Abstract
Background
Little is known about the relative impact of different mental disorders on adult quality of life (QOL). This study estimated associations between several mental disorders and QOL in a representative American community sample.
Methods
The QOL instrument was administered to 640 adult participants in the Children in the Community Study, a population-based longitudinal study. DSM-Axis I and Axis II mental disorder diagnoses were assessed by psychiatric interview.
Results
Poorer QOL was strongly associated with having a mood disorder, especially major depression disorder (MDD) (effect size, ES = −0.57, p <0.01), whereas poorer quality social relationships were associated with having dysthymia and bipolar disorders (ES = −0.92, p<0.01; ES = −0.80, p <0.05, respectively). Most anxiety disorders were not independently related to QOL with the exception of post traumatic stress disorder (PTSD), which was significantly related to poorer physical health (ES = −0.78, p <0.01) and psychological well-being (ES = −0.73, p <0.01) and to less overall QOL (ES = −0.57, p <0.01).
Conclusions
MDD and PTSD are independently related to impaired QOL and dysthymia and bipolar disorder negatively influence social relationships.
Keywords: Depression, Anxiety, Quality of Life, Personality Disorder
1. Introduction
The concept of quality of life (QOL) covers a range of objective and subjective domains that reflect an individual’s global physical and mental well-being, including family and social relations, scholastic and work function, financial and health status, and living situation (Lochner et al., 2003). The relationship between Axis I mental disorder and QOL has been examined in many research studies, with findings suggesting that disorder is associated with impaired QOL. A number of studies have established that individuals with major depression disorder (MDD) experience significant disability and poorer QOL (Papakostas et al., 2004). Dysthymia also has been associated with loss of QOL and an annual loss of quality-adjusted life years (Saarni et al., 2006, 2007). Four studies have compared QOL in individuals with bipolar disorder to individuals in a general population sample; not surprisingly, those with bipolar disorder scored significantly lower in QOL (Arnold et al., 2000; Goossens et al., 2008; Kebede et al., 2006; Sierra et al., 2005). Even in the stable phase of bipolar disorder, patients still experienced lower functioning and well-being than individuals in the general population (Sierra et al., 2005).
Although fewer studies have addressed impaired QOL in individuals with anxiety disorders than in individuals with mood disorders (Mogotsi et al., 2000), interest in the impact of anxiety disorders on QOL is growing. Persons with panic disorder scored in the impaired range (relative to general population norms) on all subscales of the SF-36 (Candilis et al., 1999; Ettigi et al., 1997), whereas those with generalized anxiety disorder (GAD) and social phobia showed the largest loss of EQ-5D and 15D scores (Saarni et al., 2007). Patients with obsessive compulsive disorder (OCD) were shown to be substantially impaired in 16 life domains, and particularly in the areas of self-esteem and work (Norberg et al., 2008). Much of the community data on QOL and PTSD is based on military veteran populations, a large proportion of which report problems in employment, lower work functioning, worse physical health, poorer subjective well-being, higher levels of impairment in interpersonal relationship, marital and family difficulties, and more exposure to violence (Engelhard et al., 2007; Jordan et al., 1992; Rona et al., 2009; Zatzick et al., 1997a, 1997b). These findings suggest that anxiety disorders have a negative impact on QOL in a number of areas. Several studies have compared QOL in subjects with substance use disorders to general population norms for QOL (Daeppen et al., 1998; Morgan et al., 2004; Smith and Larson, 2003). Alcohol dependent patients reported poorer QOL, especially in psychological and role dimensions (Daeppen et al., 1998), social functioning, and in limitations in physical and emotional roles (Morgan et al., 2004). Substance abusers had much lower mean scores than was indicated in general population norms on both the SF-12 mental health and physical health component scales (Smith and Larson, 2003).
While QOL impairment has been established with each of the individual Axis I disorders, relatively less research has focused on comparing QOL impairment among the Axis I disorders (Cramer et al., 2007; Sanderson and Andrews, 2002). Moreover, despite the high rate of concurrence among persons with Axis I disorders, personality disorders (PDs) have generally been ignored in such QOL studies (Chen et al., 2006a, 2006b). The rates of PDs in Axis I patients have varied across studies, but are consistently quite high (Echeburua et al., 2007; Grant et al., 2005; Kantojarvi et al., 2006). Further, individuals with an Axis I disorder and comorbid PD were reported to have a poorer QOL compared to individuals with Axis I disorders without PD in both cross-sectional and longitudinal studies (Chen, et al., 2006a, 2006b, 2009; Newton-Howes et al., 2006). The aim of the present study was to examine and compare the relative impact of common Axis I disorders on QOL net of the effects of relevant demographic variables, physical illnesses and PDs in a community adult sample.
2. Methods
2.1 Participants and procedures
This study examined longitudinal data from the Children in the Community Study, an ongoing investigation of childhood behavior and development based on a sample of families randomly selected in 1975 on the basis of residence in 2 upstate New York counties (Cohen and Cohen, 1996). Approximately 800 mothers and 1 randomly sampled child from each family (mean ± SD age, 5.5 ± 2.8 years; in 1975) have been re-interviewed in their homes by extensively trained and supervised lay interviewers in a series of follow-up surveys during the past 30 years. These families were generally representative of families in the northeastern United States with regard to most demographic variables (e.g., socioeconomic status). However, the sample also reflects the relatively high proportion of Catholic (54%) and white (91%) residents living in the sampled region. Details of sampling, comparison with population, and retention rates are provided on the study website (www.nyspi.org/childcom). Earlier retention rates of 95% have dropped as the cohort became adults, especially among male participants; this problem is shared by virtually all other recent longitudinal studies of community and clinical samples.
The present study focuses on the 640 participants who were fully assessed in 2001–2004 at ages 28 to 40 (mean age=33; SD=2.9). After home interviews assessing a wide range of psychosocial variables had been completed, psychiatric interviews were administered over the telephone by professionals with advanced degrees in social work or clinical psychology and extensive experience in semi-structured psychiatric research interviews. Study procedures were approved in accordance with appropriate institutional guidelines by the Institutional Review Boards of the Columbia University College of Physicians and Surgeons and the New York State Psychiatric Institute. A National Institute of Health Certificate of Confidentiality has been obtained for study data. Written informed consent was obtained from all participants after the interview procedures were fully explained. Additional information regarding the study methodology is available from previous reports (Cohen and Cohen, 1996; Cohen et al., 1987a, 1987b; Kogan et al., 1977) and on the study website (www.nyspi.org/childcom).
2.2 Measures
2.2.1 Axis I disorders
Axis I disorders at mean age 33 years were assessed with the non-patient version of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-IV/NP, First et al., 2000). The SCID-IV/NP was used to identify those who had experienced Axis I disorders including substance use disorders (alcohol use disorders, drug use disorders), mood disorders (MDD, dysthymic disorder, bipolar disorder), and anxiety disorders (panic disorder, agoraphobia, OCD, social phobia, GAD, PTSD).
2.2.2 Personality disorders
The Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II, First et al., 1997) first was used in this sample to assess PDs at mean age 33 years. The SCID-II is a two-stage diagnostic procedure which includes a screening questionnaire, followed by a semi-structured interview to determine whether affirmative responses on the questionnaire indicate the presence of clinically significant symptoms. The SCID-II interview test-retest reliability has been found to be satisfactory: K=0.51 for “any personality disorder”' in patients and K=0.48 in non-patients (First et al., 1995). Interrater reliability was satisfactory for any personality disorder: K=0.62 (Crawford et al, 2005). The following PDs were included in this study: paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, avoidant, obsessive-compulsive, dependent, depressive and passive-aggressive PDs.
2.2.3 Self-reported physical illnesses
Interviews also covered physical illness in the past year, including musculoskeletal diseases (orthopedic problems or chronic pain or arthritis or gout), neurologic diseases (migraine or other chronic headaches or epilepsy or other neurologic problems), severe allergy, respiratory disease (asthma, chronic bronchitis, emphysema or pneumonia), chronic skin problems, chronic gastrointestinal problems, urinary problems, cardiovascular diseases (heart disease, other vascular problem or hypertension), severe visual impairment, cancer, diabetes and mononucleosis. For each physical illness, we asked participants, “Have you ever suffered from this problem?”, “How much of the past year did this bother you?” and “in the past year did this limit your activities?”
2.2.4 Quality of life
At mean age 33 the Quality of Life Instrument for Young Adults (YAQOL) (Chen et al., 2004, 2006a, 2006b, 2009) assessed five QOL domains. The physical health domain was measured with eight items that assessed overall health, incapacitation due to illness, and energy level. The social relationships domain was measured with nine items covering the extent of contact and quality of relationships and a second 9-item scale that assessed the quality of relationship with a partner or close confidante. The psychological well-being domain is composed of two scales: positive outlook on the future (5 items) and negative affect (5 items, scored for low frequency). The role function domain was measured with four scales that assess stress in a major productive role (employment, school, and home) due to excessive demand, conflict, safety, or health risk (6 items); degree of influence over role organization, scheduling, and decisions (5 items); role satisfaction and consistency with long-term goals (5 items); and role morale of coworkers or other students (6 items).The environmental context domain is composed of four scales assessing home quality, including comfort, safety, quietness, and privacy (9 items); community quality including social and service aspects of the neighborhood context (8 items); mobility of ease of access to work, school, shopping, leisure, and social activities settings (6 items); and resources assessing the adequacy of access to dental, medical and related services, and financial support. Internal consistency reliability of the YAQOL ranged from 0.88 to 0.63 (mean, 0.73). Detailed information regarding the reliability and validity of YAQOL is available in a previous report (Chen et al., 2004).To enhance interpretability and comparability among these scales, rescaling defined the minimum possible score as 0 and the maximum possible score as 100, with higher scores indicating better QOL.
2.3 Statistical analysis
Linear regression analyses were conducted to investigate the associations between adulthood Axis I disorders and QOL. All analyses controlled for demographic variables (sex, race, family socioeconomic status, earned income, marital status, and education) because there are significant variations in aspects of QOL for those groups (Cramer et al., 2007; Sanderson and Andrews, 2002). Unstandardized regression coefficients were interpreted as the mean difference (MD) on each QOL domain score between those with an Axis I disorder and those without an Axis I disorder (reference group, n=457) after adjusting for all demographic variables, physical illnesses and comorbid personality disorders in the equation. Regression analyses that adjusted for Axis I disorder comorbidity also were conducted to identify the independent association of each disorder with each of the QOL domains. The reference group was composed of participants without the disorder being examined. Effect sizes (ES) of 0.20, 0.50, and 0.80 or greater often are considered small, moderate, and large, respectively (Cohen, 1988).
3. Results
3.1 Sample characteristics and prevalence of disorders
Participants were on average age 33 and 47.2% male; 91% were Caucasian and the remainder were Black Americans. They had been raised in urban areas (64.5%), as well as in suburban, small town and rural areas. Two thirds had some post high school education; 56% were married or cohabiting; and 87.3% were currently employed. Median income was $25,000–$34,999 per year. Sixty-two percent of the sample had an income over $25,000, with 21.5% reporting income over $50,000. Mean QOL domain scores were 67.4, 77.4, 80.1, 63.7, and 75.2 for physical health, social relationships, psychological well-being, role function and environmental context, respectively.
One hundred eighty-three subjects (28.6%) met the criteria for at least one Axis I disorders. Substance-use disorders were the most prevalent (13.3%), followed by mood (13.1%) and anxiety disorders (12.7%). The prevalence of specific Axis I disorders ranged from 12.2% to 1.6%. Major depressive disorder (12.2%) was the most prevalent diagnosis followed by an alcohol use disorder (11.2%); all other Axis I disorders each were diagnosed in less than 5% of the sample. Additionally, 71 (11.1%) participants had more than two Axis I disorders; 102 (15.9%) had at least one personality disorder; 58 (9.1%) had co-morbid Axis I and personality disorders; and 123 (19.2%) had concurrent Axis I disorders and physical illnesses.
3.2 Association of QOL impairment with specific axis I disorders
The mean QOL score for participants with an Axis I disorder was calculated and compared with the mean QOL score for 457 participants without any Axis I disorder. Table 1 presents the mean difference in QOL scores in relation to each specific Axis I disorder, adjusted by regression analysis for all demographic variables, physical illnesses and personality disorders comorbidity, demonstrating the severity of impairment compared to those without Axis I disorders.
Table 1.
QOL scores (mean differences) of individuals with and without each Axis I disorder at mean age 33 (N=640)
| Axis I Disorders | No. (%) of participants |
Physical Health |
Social Relationship |
Psychological Well-being |
Role Function |
Environmental Context |
|---|---|---|---|---|---|---|
| No Axis I disorder Mean (SD) |
457 |
70.0(17.3) |
79.1(10.5) |
83.2(11.7) |
65.1(15.2) |
76.7(8.9) |
| Alcohol use | 72(11.2) | −5.3* | −4.1** | −6.3*** | −3.8 | −4.5*** |
| Drug use | 24(3.8) | −2.8 | −3.2 | −1.4 | −2.5 | −3.2 |
| MDD | 78(12.2) | −13.9*** | −5.2*** | −13.3*** | −3.2 | −5.0*** |
| Dysthymia | 14(2.2) | −13.3** | −16.5*** | −21.0*** | 0.1 | −3.8 |
| Bipolar | 10(1.6) | −15.8**) | −18.4*** | −22.1*** | −1.3 | −11.5*** |
| Panic | 29(4.5) | −16.3*** | −7.4** | −11.6*** | 2.3 | −4.4* |
| GAD | 16(2.5) | −15.4** | −11.3*** | −13.8*** | −2.4 | −6.3** |
| OCD | 26(4.1) | −12.6** | −8.7*** | −13.4*** | −3.6 | −5.3** |
| Agoraphobia | 28(4.4) | −12.0** | −10.8*** | −13.7*** | −1.6 | −4.9** |
| Social phobia | 24(3.8) | −4.9 | −7.4** | −8.6** | 3.9 | −3.5 |
| PTSD | 17(2.7) | −21.5** | −8.8** | −20.8*** | −0.2 | −2.4 |
| Any Axis I disorder | 183(28.6) | −8.8*** | −4.0*** | −8.2*** | −3.2* | −4.0*** |
Separate regression analyses for each QOL domain score in patients with each disorder compared with the 457 participants with no Axis I disorders, adjusted for all demographic variables, any physical illness and personality disorder.
p<0.05;
p <0.01;
p <0.001
As compared to those without Axis I disorders, participants with an Axis I disorder had lower scores across the five domains of covered by the QOL scales. Each Axis I disorder produced a distinctive pattern of impairment in QOL. With the exception of drug use disorders, all disorders were associated with impaired QOL in at least two and up to four domains (Table 1). Participants diagnosed with an alcohol use disorder, MDD, bipolar disorder, panic disorder, GAD, OCD, or agoraphobia had a significantly lower score on physical health, social relationship, psychological well-being and environmental context. Having PTSD was related to poorer physical status, dysfunctional social relationships and poorer psychological well-being. Participants with dysthymia disorder and social phobia reported a problematic social relationship and poorer psychological well-being; in addition, dysthymia was associated with poorer physical status.
3.3 Independent effect of Axis I disorders on five QOL domains
Regression analyses were adjusted for all demographic variables, comorbid physical illnesses, Axis I disorders and personality disorder to identify the independent association of Axis I disorder with each of the QOL domains and QOL overall scores (Table 2). The effect size (ES) is the mean difference in QOL score between participants with and without the Axis I disorder divided by the standard deviation of the QOL score in the total sample. It should be noted that whereas in Table 1 all subjects with an Axis I disorder were contrasted to the same reference group (participants without any Axis I disorder, n=457), in Table 2 the reference group was composed of participants without the Axis I disorder being examined.
Table 2.
QOL of individuals with each Axis I disorder net of demographic, physical illness and comorbid Axis I and personality disorder
| Physical Health |
Social Relationships |
Psychological Well-being |
Role Function |
Environmental Context |
|
|---|---|---|---|---|---|
| Alcohol use | −0.16 | −0.21 | −0.28* | −0.20 | −0.33** |
| Drug use | 0.12 | 0.03 | 0.41* | −0.03 | 0.05 |
| MDD | −0.55** | −0.14 | −0.70** | −0.17 | −0.42** |
| Dysthymia | 0.04 | −0.92** | −0.66** | −0.08 | −0.05 |
| Bipolar | 0.18 | −0.80* | −0.54 | −0.02 | −0.74* |
| Panic | −0.38 | 0.01 | −0.05 | 0.27 | 0.01 |
| GAD | −0.17 | 0.07 | 0.25 | −0.07 | 0.11 |
| OCD | −0.18 | −0.20 | −0.24 | −0.29 | −0.10 |
| Agoraphobia | −0.15 | −0.34 | −0.29 | −0.19 | −0.13 |
| Social phobia | 0.37 | −0.16 | 0.17 | 0.38 | 0.09 |
| PTSD | −0.78** | −0.07 | −0.73** | 0.03 | 0.29 |
Each disorder is compared with participants without that disorder.
Separate regression analyses for QOL scores net of other Axis I disorders, PD, demographic risk and physical illness.
p <0.05;
p <0.01
After adjusting for all demographic variables, physical illnesses, and co-morbidity with any other mental disorder, the negative effect of many Axis I disorders was diminished, especially among anxiety disorders, although PTSD still showed a negative effect on physical health (ES =−0.78, p =0.001) and psychological well-being (ES =−0.73, p =0.001). Those with an alcohol use disorder had poorer psychological well-being (ES =−0.28, p =0.015) and more adverse environmental contexts (ES =−0.33, p = 0.006); in contrast, having a drug use disorder appeared to protect psychological well-being (ES =0.41, p =0.026). Independent MDD effects were found for the domains of physical health (ES =−0.55, P<0.001), psychological well-being (ES =−0.70, p<0.001) and environmental context (ES =−0.42; p =0.001). Dysthymia and bipolar disorders had significantly large effects on social relationships (ES =−0.92, p =0.001; ES =−0.80, p =.019, respectively). Additionally, dysthymia was related to poorer psychological health (ES =−0.66, p =0.009), and bipolar disorder was related to a more adverse environmental context (ES =−0.74, p=0.029).
3.4 Axis I disorders and overall QOL
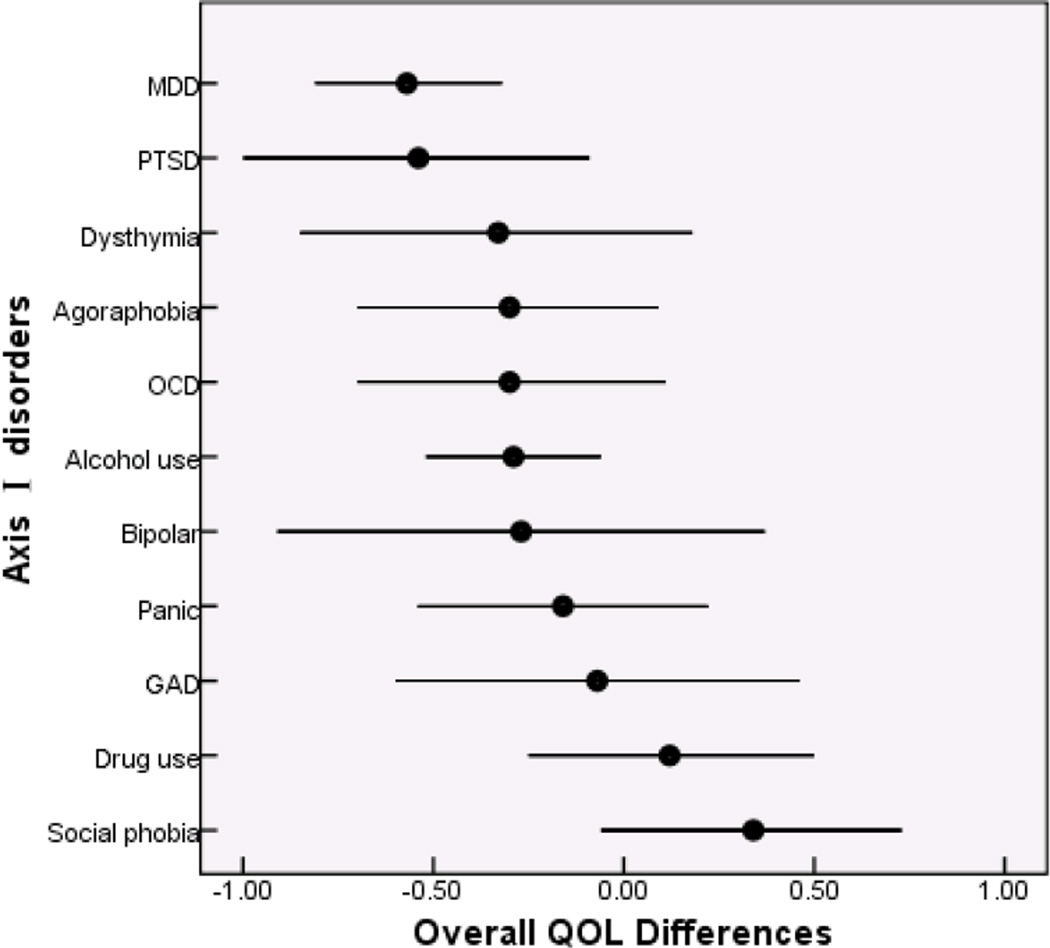
We examined the unique associations between overall QOL and eleven individual Axis I disorders. MDD, PTSD and alcohol use disorders were independently associated with significantly elevated impairment in overall QOL, with ESs ranging from −0.57 to −0.29 (p<0.05). Effects of dysthymia, agoraphobia, OCD, bipolar disorder, panic disorder, and GAD were in the same direction with reduced overall QOL, but did not reach statistical significance (ES from −0.30 to −0.07). Drug use disorders and social phobia were related to better overall QOL, but did not reach statistical significance (ES from 0.12 to 0.34) (Table 3 and Figure 1).
Table 3.
Overall quality of life net of demographic, physical illness and comorbid Axis I and personality disorder
| Disorders | Effect Size | 95% Confidence Interval |
|---|---|---|
| MDD | −0.57** | −0.81 ~ −0.32 |
| PTSD | −0.54* | −1.00 ~ −0.09 |
| Dysthymia | −0.33 | −0.85 ~ 0.18 |
| Agoraphobia | −0.30 | −0.70 ~ 0.09 |
| OCD | −0.30 | −0.70 ~ 0.11 |
| Alcohol use | −0.29* | −0.52 ~ −0.06 |
| Bipolar | −0.27 | −0.91 ~ 0.37 |
| Panic | −0.16 | −0.54 ~ 0.22 |
| GAD | −0.07 | −0.60 ~ 0.46 |
| Drug use | 0.12 | −0.25 ~ 0.50 |
| Social phobia | 0.34 | −0.06 ~ 0.73 |
Each disorder is compared with participants without that disorder.
Separate regression analyses for overall QOL score net of other Axis I disorders, PD, demographic risk and physical illness.
p <0.05;
p <0.01
Figure 1.
Mean effects per Axis I disorders (and 95% confidence interval) with overall quality of life (QOL) at mean age 33
4. Discussion
We estimated the relative impact of major DSM-IV Axis I disorders on QOL in an American adult sample, assessed between the ages of 28 and 40. QOL was measured with the YAQOL instrument, which is able to estimate the multi-dimensions of QOL, including physical status, quality of relationship, positive outlook and negative affect, social role function, and environmental context.. The major findings of the present study were as follows: (1) poorer QOL was associated with having a current DSM-IV Axis I disorders when compared to having no Axis I disorders; (2) mood disorders were strongly associated with poorer QOL, especially MDD with overall QOL, and dysthymia and bipolar disorders with social relationship; (3) most anxiety disorders were not independently related to QOL except for PTSD, which was negatively associated with physical health status, psychological well-being and overall QOL; (4) drug use disorders had a small but significant positive association with psychological well-being.
Whether comorbidity among the Axis I disorders was controlled or not, MDD, dysthymia and bipolar disorders all were associated with diminished QOL in several domains. The negative effect of MDD and dysthymia on psychological well-being was moderate. Similarly, the negative effect of bipolar disorder on environmental context also was moderate, and the effect of MDD on environmental context was small. MDD was the only mood disorder independently associated with a poorer physical health. Furthermore, MDD was associated with the largest decrement in overall QOL. Two similar studies reported an inverse relation between MDD and global QOL net of controls that included personality disorders (Cramer et al., 2007; Sanderson & Andrews, 2002): Cramer et al (2007) also found an independent negative effect of dysthymia disorder on global QOL; however neither study observed an association between bipolar disorder and any specific aspect of QOL or global QOL. Although in our study dysthymia and bipolar disorders did not significantly affect overall QOL independent of controls, both disorders were independently associated with the greatest loss of social relationship, even more so than MDD.
Previous studies have suggested that differences in overall QOL are not attributable to anxiety disorders (Barrera and Norton, 2009; Lochner et al., 2003; Olatunji et al., 2007). In the present study, when compared to individuals with no Axis I disorders, individuals with all but one anxiety disorder (social phobia) showed compromised overall QOL and lower scores across comprehensive domains. Social phobia, on the other hand, was associated with poorer social problems and worse psychological well-being. Although no independent effect of anxiety disorders except PTSD could be found on overall QOL net of comorbidity, there still are differences in effect sizes. The number of samples for many of the specific Axis I disorder is small, whereas the finding does hint that PTSD play a prominent role in impairing QOL among anxiety disorders, with subjects with PTSD reporting severe problems in relation to physical health and psychological well-being even after controlling for comorbidity. This suggestive finding seems to fit well with current research. For example, Olatunji used meta-analysis as a tool and found that more QOL impairment is reported by patients with PTSD (Olatunji et al., 2007).
In general our data suggest that after controlling for demographic variables, co-morbidity among physical illness, personality disorder, and Axis I disorders negatively influence the QOL of American adults. MDD and PTSD are independently related to decreased overall QOL and dysthymia and bipolar disorders are strongly associated with a lower quality of social relationships; whereas drug use disorder appears to be related to increased positive outlook and reduced negative affect in this age group American adults. Our findings complement other evidence concerning impairment associated with Axis I disorders and would be useful in developing and improving comprehensive programs of treatment and counseling that focus on both psychiatric disorders and functional disability. Additionally, these findings would be especially helpful for improving the QOL of targeted American adults with Axis I disorders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arnold LM, Witzeman KA, Swank ML, McElroy SL, Keck PE., Jr Health-related quality of life using the SF-36 in patients with bipolar disorder compared with patients with chronic back pain and the general population. J. Affect. Disord. 2000;57:235–239. doi: 10.1016/s0165-0327(99)00042-7. [DOI] [PubMed] [Google Scholar]
- Barrera TL, Norton PJ. Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. J. Anxiety. Disord. 2009;23:1086–1090. doi: 10.1016/j.janxdis.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candilis PJ, McLean RY, Otto MW, Manfro GG, Worthington JJ, 3rd, Penava SJ, Marzol PC, Pollack MH. Quality of life in patients with panic disorder. J. Nerv. Ment. Dis. 1999;187:429–434. doi: 10.1097/00005053-199907000-00006. [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Kasen S, Gordan K, Dufur R, Smailes E. Construction and validation of a quality of life instrument for young adults. Qual. Life Res. 2004;13:747–759. doi: 10.1023/B:QURE.0000021700.42478.ab. [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Kasen S, Johnson JG. Adolescent axis I and personality disorders predict quality of life during young adulthood. J. Adolesc. Health. 2006a;39:14–19. doi: 10.1016/j.jadohealth.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Kasen S, Johnson JG, Berenson K, Gordon K. Impact of adolescent mental disorders and physical illnesses on quality of life 17 years later. Arch. Pediatr. Adolesc. Med. 2006b;160:93–99. doi: 10.1001/archpedi.160.1.93. [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Crawford TN, Kasen S, Guan B, Gorden K. Impact of early adolescent psychiatric and personality disorder on long-term physical health: a 20-year longitudinal follow-up study. Psychol. Med. 2009;39:865–874. doi: 10.1017/S0033291708004182. [DOI] [PubMed] [Google Scholar]
- Cohen P, O'Connor P, Lewis S, Velez CN, Malachowski B. Comparison of DISC and K-SADS-P interviews of an epidemiological sample of children. J. Am. Acad. Child. Adolesc. Psychiatry. 1987a;26:662–667. doi: 10.1097/00004583-198709000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen P, Velez N, Kohn M, Schwab-Stone M, Johnson J. Child psychiatric diagnosis by computer algorithm: theoretical issues and empirical tests. J. Am. Acad. Child. Adolesc. Psychiatry. 1987b;26:631–638. doi: 10.1097/00004583-198709000-00004. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Life Values and Adolescent Mental Health. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Mahwah, NJ: Lawrence Erlbaum Association, Inc.; 1988. [Google Scholar]
- Cramer V, Torgersen S, Kringlen E. Socio-demographic conditions, subjective somatic health, Axis I disorders and personality disorders in the common population: the relationship to quality of life. J. Pers. Disord. 2007;21:552–567. doi: 10.1521/pedi.2007.21.5.552. [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Johnson JG, Kasen S, First MB, Gordon K, Brook JS. Self-reported personality disorder in the children in the community sample: convergent and prospective validity in late adolescence and adulthood. J. Pers. Disord. 2005;19:30–52. doi: 10.1521/pedi.19.1.30.62179. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Krieg MA, Burnand B, Yersin B. MOS-SF-36 in evaluating health-related quality of life in alcohol-dependent patients. Am. J. Drug Alcohol Abuse. 1998;24:685–694. doi: 10.3109/00952999809019617. [DOI] [PubMed] [Google Scholar]
- Echeburua E, De Medina RB, Aizpiri J. Comorbidity of alcohol dependence and personality disorders: a comparative study. Alcohol Alcohol. 2007;42:618–622. doi: 10.1093/alcalc/agm050. [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, Weerts J, Arntz A, Hox JJ, McNally RJ. Deployment-related stress and trauma in Dutch soldiers returning from Iraq. Prospective study. Br. J. Psychiatry. 2007;191:140–145. doi: 10.1192/bjp.bp.106.034884. [DOI] [PubMed] [Google Scholar]
- Ettigi P, Meyerhoff AS, Chirban JT, Jacobs RJ, Wilson RR. The quality of life and employment in panic disorder. J. Nerv. Ment. Dis. 1997;185:368–372. doi: 10.1097/00005053-199706000-00002. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Davies M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B. The structured clinical interview for DSM-III-R personality disorders (SCID-II). Part II: Multi-site test-retest reliability study. J. Pers. Disord. 1995;9:92–104. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User's guide for the Structured Clinical Interview for the DSM-IV Personality Disorders. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, non-patient version (SCID-IV-NP) New York, NY: New York State Psychiatric Institute; 2000. [Google Scholar]
- Goossens PJ, Hartong EG, Knoppert-van der Klein EA, van Achterberg T. Self-reported psychopathological symptoms and quality of life in outpatients with bipolar disorder. Perspect. Psychiatr. Care. 2008;44:275–284. doi: 10.1111/j.1744-6163.2008.00187.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Patricia Chou S, June Ruan W, Huang B. Co-occurrence of 12-month mood and anxiety disorders and personality disorders in the US: results from the national epidemiologic survey on alcohol and related conditions. J. Psychiatr. Res. 2005;39:1–9. doi: 10.1016/j.jpsychires.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS. Problems in families of male Vietnam veterans with posttraumatic stress disorder. J. Consult. Clin. Psychol. 1992;60:916–926. doi: 10.1037//0022-006x.60.6.916. [DOI] [PubMed] [Google Scholar]
- Kantojarvi L, Veijola J, Laksy K, Jokelainen J, Herva A, Karvonen JT, Kokkonen P, Jarvelin MR, Joukamaa M. Co-occurrence of personality disorders with mood, anxiety, and substance use disorders in a young adult population. J. Pers. Disord. 2006;20:102–112. doi: 10.1521/pedi.2006.20.1.102. [DOI] [PubMed] [Google Scholar]
- Kebede D, Alem A, Shibire T, Deyassa N, Negash A, Beyero T, Medhin G, Fekadu A. Symptomatic and functional outcome of bipolar disorder in Butajira, Ethiopia. J. Affect. Disord. 2006;90:239–249. doi: 10.1016/j.jad.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Kogan LS, Smith J, Jenkins S. Ecological validity of indicator data as predictors of survey findings. J. Soc. Serv. Res. 1977;1:117–132. [Google Scholar]
- Lochner C, Mogotsi M, du Toit PL, Kaminer D, Niehaus DJ, Stein DJ. Quality of life in anxiety disorders: a comparison of obsessive-compulsive disorder, social anxiety disorder, and panic disorder. Psychopathology. 2003;36:255–262. doi: 10.1159/000073451. [DOI] [PubMed] [Google Scholar]
- Mogotsi M, Kaminer D, Stein DJ. Quality of life in the anxiety disorders. Harv. Rev. Psychiatry. 2000;8:273–282. [PubMed] [Google Scholar]
- Morgan TJ, Morgenstern J, Blanchard KA, Labouvie E, Bux DA. Health-related quality of life for adults participating in outpatient substance abuse treatment. Am. J. Addict. 2003;12:198–210. [PubMed] [Google Scholar]
- Morgan MY, Landron F, Lehert P. Improvement in quality of life after treatment for alcohol dependence with acamprosate and psychosocial support. Alcohol. Clin. Exp. Res. 2004;28:64–77. doi: 10.1097/01.ALC.0000108652.73143.4B. [DOI] [PubMed] [Google Scholar]
- Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br. J. Psychiatry. 2006;188:13–20. doi: 10.1192/bjp.188.1.13. [DOI] [PubMed] [Google Scholar]
- Norberg MM, Calamari JE, Cohen RJ, Riemann BC. Quality of life in obsessive-compulsive disorder: an evaluation of impairment and a preliminary analysis of the ameliorating effects of treatment. Depress. Anxiety. 2008;25:248–259. doi: 10.1002/da.20298. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: a meta-analytic review. Clin. Psychol. Rev. 2007;27:572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Papakostas GI, Petersen T, Mahal Y, Mischoulon D, Nierenberg AA, Fava M. Quality of life assessments in major depressive disorder: a review of the literature. Gen. Hosp. Psychiatry. 2004;26:13–17. doi: 10.1016/j.genhosppsych.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Rona RJ, Jones M, Iversen A, Hull L, Greenberg N, Fear NT, Hotopf M, Wessely S. The impact of posttraumatic stress disorder on impairment in the UK military at the time of the Iraq war. J. Psychiatr. Res. 2009;43:649–655. doi: 10.1016/j.jpsychires.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Saarni SI, Harkanen T, Sintonen H, Suvisaari J, Koskinen S, Aromaa A, Lonnqvist J. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Qual. Life Res. 2006;15:1403–1414. doi: 10.1007/s11136-006-0020-1. [DOI] [PubMed] [Google Scholar]
- Saarni SI, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A, Lonnqvist J. Impact of psychiatric disorders on health-related quality of life: general population survey. Br. J. Psychiatry. 2007;190:326–332. doi: 10.1192/bjp.bp.106.025106. [DOI] [PubMed] [Google Scholar]
- Sanderson K, Andrews G. Prevalence and severity of mental health-related disability and relationship to diagnosis. Psychiatr. Serv. 2002;53:80–86. doi: 10.1176/appi.ps.53.1.80. [DOI] [PubMed] [Google Scholar]
- Sierra P, Livianos L, Rojo L. Quality of life for patients with bipolar disorder: relationship with clinical and demographic variables. Bipolar Disord. 2005;7:159–165. doi: 10.1111/j.1399-5618.2005.00186.x. [DOI] [PubMed] [Google Scholar]
- Smith KW, Larson MJ. Quality of life assessments by adult substance abusers receiving publicly funded treatment in Massachusetts. Am. J. Drug Alcohol Abuse. 2003;29:323–335. doi: 10.1081/ada-120020517. [DOI] [PubMed] [Google Scholar]
- Stein MD, Mulvey KP, Plough A, Samet JH. The functioning and well being of persons who seek treatment for drug and alcohol use. J. Subst. Abuse. 1998;10:75–84. doi: 10.1016/s0899-3289(99)80142-4. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Weiss DS, Marmar CR, Metzler TJ, Wells K, Golding JM, Stewart A, Schlenger WE, Browner WS. Post-traumatic stress disorder and functioning and quality of life outcomes in female Vietnam veterans. Mil. Med. 1997a;162:661–665. [PubMed] [Google Scholar]
- Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Stewart A, Schlenger WE, Wells KB. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am. J. Psychiatry. 1997b;154:1690–1695. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]