Abstract
Background
Alcohol consumption causes motor vehicle accident (MVA) injury in a dose-response fashion. However, the relationship between how this risk is different with respect to fatal and non-fatal outcomes is not clear. A meta-analysis has already been completed for alcohol and consumption and non-fatal MVA injury, but none exists for fatal injury. Thus, an analysis of the acute dose-response relationship between alcohol and motor vehicle injury death is warranted to generate single occasion- and dose-specific relative risks for the first time.
Methods
A systematic literature review and inverse-variance weighted, random effects meta-analysis was conducted to fill this gap. Fractional polynomial regression was used to model the dose-response relationship. Usual tests of heterogeneity and publication bias were run.
Results
Five studies meeting the inclusion criteria of this analysis were selected. At all levels of BAC, the odds ratio (OR) of fatal motor vehicle injury was significant. Overall, the 5 combined studies yielded an OR of fatal injury of 1.74 (95% CI: 1.43 – 2.14) for every 0.02% increase in BAC. At 0.08, the legal limit in most countries, the OR was 13.0 (95% CI: 11.1 – 15.2).
Conclusions
This study is able to definitively show and quantify, for the first time, the significantly increased OR for fatal motor vehicle injury. This analysis showed some evidence of both study heterogeneity and publication bias, likely due to the increased variation we could expect from a small study number. The alcohol-caused fatal motor vehicle injury literature is sparse with respect to dose-response information. More studies investigating this relationship and other injury types are recommended in this area to be able to calculate stable estimates of risk overall and by injury type specifically.
Keywords: alcohol, motor vehicle injury, mortality, risk, meta-analysis
Introduction
There is little doubt that alcohol consumption causes injury (Rehm et al., 2003). Alcohol has been shown to be causal for a wide range of injuries through a number of studies, including cross-sectional (Watt et al., 2005, Vingilis et al., 2007, Goodman et al., 1991, Malmivaara et al., 1993, Ivers et al., 2006), case-crossover (Borges et al., 2006, Vinson et al., 2003), and case-control analyses (Peck et al., 2008, Smith et al., 2001, Hingson and Howland, 1993). The most important relationship, however, from a burden of disease, risk relationship, and public health standpoint, is the risk of injury from alcohol-attributable motor vehicle accidents (MVA). Since the original Grand Rapids study of 1964 (Borkenstein et al., 1964) and the subsequent re-analyses from Hurst (Hurst et al., 1994), which resolved the famous Grand Rapids Dip in risk at low alcohol blood alcohol concentration (BAC) levels, this relationship has been characterized by a linear, dose-response relationship. It has persisted throughout time (Borkenstein et al., 1964, Anda et al., 1988), in different countries and cultures (Fabbri et al., 2001, Kasantikul et al., 2005), for the young and old, and men and women alike (Corrao et al., 1999, Taylor et al., 2010). Despite this, though, the field of alcohol consumption and motor vehicle injury is far from homogeneous. In particular, two problem areas exist: exposure measurement and outcome measurement. The first pertains to the use of usual consumption patterns to assess the risk of injury, which is in direct opposition to the model of acute alcohol consumption causing harm i.e. information on usual consumption patterns does not capture the influence of alcohol on a particular episode of injury. What’s more, it may not even relate to the event when the injury occurred and, even when acute exposure is measured and we can be certain the alcohol consumption occurred prior to the injury, many studies only report a dichotomous (YES/NO) measure of alcohol consumption, which does not permit risk curve generation. The second gap in the literature reflects outcome measurement. This issue will be resolved by treating fatal and non-fatal injury as distinct outcomes. There is some literature that points to alcohol-attributable injury death having a higher dose-response risk than for non-fatal injury, particularly with respect to head injuries (Andelic et al., 2010, Cunningham et al., 2002, Golan et al., 2007) and this is certainly reflected in burden of disease estimates (Shield et al., 2010, Rehm et al., 2004, Lopez et al., 2006), but quantification of this mortality-specific dose-response risk curve is nonexistent for MVA mortality specifically. Dose-specific curves for non-fatal motor vehicle injury have been previously developed and published by our research group for non-fatal injury with some separation by injury type (Taylor et al., 2010), so the current work will aim to build on and add to this knowledge.
This systematic review and meta-analysis will fill a much-needed gap in the alcohol-injury literature by providing data that will enable the development of stable dose-response risk curves for alcohol consumption and MVA fatal injury where none currently exist.
Materials and Methods
This study was completed in four main phases: (1) the systematic search, (2) the data extraction, (3) the meta-analysis, and (4) the dose-response curve-generating step. Before these, however, it was necessary to identify key concepts and definitions of fatal injury outcomes. For completion of steps 3 and 4, the authors used STATA software version 10.1 (Stata Corporation, College Station, TX).
Case Definition
The definition of fatal injury was purposefully broad in the sense that no strict adherence to ICD codes or rigid diagnostic criteria was followed, since, at least in earlier phases of article selection, some studies only used qualitative descriptions of motor vehicle injury (e.g. “crash”, “accident”) while others used more traditional ICD-9 or ICD-10-based definitions. Most studies were either MVA studies based on roadside accident data (e.g. (Keall et al., 2004)), medical record/coroner’s file review (e.g. (Smith et al., 2001), or combination of the two (e.g. (Zador et al., 2000)).
Systematic Review
A systematic review of the literature published between 1 January, 1980 and 31 December, 2010 was completed. Databases queried were Medline, EMBASE, CINAHL, PubMED, Google Scholar, CABS, WHOLIST, SIGLE, ETOH, Alcohol in Moderation, and ISI Web of Science using a pre-defined key word algorithm. Initially, the search was quite relaxed in order to cast the widest net from which articles could be selected. It combined the search terms “alcohol” AND “case control” OR “case crossover” AND “risk” AND [“injury” OR specific outcomes: “motor vehicle accidents”], and was restricted to full articles (excluded reviews, editorials, and letters) of human studies only. After removing duplicate titles, suitable abstracts were selected from the total pool of identified citations and were excluded from further investigation if at least one of the following criteria were met:
No indication of any information pertaining to an association between alcohol and injury mortality
The study was NOT a case-control or cohort
Inappropriate exposure data: No dose-response information presented (e.g., “yes” versus “no” alcohol consumption was unacceptable in this case). All studies included in this review used BAC as the main measure of acute alcohol consumption.
The article did not measure fatal MVA injury specifically or did not specify only fatal MVA injury
Acute consumption immediately preceding the MVA fatal injury was not presented e.g. only average or some measure of usual consumption was used
In the event no abstract was available or existed, the full journal article was obtained and the abstract was reviewed and assessed based on the same criteria as the abstract selection phase. For non-English articles, a native speaker of the language in which the article was written completed the translation. For those abstracts selected for further investigation, the full article was obtained and judged based on the same five criteria. Only those articles that did NOT meet any of the five exclusion criteria were selected for data extraction and were included in the analysis portion of this study. Lastly, full reference lists of selected articles and key reviews were hand-searched to identify any studies that may have been missed in the systematic search.
Data extraction
Information about the level of alcohol exposures in each study, the number of cases at each exposure level, the total population at risk at each exposure level, the adjusted estimates of relative risk (RR) or odds ratios (OR), and the corresponding upper and lower 95% confidence intervals of the adjusted RR were all recorded. When ranges of BAC were given, the midpoint between the upper and lower bound was taken. In cases where no upper bound for the highest category existed, 75% of the length of the previous category range was added to the low bound and this measure was used.
Meta-analysis
Step 1: Once the data had been abstracted and inputted into Stata, log-linear dose- response models were generated for each single study using the glst command, which accounts for correlation among RRs within the same study due to the identical reference group (Orsini et al., 2006). The summary estimates for each study were then used as input into the metan command within Stata, but the non-summarized data was used for the curve-generating step.
Step 2: Quantifying the heterogeneity of risk estimates across all studies was important given the diversity of study methods, effect sizes, and controlled variables (Thompson, 1994). Heterogeneity was quantitatively assessed among studies by using both the Q statistic and the I2 statistic (Higgins and Thompson, 2002). To assess publication bias, two independent tests were used - Begg’s and Egger’s regression asymmetry test for publication (Begg and Mazumdar, 1994, Egger et al., 1997). This was done to investigate whether the existing literature was reflective of all studies (i.e. to assess whether the published literature is biased), including negative or null associations, as well as those reporting positive associations and high risk estimates. If the studies were found to be highly heterogeneous and a large amount of between-study variation existed, it would be important to account for this variation by using a random effects model. If the opposite were true, a fixed effects model may be justified (Field, 2001, Field, 2003).
-
Step 3: The meta-analysis step was the curve-generating step, using linear and first-order fractional polynomial regression of the inverse-variance weighted data to estimate a best fitting curve to the data according to Royston (Royston, 2000). First order fractional polynomials take the general form shown in Equation 1:
(Equation 1) (Equation 2) Where x is the alcohol exposure level (in BAC (g/dL%), P1 and P2 are the polynomial powers, and β1 and β2 are the corresponding coefficients. No intercept term exists since all models have a start point of Log RR = 0 (OR/RR = 1 at zero consumption). For first-order models, P1 takes values from −2 to +3 and for second order models, P1 or P2 can take on any of these values, for a total of 44 different possible models available to fit the dose-response data. For model fitting, models were tested systematically from least to most complicated (linear, first order, second order) using the GLST command in STATA (Orsini et al., 2006).
Best-fit curves or lines were assessed using standard goodness-of-fit statistics, with an emphasis on decreased deviance (gain) compared to the referent model. Comparisons of curves to determine the best fit were made using a Chi-square distribution, as recommended by Royston and Altman (Royston and Altman, 1994), using the linear (P = 1) as the referent for all first-order polynomials and the quadratic (P1 = 1, P2 = 2) as the referent for all second-order polynomials.
Results
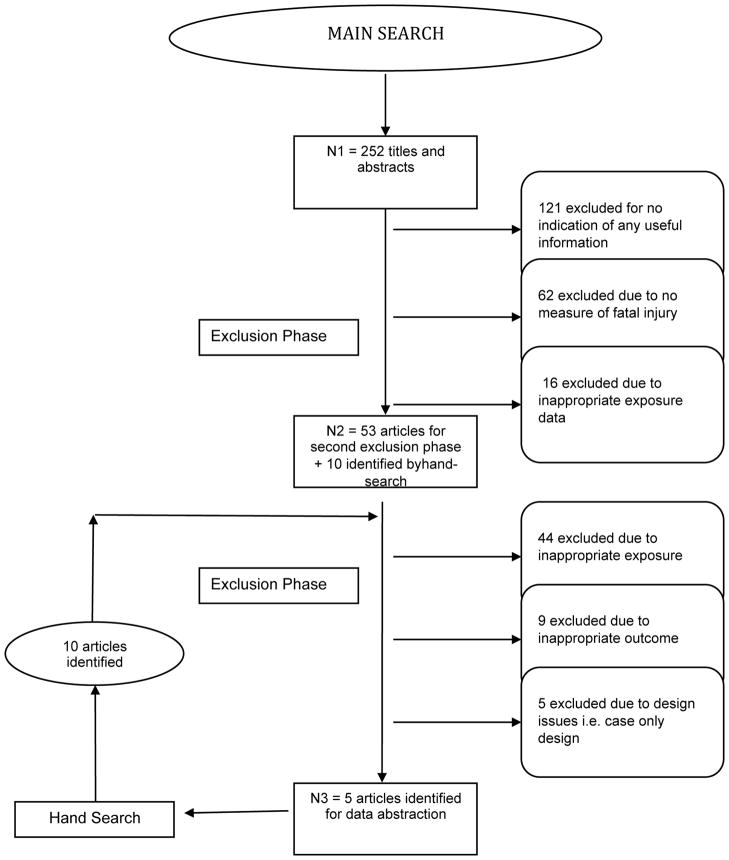
Figure 1 illustrates the search and article selection process, with numbers of articles retrieved in the main and hand searches and numbers discarded at the title/abstract and full article selection phases.
Figure 1.
Flowchart illustrating the sequential process and results of the systematic review of the relationship between alcohol and injury.
3.1. Systematic Review
The systematic review identified 5 articles (Zador et al., 2000, Keall et al., 2004, Smith et al., 2001, Evans and Frick, 1993a, Haworth, 2000) assessing the relationship between acute alcohol and fatal motor vehicle injury. One of the articles presented six separate analyses (Zador et al., 2000) by age and gender. Thus, overall, 10 datasets from the 5 articles were included in this meta-analysis (see Table 1 for a description of each study). All of the studies reported data on BAC and motor vehicle crashes except for one (Smith et al., 2001) which was a study of alcohol and boating fatalities.
Table 1.
Description of studies identified by the search that were included in the systematic review
| Study | Year | Location | Design | Injury Type | Cases | Controls | Age | Sex | Covariates Included |
|---|---|---|---|---|---|---|---|---|---|
| Smith et al. (Smith et al., 2001) | 2001 | United States | Case-control | Boating | 221 | 3943 | 43.5 | Both | 1, 2, 3, 4, 5, 6, 7 |
| Haworth et al.(Haworth, 2000) | 2000 | Australia | Case-control | MVA* | 114 | 847 | 27.5 | Both | 1, 2, 5, 6 |
| Keall et al. (Keall et al., 2004) | 2004 | New Zealand | Case-control | MVA | 85 | 85, 163 | 15+** | Both | CE*** |
| Zador et al. (M:16–20) (Zador et al., 2000) | 2000 | United States | Case-control | MVA | 432 | 609 | 16–20 | Men | CE |
| Zador et al. (M:21–34) (Zador et al., 2000) | 2000 | United States | Case-control | MVA | 1040 | 1652 | 21–34 | Men | CE |
| Zador et al. (M:35+) (Zador et al., 2000) | 2000 | United States | Case-control | MVA | 659 | 1508 | 35+ | Men | CE |
| Zador et al. (F:16–20) (Zador et al., 2000) | 2000 | United States | Case-control | MVA | 89 | 322 | 16–20 | Women | CE |
| Zador et al. (F:21–34) (Zador et al., 2000) | 2000 | United States | Case-control | MVA | 191 | 762 | 21–34 | Women | CE |
| Zador et al. (F:35+) (Zador et al., 2000) | 2000 | United States | Case-control | MVA | 134 | 702 | 35+ | Women | CE |
| Evans & Frick (Evans and Frick, 1993b) | 1993 | United States | Case-control | MVA | 307 | 1149 | N/A* | Both | CE |
MVA = motor vehicle accident
not reported or estimable
CE = crude estimate only, unadjusted
Covariates: 1: age, 2: sex, 3:race 4: other occupants 5: time of day 6: location 7:weekday/weekend
3.2. Meta-analysis
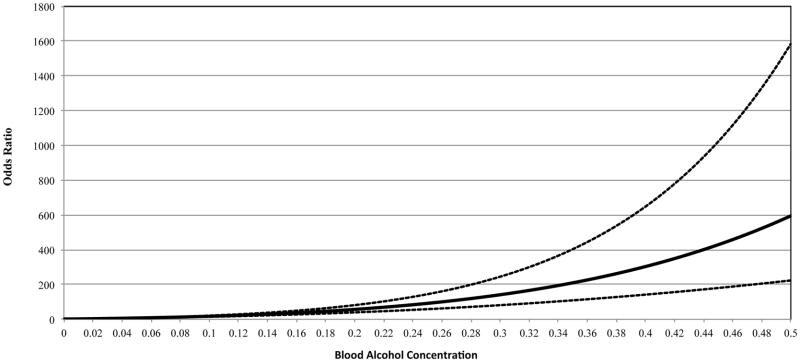
Figure 2 shows the forest plot of the relative contributions of each study to the pooled estimate, which estimated that the odds of fatal motor vehicle injury increased by 1.74 (95% CI: 1.43 – 2.14) for every 0.02 % increase in BAC. The assessment of heterogeneity for all studies indicated significant heterogeneity between these studies (Q-statistic = 1504.5 df = 9 I2 = 99.4% p < 0.0001), which was acceptable given the small number of studies and their widely varying collection methods. The meta-analysis was run as a random effects model in order to account for this variability. Publication bias was detected by the Begg’s (p = 0.421) and Egger’s (p = 0.032) tests, but both of these tests have been reported to have lower power when study numbers are low (Egger et al., 1997, Begg and Mazumdar, 1994), although the visual inspection of the funnel plot (Figure 3), showed scarcity of studies reporting lower or null effects.
Figure 2.
Forest plot for all studies of fatal motor vehicle injury and estimated relative risks associated with a 0.02 increase in BAC: Estimates were derived from a random effects linear model.
Figure 3.
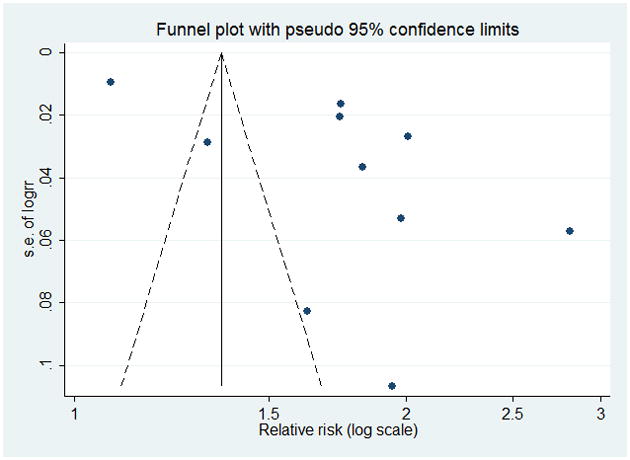
Funnel plot for all studies of fatal motor vehicle injury.
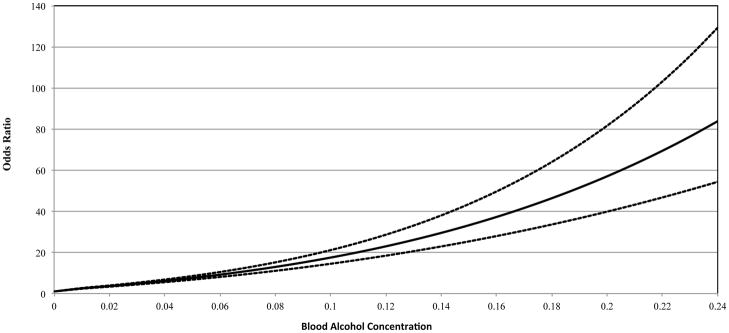
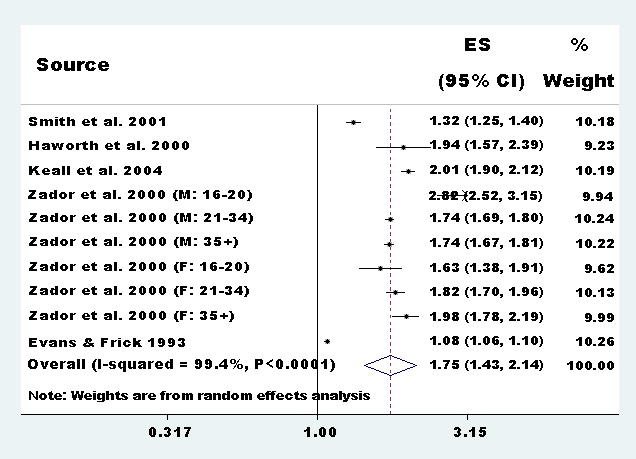
3.2. Fractional polynomial regression
The results of the fractional polynomial regression (Figure 4) showed a strong dose-response relationship between BAC and fatal motor vehicle injury. Initially, the linear model was fit to the pooled data, and then a first-order best-fit curve was attempted to try and improve the fit of the line to the data. The best-fit fractional polynomial was P1 = 0.5 and P2 = 0.5, which had a significantly lower deviance score than either the linear single-order, or the quadratic polynomial. Figure 4 shows the relationship between BAC and OR for fatal motor vehicle injury from BAC = 0 to 0.5% and Figure 5 shows only it up to 0.24 to highlight the risk at low BAC levels.
Figure 4.
Dose-response curve for the BAC level and the odds of a fatal motor vehicle injury for all 5 studies combined for BAC levels from 0 to 0.5%
Figure 5.
Dose-response curve for the BAC level and the odds of a fatal motor vehicle injury for all 5 studies combined for BAC levels from 0 to 0.24%.
At a BAC of 0.5%, the maximum odds ratio of alcohol-attributable fatal injury was 595.05 (95% CI: 223.5 – 1584.0). At a BAC level of 0.02 (roughly the equivalent of one standard drink), this analysis estimated the OR to be 3.64 (95% CI: 3.37 – 3.94) (see Figure 5). At the legal limit of 0.08, the legal BAC limit in most countries, the OR was calculated to be 13.0 (95% CI: 11.1 – 15.2) (see Figure 5). At levels above 0.08, the curve started to get much steeper with exponentially larger increases in fatal motor vehicle injury risk at these levels.
3.4. Sensitivity Analysis
A post-hoc sensitivity analysis was performed due to the inclusion of 6 different Zador et al datasets in the meta-analysis, in order to test whether the inclusion of six separate datasets had any more influence over the pooled estimate than just one aggregated dataset from this study. For this analysis, the six Zador datasets were aggregated together to make one dataset only, resulting in 5 datasets being entered into the meta-analysis instead of 10. To aggregate the 6 Zador datasets, the relative risks were linearized by taking the natural logarithm of the RR across each BAC level and then a weighted average was computed by the number of cases in order to correctly combine each age- and sex-specific across each BAC level. Next, the same meta-analysis steps were applied to this new dataset, but instead of representing 6 studies, Zador et al, now only represented one study. Figure 6 shows the forest plot of the meta-analysis. For every 0.02% increase in BAC, the OR was found to increase by 1.60 (1.17 – 2.20), which was not statistically significantly different from the meta-analysis which included all six datasets from Figure 2, since the confidence interval was covered. The heterogeneity assessment remained significant (p<0.0001), I2 = 99.6%.
Figure 6.
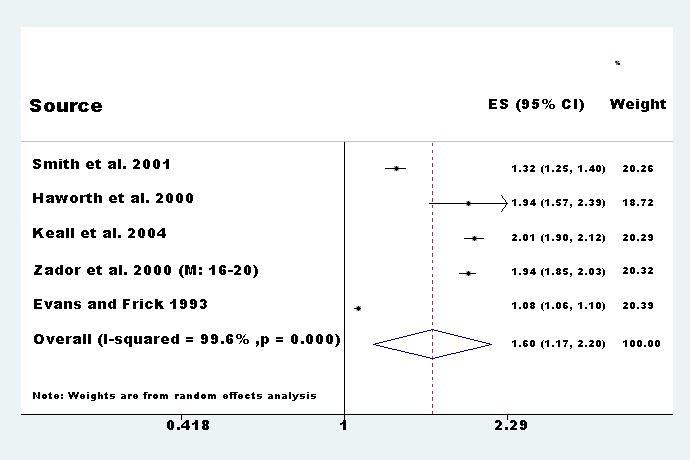
Forest plot for the sensitivity analysis for which Zador et al. was aggregated across BAC categories. Estimates of OR for a corresponding 0.02 % increase in BAC were derived from a random effects linear model.
Discussion
This is the first meta-analysis to quantify the overall relationship between acute alcohol consumption and the risk of fatal motor vehicle crash injury. One previous meta-analysis (by this author) on alcohol and the risk of non-fatal motor vehicle injury has been published and provides the closest comparison due to similar methodology (Taylor et al., 2010). Although the alcohol consumption measure differed (grams of alcohol consumed 3 hours prior to the injury versus BAC), the odds of fatal injury due to motor vehicle accidents were significantly higher compared to non-fatal injury at similar alcohol consumption levels, definitively showing this comparison quantitatively for the first time. In this study, an OR of 1.75 (95% CI: 1.43 – 2.14) per 0.02 % rise in BAC was found, whereas for no-fatal motor vehicle injury the OR was 1.24 (95% CI: 1.18–1.31) for approximately a 1 drink increase (which generally results in a BAC of about 0.02%) (Brouwer, 2004). What’s more, the risk curve for fatal injury was consistently far steeper than for non-fatal injury at all levels of alcohol consumption.
Before discussing these results further, it is important to discuss some of the limitations of this analysis. First, it is important to recognize the contribution of the Zador et al. (Zador et al., 2000) paper, which contributed 6 data sets out of 10 used in the main analysis. Despite the Zador et al. study being a very high quality study, by its mere inclusion, over half of the datasets would be subject to the same biases inherent to this one study alone. To investigate the influence of the inclusion of all 6 Zador papers, the sensitivity analysis was complete, this time pooling the Zador data into 1 study only by aggregating the samples and RR across BAC categories. The sensitivity analysis showed that the aggregation made no appreciable difference to the meta-analytic results either quantitatively nor qualitatively compared to the six separate datasets. So, for this analysis, the main analysis included all 6 separate datasets simply for the reason that aggregating this data would result in valuable information being lost in an already small dataset, leading to the estimation of a less precise estimate.
Second, this systematic review only resulted in only 5 eligible papers, which highlights how understudied the relationship between acute alcohol consumption and fatal motor vehicle injury is compared to non-fatal motor vehicle injury, and highlights the major disparities between the study of fatal and non-fatal injuries generally. Exposure data for studies of fatal injury tends to rely more on data from coroner’s reports, mortality statistics, and police files compared to inhospital and in-person questionnaires of case-control or case-crossover data that characterizes investigations of alcohol-attributable non-fatal injuries, which tend to be based on self-reported consumption in emergency room settings (Gmel et al., 2009, Borges et al., 2005, Borges et al., 2008, Cherpitel et al., 2006), making access to cases more difficult and time-intensive. As well, measuring the relationship between acute alcohol consumption and fatal injury may be more difficult than for non-fatal injury and may tend to underestimate the true relationship between alcohol and fatal injury, particularly given that BAC calculations may result in underestimation of true consumption (Gullberg, 2007, Brouwer, 2004). BAC is often measured long after the initial accident took place, which may underestimate the true exposure (e.g. (Keall et al., 2004)) and thus the dose-specific relative risk, making the results of the current analysis conservative. The time between and injury occurring and the forensic pathological investigation may be some time, and time – and temperature – dependent degradation ethanol metabolites in blood have been reported in the forensic pathology literature (Halter et al., 2009, Ferrari et al., 2006). The overestimation of BAC may also be possible, although unlinkely, due to a build-up of ethanol-producing bacteria that may occur after death, (Appenzeller et al., 2008, Collison, 2005). In recent years (since the mid-nineteen nineties), this problem has largely been resolved via the testing of other bodily fluids, such as vitreous humor, where ethanol levels have been shown to be very stable over time (Chao and Lo, 1993).
Third, control selection is also important in this relationship. For a number of studies included in this report, control groups were made up of severely injured individuals (Evans and Frick, 1993b) or population controls (Keall et al., 2004, Zador et al., 2000). Using the injured group as a reference would underestimate the OR since the likelihood of all non-fatal injury is also increased with alcohol consumption, thereby falsely deflating the resulting OR compared to a non-injured control group.
Fourth, prior research in this area has shown that the relationship between alcohol and injury may be confounded by usual drinking patterns, risk-taking behavior and substance use (Watt et al., 2004). Studies included in this meta-analysis did not control for these factors, or only controlled just one or two of them. This means the overall pooled estimate may be biased from the outset with respect to these confounders. On the other side of this argument, though, is that explicitly controlling for some of these types of confounders may lead to biased risk estimates due to the fact that alcohol and risk-taking behavior, for example, are on the causal path from alcohol consumption to injury. Decisions to engage in activities that are likely to lead to an injury are positively influenced to a large degree by the consumption of alcohol, so over-controlling by including these confounders would result in incorrect RR/OR as well (Deery and Love, 1996, Bazargan-Hejazi et al., 2007, Greenfield and Rogers, 1999). Lastly, there is some evidence that some bias may be introduced in cases of hit and run drivers, who are not tested (Blomberg et al., 2009), although this would result in even more conservative estimates than those presented here. Thus the results of this study, even though it shows high risk relationships of fatal crash and BAC, can be seen as an underestimate of the true relationship.
This meta-analysis summarized the available, high quality literature to date on the relationship between acute alcohol consumption and death from motor vehicle accidents. At all levels of consumption, the odds of dying in a motor vehicle crash were significantly higher than for zero alcohol consumption, and were approximately 13 times higher at the current legal limit of BAC = 0.08. The policy implications of this are obvious – at this BAC, the risk is simply too high and efforts to lower the legal limit while operating a motor vehicle must be increased based on this available evidence. There is clear evidence that, upon a reduction in the legal limit from BAC = 0.10 to 0.08 reduced fatal accidents in the US (Hingson et al., 1996a, Hingson et al., 1996b), but the implications from this report would call for even more drastic measures, to 0.05, or even lower, particularly in younger drivers, who appear to be at the most risk based on single studies (Zador et al., 2000).
Clearly, risk relationship studies of alcohol-attributable fatal motor vehicle injuries is an area of research that is in need of more, higher quality studies. In order to get more stable risk curves at all levels of alcohol consumption that will inform public health and burden of disease and monitoring-type analyses, more in-depth risk modeling methods and procedures are required (Shield et al., 2010). In particular, studies that separate injury types and present sex-specific data are needed. However, there are significant barriers to completion of these studies, most notably in the areas of exposure assessment, selection of control groups, and access to and completeness of secondary data sources with relevant exposure information.
Acknowledgments
BT’s doctoral research is supported by a Sir Frederick Banting and Charles Best Canada Graduate Scholarship administered by the Canadian Institutes of Health Research. Financial support for this study was provided to JR by the National Institute for Alcohol Abuse and Alcoholism (NIAAA) with contract # HHSN267200700041C to conduct the study titled “Alcohol- and Drug-attributable Burden of Disease and Injury in the US”. In addition, JR received a salary and infrastructure support from the Ontario Ministry of Health and Long-Term Care.
References
- Anda RF, Williamson DF, Remington PL. Alcohol and fatal injuries among US adults. Findings from the NHANES I Epidemiologic Follow-up Study. JAMA. 1988;260:2529–2532. [PubMed] [Google Scholar]
- Andelic N, Jerstad T, Sigurdardottir S, Schanke AK, Sandvik L, Roe C. Effects of acute substance use and pre-injury substance abuse on traumatic brain injury severity in adults admitted to a trauma centre. J Trauma Manag Outcomes. 2010;4:6. doi: 10.1186/1752-2897-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appenzeller BM, Schuman M, Wennig R. Was a child poisoned by ethanol? Discrimination between ante-mortem consumption and post-mortem formation. Int J Legal Med. 2008;122:429–434. doi: 10.1007/s00414-008-0245-3. [DOI] [PubMed] [Google Scholar]
- Bazargan-Hejazi S, Gaines T, Duan N, Cherpitel CJ. Correlates of injury among ED visits: effects of alcohol, risk perception, impulsivity, and sensation seeking behaviors. Am J Drug Alcohol Abuse. 2007;33:101–108. doi: 10.1080/00952990601087455. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- Blomberg RD, Peck RC, Moskowitz H, Burns M, Fiorentino D. The Long Beach/Fort Lauderdale relative risk study. Journal of safety research. 2009;40:285–292. doi: 10.1016/j.jsr.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel CJ, Orozco R, Bond J, Ye Y, Macdonald S, Giesbrecht N, Stockwell T, Cremonte M, Moskalewicz J, Swiatkiewicz G, Poznyak V. Acute alcohol use and the risk of non-fatal injury in sixteen countries. Addiction. 2006;101:993–1002. doi: 10.1111/j.1360-0443.2006.01462.x. [DOI] [PubMed] [Google Scholar]
- Borges G, Mondragon L, Medina-Mora ME, Orozco R, Zambrano J, Cherpitel C. A case-control study of alcohol and substance use disorders as risk factors for non-fatal injury. Alcohol Alcohol. 2005;40:257–262. doi: 10.1093/alcalc/agh160. [DOI] [PubMed] [Google Scholar]
- Borges G, Orozco R, Cremonte M, Buzi-Figlie N, Cherpitel C, Poznyak V. Alcohol and violence in the emergency department: a regional report from the WHO collaborative study on alcohol and injuries. Salud Publica Mex; 2008. p. 50. [DOI] [PubMed] [Google Scholar]
- Borkenstein RF, Crowther FR, Shumate RP, Ziel WB, Zylman R. DEPARTMENT OF POLICE ADMINISTRATION IU . Series The role of the drinking driver in traffic accidents. 1964. The role of the drinking driver in traffic accidents. [Google Scholar]
- Brouwer IG. The Widmark formula for alcohol quantification. SADJ. 2004;59:427–428. [PubMed] [Google Scholar]
- Chao TC, Lo DS. Relationship between postmortem blood and vitreous humor ethanol levels. The American journal of forensic medicine and pathology. 1993;14:303–308. doi: 10.1097/00000433-199312000-00006. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Bond J, Ye Y. Alcohol and injury: a risk function analysis from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) Eur Addict Res. 2006;12:42–52. doi: 10.1159/000088582. [DOI] [PubMed] [Google Scholar]
- Collison IB. Elevated postmortem ethanol concentrations in an insulin-dependent diabetic. J Anal Toxicol. 2005;29:762–764. doi: 10.1093/jat/29.7.762. [DOI] [PubMed] [Google Scholar]
- Corrao G, Bagnardi V, Zambon A, Arico S. Exploring the dose-response relationship between alcohol consumption and the risk of several alcohol-related conditions: a meta-analysis. Addiction. 1999;94:1551–1573. doi: 10.1046/j.1360-0443.1999.9410155111.x. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Maio RF, Hill EM, Zink BJ. The effects of alcohol on head injury in the motor vehicle crash victim. Alcohol Alcohol. 2002;37:236–240. doi: 10.1093/alcalc/37.3.236. [DOI] [PubMed] [Google Scholar]
- Deery HA, Love AW. The effect of a moderate dose of alcohol on the traffic hazard perception profile of young drink-drivers. Addiction. 1996;91:815–827. doi: 10.1046/j.1360-0443.1996.9168158.x. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans L, Frick MC. Alcohol's effect on fatality risk from a physical insult. J Stud Alcohol. 1993a;54:441–449. doi: 10.15288/jsa.1993.54.441. [DOI] [PubMed] [Google Scholar]
- Evans L, Frick MC. Mass ratio and relative driver fatality risk in two-vehicle crashes. Accid Anal Prev. 1993b;25:213–224. doi: 10.1016/0001-4575(93)90062-2. [DOI] [PubMed] [Google Scholar]
- Fabbri A, Marchesini G, Morselli-Labate AM, Rossi F, Cicognani A, Dente M, Iervese T, Ruggeri S, Mengozzi U, Vandelli A. Blood alcohol concentration and management of road trauma patients in the emergency department. J Trauma. 2001;50:521–528. doi: 10.1097/00005373-200103000-00018. [DOI] [PubMed] [Google Scholar]
- Ferrari LA, Triszcz JM, Giannuzzi L. Kinetics of ethanol degradation in forensic blood samples. Forensic Sci Int. 2006;161:144–150. doi: 10.1016/j.forsciint.2006.02.049. [DOI] [PubMed] [Google Scholar]
- Field AP. Meta-analysis of correlation coefficients: a Monte Carlo comparison of fixed-and random-effects methods. Psychol Methods. 2001;6:161–180. doi: 10.1037/1082-989x.6.2.161. [DOI] [PubMed] [Google Scholar]
- Field AP. The problems in using fixed-effects models of meta-analysis on real-world data. Understanding Statistics. 2003;2:77–96. [Google Scholar]
- Gmel G, Kuendig H, Rehm J, Schreyer N, Daeppen JB. Alcohol and cannabis use as risk factors for injury--a case-crossover analysis in a Swiss hospital emergency department. BMC Public Health. 2009;9:40. doi: 10.1186/1471-2458-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golan JD, Marcoux J, Golan E, Schapiro R, Johnston KM, Maleki M, Khetarpal S, Jacques L. Traumatic brain injury in intoxicated patients. J Trauma. 2007;63:365–369. doi: 10.1097/TA.0b013e31811ec178. [DOI] [PubMed] [Google Scholar]
- Goodman RA, Istre GR, Jordan FB, Herndon JL, Kelaghan J. Alcohol and fatal injuries in Oklahoma. J Stud Alcohol. 1991;52:156–161. doi: 10.15288/jsa.1991.52.156. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rogers JD. Alcoholic beverage choice, risk perception and self-reported drunk driving: effects of measurement on risk analysis. Addiction. 1999;94:1735–1743. doi: 10.1046/j.1360-0443.1999.9411173510.x. [DOI] [PubMed] [Google Scholar]
- Gullberg RG. Estimating the uncertainty associated with Widmark's equation commonly applied in forensic toxicology. Forensic Sci Int. 2007;172:33–39. doi: 10.1016/j.forsciint.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Halter CC, Laengin A, Al-Ahmad A, Wurst FM, Weinmann W, Kuemmerer K. Assessment of the stability of the ethanol metabolite ethyl sulfate in standardised degradation tests. Forensic Sci Int. 2009;186:52–55. doi: 10.1016/j.forsciint.2009.01.009. [DOI] [PubMed] [Google Scholar]
- Haworth NL. Alcohol and Risk of Accident. 2000. Comparing the involvement of alcohol in fatal and serious injury single vehicle crashes, in Series Comparing the involvement of alcohol in fatal and serious injury single vehicle crashes; pp. 53–58. [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Hingson R, Heeren T, Winter M. Lowering state legal blood alcohol limits to 0.08%: the effect on fatal motor vehicle crashes. American journal of public health. 1996a;86:1297–1299. doi: 10.2105/ajph.86.9.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Howland J. Alcohol and non-traffic unintended injuries. Addiction. 1993;88:877–883. doi: 10.1111/j.1360-0443.1993.tb02105.x. [DOI] [PubMed] [Google Scholar]
- Hingson R, McGovern T, Howland J, Heeren T, Winter M, Zakocs R. Reducing alcohol-impaired driving in Massachusetts: the Saving Lives Program. American journal of public health. 1996b;86:791–797. doi: 10.2105/ajph.86.6.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurst PM, Harte D, Frith WJ. The Grand Rapids dip revisited. Accid Anal Prev. 1994;26:647–654. doi: 10.1016/0001-4575(94)90026-4. [DOI] [PubMed] [Google Scholar]
- Ivers RQ, Blows SJ, Stevenson MR, Norton RN, Williamson A, Eisenbruch M, Woodward M, Lam L, Palamara P, Wang J. A cohort study of 20,822 young drivers: the DRIVE study methods and population. Inj Prev. 2006;12:385–389. doi: 10.1136/ip.2006.011825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasantikul V, Ouellet JV, Smith T, Sirathranont J, Panichabhongse V. The role of alcohol in Thailand motorcycle crashes. Accid Anal Prev. 2005;37:357–366. doi: 10.1016/j.aap.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Keall MD, Frith WJ, Patterson TL. The influence of alcohol, age and number of passengers on the night-time risk of driver fatal injury in New Zealand. Accid Anal Prev. 2004;36:49–61. doi: 10.1016/s0001-4575(02)00114-8. [DOI] [PubMed] [Google Scholar]
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- Malmivaara A, Heliovaara M, Knekt P, Reunanen A, Aromaa A. Risk factors for injurious falls leading to hospitalization or death in a cohort of 19,500 adults. Am J Epidemiol. 1993;138:384–394. doi: 10.1093/oxfordjournals.aje.a116871. [DOI] [PubMed] [Google Scholar]
- Orsini N, Bellocco R, Greenland S. Generalizedleast squares for trend estimation of summarized dose-response data. Stata Journal. 2006;6:40–57. [Google Scholar]
- Peck RC, Gebers MA, Voas RB, Romano E. The relationship between blood alcohol concentration (BAC), age, and crash risk. J Safety Res. 2008;39:311–319. doi: 10.1016/j.jsr.2008.02.030. [DOI] [PubMed] [Google Scholar]
- Rehm J, Gmel G, Sempos CT, Trevisan M. Alcohol-related morbidity and mortality. Alcohol Res Health. 2003;27:39–51. [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos C, Frick U, Jernigan D. Alcohol Use, in Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. In: EZZATI M, LOPEZ AD, RODGERS A, MURRAY C, editors. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Vol. 1. World Health Organization; Geneva: 2004. pp. 959–1109. [Google Scholar]
- Royston P. A strategy for modelling the effect of a continuous covariate in medicine and epidemiology. Stat Med. 2000;19:1831–1847. doi: 10.1002/1097-0258(20000730)19:14<1831::aid-sim502>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Royston P, Altman DG. Regression using fractional polynomials ofcontinuous covariates: parsimonious parametric modeling. Appl Stat. 1994;43:429–467. [Google Scholar]
- Shield K, Kehoe T, Taylor B, Patra J, Rehm J. Mortality and potential years of life lost attributable to alcohol consumption for individuals 0 to 64 years of age in Canada in 2005. Addiction. 2010 doi: 10.1186/1471-2458-12-91. (Submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GS, Keyl PM, Hadley JA, Bartley CL, Foss RD, Tolbert WG, McKnight J. Drinking and recreational boating fatalities: a population-based case-control study. JAMA. 2001;286:2974–2980. [PubMed] [Google Scholar]
- Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, Greenfield T, Rehm J. The more you drink, the harder you fall: a systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110:108–116. doi: 10.1016/j.drugalcdep.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson SG. Why sources of heterogeneity in meta-analysis should be investigated. BMJ. 1994;309:1351–1355. doi: 10.1136/bmj.309.6965.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vingilis E, McLeod AI, Stoduto G, Seeley J, Mann RE. Impact of extended drinking hours in Ontario on motor-vehicle collision and non-motor-vehicle collision injuries. J Stud Alcohol Drugs. 2007;68:905–911. doi: 10.15288/jsad.2007.68.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinson DC, Maclure M, Reidinger C, Smith GS. A population-based case-crossover and case-control study of alcohol and the risk of injury. J Stud Alcohol. 2003;64:358–366. doi: 10.15288/jsa.2003.64.358. [DOI] [PubMed] [Google Scholar]
- Watt K, Purdie DM, Roche AM, McClure RJ. Risk of injury from acute alcohol consumption and the influence of confounders. Addiction. 2004;99:1262–1273. doi: 10.1111/j.1360-0443.2004.00823.x. [DOI] [PubMed] [Google Scholar]
- Watt K, Purdie DM, Roche AM, McClure RJ. The relationship between acute alcohol consumption and consequent injury type. Alcohol Alcohol. 2005;40:263–268. doi: 10.1093/alcalc/agh164. [DOI] [PubMed] [Google Scholar]
- Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: an update using 1996 data. J Stud Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]