Abstract
In children, blood pressure (BP) and risk for hypertension are proportional to degree of adiposity. Whether the relationship to BP is similar over the full range of adiposity is less clear. Subjects from a cohort study (n=1,111; 50% male and 42% black) contributed 9,102 semiannual BP and height/weight assessments. The mean enrollment age was 10.2 years and mean follow-up was 4.5 years. Adiposity was expressed as body mass index (BMI) percentile, which accounted for effects of age and sex. The following observations were made. The effect of relative adiposity on BP was minimal until the BMI percentile reached 85, beginning of the overweight category, at which point the effect of adiposity on BP increased by four-fold. Similarly intensified adiposity effects on BP were observed in children aged 10 or younger, 11 to 14 years, and 15 years or older. Serum levels of the adipose tissue-derived hormone, leptin, together with heart rate showed an almost identically patterned relation to BP to that of BMI percentile and BP thus implicating a possible mediating role for leptin. In conclusion, there is a marked intensification of the influence of adiposity on BP when children reach the categories of overweight and obese. Among the possible pathways, leptin may be a potentially important mediator acting through the sympathetic nervous system (reflected in heart rate). The findings have relevance to interventions designed to prevent or treat adiposity-related increases in BP and to the analytical approaches used in epidemiologic studies.
Keywords: Hypertension, obesity, leptin, heart rate, sympathetic nervous system
Introduction
Overweight and obesity, defined by body mass index (BMI) cutoff points, have long been recognized as risk factors for hypertension.1,2 Although the physiological mechanisms that modulate the effects of obesity on blood pressure (BP) are not fully elucidated,3,4 epidemiological data that link increased BMI to higher BP are remarkably consistent across different populations.5-8 In children, hypertension is often accompanied by detectable target organ damage and the elevated BP typically continues into adulthood. 9,10 Overweight and obese children are known to face significantly increased risk for hypertension as adults.11-14
Clinical data from pediatric primary care practices in the United States showed greater mean systolic and diastolic BP, and higher hypertension prevalence rates in overweight and obese children.15 Recent studies now report on worldwide increases in prevalence rates of hypertension in obese children.16-18 Less is known about the extent to which adiposity influences BP in children of different weight categories. For example, it is unclear whether adiposity influences BP in normal weight children as it does in overweight children. From a clinical perspective, differentially manifested adiposity effects in children of different weight categories would justify more targeted intervention strategies.
In the present study, we analyzed BMI and BP data collected in a cohort of healthy children. Since BMI increases with age in children, it is recommended that BMI percentile be used, which takes into account an individual's age and sex.19 BP was similarly converted to percentile values for the purpose of defining prehypertension and hypertension.20 In a series of secondary analyses, we found evidence that favored a role of leptin in linking an effect of adiposity on BP.
Methods
Study protocol
Subjects were healthy children from a cohort study of BP regulation.21,22 They were recruited from schools in Indianapolis selected to provide a range in socioeconomic status. Most of the recruitment took place over the first three years (795 individuals were recruited in year one). Follow-up measurements were carried out semiannually (between 0800 and 1200 hr) at the subject's school (33 participated) or in some instances in the Indiana University Clinical Research Center or in the subject's home. BP was measured in the right arm with a random zero sphygmomanometer (Hawksley and Sons, Lancing, West Sussex, UK) while the subject was in a seated position. The first and fifth Korotkoff sounds were used for systolic and diastolic BP measurements, respectively. Three readings were obtained at intervals of at least 2 minutes, and the average of the last two readings was used in the analyses. A majority of study subjects also contributed at least one blood sample from which serum was separated and stored at -20° C. The study protocol was approved by the Indiana University Institutional Review Board. All participants (and a parent) provided written informed consent or assent as appropriate.
BMI and BP percentiles
BMI was calculated from the height and weight [BMI = Weight / Height2]. A methodological challenge in assessing the BMI-BP relationship in children is to deal with the confounding effect of age. The concurrent increases of BMI and age make it difficult to distinguish an effect of BMI from that of age. To minimize the impact of such confounding, we converted the BMI to age and sex adjusted percentile values by comparing the raw BMI values with the CDC BMI-for-age growth data.19 The resulting percentile indicated the relative position of each child's BMI among children of the same age and sex. With percentile values of BMI, we were able to define the weight status of children at different ages. Consistent with the current clinical practice, we considered children with BMI percentile values between 85% and 95% as overweight, and those with percentile values greater than 95% as obese.23
For similar reasons, we converted levels of BP to percentile values so that hypertension status of the study subjects could be determined. We obtained age, sex, and height adjusted percentile values of systolic and diastolic BP by comparing the raw BP data to the national normative data.20 We used the criteria described by the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents to define BP levels in the hypertensive and prehypertensive range.20 Specifically, we considered systolic and diastolic BP between the 90th and 94th percentiles in the prehypertensive range, and levels at or above the 95th percentile in the hypertensive range. Because relatively few BP were in the hypertensive range, we combined categories of prehypertension or hypertension in this analysis.
Leptin assay
Serum concentrations of leptin were determined using a commercial radioimmunoassay kit (Linco Research, Inc., St. Charles, MO) as previously described. 24 The sensitivity of the assay was 0.5 ng/ml and the interassay precision ranged from 3.6 to 6.2%.
Data analysis
Demographic and clinical characteristics of the study subjects were summarized, stratified by subjects' weight status. We examined the relationships between BMI and BP percentiles graphically for indications of differential adiposity effect on blood pressure, in boys and girls of different races. Using the 85th percentile of BMI as the overweight cutoff point, we fitted piecewise regression models for examination of the associations between BMI and BP percentiles in normal weight and overweight children. The estimated slope parameters from regression analysis quantified the magnitude of the adiposity effects. Two slopes were obtained from each regression model, one for normal weight and one for overweight and obese children. Comparing the two estimated slope parameters identified the differences in magnitude of adiposity effects between normal weight and overweight/obese children. Similarly, we used piecewise logistic regression analysis to quantify the effects of BMI percentile on the risk of having prehypertensive and hypertensive levels of BP, defined as either systolic or diastolic BP being in the 90th percentile. In the logistic regression analysis, BMI percentile effects were quantified as odds ratios. It should be noted that our analysis utilized repeated BMI and BP assessments, thus affording improved analytical power and wider age range for the examination of BMI-BP relationship. To accommodate the potential correlations among the repeated measurements contributed by the same subject, we used mixed models to fit the linear regressions (SAS PROC MIXED) and the generalized estimation equations (GEE) technique to fit the logistic regression models (PROC GENMOD),25 with age and race/sex group included as covariates. We repeated the regression analysis in age-stratified samples to examine the BMI effects on BP in children of different age. The sample was stratified into three age groups: 10 years or younger, 11-14 years, 15 years or older. In light of recent data suggesting other cutoff points,26 we performed a sensitivity analysis on the adiposity effect on BP using the 90th percentile BMI cutoff point. To examine the potentially nonlinear relationships between BMI percentile risk of prehypertension/hypertension, we estimated the probability of having a BP measurement in the prehypertension or hypertension range as a smooth function of the BMI percentile using semiparametric regression analysis.27 A similar technique was used to examine the effects of BMI percentiles on serum leptin concentration and heart rate, as well as the effects of leptin on BP and heart rate. In these analyses, leptin's relationships to BMI and BP were modeled as nonlinear functions; estimated effects were presented graphically. Analyses were performed using SAS Version 9.3, and R Version 2.11. P values less than 0.05 were considered statistically significant.
Results
A group of 1111 subjects (50% male; 42% black) contributed a total of 9102 semiannual BP and height/weight assessments, averaging 8.2 assessments per subject. The mean length of follow-up was 4.5 years (standard deviation 3.7 years). Mean enrollment age was 10.2 years (range, 4-17 years).
BP percentiles were calculated using national normative data from the 1999 and 2000 National Health and Nutrition Examination Survey (NHANES),20 and BMI percentiles using national normative data collected in the 1970s.19 As shown in Table 1, the mean systolic BP percentile was significantly higher for overweight/obese children than normal weight children (51% vs 35%, p < 0.0001); the average value of diastolic BP percentile was also significantly higher for overweight children (54% vs 44%, p < 0.0001). Overweight children had a significantly greater proportion of BP measurements in the prehypertension or hypertension range (14% in overweight vs 5% in normal weight children, p < 0.0001). Additionally, we noted that children whose BMI had not exceeded the 85th percentile threshold before age 15 tended to have lower BMI percentiles and systolic BP after age 15 (BMI percentile 52 vs 89, p<0.0001; systolic BP 107 vs 118 mm Hg, p<0.0001).
Table 1.
Summary statistics of study sample for normal weight and overweight children.
| Variables | Full Sample | Overweight (BMI>85th percentile) | Normal weight (BMI≤85th percentile) |
|---|---|---|---|
| Mean (SD) [sample size] | Mean (SD) [sample size] | Mean (SD) [sample size] | |
| Total number of visits | 9102 | 2655 | 6447 |
| BP in Hypertensive level (%) * | 312 (3%) | 195 (7%) | 117 (2%) |
| BP in Prehypertensive or hypertensive levels (%) * | 687 (8%) | 370 (14%) | 317 (5%) |
| Systolic BP percentile * | 39 (26) [9102] | 51 (27) [2655] | 35 (25) [6447] |
| Diastolic BP percentile * | 47 (26) [9102] | 54 (26) [2655] | 44 (26) [6447] |
| Leptin † | 9.9 (10.98) [301] | 19.7 (15.02) [88] | 5.85 (4.67) [213] |
| Heart rate † | 81 (12) [9094] | 82 (12) [2653] | 80 (11) [6441] |
Notes:
indicates statistical significance between normal weight and overweight children (unadjusted p<0.05).
indicates statistical significance (p<0.05) per analysis of covariance (ANCOVA) on logarithmic transformed data. We adjusted the effects of age, sex, race in the analysis
Scatter plots of BP and BMI percentiles revealed that before the BMI percentile reached its upper spectrum, the BP effect of BMI percentile was relatively modest (exploratory graphs not shown). Once BMI reached the overweight/obesity category (> 85th percentile), the adiposity effect on BP was greatly intensified. Using the 90th percentile BMI as the cutoff point, the increase in the slope was even more dramatic, suggesting substantially increased adiposity effect on BP in overweight and obese children. Importantly, such an intensification of the BMI percentile effect was observed in all sex and race groups.
The greatly increased adiposity effects were confirmed by regression analysis. As shown in Table 2, the estimated BMI percentile effects on systolic BP were approximately four-fold greater for overweight children than for children who were normal weight. For example, in normal weight black boys, the estimated BMI percentile effect on systolic BP percentile was 0.1 (95% confidence interval [CI]: 0.06, 0.14), while the corresponding effect in overweight black males was 0.49 (95% CI: 0.35, 0.64), a nearly five-fold increase. For other race and sex groups, the increases were also more than quadrupled. In a sensitivity analysis, we observed that the adiposity effects would have increased by more than six fold had we used 90th percentile BMI as a cutpoint. Similar changes in magnitude of BMI percentile effect were also observed between normal weight and overweight children for diastolic BP.
Table 2.
Regression coefficients (slopes) of BMI percentile (BMI%) for systolic and diastolic BPs from piecewise linear regression models, with BMI cutoffs at the 85th percentile. Odds ratios of BP in the prehypertension or hypertension range (i.e., either systolic and diastolic BP in the top 90th percentile) associated with a 5-percent increase in the BMI% from piecewise logistic regression models, with BMI cutoffs at the 85th percentile. For comparison purposes, we also included the estimated regression coefficients from linear regression models without BMI cutoffs. Abbreviations BF: black female; BM: black male; WF: white female; WM: white male.
| BMI% cutoff | Race/Sex | N (subject) | n (visit) | SBP Slope | DBP Slope | Odds Ratios for PreHTN/HTN |
|---|---|---|---|---|---|---|
| Using BMI% cutoff | ||||||
| All | 880 | 6446 | 0.08 (0.06, 0.09) | 0.02 (0.01, 0.04) | 1.02 (0.99, 1.04) | |
| BF | 176 | 1065 | 0.06 (0.03, 0.09) | 0.03 (0.00, 0.06) | 1.03 (0.97, 1.10) | |
| BMI% < 85 | BM | 155 | 906 | 0.10 (0.06, 0.14) | -0.01 (-0.05, 0.03) | 1.03 (0.94, 1.12) |
| WF | 269 | 2146 | 0.05 (0.03, 0.07) | 0.02 (0.00, 0.05) | 1.03 (0.98, 1.08) | |
| WM | 280 | 2329 | 0.10 (0.08, 0.12) | 0.03 (0.00, 0.05) | 1.01 (0.96, 1.06) | |
| All | 447 | 2656 | 0.44 (0.37, 0.51) | 0.33 (0.26, 0.40) | 1.76 (1.55, 2.00) | |
| BF | 117 | 629 | 0.33 (0.19, 0.47) | 0.29 (0.15, 0.44) | 1.33 (1.07, 1.67) | |
| BMI% > 85 | BM | 105 | 625 | 0.49 (0.35, 0.64) | 0.34 (0.19, 0.49) | 1.94 (1.48, 2.53) |
| WF | 96 | 626 | 0.47 (0.33, 0.62) | 0.41 (0.25, 0.57) | 1.80 (1.36, 2.38) | |
| WM | 129 | 776 | 0.44 (0.32, 0.56) | 0.32 (0.19, 0.45) | 1.90 (1.47, 2.45) | |
| Using no BMI% cutoff | ||||||
| All | 1111 | 9102 | 0.11 (0.10, 0.12) | 0.05 (0.04, 0.06) | 1.11 (1.08, 1.14) | |
| BF | 245 | 1694 | 0.09 (0.06, 0.11) | 0.06 (0.03, 0.08) | 1.07 (1.02, 1.13) | |
| BM | 217 | 1531 | 0.15 (0.12, 0.18) | 0.04 (0.01, 0.07) | 1.21 (1.11, 1.31) | |
| WF | 312 | 2772 | 0.08 (0.06, 0.10) | 0.05 (0.03, 0.07) | 1.10 (1.05, 1.15) | |
| WM | 337 | 3105 | 0.13 (0.11, 0.15) | 0.05 (0.03, 0.07) | 1.11 (1.06, 1.16) |
Prehypertension and hypertension in children are defined as either systolic or diastolic BP exceeding their respective 90th and 95th percentile thresholds. Using logistic regression analysis, we examined the effect of the BMI percentile on the risk of having a BP in the prehypertension or hypertension range. Analysis showed that for normal weight children, BMI percentile was not significantly associated with prehypertension/hypertension risk in normal weight children (Odds ratio (OR) = 1.02, 95% CI: 0.99, 1.04). Similar conclusions held true for boys and girls of all races. But for overweight children, the estimated BMI percentile effects were significantly greater. For example, in overweight black females, for each 5% increase in the BMI percentile, there was a 33% increase in the odds of having BP in the prehypertension and hypertension range (OR=1.33, 95% CI: 1.07, 1.67), compared to a non-significant increase in normal weight black females (OR=1.03, 95% CI: 0.97-1.10). For other groups, the risk was nearly doubled.
Had we not stratified the study sample by weight status, the magnitude of the resulting estimate of BMI percentile would be very different, as shown in the bottom panel of Table 2: the estimates based on combined sample would lie between the corresponding estimates for normal weight children and overweight children.
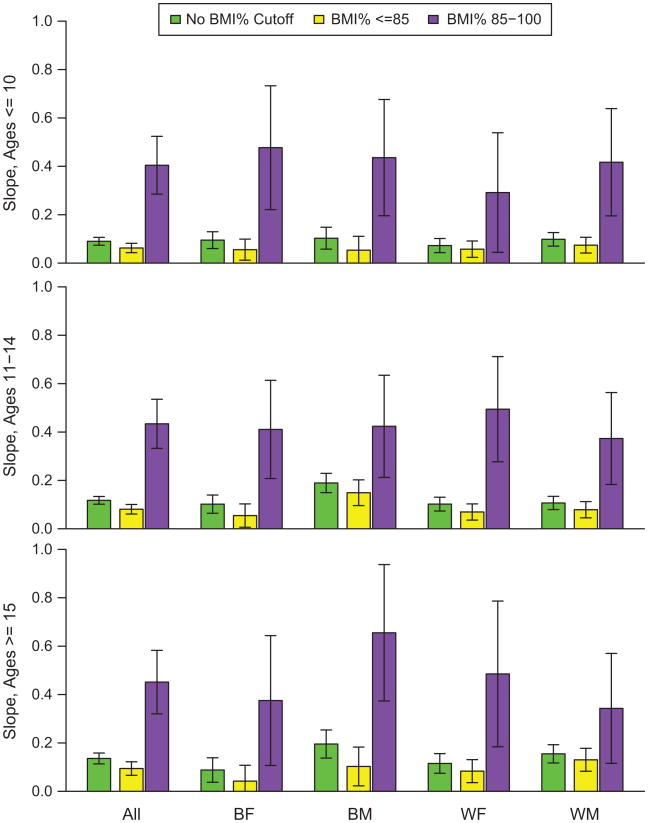
Importantly, the much intensified adiposity effects on BP were quite similar at different age. To highlight the similarly increased BMI percentile effects on BP in normal weight and overweight/obese children at different age, we presented the magnitudes of the estimated slopes in Figure 1. The figure again demonstrated that without a BMI cutoff point, the adiposity effects on BP tended to be severely underestimated for overweight and obese children, and overestimated for normal weight children.
Figure 1.
Comparisons of the BMI percentile effects on systolic BP percentile for normal weight and overweight children of different age groups. Purple bars represented the estimated adiposity effects on BP in overweight and obese children; yellow bars represented the estimated adiposity effects on BP in normal weight children. Green bars represented the adiposity effect estimates when no BMI percentile cutoff point was used. The figure showed that without weight status stratification, one could severly underestimate the adiposity effects on BP in overweight and obese children, and overestimates the effect in normal weight children. Top panel: Estimates for children 10 years of age or younger. Middle panel: Estimates for children 11 to 14 years of age. Bottom panel: Estimates for children 15 years of age or older. The figure showed that adiposity effects on BP were similarly intensified in overweight and obese children of all age groups.
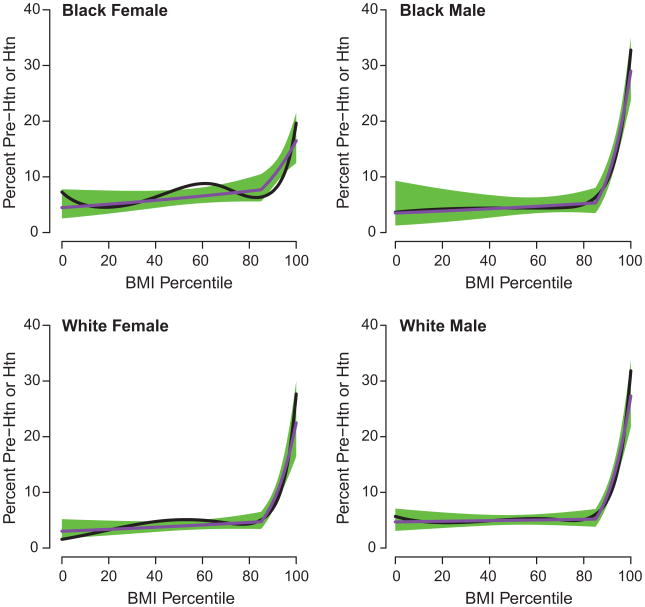
To better understand the adiposity effect on the risk prehypertension/hypertension in the entire continuum of BMI percentile, we used semiparametric logistic regression analysis to examine the probability of having BP measurement in the prehypertension/hypertension range. The analysis showed that there was minimal adiposity effect until the BMI percentile reached the 85th percentile threshold, from which point on the prehypertension risk increased very significantly, as shown by the dramatic upswings in upper BMI percentiles (see Figure 2). Similar effect patterns were confirmed by piece-wise logistic regression analysis.
Figure 2.
Estimated probability of BP reaching prehypertension (pre-HTN) and hypertension (HTN) levels. The black lines are smooth functions of the BMI percentile from semiparametric logistic regression analysis, and the purple lines are from the piece-wise linear logistic regression analysis with an inflection point at the 85th percentile of BMI. The green bands represent the 95% confidence intervals for the mean proportion of BP measurements in the pre-HTN/ HTN levels estimated from the piece-wise logistic regression analysis.
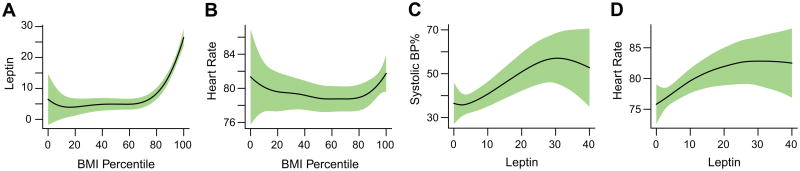
Accompanying the elevated BP and prehypertension/hypertension risk in the overweight and obese children were noticeably higher serum leptin concentrations (19.7 ng/ml in overweight and obese children versus 5.85 ng/ml in normal weight children; p < 0.0001), even after adjusting for the effects of age, sex, and race. Interestingly, we also observed a similar upswing in the leptin level mirroring the increase of BP effect of adiposity in overweight and obese children (Figure 3a). Graphical examination showed that leptin levels remained stable over the entire age range of our study subjects.
Figure 3.
Estimated levels of serum leptin concentration (a) and heart rate (b) at different BMI percentiles. Estimated levels of systolic blood pressure percentile (c) and heart rate (d) at different levels of serum leptin concentration.
We then examined heart rates of overweight and normal weight children. Although the mean heart rates were quite close (82 for overweight and obese children and 80 for normal weight children), analysis of covariance adjusting for age, sex, and race, showed that overweight and obese children tended to have significantly greater heart rate than those of normal weight (p=0.025). For a more detailed exploration, we examined the mean heart rates over the entire continuum of BMI percentile, which revealed greater mean heart rates at both ends of the BMI percentile spectrum (Figure 3b). Similar analyses also revealed that leptin was positively associated with systolic and diastolic BP percentiles (systolic data presented in Figure 3c; diastolic data not shown), and heart rates (Figure 3d). It should be noted in this study, leptin was not measured as frequently as BP and BMI. As a result, we did not have sufficient power to use leptin to predict future BP.
Discussion
It is well accepted that BP increases as BMI increases in persons of all ages and that hypertension is more prevalent in higher BMI categories. In the present study of children, we further quantified and compared the magnitudes of BP effects of relative adiposity (depicted by BMI percentiles) in children of different weight categories. Surprisingly, the data showed that the effect of adiposity on BP was rather modest until a child's BMI reached the overweight category at which point the effect on BP quadrupled. Similar results were observed in males and females and in both race groups. The fact that the intensified adiposity effects on BP were similarly observed in children regardless of age group reveals the persistent nature of this relationship. Practically, it highlights the importance of recognizing the much added risk that accompanies true obesity in children.
The differential BP effect of adiposity points to the need for more targeted interventions to reduce cardiovascular morbidity in overweight and obese children since even a small decrease in BMI percentile may produce significant health benefits. Along the same line, further research is needed to establish evidence-based weight management targets for hypertension risk reduction in the context of somatic growth.
The marked difference in the adiposity effect of normal and overweight children highlights the importance of weight category stratification when quantifying the BP effects of adiposity. Since the adiposity effect on BP is primarily manifested in overweight and obese children (Table 2 and Figure 1), estimates based on unstratified samples will likely result in overestimates of the adiposity effect for normal weight children and underestimates of the effect for overweight children.
Although a mechanistic explanation for the intensified adiposity effect on BP was not within the original scope of this investigation, with the observed pattern of adiposity effect on BP, we made the assumption that an important mediator might be suggested if its levels shared a similar pattern with the effect of adiposity on BP. To this end, the intensification of adiposity influences on BP at the upper range of BMI percentiles afforded an opportunity to look for potential mediators. We selected to study in a preliminary fashion the adipose tissue-derived hormone leptin which has been implicated in mediating obesity-induced increases in BP. Indeed, the spike in leptin levels closely resembled the patterns of BP sensitivity to BMI percentile. The concurrent upswings of leptin, heart rate, and BP in the upper BMI percentiles, as well as leptin's positive associations with heart rate and BP appear to give additional credence to the notion that leptin influences BP possibly by its known ability to enhance sympathetic nervous system (SNS) activity (reflected in the increase in heart rate). Establishing such a role for leptin, however, is complicated by the fact that both leptin and BMI are markers of adiposity. Including both in the same model would leave leptin depleted of a detectable influence on BP. Nonetheless, we noted that when leptin was added to the regression model, the significance level of BMI was greatly reduced, although it remained statistically significant, suggesting the existence of still other mechanistic pathways.3,4,28-32 We also examined BMI's relation to plasma aldosterone levels but did not see an identifiable pattern. It would be of interest to examine other possible factors related to adiposity, such as insulin, adiponectin, and inflammatory cytokines, which were not measured in our study.
We recognize several limitations to the current study. Despite the reasonably large sample size, the analytical power remained limited to exam prehypertensive and hypertensive BP levels separately. The focus on healthy children, who were at an age when development of hypertension was still uncommon, could also be considered a limiting factor. On the other hand, we were afforded the opportunity to observe the normal physiology unencumbered by confounders that result from the hypertension and/or its treatment. Indeed, we may not have observed the relationships described had we studied an older adult population. In this sense, it is unclear to what extent we might be able to generalize the findings to an adult population or to hypertensive individuals. A recent study has reported on the existence of a distinct difference between those with and without hypertension with respect to relationships to BMI: hypertensives in contrast to normotensives did not show the relationship of BP to level of adiposity.33 Thus, there may be multiple examples wherein relationships of adiposity to BP are not fully predictable.
Perspective
Results from the present study of young people could change the way we approach the relationship of body size to the level of BP. Clearly, behavioral measures that are more difficult to implement, such as dietary changes and increases in physical activity, should perhaps be directed more towards those at the upper end of the BMI percentile scale. Possibly as important are the considerations that need to be given to future epidemiologic studies of adiposity and BP. Analyses where adjustments are made for body size, at least in young people, may require modification based on the relative standing of an individual on the BMI percentile scale. These adjustments may serve, as they did in the present study, to uncover unanticipated observations. Indeed, we were able to show a differential sensitivity of BP to adiposity that appeared to be mediated by leptin. These compelling findings might have been missed without weight status stratification. The relationship of increased adiposity in children to later in life cardiovascular disease is clear but what conveys the effects of adiposity remains less than conclusive. An understanding of the differential sensitivity of BP to adiposity via leptin could be worthwhile investigative goal.
Acknowledgments
Sources of Funding: This work was supported by National Heart, Lung, and Blood Institute Grant RO1-HL095086 and a Veterans Health Administration Merit Review Grant.
Footnotes
Disclosures: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Masuo K, Mikami H, Ogihara T, Tuck ML. Weight gain-induced blood pressure elevation. Hypertension. 2000;35:1135–1140. doi: 10.1161/01.hyp.35.5.1135. [DOI] [PubMed] [Google Scholar]
- 2.Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B, Mietus-Snyder ML. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2009;119:628–647. doi: 10.1161/CIRCULATIONAHA.108.191394. [DOI] [PubMed] [Google Scholar]
- 3.Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;4:625–633. doi: 10.1161/01.HYP.0000052314.95497.78. [DOI] [PubMed] [Google Scholar]
- 4.Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, Munusamy S, Smith G, Stec DE. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. J Biol Chem. 2010;285:17271–17276. doi: 10.1074/jbc.R110.113175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, Colditz GA. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128:81–88. doi: 10.7326/0003-4819-128-2-199801150-00001. [DOI] [PubMed] [Google Scholar]
- 6.Dyer AR, Liu K, Walsh M, Kiefe C, Jacobs DR, Jr, Bild DE. Ten-year incidence of elevated blood pressure and its predictors: the CARDIA study. Coronary Artery Risk Development in (Young) Adults. J Hum Hypertens. 1999;13:13–21. doi: 10.1038/sj.jhh.1000740. [DOI] [PubMed] [Google Scholar]
- 7.Davy KP, Hall JE. Obesity and hypertension: two epidemics or one? Am J Physiol Regul Integr Comp Physiol. 2004;286:R803–813. doi: 10.1152/ajpregu.00707.2003. [DOI] [PubMed] [Google Scholar]
- 8.Levin A, Morad Y, Grotto I, Ravid M, Bar-Dayan Y. Weight disorders and associated morbidity among young adults in Israel 1990-2003. Pediatr Int. 2010;52:347–352. doi: 10.1111/j.1442-200X.2009.02972.x. [DOI] [PubMed] [Google Scholar]
- 9.Falkner B. Hypertension in children and adolescents: epidemiology and natural history. Pediatr Nephrol. 2010;25:1219–1224. doi: 10.1007/s00467-009-1200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falkner B, Lurbe E, Schaefer F. High blood pressure in children: clinical and health policy implications. J Clin Hypertens (Greenwich) 2010;12:261–276. doi: 10.1111/j.1751-7176.2009.00245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1989;84:633–641. [PubMed] [Google Scholar]
- 12.Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–2337. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- 14.Tirosh A, Afek A, Rudich A, Percik R, Gordon B, Ayalon N, Derazne E, Tzur D, Gershnabel D, Grossman E, Karasik A, Shamiss A, Shai I. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension. 2010;56:203–209. doi: 10.1161/HYPERTENSIONAHA.109.146415. [DOI] [PubMed] [Google Scholar]
- 15.Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr. 2006;148:195–200. doi: 10.1016/j.jpeds.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 16.Stray-Pedersen M, Helsing RM, Gibbons L, Cormick G, Holmen TL, Vik T, Beliźan JM. Weight status and hypertension among adolescent girls in Argentina and Norway: data from the ENNyS and HUNT studies. BMC Public Health. 2009;9:398. doi: 10.1186/1471-2458-9-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raj M, Sundaram KR, Paul M, Sudhakar A, Kumar RK. Body mass index trend and its association with blood pressure distribution in children. J Hum Hypertens. 2010;24:652–658. doi: 10.1038/jhh.2010.6. [DOI] [PubMed] [Google Scholar]
- 18.Mazicioglu MM, Yalcin BM, Ozturk A, Ustunbas HB, Kurtoglu S. Anthropometric risk factors for elevated blood pressure in adolescents in Turkey aged 11-17. Pediatr Nephrol. 2010;25:2327–2334. doi: 10.1007/s00467-010-1623-x. [DOI] [PubMed] [Google Scholar]
- 19.Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr. 2002;75:978–985. doi: 10.1093/ajcn/75.6.978. [DOI] [PubMed] [Google Scholar]
- 20.The Fourth Report on the Diagnosis Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 21.Pratt JH, Jones JJ, Miller JZ, Wagner MA, Fineberg NS. Racial differences in aldosterone excretion and plasma aldosterone concentrations in children. N Engl J Med. 1989;321:1152–1157. doi: 10.1056/NEJM198910263211703. [DOI] [PubMed] [Google Scholar]
- 22.Manatunga AK, Jones JJ, Pratt JH. Longitudinal assessment of blood pressures in black and white children. Hypertension. 1993;22:84–89. doi: 10.1161/01.hyp.22.1.84. [DOI] [PubMed] [Google Scholar]
- 23.WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. In: WHO, editor. WHO Technical Report. Series 894. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 24.Ambrosius WT, Compton JA, Bowsher RR, Pratt JH. Relation of race, age, and sex hormone differences to serum leptin concentrations in children and adolescents. Horm Res. 1998;49:240–246. doi: 10.1159/000023178. [DOI] [PubMed] [Google Scholar]
- 25.Diggle PJ, Heagert P, Liang KY, Zeger SL. Analysis of Longitudinal Data. New York: Oxford University Press; 2002. See Chapters 4 and 5, page 55-113 for GEE models, and Chapter 8, page 141-160 for mixed effect models. [Google Scholar]
- 26.Skinner AC, Mayer ML, Flower K, Perrin EM, Weinberger M. Using BMI to determine cardiovascular risk in childhood: how do the BMI cutoffs fare? Pediatrics. 2009;124:e905–912. doi: 10.1542/peds.2009-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruppert D, Wand MP, Carroll RJ. Semiparametric Regression. Cambridge, UK: Cambridge University Press; 2003. pp. 214–222. Chapter 11. [Google Scholar]
- 28.Hall JE, Kuo JJ, da Silva AA, de Paula RB, Liu J, Tallam L. Obesity-associated hypertension and kidney disease. Current opinion in nephrology and hypertension. 2003;12:195–200. doi: 10.1097/00041552-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Halle M, Persson PB. Role of leptin and leptin receptor in inflammation. Am J Physiol Regul Integr Comp Physiol. 2003;284:R760–762. doi: 10.1152/ajpregu.00712.2002. [DOI] [PubMed] [Google Scholar]
- 30.Rahmouni K, Correia ML, Haynes WG, Mark AL. Obesity-associated hypertension: new insights into mechanisms. Hypertension. 2005;45:9–14. doi: 10.1161/01.HYP.0000151325.83008.b4. [DOI] [PubMed] [Google Scholar]
- 31.Goodfriend TL, Calhoun DA. Resistant hypertension, obesity, sleep apnea, and aldosterone: theory and therapy. Hypertension. 2004;43:518–524. doi: 10.1161/01.HYP.0000116223.97436.e5. [DOI] [PubMed] [Google Scholar]
- 32.Rahmouni K, Haynes WG, Morgan DA, Mark AL. Selective resistance to central neural administration of leptin in agouti obese mice. Hypertension. 2002;39:486–490. doi: 10.1161/hy0202.102836. [DOI] [PubMed] [Google Scholar]
- 33.Kotchen TA, Grim CE, Kotchen JM, Krishnaswamy S, Yang H, Hoffman RG, McGinley EL. Altered relationship of blood pressure to adiposity in hypertension. American journal of hypertension. 2008;21:284–289. doi: 10.1038/ajh.2007.48. [DOI] [PubMed] [Google Scholar]