‡ |
4,588 |
53.7‡ |
4,102 |
48.0‡ |
1,399 |
16.4* |
713 |
8.3† |
| Yes |
10,249 |
58.7 |
9,633 |
55.2 |
8,772 |
50.3 |
3,478 |
19.9 |
1,643 |
9.4 |
| Child had at least one Medicaid-enrolled adult |
|
|
|
|
|
|
|
|
|
|
| No |
6,808 |
58.9 |
6,313 |
54.6 |
5,772 |
49.9 |
2,036 |
17.6* |
956 |
8.3* |
| Yes |
8,339 |
57.8 |
7,908 |
54.8 |
7,102 |
49.2 |
2,841 |
19.7 |
1,400 |
9.7 |
| Immediate factor |
|
|
|
|
|
|
|
|
|
|
| Rurality |
|
|
|
|
|
|
|
|
|
|
| Metropolitan |
8,499 |
59.2† |
7,990 |
55.7† |
7,395 |
51.5* |
2,722 |
19.0 |
1,346 |
9.4 |
| Urban adjacent to metropolitan |
2,855 |
57.4 |
2,670 |
53.6 |
2,371 |
47.6 |
890 |
17.9 |
433 |
8.7 |
| Urban non-adjacent to metropolitan |
2,962 |
56.6 |
2,781 |
53.1 |
2,435 |
46.5 |
973 |
18.6 |
454 |
8.7 |
| Rural |
831 |
58.3 |
780 |
54.7 |
673 |
47.2 |
292 |
20.5 |
123 |
8.6 |
| Distal factor |
|
|
|
|
|
|
|
|
|
|
| Child lived in a dental Health Professional Shortage Area |
|
|
|
|
|
|
|
|
|
|
| No |
5,297 |
59.6† |
4,932 |
55.5 |
4,482 |
50.5‡ |
1,662 |
18.7 |
812 |
9.1 |
| Yes | 9,850 | 57.6 | 9,289 | 54.3 | 8,392 | 49.0 | 3,215 | 18.8 | 1,544 | 9.0 |
Pearson Chi Square test to evaluate bivariate relationship between each chronic condition and outcome measure.
* p < .0001.
† p < .01.
‡ p < .05.
Significantly lower proportions of children with catastrophic neurological conditions used all types of dental care, expect for complex restorative care, for which there was no difference. Larger proportions of children with respiratory, ear/nose/throat, digestive, or musculoskeletal conditions used most types of dental care than did children with chronic conditions without these specific conditions. There was no difference in use across all types of dental care for children with and without diabetes or cardiovascular conditions. Utilization was inconsistent across the different types of dental care for children with hematologic, endocrine, or craniofacial conditions and those children with chronic conditions but without these specific conditions.
In regards to other variables, significantly larger proportions of children ages 3-7 and 8-12 years utilized all types of dental care, except routine restorative care, than did children ages 13-14 years. Compared to children with the least severe chronic conditions (episodic), larger proportions of children with a malignancy (the second highest severity group) utilized all types of dental care except for preventive dental care whereas children with a catastrophic condition (the most severe chronic condition group) utilized all types of dental care at the lowest rates.
Larger proportions of children who utilized preventive medical care in 2005 subsequently utilized dental care in 2006. Significantly larger proportions of children with a Medicaid-enrolled sibling utilized all types of dental care, whereas this relationship was statistically significant only for routine and complex restorative dental care for the children with a Medicaid-enrolled adult in the household. Significantly larger proportions of children in metropolitan areas utilized any, preventive, or diagnostic dental care; there were no significant differences by rurality for routine and complex restorative dental care. Finally, children who lived in a dental HPSA were less likely to utilize all types of dental care, though these differences were significant only for any dental care and for preventive dental care.
Poisson regression models
The statistical interaction between the two immediate factors, having a Medicaid-enrolled sibling or adult in the household, was statistically significant for routine restorative dental care use across all 10 chronic condition subgroups and for preventive dental care use for some of the chronic condition subgroups. The interaction term was included only in the models in which it was statistically significant. Covariate-adjusted relative risks (RR) corresponding to the 10 chronic condition subgroups are summarized in Table 5. Relative risks for other model covariates are available upon request. Our findings are organized into 4 groupings.
Table 5.
Covariate-adjusted relative risk (RR) associated with dental use across chronic condition subgroups
| |
Models A |
Model B |
Model C |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Utilized any dental care in 2006 | Utilized any diagnostic dental care in 2006 | Utilized any preventive dental care in 2006 | Utilized any routine restorative dental care in 2006 | Utilized any complex restorative dental care in 2006 | ||||||
| |
RR* |
95% CI |
RR |
95% CI |
RR* |
95% CI |
RR† |
95% CI |
RR* |
95% CI |
| Main exposure variables (reference group = no) |
|
|
|
|
|
|
|
|
|
|
| Respiratory condition |
1.06 |
1.03, 1.10 |
1.09* |
1.05, 1.13 |
1.07 |
1.03, 1.11 |
1.10 |
1.02, 1.19 |
1.13 |
1.01, 1.26 |
| Ear/nose/throat condition |
1.02 |
0.99, 1.05 |
1.04† |
1.01, 1.07 |
1.03 |
1.01, 1.07 |
1.03 |
0.97, 1.10 |
1.12 |
1.01, 1.24 |
| Digestive condition |
1.03 |
1.01, 1.05 |
1.03† |
1.01, 1.06 |
1.02 |
0.99, 1.04 |
0.98 |
0.93, 1.04 |
1.04 |
0.96, 1.13 |
| Musculoskeletal condition |
1.06 |
1.04, 1.08 |
1.06† |
1.04, 1.09 |
1.06 |
1.03, 1.08 |
1.08 |
1.02, 1.13 |
1.08 |
0.99, 1.17 |
| Endocrine condition |
0.99 |
0.96, 1.02 |
0.99† |
0.97, 1.02 |
0.97 |
0.94, 1.01 |
0.83 |
0.77, 0.89 |
0.92 |
0.84, 1.02 |
| Cardiovascular condition |
1.00 |
0.97, 1.04 |
1.01† |
0.97, 1.04 |
0.98 |
0.94, 1.02 |
0.98 |
0.90, 1.06 |
1.09 |
0.96, 1.23 |
| Hematologic condition |
1.04 |
0.99, 1.08 |
1.03† |
0.99, 1.08 |
1.03 |
0.98, 1.08 |
0.99 |
0.89, 1.10 |
0.82 |
0.70, 0.98 |
| Catastrophic neurological condition |
0.72 |
0.63, 0.81 |
0.68* |
0.60, 0.78 |
0.73 |
0.63, 0.84 |
0.48 |
0.34, 0.67 |
1.11 |
0.79, 1.56 |
| Craniofacial condition |
0.99 |
0.92, 1.07 |
0.98† |
0.90, 1.06 |
0.92 |
0.83, 1.01 |
0.76 |
0.61, 0.96 |
0.83 |
0.61, 1.13 |
| Diabetes | 0.95 | 0.87, 1.05 | 0.95† | 0.86, 1.05 | 0.98 | 0.87, 1.10 | 0.89 | 0.71, 1.13 | 0.67 | 0.44, 1.02 |
* Models adjusted for age, sex, race/ethnicity, chronic condition severity, preventive medical care use in 2005, Medicaid-enrolled sibling, Medicaid-enrolled adult, rurality, and living in a dental Health Professional Shortage Area.
† Models adjusted for age, sex, race/ethnicity, chronic condition severity, preventive medical care use in 2005, Medicaid-enrolled sibling, Medicaid-enrolled adult, statistical interaction between Medicaid-enrolled sibling and Medicaid-enrolled adult, rurality, and living in a dental Health Professional Shortage Area.
First, children with catastrophic neurological conditions were significantly less likely (RR: 0.48 to 0.73) to use most types of dental care than other children with chronic conditions but without a catastrophic neurological condition. There was no difference in complex restorative dental care use (p = .56). Children with an endocrine condition were slightly less likely to use preventive care and routine restorative dental care than children with chronic conditions but without an endocrine condition (p = .049 and p < .0001; respectively). Children with craniofacial conditions were also less likely to use routine restorative care and children with hematologic conditions were less likely to utilize complex restorative dental care than children with chronic conditions who did not have these particular conditions (p = .02 and p = .03; respectively). In other words, when there were differences, children with catastrophic neurological, endocrine, craniofacial, or hematologic conditions were less likely to utilize dental care than children with chronic conditions but without these specific conditions.
Second, children with respiratory or musculoskeletal conditions were significantly more likely to use most types of dental care than other children with chronic conditions but without these specific conditions (RR: 1.06 to 1.13 and 1.06 to 1.08; respectively). Among children with chronic conditions, there was no difference in complex restorative dental care use for children with and without musculoskeletal conditions. Children with ear/nose/throat conditions were significantly more likely to use diagnostic, preventive, and complex restorative dental care and there was no difference in use of any or routine restorative dental care. Children with digestive conditions were significantly more likely to use any dental care or diagnostic dental care than other children with chronic conditions without these specific conditions (RR: 1.03 for both types of dental care). There was no difference in use of the other three types of dental care. In other words, when there were differences, children with respiratory, musculoskeletal, ear/nose/throat, or digestive conditions were significantly were more likely to utilize dental care than other children with chronic conditions who did not have these particular chronic conditions.
Third, there was no significant difference across all five outcome measures for children with diabetes or cardiovascular conditions and children with other types of chronic conditions but without these specific conditions.
Fourth, in regards to other model covariates there are three sets of findings (data not shown). In the any, diagnostic, and preventive dental care use models (Models A), children in the following subgroups were significantly less likely to use dental care: children ages 13-14 (referent = ages 3-7); males; Blacks (referent = Whites); children with the most severe chronic health conditions; children who did not use preventive medical care in 2005; children without a Medicaid-enrolled sibling; those living in urban areas (referent = metropolitan); and those living in a dental HPSA. In the routine restorative dental care use models (Model B), findings were similar to those from Models A except that children ages 13-14 were more likely to use routine restorative care. There were no significant differences in the risk ratios of routine restorative dental care use across sex and dental HPSA status. For the complex restorative dental care use models (Model C), findings were similar to those from Models A except that there were no significant differences across sex, whether the child used preventive medical care in 2005, whether the child had a Medicaid-enrolled sibling, or whether the child lived in a dental HPSA.
Discussion
This is the first known study, to our knowledge, that examined dental care use for Medicaid-enrolled children with chronic conditions with an emphasis on body system-based subgroups. We compared dental care use for Medicaid-enrolled children across 10 chronic condition subgroups. Collectively, our data support two findings that are new to the dental health services literature: (1) dental care use is heterogeneous across chronic condition subgroups; and (2) the determinants of dental care use vary across different types of dental care.
There were three main findings in regards to specific chronic conditions. The first is that when there were differences children in certain subgroups (e.g., catastrophic neurologic, endocrine, craniofacial, hematologic conditions) were significantly less likely to use dental care than other children with chronic conditions who did not have these particular conditions. Children with these chronic conditions may be at the greatest risk for disparities in dental care use. There are two possible explanations. Many of these children have developmental or acquired cognitive deficits and may have difficulty cooperating during dental visits. Dentists could be less willing to treat these children because of inadequate training [22]. Another explanation is that caregivers may have high levels of stress associated with managing the child’s other systemic health care needs [23], which pushes oral health down on the priority list. It is particularly worrisome that children with catastrophic neurologic conditions were significantly less likely to use preventive dental care. This finding has oral health-related implications especially if the child has a poor diet or behavioral comorbidities that make it difficult for caregivers to brush the child’s teeth regularly with fluoridated toothpaste. These findings appear to conflict with previous work suggesting that Medicaid-enrolled children with intellectual or developmental disabilities are equally as likely to use preventive dental care as those without [13]. A possible explanation for this inconsistency is that children with intellectual or developmental disabilities present with varying degrees of disability. The previous study did not control for this factor while the current study did.
The second finding is that children with respiratory, musculoskeletal, ear/nose/throat, or digestive conditions were more likely to use most types of dental care compared to children with other types of chronic conditions but without these spe-cific conditions. Children with respiratory conditions (e.g., asthma, cystic fibrosis) may require medications or have enamel defects – factors that increase their risk for dental caries [24-26]. Children with musculoskeletal conditions (e.g., arthritis) are also at risk for oral health problems [27]. Children with ear/nose/throat conditions undergo procedures involving the mouth and oral structures, making it plausible that these children receive team-based medical care. These factors may increase caregiver awareness of the importance of dental visits or the likelihood of dental referrals by physicians, though there are no published data to support these hypotheses. Studies from the medical literature report low adherence to inhaler medication for Medicaid-enrolled children with asthma because of caregiver misunderstanding of medications, which makes the former explanation unlikely [28]. We recognize that the risk ratios from our models are small (ranging from 1.02 to 1.13). However, on a population-level, small risk ratios are meaningful, especially when the prevalence of a particular chronic condition is high [29]. The prevalence of respiratory conditions was over 80% and over 40% of children in our study had a musculoskeletal or ear/nose/throat condition. Identifying the mechanisms underlying higher rates of dental use for children with specific types of chronic conditions in future studies may provide insight on how to improve utilization rates for children in other chronic condition subgroups that are not as likely to use dental care.
The third finding is that there was no difference in dental use for children with diabetes or cardiovascular conditions compared to children with other chronic conditions but without these conditions. Non-significant differences in dental care use may not be a clinically significant problem as long as children are receiving appropriate dental care. However, this is unlikely, especially because these chronic conditions have oral health-related sequelae that make dental visits important. For instance, the link between pediatric diabetes and periodontal disease [30,31] underscores the importance of regular maintenance and monitoring therapy that might require additional dental visits for children with diabetes. Future studies should investigate whether no differences in dental care use across subgroups actually means that children in these subgroups are receiving appropriate dental care.
In addition to the findings related to specific chronic conditions, we found that children who used preventive medical care are significantly more likely to use all types of dental care, except for complex restorative care. While there is potential for selection bias [32], this finding reinforces the importance of strengthening the clinical ties between pediatric medicine and dentistry [33]. The mechanisms between use of medical and dental care have not yet been elucidated and require further investigation.
In term of the research significance of the our study, any dental care use, a standard measure of access to dental care services, may be a more appropriate proxy for use of diagnostic or preventive dental care services rather than routine or complex restorative dental care. When developing oral health intervention and polices, it may be most effective for planners to specify the particular types of dental care the program seeks to improve use of by taking into consideration the differential determinants of dental care. This maximizes the likelihood that children have appropriate access to preventive as well as restorative dental care when needed [34].
As with all studies, our investigation has strengths and limitations. The primary strength is that we used validated methods, 3M Clinical Risk Groups, to identify children with chronic conditions and to adjust for the severity of those chronic conditions in the models. In addition, we adopted an a priori conceptual model that helped to guide model covariate selection. Finally, we examined use of different types of dental care to obtain a more complete view of dental utilization for children with chronic conditions. The major limitation is the lack of clinical oral health data, which precluded us from determining whether the observed utilization rates were appropriate. This limitation can be addressed with future studies by collecting clinical data and linking these data with dental claims data. Another limitation is that we measured dental use during a single calendar year, which provides a snapshot rather than a longitudinal perspective on dental use. Future studies might examine utilization trends over time across the different chronic condition subgroups. Finally, because this was an observational study, there is potential for residual confounding, which we attempted to minimize by adopting a conceptual model that we used to develop our empirical model. In the future, there is the potential to link claims data with survey data that might be used to collect social and behavioral measures that potentially confound the relationship between chronic conditions and dental use.
Conclusion
The goal of pediatric dentistry is to ensure optimal oral health for all children, including children with chronic conditions. An important component of optimal oral health is regular visits to the dentist for preventive dental care and restorative care when needed. Our findings suggest heterogeneous dental utilization patterns for children across different chronic condition subgroups. It is important to note that nearly 42% of children in our study did not utilize any dental care in 2006, which highlights the barriers to dental care that many Medicaid-enrolled children with chronic condition encounter. Some of these barriers may be system-level (e.g., low reimbursement to dentists for treatment) whereas others are environmental/social (e.g., lack of dental offices in areas where Medicaid enrollees live) or behavioral (e.g., dentists’ unwillingness to see Medicaid patients or symptom-driven dental utilization patterns by patients). The next step for researchers is to identify the social and behavioral determinants of particular types of dental care use that exist at these various levels (e.g., ascribed, proximal, immediate, intermediate, distal). This information can then be used to develop and test multilevel clinical interventions aimed at improving dental utilization for specific subgroups of children with chronic conditions who exhibit the greatest disparities in dental care use.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DC conceived of the study, designed the study, conducted the statistical analyses, and drafted the manuscript. NR conducted the statistical analyses and drafted the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Donald L Chi, Email: dchi@uw.edu.
Nicholas A Raklios, Email: nickrak@uw.edu.
Acknowledgements
Thank you to the 3M Corporation for a no-cost Clinical Risk Grouping (CRG) Software license and the Iowa Department of Human Services and the University of Iowa Public Policy Center for access to Iowa Medicaid data. This study was supported in part by NIDCR/NIH Grant Numbers K08DE020856 and TL1RR025016.
References
- Institute of Medicine (IOM) and National Research Council (NRC) Improving access to oral health care for vulnerable and underserved populations. The National Academies Press, Washington, DC; 2011. [Google Scholar]
- Newacheck P, McManus M, Fox H, Hung Y, Halfon N. Access to health care for children with special health care needs. Pediatrics. 2000;105:760–766. doi: 10.1542/peds.105.4.760. [DOI] [PubMed] [Google Scholar]
- Neff J, Sharp V, Popalisky J, Fitzgibbon T. Using medical billing data to evaluate chronically ill children over time. J Ambul Care Manage. 2006;29:283–290. doi: 10.1097/00004479-200610000-00004. [DOI] [PubMed] [Google Scholar]
- Muldoon J, Neff J, Gay J. Profiling the health service needs of populations using diagnosis-based classification systems. J Ambul Care Manage. 1997;20:1–18. doi: 10.1097/00004479-199707000-00002. [DOI] [PubMed] [Google Scholar]
- Lewis C, Robertson AS, Phelps S. Unmet dental care needs among children with special health care needs: implications for the medical home. Pediatrics. 2005;116:e426–e431. doi: 10.1542/peds.2005-0390. [DOI] [PubMed] [Google Scholar]
- Burwell B, Crown W, Drabek J. Department of Health and Human Services, Washington, DC: U.S; 1997. Children with severe chronic conditions on Medicaid. [Google Scholar]
- Johnson P. Medicaid: Medicaid: benefits and services—2005. End of Year Issue Brief. Issue Brief Health Policy Track Serv. 2005;31:1–21. [PubMed] [Google Scholar]
- Dubay L, Kenney GM. Health care access and use among low-income children: who fares best? Health Aff (Millwood) 2001;20:112–121. doi: 10.1377/hlthaff.20.1.112. [DOI] [PubMed] [Google Scholar]
- Bloom B, Dey AN, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2005. Vital Health Stat 10. 2006;231:1–84. [PubMed] [Google Scholar]
- Buescher PA, Horton SJ, Devaney BL, Roholt SJ, Lenihan AJ, Whitmire JT, Kotch JB. Differences in use of health services between White and African American children enrolled in Medicaid in North Carolina. Matern Child Health J. 2003;7:45–52. doi: 10.1023/A:1022541617877. [DOI] [PubMed] [Google Scholar]
- Dasanayake AP, Li Y, Chhun N, Bronstein JM, Childers NK. Challenges faced by minority children in obtaining dental care. J Health Care Poor Underserved. 2007;18:779–789. doi: 10.1353/hpu.2007.0093. [DOI] [PubMed] [Google Scholar]
- Chi DL, Momany ET, Neff J, Jones MP, Warren JJ, Slayton RL, Weber-Gasparoni K, Damiano PC. Impact of chronic condition status and severity on dental utilization for Iowa Medicaid-enrolled children. Med Care. 2011;49:180–192. doi: 10.1097/MLR.0b013e3181f81c16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. J Public Health Dent. 2010;70:35–44. doi: 10.1111/j.1752-7325.2009.00141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff J, Clifton H, Park K, Goldenberg C, Popalisky J, Stout JW, Danielson BS. Identifying children with lifelong chronic conditions for care coordination by using hospital discharge data. Acad Pediatr. 2010;10:417–423. doi: 10.1016/j.acap.2010.08.009. [DOI] [PubMed] [Google Scholar]
- Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;15:S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto-Martin JA, Dunkle M, Earls M, Fliedner D, Landes C. Developmental stages of developmental screening: steps to implementation of a successful program. Am J Public Health. 2005;95:1928–1932. doi: 10.2105/AJPH.2004.052167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eklund SA, Pittman JL, Clark SJ. Michigan Medicaid's Healthy Kids Dental program: an assessment of the first 12 months. J Am Dent Assoc. 2003;134:1509–1515. doi: 10.14219/jada.archive.2003.0083. [DOI] [PubMed] [Google Scholar]
- 3M Health Information Systems. 3M Health Information Systems, Wallingford, CT; 2008. 3M Clinical Risk Grouping Software (for Windows), Version 6.1. [Google Scholar]
- 3M Health Information Systems. 3M Health Information Systems, Wallingford, CT; 2003. All patient refined diagnosis related groups (APR-DRGs), version 20.0, methodology overview. [Google Scholar]
- Healthcare Effectiveness Data and Information Set (HEDIS) Technical specifications manual, volume 2. National Committee for Quality Assurance, Washington, DC; 2004. [Google Scholar]
- McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- Casamassimo PS, Seale NS, Ruehs K. General dentists' perceptions of educational and treatment issues affecting access to care for children with special health care needs. J Dental Educ. 2004;68:23–28. [PubMed] [Google Scholar]
- Viner-Brown SI, Kim HK. Impact of caring for children with special health care needs on the family: Rhode Island's experience. Matern Child Health J. 2005;9:S59–S66. doi: 10.1007/s10995-005-4483-4. [DOI] [PubMed] [Google Scholar]
- Narang A, Maguire A, Nunn JH, Bush A. Oral health and related factors in cystic fibrosis and other chronic respiratory disorders. Arch Dis Child. 2003;88:702–707. doi: 10.1136/adc.88.8.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bimstein E, Wilson J, Guelmann M, Primosch RE. The relationship between oral and demographic characteristics of children with asthma. J Clin Pediatr Dent. 2006;31:86–89. doi: 10.17796/jcpd.31.2.977776084511l005. [DOI] [PubMed] [Google Scholar]
- Widmer RP. Oral health of children with respiratory diseases. Paediatr Respir Rev. 2010;11:226–232. doi: 10.1016/j.prrv.2010.07.006. [DOI] [PubMed] [Google Scholar]
- Barr T, Carmichael NM, Sándor GK. Juvenile idiopathic arthritis: a chronic pediatric musculoskeletal condition with significant orofacial manifestations. J Can Dent Assoc. 2008;74:813–821. [PubMed] [Google Scholar]
- Farber HJ, Capra AM, Finkelstein JA, Lozano P, Quesenberry CP, Jensvold NG, Chi FW, Lieu TA. Misunderstanding of asthma controller medications: association with nonadherence. J Asthma. 2003;40:17–25. doi: 10.1081/JAS-120017203. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Loh C. Effect sizes and statistical testing in the determination of clinical significance in behavioral medicine research. Ann Behav Med. 2004;27:138–145. doi: 10.1207/s15324796abm2702_9. [DOI] [PubMed] [Google Scholar]
- Lalla E, Cheng B, Lal S, Tucker S, Greenberg E, Goland R, Lamster IB. Periodontal changes in children and adolescents with diabetes: a case-control study. Diabetes Care. 2006;29:295–299. doi: 10.2337/diacare.29.02.06.dc05-1355. [DOI] [PubMed] [Google Scholar]
- Lalla E, Cheng B, Lal S, Kaplan S, Softness B, Greenberg E, Goland RS, Lamster IB. Diabetes mellitus promotes periodontal destruction in children. J Clin Periodontol. 2007;34:294–298. doi: 10.1111/j.1600-051X.2007.01054.x. [DOI] [PubMed] [Google Scholar]
- Lee JY, Rozier RG, Norton EC, Vann WF. Addressing selection bias in dental health services research. J Dent Res. 2005;84:942–946. doi: 10.1177/154405910508401013. [DOI] [PubMed] [Google Scholar]
- Rozier RG, Sutton BK, Bawden JW, Haupt K, Slade GD, King RS. Prevention of early childhood caries in North Carolina medical practices: implications for research and practice. J Dent Educ. 2003;67:876–885. [PubMed] [Google Scholar]
- Taichman LS, Sohn W, Lim S, Eklund S, Ismail A. Assessing patterns of restorative and preventive care among children enrolled in Medicaid, by type of dental care provider. J Am Dent Assoc. 2009;140:886–889. doi: 10.14219/jada.archive.2009.0282. [DOI] [PubMed] [Google Scholar]