To the Editor:
Examination of the ocular fundus is imperative in the diagnosis and treatment of many acute medical and neurologic conditions, but direct ophthalmoscopy is underused and difficult to perform without pharmacologic pupillary dilation.1,2 We believe that nonmydriatic ocular fundus photography (i.e., performed without pupillary dilation) represents a promising alternative to direct ophthalmoscopy, particularly in the emergency department, where limited training in ophthalmoscopy, increased demands on physicians' time, and underappreciation of the prognostic value of ocular fundus examination can place patients at risk for poor outcomes and expose their caregivers to medicolegal liability.1,3 The FOTO-ED (Fundus Photography vs. Ophthalmoscopy Trial Outcomes in the Emergency Department) study hypothesized that the use of nonmydriatic fundus photography4,5 in the emergency department would result in increased detection of abnormalities in the ocular fundus relevant to emergency-department care, a majority of which would be missed during routine clinical practice in the department.
We enrolled 350 adult patients whose chief symptom on presentation to the emergency department was headache (65%), acute focal neurologic deficit (29%), or acute visual change (26%) or whose diastolic blood pressure was 120 mm Hg or higher (6%). Patients could meet more than one inclusion criterion. Trained nurse practitioners obtained ocular fundus photographs with a nonmydriatic fundus camera (Kowa α-D). Photographs were reviewed by a neuro-ophthalmologist within 24 hours for findings relevant to treatment in the emergency department. The performance of emergency department physicians and the findings on direct ophthalmoscopy were prospectively recorded, with the physicians unaware of the photography results.
During routine evaluation, ophthalmoscopy was performed by an emergency department physician for only 48 of the 350 patients (14%; 95% confidence interval [CI], 10 to 18). In 44 enrolled patients, relevant ocular findings (13%; 95% CI, 9 to 17) were identified with the use of nonmydriatic fundus photography: 13 cases of optic-nerve edema, 13 intraocular hemorrhages, 10 instances of hypertensive retinopathy (grade 3 or 4), 4 cases of arterial vascular occlusion, and 4 instances of optic-nerve pallor (for details see the table in the Supplementary Appendix). Eleven of the findings were known before patients presented to the emergency department. Of the remaining 33 relevant findings, 6 were identified on ophthalmologic consultation to the emergency department and 27 solely by means of fundus photography (82%; 95% CI, 65 to 93). (In only 5 of these 33 patients was ophthalmoscopy performed by an emergency department physician; results were recorded as normal for all 5 patients.) The photographs were of diagnostic value for 97% of enrolled patients. Median photography time was 1.9 minutes (interquartile range, 1.3 to 2.9).
Ophthalmoscopy was performed infrequently and poorly by emergency department physicians. We observed that 13% of patients presenting to the emergency department at a large academic center with symptoms or conditions warranting ocular fundus examination had a finding that was relevant to the systemic and ophthalmic management and disposition of their case by the department. Nonmydriatic fundus photography easily detected relevant ocular fundus findings that were otherwise overlooked, and the photography was performed efficiently by nonphysician staff.
Supplementary Material
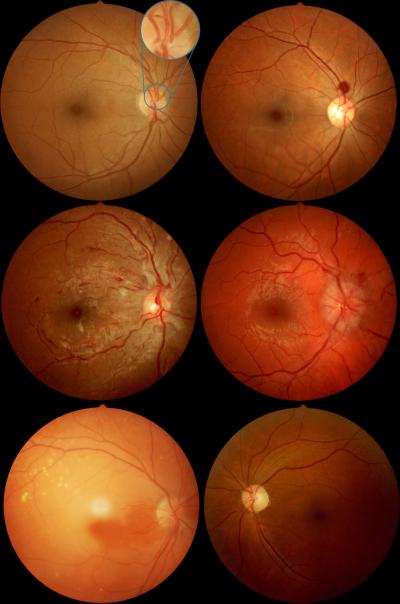
Figure.
Examples of non-mydriatic fundus photographs obtained by nurse practitioners during the FOTO-ED study. Top left: Normal posterior pole, showing the normal field of view of non-mydriatic fundus photography, which includes the optic nerve, macula, and major retinal vessels. The enlarged inset compares the single field of view of the most commonly used conventional direct ophthalmoscope which only shows part of the optic nerve head, and requires active exploration of the fundus by the examiner. Top right: Intraocular hemorrhage. Middle left: Grade IV hypertensive retinopathy with optic nerve edema, arterial attenuation, and retinal hemorrhages. Middle right: Optic nerve edema from intracranial hypertension. Bottom left: Acute retinal ischemia from central retinal artery occlusion. Bottom right: Optic nerve pallor. The black backgrounds of the original images were cropped and the brightness/contrast was adjusted.
Acknowledgments
This study was supported in part by a departmental grant (Department of Ophthalmology) from Research to Prevent Blindness, Inc., New York, by core grant P30-EY06360 (Department of Ophthalmology). Dr. Bruce has received research support from NIH/NCRR (KL2- RR025009, UL1-RR025008), the NIH/NEI (K23-EY019341), Knights Templar Eye Foundation, and received the American Academy of Neurology Practice Research Fellowship. Dr. Lamirel receives research support from Institut Servier (Paris, France), Fondation Planiol (Varennes, France), Ophtalmologie Progrès en Anjou (Angers, France), and the Philippe Foundation, Inc. (New York, NY). Dr. Wright received research support from NIH/PHS (KL2-RR025009). Dr. Biousse received research support from NIH/PHS (UL1-RR025008) and the Knights Templar Eye Foundation. Dr. Newman is a recipient of the Research to Prevent Blindness Lew R. Wasserman Merit Award.
Footnotes
None of the authors have any conflict of interest with regard to this work.
References
- 1.Roberts E, Morgan R, King D, Clerkin L. Funduscopy: a forgotten art? Postgrad Med J. 1999;75:282–284. doi: 10.1136/pgmj.75.883.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breen DP, Duncan CW, Pope AE, Gray AJ, Al-Shahi Salman R. Emergency department evaluation of sudden, severe headache. QJM. 2008;101:435–443. doi: 10.1093/qjmed/hcn036. [DOI] [PubMed] [Google Scholar]
- 3.Wash. App. (Wash. Ct. App., Nov. 15, 2005) 2005. Schliep v. Providence Yakima Med. Ctr. [Google Scholar]
- 4.Chabouis A, Berdugo M, Meas T, et al. Benefits of Ophdiat, a telemedical network to screen for diabetic retinopathy: a retrospective study in five reference hospital centres. Diabetes Metab. 2009;35:228–232. doi: 10.1016/j.diabet.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Massin P, Erginay A, Ben Mehidi A, et al. Evaluation of a new non-mydriatic digital camera for detection of diabetic retinopathy. Diabet Med. 2003;20:635–641. doi: 10.1046/j.1464-5491.2003.01002.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.