Abstract
We report an incarcerated internal hernia in a huge irreducible parastomal hernia-"hernia within hernia." A 70-year-old obese woman with diabetes who underwent an abdomino-perineal resection 20 years ago was admitted to our hospital with 20 years history of a huge irreducible bulge, 25 cm in diameter. An internal hernia due to an adhesive band extending from the sac wall to proximal colon was found in the parastomal hernia sac during an emergency laparotomy. We cut off the distal colon and relocated the colostomy stoma. The patient was discharged uneventfully 2 weeks after the surgery and was readmitted to have a further laparoscopic hernia repair 8 months later. Unfortunately, an unrecognized enterotomy occurred during the secondary surgery that led to an additional laparotomy during which the mesh was not contaminated by the bowel contents and was kept in place. At 22-month follow-up, there were no evidences of recurrence.
Keywords: Ventral hernia, Incarceration, Intestinal obstruction, Herniorrhaphy
INTRODUCTION
Parastomal hernia is a common complication of colostomy formation that has an incidence rate varying between 5% and 52% [1,2]. Parastomal hernia is usually asymptomatic and rarely leads to bowel obstruction and a majority of the patients with parastomal hernias can be treated by conservative therapies [3]. There were sporadic reports of severe complications such as incarceration, strangulation, and obstruction resulting from parastomal hernia. We report a rare case of "hernia within hernia" presenting an incarcerated internal hernia in a huge irreducible parastomal hernia with intestinal obstruction.
CASE REPORT
A 70-year-old obese woman with diabetes who underwent an abdomino-perineal resection due to rectal cancer 20 years ago was admitted to our hospital with a 20-year history of a huge irreducible bulge occupying her left abdomen (Fig. 1) and presented with intermittent abdominal pain, abdominal distention, nausea, vomiting and no discharge from her colostomy stoma for 3 days. On physical examination, her abdomen was soft and distended. There was a huge irreducible bulge around the colostomy stoma in the left lower quadrant. A mild tenderness in the bulge was detected with no guarding and rebound tenderness. Abdominal computed tomography showed an abdominal wall defect 10 cm in diameter and a huge mass 25 cm in diameter containing loops of bowel (Fig. 2). Diagnosis of parastomal hernia with intestinal obstruction was established preoperatively. An emergency exploratory laparotomy revealed an incarcerated internal hernia due to an adhesive band extending from the hernia sac wall to distal colon in the huge parastomal hernia (Fig. 3). Two hernia rings were found in this patient: one was around the defect of the abdominal wall (primary parastomal hernia) and the other was composed of an adhesive band resulting in an incarcerated internal hernia. So diagnosis of "incarcerated internal hernia within primary parastomal hernia (hernia within hernia)" was confirmed during the operation. The lysis of the adhesive band and the removal of the distal colon were performed to relieve intestinal obstruction and the colostomy stoma was relocated into the left upper quadrant of the abdominal wall (Fig. 4). Abdominal wall defect repair with prosthetic mesh was not performed due to concerns of incisional infection and consequent removal of the mesh. The patient was discharged uneventfully 2 weeks after the surgery and was readmitted to have further laparoscopic intraperitoneal onlay mesh (IPOM) repair procedure 8 months later.
Fig. 1.

A huge irreducible bulge occupying the patient's left abdomen.
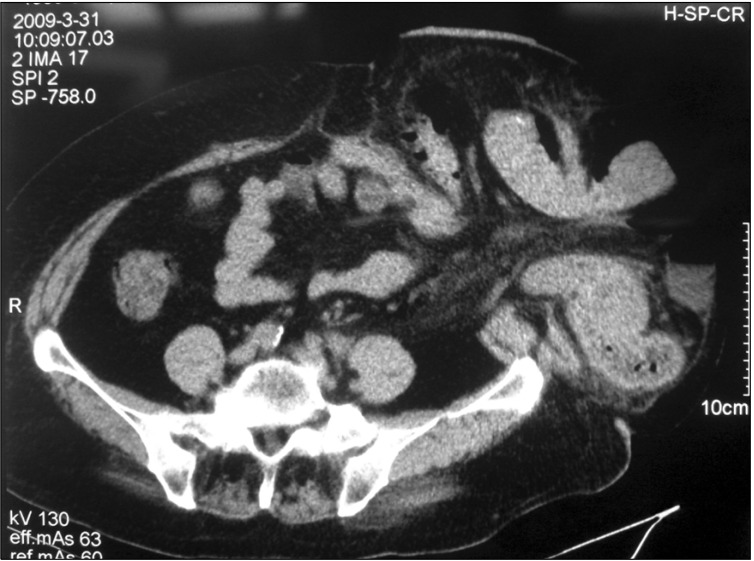
Fig. 2.
Computed tomography scanning showed an abdominal wall defect with 10 cm in diameter and a huge mass with 25 cm in diameter containing loops of bowel.
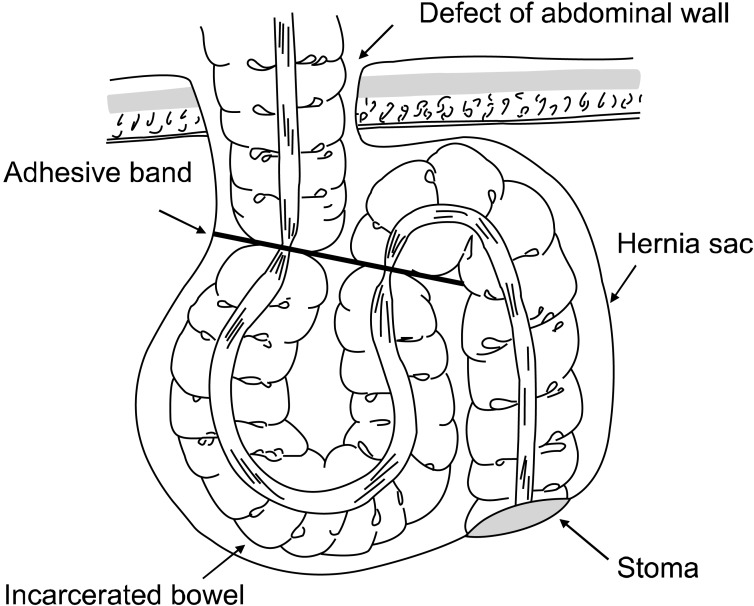
Fig. 3.
An adhesive band extending from the parastomal hernia sac wall to distal colon was found in the primary parastomal hernia. Some proximal colon and loops of small intestine (not included in this sketch) were incarcerated into the hernia ring formed by this adhesive band.
Fig. 4.

The colostomy stoma was relocated into the left upper quadrant of the abdominal wall.
Massive abdominal adhesion and two adjoined abdominal wall defects were found by diagnostic laparoscopy during the second procedure. One defect with about 12 × 10 cm in diameter located at the original stoma site while another defect with about 5 × 5 cm in diameter located at the new colostomy site (Fig. 5). A large mesh with a 5 cm orifice through which the stoma was able to go was used with the IPOM technique to cover both defects. Unfortunately, the patient presented with a right lower abdominal pain and high fever three days after the surgery. Some bile-like juice drained out from the abdominal drain tube. An emergency exploratory laparotomy was done revealing an intestinal perforation and an infected fluid collection in the right lower abdominal cavity confined by omentum and adjacent bowels. Fortunately, the intestinal fluid did not contaminate the mesh placed in the left side of the abdominal wall, so we were determined to keep the mesh in place. Resection of the affected portion of the small intestine and an end-to-end anastomosis were performed. After the third surgery, no other complications but incision infection developed in this patient. At 22-month follow-up, there were no evidences of recurrence.
Fig. 5.
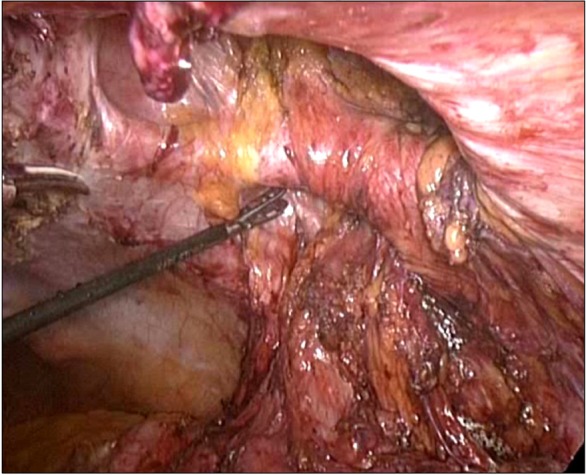
Laparoscopic view of the two defects of left abdominal wall. One defect with about 12 × 10 cm in diameter located at the original stoma site while another defect with about 5 × 5 cm in diameter located at the new site of colostomy.
DISCUSSION
Patients with parastomal hernia seldom develop severe situations such as incarceration and intestinal obstruction, because parastomal hernias usually have a big hernia ring through which hernia contents can pass freely. Only a small percentage of patients with parastomal hernia accept surgical repair due to the bulge that has affected daily life and ruined body image. This patient exceptionally developed an internal hernia caused by an adhesive band constricting the proximal colon and some small intestine in the parastomal hernia. It is a rare case of "hernia within hernia" that indicates prophylactic surgical repair; laparoscopic procedure may be a good option for patients with parastomal hernia in early stage to prevent such severe conditions. Several studies concluded that using a prophylactic mesh in a sublay position at primary stoma formation procedure is a promising method that lowers the high incidence rate of parastomal hernia [4,5].
In this complicated case of "hernia within hernia", we preferred a relatively conservative therapy that consisted of lysis of the adhesive band, removal of the distal colon, and relocation of the stoma but did not include a hernia repair in emergency. Placing an IPOM or a sublay position in this kind of patient without bowel preparation may result in a disastrous infection. We had experienced a similar case of incarcerated ventral hernia using a prosthetic mesh in emergency surgery that finally led to a fatal infection. So postponing the hernia repair to a scheduled surgery might be more feasible and safer.
It is a principle that the stoma should be relocated into a quadrant of the contrary side of the abdominal wall in parastomal hernia repair procedures. Relocation of the stoma into a quadrant of the same side of the abdominal wall may increase recurrence rates in the new site [6]. In this case, we relocated the stoma into the nearby area of the primary stoma, because the recurrence of the parastomal hernia in the new site in this obese patient with diabetes was anticipated and the secondary parastomal hernia repair surgery was scheduled during the first operation. It is more convenient for surgeons to repair two defects in same side using single mesh than in two sides using two meshes. Another reason we put the stoma into the same side is that the mobility of the distal colon was decreased because of massive adhesion in the abdominal cavity.
The incidence of iatrogenic bowel injury during incisional and ventral hernia repair was reported to be 1.78% in a systematic review [7]. Unrecognized bowel injury is a serious complication of laparoscopic incisional hernia repair and is usually due to thermal, trocar or tack injuries to intestines. Inadvertent enterotomy during separation of adhesions with ultrasonic scalpel usually results in acute peritonitis that needs an emergency exploratory laparotomy to repair the bowel perforation. Mesh tiled on the abdominal peritoneum usually needs to be removed from the anchoring site when it has been contaminated by the bowel contents spilled from a ruptured bowel, because the contaminated mesh being kept in place may lead to a catastrophic abdominal infection or some late complications such as enterocutaneous fistula due to erosion of intestines by the mesh. Fortunately, in this case, the perforated bowel was located in the right lower abdominal cavity so the tainted fluid did not contaminate the mesh overlaying on the opposite side of the abdominal wall. Another reason for our bold decision of keeping the mesh in place is that the prosthetic mesh Proceed (Ethicon Inc., Somerville, NJ, USA) we used in this patient is distinctive for its large-pore and monofilament technology [8] that together enable fluid to be easily drained through the mesh and keep bacteria from retaining and proliferating. There are still controversies in the management of bowel injury and the methods of hernia repair following the recognition of an enterotomy. Many surgeons are determined to proceed with hernia repair using a prosthetic mesh as planned if the contamination is minimal or absent [9,10]. Although we succeeded in this casein which the enterotomy was unrecognized initially, removal of the mesh was strongly recommended when a ruptured bowel and intestinal spillage were confirmed during the secondary laparotomy.
In summary, this is a rare case of "hernia within hernia" because of the large parastomal hernia sac and an adhesive band that extended from the hernia sac wall to distal colon and formed an internal hernia ring. It should be kept in mind that some serious complications may occur during the treatment of huge parastomal hernias. Prophylactic mesh fixed in a sublay position at primary abdomino-perineal resection and stoma formation procedure may lower the high incidence of parastomal hernia and consequent complications.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Israelsson LA. Parastomal hernias. Surg Clin North Am. 2008;88:113–125. doi: 10.1016/j.suc.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Seo SH, Kim HJ, Oh SY, Lee JH, Suh KW. Computed tomography classification for parastomal hernia. J Korean Surg Soc. 2011;81:111–114. doi: 10.4174/jkss.2011.81.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg. 2003;90:784–793. doi: 10.1002/bjs.4220. [DOI] [PubMed] [Google Scholar]
- 4.Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J, Darnell A, Mora-Lopez L, Alcantara-Moral M, et al. Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg. 2009;249:583–587. doi: 10.1097/SLA.0b013e31819ec809. [DOI] [PubMed] [Google Scholar]
- 5.Janes A, Cengiz Y, Israelsson LA. Preventing parastomal hernia with a prosthetic mesh: a 5-year follow-up of a randomized study. World J Surg. 2009;33:118–121. doi: 10.1007/s00268-008-9785-4. [DOI] [PubMed] [Google Scholar]
- 6.Allen-Mersh TG, Thomson JP. Surgical treatment of colostomy complications. Br J Surg. 1988;75:416–418. doi: 10.1002/bjs.1800750507. [DOI] [PubMed] [Google Scholar]
- 7.LeBlanc KA, Elieson MJ, Corder JM., 3rd Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: a review of the literature. JSLS. 2007;11:408–414. [PMC free article] [PubMed] [Google Scholar]
- 8.Berrevoet F, Fierens K, De Gols J, Navez B, Van Bastelaere W, Meir E, et al. Multicentric observational cohort study evaluating a composite mesh with incorporated oxidized regenerated cellulose in laparoscopic ventral hernia repair. Hernia. 2009;13:23–27. doi: 10.1007/s10029-008-0418-5. [DOI] [PubMed] [Google Scholar]
- 9.Franklin ME, Jr, Gonzalez JJ, Jr, Glass JL, Manjarrez A. Laparoscopic ventral and incisional hernia repair: an 11-year experience. Hernia. 2004;8:23–27. doi: 10.1007/s10029-003-0163-8. [DOI] [PubMed] [Google Scholar]
- 10.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years' experience with 850 consecutive hernias. Ann Surg. 2003;238:391–399. doi: 10.1097/01.sla.0000086662.49499.ab. [DOI] [PMC free article] [PubMed] [Google Scholar]