Abstract
Efficiency and effectiveness of care coordination depends on a match between the needs of the population and the skills, scope of practice, and intensity of services provided by the care coordinator. There is limited existing literature that addresses the relevance of the APN role as a fit for coordination of care for children with SHCN. The objective of this paper is to describe the value of the advanced practice nurse’s (APN’s) enhanced scope of knowledge and practice for relationship-based care coordination in healthcare homes that serve children with complex special health care needs (SHCN). The TeleFamilies project is provided as an example of the integration of an APN care coordinator in a healthcare home for children with SHCN.
Keywords: advanced practice nursing, special health care needs, children with medical complexity, healthcare home, care coordination
Approximately 14% of all children under age 18 have a special health care need (SHCN), defined as having a chronic physical, developmental, behavioral, or emotional condition and requiring more services than typical children (USDHHS, 2008). The number of children in the U.S. with SHCN has increased dramatically in the past four decades (Burns et al., 2010). Because of the higher need for and use of health care services, the costs per capita of healthcare for children with SHCN are nearly three times higher than for children in the general population (Grupp-Phelan, Lozano, & Fishman, 2001; Newacheck & Kim, 2005). In a study of more than 46,000 children enrolled in a state health plan, Neff et al. (2004) found that children with one or more chronic conditions accounted for more than 45% of all pediatric charges.
Children with Complex SHCN
A subset of children with SHCN has unique needs due to the complexity of their conditions. Cohen et al. (2011) termed this subgroup children with medical complexity (CMC) and proposed a definitional framework with four domains based on a systematic review of chronic disease of childhood. In their framework, CMC have: (a) characteristic patterns of family-identified health care service needs; (b) lifelong chronic conditions that are severe and/or associated with medical fragility; (c) functional limitations that may be severe requiring assistance from technology; and (d) high utilization health resources such as hospitalizations and/or the involvement of multiple subspecialists (Cohen et al.). Children with complex SHCN are a rapidly growing group of healthcare consumers (Tennant, Pearce, Bythell, & Rankin, 2010; Wise, Huffman, & Brat, 2007). These children are more likely to need health services and have a significantly higher financial impact on families in terms of days missed from work and school due to illness and health care encounters (Nageswaran, Silver, & Stein, 2008). Compared to other children, children who have functional limitations have the highest needs for outpatient and emergency care. Also, their health conditions place significantly greater demands on their families’ time and finances, and medical expenditures for children with SHCN are two to three times higher than those of children without functional limitations. The increasing numbers of children with SHCN and the complexity of their conditions, in particular, have significant implications for utilization of public and private health resources (Perrin, Bloom, & Gortmaker, 2007).
Coordinated Care
Health care providers face challenges related to the management of health and service needs of children with complex SHCN. Among these challenges is coordination of care. The Institute of Medicine (IOM) has identified care coordination as one of its twenty national priorities for improving the quality of health care and a primary area for performance measurement following the landmark publication Crossing the Quality Chasm: A New Health System for the 21st Century (National Research Council, 2001). The Affordable Care Act (ACA) recognizes the value of coordinated care as essential for the optimal delivery of health care in the United States (Orszag & Emanuel, 2010). Specifically, Section 2717 of the ACA requires that experts in health care quality and stakeholders “shall develop…health care provider reimbursement structures that improve health outcomes through activities such as effective case management, care coordination, [and] chronic disease management” (Office of the Legislative Council, US House of Representatives, 2010, p.19). The ACA further recommends rewarding quality with market-based incentives through a payment structure that provides incentives for care coordination and directs systems to include a nurse care coordinator on the health team.
Care coordination is a key component of the healthcare home (medical home) model of care. The pediatric healthcare home is a model of care that promotes holistic care of children and their families that provides management of both acute and chronic issues, and where each family has an ongoing relationship with a healthcare professional (National Association of Pediatric Nurse Practitioners, NAPNAP, 2009). The concept of a medical home for children with SHCN is not new; the term first appeared in a book published by the American Academy of Pediatrics (AAP) in the 1960s, where the Council on Pediatrics noted a concern about “duplication and gaps in services that occur as a result of lack of communication and coordination” (AAP, 1967, p. 78). The medical home concept evolved and gained recognition nationally over the next four decades, with policy statements from professional organizations including the AAP (2002) and NAPNAP (2009) supporting a comprehensive, coordinated model of care with families at the center.
Coordinated care is a vital component of the healthcare home approach (Palfrey, 2009), but this coordination requires an investment of dedicated time and resources to develop, implement, and evaluate the processes and activities that comprise comprehensive, coordinated and compassionate care (Safriet, 2011). It is also important to distinguish between care coordination as a task-oriented process supported by systems-level infrastructure, and care coordination as relationship-based approach to complex problem-solving with families of children with SHCN. Antonelli, McAllister, and Popp (2009) identify four foundational characteristics and attributes of high quality pediatric care coordination: (1) it is patient-and family-centered; (2) it is proactive, planned, and comprehensive; (3) it promotes self-care skills and independence; and (4) it emphasizes cross-organizational relationships. As a process, care coordination in a healthcare home is designed to achieve the following outcomes:
facilitate the provision of comprehensive health promotion and chronic condition care;
ensure a locus of ongoing, proactive, planned care activities;
build and use effective communication strategies among family, the medical home, schools, specialists, and community professionals and community connections; and
help improve, measure, monitor and sustain quality outcomes (clinical, functional, satisfaction and cost) (McAllister, Presler, & Cooley, 2007, p. e726).
While many primary care providers report they are coordinating care in their practice through an approach that involves distributing tasks across personnel, there is evidence that the effectiveness of such an approach to coordination is limited. The primary barriers to providing comprehensive care coordination for chronic conditions in pediatric practices are lack of time, lack of medical staff to provide the service, and inadequate reimbursement for this service (Gupta, O’Conner, & Quesada-Gomez, 2004).
Despite consensus on the benefit, care coordination interventions are rarely defined in terms of the structure (e.g. role preparation, scope of practice, and setting) and process (e.g. responsibilities, dedicated time for care coordination, and amount of care provided) of that service. Historically, care coordination roles have been held by a variety of provider types including nursing, social work, payor-based lay and nursing staff, health coaches, community coordinators and county case workers (Bodenheimer, 2008; McAllister, et al., 2007; McDonald, Sundaram, & Bravata, 2007). However, there is relatively little written on the core functions that should be embedded in the care-coordinator professional role and the core competencies, training, and methods for implementing and evaluating this service (McAllister, et al., Wise, et al., 2007).
Advanced Practice Nursing and Care Coordination: Value-Added
The effectiveness of nurse care coordination for varying levels of patient complexity is dependent on the educational preparation and scope of practice of the nurse and the ability of the care coordinator to develop a relationship with families over time. There is evidence that healthcare charges for typically high-cost patient groups are lower when advanced practice nurses (APNs) have the autonomy to act on their knowledge and clinical judgment, and that savings are proportional to nurse dose (time with patients and number of contacts; Brooten & Youngblut, 2006). Compared to a nurse prepared at the associate or baccalaureate level, the advanced practice nurse who is prepared at the graduate level has increased depth and breadth of knowledge, higher complexity of skills and interventions, and increased role autonomy.
Brooten et al. (2003) identified five key factors that contribute to the APN’s effectiveness: content expertise, interpersonal skills, knowledge of systems, the ability to implement change, and the ability to access resources. The match between the characteristics of the care coordinator and the roles, responsibilities, and core functions is essential to the success of care coordination as an intervention. Children who have multiple complex health needs, psychosocial risk factors, frequent service use, and/or multiple providers require high-complexity care coordination. This level of care coordination consists of proactive health management and requires advanced skills in assessment, management, and evaluation. The APN approach is a blending of counseling with clinical care, coordination of health services and identification and referral to appropriate community resources in support of patients (Safriet, 2011). This blending of skills is critical to coordination of the psychosocial and financial needs of families beyond the medical challenges of their child. This is particularly true for children with complex SHCN who need a more complex level of care coordination (Wise, et al., 2007).
Both low- and high-complexity care coordination are essential components of high-quality, family-centered care, and have unique value in systems of care. Aims of both levels of care coordination include building care relationships among the family and the health care team, assessing family strengths and assets, and supporting primary care and specialty co-management (see Table 1).
Table 1.
Characteristics of Low- and High-Intensity Care Coordination for Children with Special Health Care Needs
| Low Intensity | High Intensity | |
|---|---|---|
| Description | Functional, episodic, task-oriented | Relationship-based with proactive health management |
| Population served | CSHCN* with routine and predictable health needs, low service use, limited number of providers |
CSHCN* with multiple, complex health needs, psychosocial risk factors, frequent service use, multiple providers |
| Roles and Responsibilities (examples) |
— Facilitate access to providers and resources |
—Develop, coordinate, and document plan of care |
| — Serve as contact point, advocate, and informational resource |
— Provide leadership in coordination of multidisciplinary care |
|
| — Educate and provide anticipatory guidance |
Initiate and manage referrals and monitor for overlap, gaps in service |
|
| — Coordinate efforts to gain family/youth feedback |
— Prepare for and facilitate transitions |
|
| — Participate in interventions which address family needs |
— Advanced assessment, management, evaluation |
|
| Shared Characteristics | ||
|
|
||
| Aims of care | — Build care relationships among family and team; support the primary care-giving role of the family |
|
| — Assess child/patient and family needs and unmet needs, strengths and assets | ||
| — Cultivate and support primary care & subspecialty co-management with timely communication, inquiry, follow up and integration of information into the care plan | ||
| Competencies | — Culturally effective capabilities demonstrating a sensitivity and responsiveness to varying cultural characteristics and beliefs |
|
| — Essential leadership, advocacy, communication, education and counseling, and resource research skills | ||
CSHCN: Children with special health care needs
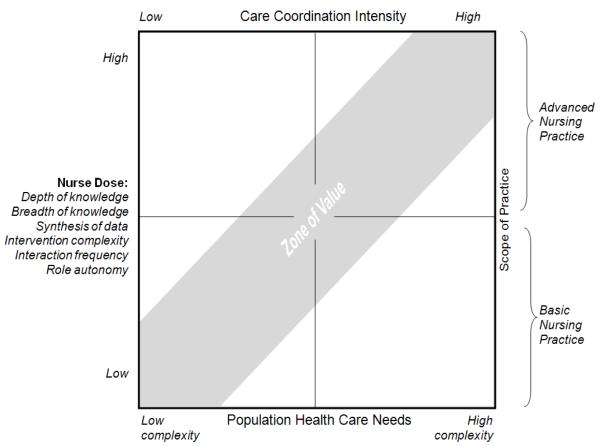
The advanced practice nurse (APN) is ideally prepared for the role of high-complexity care coordination for CSHCN and has the scope of practice that best fits the needs of these children and their families. Brooten and Youngblut (2006) proposed a concept of “nurse dose” in terms of patient and nurse characteristics. Here, nurse dose refers to both the amount of care provided by the nurse and the depth and breadth of knowledge, synthesis of data, and intervention complexity (Brooten et al., 2003). As nurse dose increases, the patient/provider ratio can increase due to the increased skills, knowledge, and scope of practice of the nurse.
The proposed Value Model of nurse dose to patient complexity (Figure 1) represents two levels of nursing based on scope of practice and education level: advanced practice nursing and basic nursing. Advancement (through graduate nursing education), specialization (provision of care for a specific population of patients with complex, unpredictable, and/or intrusive health needs), and expansion (acquisition of new knowledge and skills and role autonomy) are three characteristics that distinguish advanced practice nursing from basic nursing (Bryant-Lukosius et al., 2004; Ruel & Motyka, 2009). Advanced practice nursing involves higher clinical skill level; specialization of care; depth, breadth, and expansion of knowledge; degree of data synthesis; advanced complexity of skills and interventions; expanded theoretical and research-based interventions; and autonomous roles with expanded boundaries and scope of practice (Ruel & Motyka).
Figure 1.
Zone of Value for matching nurse scope of practice with population health care needs
Inherent in advanced nursing practice is the function of change agent (Bryant-Lukosius et al., 2004). This skill contributes to implementation strategies for incorporating care coordination into existing clinical settings. By shaping roles to address complex and dynamic health care system needs and demands for flexibility in service delivery, APNs can help to reduce fragmentation of care roles (Bryant-Lukosius et al.; Ruel & Motyka, 2009). Advanced practice nursing adds value to systems of care by decreasing cost, increasing quality and improving access. According to Bryant-Lukosius et al., “The value-added component of APN roles involves a nursing orientation to practice characterized by coordinated, integrated, holistic, and patient-centered care designed to maximize health, quality of life, and functional capacity” (2004, p. 524).
At the state and federal levels there are efforts to quantify the cost of care coordination services, which are a required component of healthcare homes. Estimates of the cost of this service are complicated by the absence of a clear method for predicting what kind of services are within the scope of care coordination, and how condition severity and comorbidities may influence the level of care coordination required to benefit patients, health systems, payors, and society in the long run. Many healthcare homes consider the cost of a care coordinator’s salary as a significant factor in deciding how to implement care coordination services. A distributed model of care coordination enables multiple providers to participate in the activities of care coordination, but the risk of fragmenting care coordination is high when the health care needs of children are complex, multiple specialty providers provides services to the same patient, and the frequency of service use is high. Maximizing return on investment for health care costs will require data on which aspects of preventive care effect the greatest reductions in costs. The TeleFamilies project provides an opportunity explore the return on investment for APN care coordination.
Measuring Outcomes of APN Care Coordination: The TeleFamilies Project
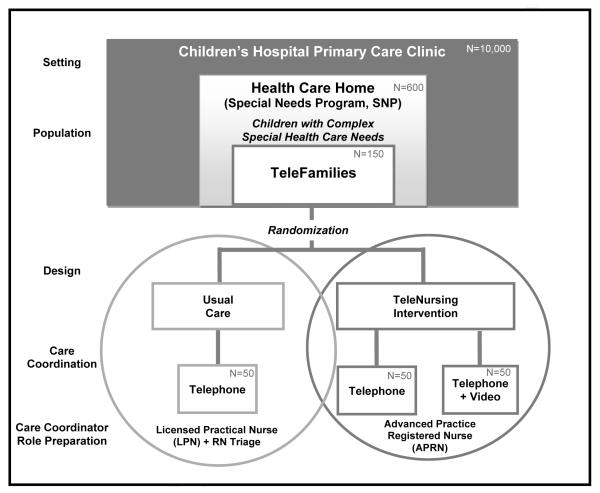
The role, process, and value of APN care coordination for children with complex SHCN can be viewed in the context of the TeleFamilies study. The TeleFamilies study (Figure 2) is a four-year, three-armed randomized controlled trial. The aim of the TeleFamilies study is to evaluate the effectiveness of enhanced, interactive telehealth technology and advanced practice nurse care coordination for children with complex health care needs. Key outcome measures are health care service utilization (location and level of service), child and family outcomes (quality of life and functional status), and satisfaction with the quality and clinical usefulness of telehealth technology. The implementation of an APN care coordination role within an existing healthcare home practice provides an exemplar for other pediatric practices.
Figure 2.
Context of the TeleFamilies study and care coordination intervention
Setting: Healthcare Home for Complex Children with Complex SHCN
The setting for this project is a large urban general pediatrics clinic affiliated with a free-standing, non-profit children’s hospital. Eight pediatricians and four nurse practitioners provide primary care to approximately 10,000 children during 25,000 outpatient visits a year. A subset of this population is enrolled in a clinic-developed Special Needs Program (SNP), which serves approximately 600 complex, chronically ill children within the practice. The SNP is certified in the state of Minnesota as a pediatric healthcare home (medical home), which is “an approach to primary care in which primary care providers, families and patients work in partnership to improve health outcomes and quality of life for individuals with chronic health conditions and disabilities” (Minnesota Department of Health, 2011). The health care home is unique in that is serves a population of children with particularly complex health care needs.
Preliminary findings from the TeleFamilies study suggest that the children in the SNP experience a significant functional deficit. According to analysis of baseline data from 94 families in the TeleFamilies study, one-quarter of respondents reported their child had five or more specialist visits in the past 12 months. Parents report that their child’s condition affects their ability to do things that other children can do “some” (32%) or “a great deal” (57%) of the time. Functional status for these children is low; scores on the Functional Status II (Stein & Jessop, 1990) measure for this sample (M=76.0, SD=19.4) are significantly lower than mean scores for a sample of 276 well children (M= 96.1, SD=8.2, p<0.001), and significantly lower than mean scores for a sample of 266 children with “significant chronic health conditions” (M= 86.8, SD=15.7, p<0.001) (Stein & Jessop, 1044). At baseline, families in the TeleFamilies study reported a high degree of need for care coordination, with 74.2 percent reporting they could have used extra help coordinating their child’s care in the past 12 months (see Table 2). Thirty-nine percent of the sample reported their child uses a personal care assistant.
Table 2.
Baseline health and service use of children in the TeleFamilies study (N=94)
| %* | |
|---|---|
| Number of specialist visits in the past 12 months | |
| 0 | 3.5 |
| 1-2 | 27.9 |
| 3-4 | 38.4 |
| 5 or more | 30.2 |
| Child’s overall health | |
| Excellent | 7.5 |
| Very Good | 28.7 |
| Good | 42.6 |
| Fair | 19.2 |
| Poor | 2.1 |
| Stability of child’s condition | |
| Changes all the time | 31.5 |
| Changes once in a while | 47.8 |
| Usually stable | 20.7 |
| How often could have used extra help coordinating | |
| child’s care in past 12 months | |
| Never | 16.0 |
| Sometimes | 57.5 |
| Usually | 13.8 |
| Always | 12.8 |
| How often got as much help as wanted with coordinating | |
| child’s care in past 12 months | |
| Never | 24.7 |
| Sometimes | 44.1 |
| Usually | 20.4 |
| Always | 10.8 |
Percentages may not add up to 100 due to rounding.
Usual Care (Non-Intervention Model) in the Special Needs Program
For families not enrolled in the TeleFamilies project, care coordination in the Special Needs Program is provided by a licensed practical nurse who has developed relationships with the families in the program over several years. This care coordinator works three days a week completing initial assessments, updating care plan information, and carrying out orders as delegated within her scope of practice. Fifty-percent of her time is dedicated office time to help parents coordinate provider visits, referrals and services, and update plans of care in the electronic health record (EHR). Telephone triage is provided for all families served by the general pediatrics clinic. One to two registered nurses provide telephone triage during business hours and field an average of 1085 calls per month, primarily from parents. Communication between triage nurses and primary care providers during a triage episode is conducted primarily by EHR messaging. After-hours and weekend triage calls are routed to an off-site triage center that has read-only access to the EHR.
Implementation of the APN Care Coordinator Role
The APN care coordinator in the TeleFamilies project is a certified pediatric nurse practitioner with specialized competencies in the area of chronic care management and family-centered care of families with children who have complex SHCN. To integrate a new APN into a well-established primary care clinic staff, key stakeholders needed to be identified and engaged. The team engaged the medical director of the SNP early in the project to ensure concurrence of mission and goals of care for children and families. Administrative staff within the hospital and clinic systems were also included in the early planning phases to incorporate existing system-level resources and negotiate the flow of resources from the study to the organization to support the project. Families on a family advisory panel were involved in the implementation stage.
A key objective of this project was to define the role and scope of practice for an APN care coordinator in the context of a healthcare home. This was accomplished by focusing the APN’s time on care coordination activities and maintaining the existing structure of providers in the general pediatric clinic to handle clinic visits for routine and illness care of the patient population. No acute visits are scheduled with the APN care coordinator. Instead, she provides between visit coordination and participates as a member of the team when families bring children for visits, checking in with them during the care episode and coordinates follow-up cares identified during the face-to-face encounters.
The existing clinic triage process diverts calls from families who are not part of the Telefamilies APN caseload to the usual triage resources. Calls from families in the project go directly to the APN’s desk or pager and bypass the clinic telephone system. The existing EHR supports the APN’s ability to manage and contribute to the data generated in the processes of care. Unique EHR templates were developed for the APN care coordination documentation. Existing plan of care templates are used to provide a patient-centered summary of the patient’s diverse services. Evaluation of the intervention and process is enabled by documentation by families and the APN as part of the study. Acceptance of the APN role was facilitated through the clear definition of the role of the APN in this setting with clinic staff and providers and reinforced as the project progressed through written updates and staff meeting presentations. Important to the continuing success of this project is the emphasis on a shared model of care. Role definition and clarity enables the team to understand the fit between the APN’s skills and focus and facilitates enactment of a shared model of care coordination, rather than division of tasks and responsibilities hierarchically. Scheduled care coordination visits with patients and families during clinic visits reinforce the strengths and focus of the APN’s role in supporting the healthcare home team.
Description of APN encounters in the first year of the intervention
An encounter is defined as the APN interacting with a parent, member of the health care system, or community service provider regarding one of the families randomized to either arms of the intervention. Because recruitment was ongoing and families entered the intervention phase of the project on a rolling basis, the number of families in the APN’s caseload steadily increased from 3 in the first month to 97 by the 9th month. Seventy-five percent of all of the encounters in the first nine months were with a total of 21 families; the greatest number of encounters with a single family was 37, which occurred over a four month period of time. Encounters took place via telephone, webcam, chart communication, fax, in the clinic, or in the hospital setting. Encounters ranged in duration from one minute to several hours, with the majority lasting one to five minutes (50%) or six to ten minutes (30%). In the majority of encounters, the APN interacted with the mother, and over half of the encounters (53%) involved multiple parties, including the child, other caregivers, and/or clinic personnel. Chronic condition management was a primary goal of 22 percent of the encounters. Other reasons for the encounters included coordination of care across systems of care, education or support, acute illness management, prescriptions, and scheduling (many encounters had multiple goals; categories are not mutually exclusive).
The TeleFamilies care coordination intervention includes the use of a webcam for real-time, face-to-face collaboration between the APN and the family in the home on an as-needed basis. Families in the video intervention group receive a netbook, webcam, and internet access to enable videoconferencing to the clinic APN from their home. The addition of videoconferencing to the traditional telephone-based communication with families has provided enhanced ability of the APN to clinically assess the child in situations where visual cues are important, such as allergic reactions, troubleshooting equipment issues, and observing child behaviors and family interactions. In addition, interactive videoconferencing between the APN and the family facilitates the development of a relationship with the family through nonverbal communication. Children particularly enjoy seeing the APN on video and are able to participate in a conversation that might have been only between a parent and the APN if only a telephone were used.
In a time-motion study conducted in conjunction with the TeleFamilies study, Cady (2011) compared standard clinic RN telephone triage and APN care coordination workflow and processes related to services for this sample of children. A key difference in the activities and workflow was that RN triage was predominantly reactive and initiated by a change in a child’s condition. Care coordination was predominately proactive and initiated by the nurse to support health and chronic condition management. Proactive care coordination activities required more time than reactive triage activities. Consistent with the Value Model of nurse dose to patient complexity (Figure 1), these findings illustrate the value of integrating both a shared model of care coordination and a proactive, relationship-based model of care coordination. Skilled triage nurses at the basic level of nursing practice can respond to populations with low-complexity care coordination needs, while a designated APN for high-complexity care coordination can provide higher levels of intervention complexity within a broader scope of practice.
Analysis of qualitative data from interviews with providers, parents, and nurses, and reviews of documented care coordination encounters indicate increased parent satisfaction with a single contact for care coordination to decrease system navigation challenges. The shortened turnaround time for health forms and prescription updates have been identified as another source of satisfaction by both families and providers within the SNP. The opportunity costs saved with an independent APN coordinating care have allowed providers to focus on other hospital and clinic demands without interruption for consultation, orders and direction. Anecdotal comments from parents suggest that working with the APN care coordinator has prevented visits to the clinic and ED.
Participating in school individual education plan (IEP) meetings has allowed the APN to help community members involved with the child understand clinical implications of the patient’s condition to optimize accommodations. The APN care coordinator for the TeleFamilies project identified medication issues as one of the clinical problems related to patient complexity and lack of timely communication between subspecialists and primary care providers, as she described in an interview:
“[Subspecialists] may see the child and adjust a dose or stop a medication without updating the pharmacy order. They will stop one med and change the dose of another one without updating documentation or correspondence. …that isn’t entered in our medical record, so when [the child] comes into clinic, [the primary care provider] might assume a child is on a medication when it’s been stopped.”
Continuity of care and the APN’s ability to develop a relationship with families over time have provided families with a sense of trust and confidence in the healthcare home’s ability to meet the needs of their children in a timely, family-centered manner. As one parent explained, “We have [the APN care coordinator], and I would not want to live life without her. I don’t know how we did it before. She is there for everything we need for [our daughter]”. The APN provides families the opportunity to release some of the responsibility for making clinical decisions about their children. As the TeleFamilies APN noted,
“One of the challenges with care coordination is the balance between empowering parents to make their own decisions, but also saying, ‘You don’t have to make this [decision] – you don’t have to own diagnosing your kid”. [It’s knowing to ask,] “Are you doing okay… Do you need support…Do you need advice…Do you want me to do something… [or] do you want me to just listen?”
Documenting and discussing the APN’s perceptions and reflections on the process of care coordination in the TeleFamilies study has provided unique insights into the value of developing relationships with families over time in the care coordinator role. The TeleFamilies APN has an orientation to practice characterized by a family-centered, strengths-based approach. In the following example, the APN describes the importance of recognizing the layers of meaning behind a parent’s request when assessing care coordination needs:
“Sometimes a parent will call about a [clinical] concern that is upsetting, but the conversation switches to the fact that it’s hard to be a parent of a special needs child. Without a relationship with the family, [I might] have responded to the [clinical] issue they were calling about, when what they were really calling about was the fact that they hit the wall about having to deal with the same issue over and over, and that forever hope that there’s going to be a treatment or a medication that’s going to fix it and make it go away. Hitting the wall means, “I just can’t do this one more time.” It’s the realization that what you’re dealing with is what you have to deal with. And you don’t want to. In that kind of situation, I switch my focus. This is probably going to be an ongoing challenge that’s not going away. It’s not about a cure. It’s about managing things over time. Sometimes when a parent calls to ask for a thing – a test, a procedure, a medicine, an appointment – I need to be able to redirect that conversation to, “this isn’t really about a medicine or a test or a visit….How can I help you where you are, rather than tell you I can’t give you what you want because it’s not possible”… It’s helping families reflect on what they bring to the table, and addressing that, rather than, “what can I do”.
Implications for policy, research, and practice
Health care reform is leading to important changes in the healthcare delivery and reimbursement systems. There is a shift from fragmented, multiple provider care to integrated care across multiple care settings. The reimbursement model for this integrated care is also transitioning from a fee-for-service payment strategy to “total care” and bundling strategies for payments. The prior structure rewarded providers for performing procedures and failed to reimburse for coordination of care to prevent gaps in care, duplication of services and redundancy of care by various sub-specialists for the same patient. The ACA calls for providers to practice in accountable care organizations which will reimburse based on outcomes rather than procedures and visits (Office of the Legislative Council, 2010). Care coordination has been identified as a key solution to successfully achieving this new care model. The enhanced value of an APN care coordinator is the ability to understand the cross setting, cross discipline clinical risks and implement strategies to meet families’ unique needs and potentially affect clinical outcomes.
The TeleFamilies APN care coordinator position is fully funded by a research grant (R01NR010883). While such funding enables the systematic study of the effectiveness of this role, care coordinators ultimately need to be supported by a combination of reimbursement and a cost structure embedded into the clinic infrastructure. In practice, care coordination activities must be documented and tracked so that the role of the care coordinator is evident in the EHR. Analysis of cost data from this study will allow a calculation of the cost-benefit of this model of care coordination compared to usual care. It will also provide evidence for the cost benefit of adding clinic-to-home videoconferencing by the care coordinator, since families are randomly assigned to one of three groups (Figure 2). Studies such as this may provide the justification for reforming the reimbursement system to pay for models of care coordination that maximize the fit between the complexity of service needs of CCSHCN and the APN role and scope of practice.
APNs are accustomed to providing direct care in a clinical setting. Although coordination of an individual patient’s care within a single setting is a core role of primary and specialty practice PNPs, the coordination across settings is a broader application of those core role functions. Expanding beyond a unique patient group to coordinate for complex children across multiple setting and multiple sub-specialties is a natural role application for APN skill sets. It is also a departure from revenue generating roles to efficiencies of care for the patient population served. Additional research in the cost effectiveness of the APN contribution to care management as compared to other clinical staff will be key to sustainability of this role as compared to less costly but less skilled alternatives.
Care coordination for children with complex health conditions is challenging and requires the infrastructure of a healthcare home where care coordination as a process is clearly articulated for families and the health care team. Having a dedicated APN care coordinator who is able to address high complexity care needs and work with families of children with SHCN over time has the potential of decreasing fragmentation of care and improving the efficiency of care delivered by the tea. Analysis of data from the TeleFamilies study will enable our team to test the hypothesis that this model of care will result in improved outcomes for children and families.
Acknowledgments
This project was supported in part by grant 1R01NR010883 from the National Institute of Nursing Research, NIH, and grant T80-MC00010 from the Maternal Child Health Bureau, Health Resources and Services Administration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Wendy S. Looman, School of Nursing, University of Minnesota, Twin Cities
Elizabeth Presler, Shriners Hospital for Children, Lexington.
Mary M. Erickson, Children’s Hospitals and Clinics of Minnesota
Ann E. Garwick, School of Nursing, University of Minnesota, Twin Cities
Rhonda G. Cady, Lab Medicine and Pathology, University of Minnesota, Twin Cities
Anne M. Kelly, Minneapolis, Minnesota
Stanley M. Finkelstein, Laboratory Medicine and Pathology, University of Minnesota, Twin Cities
References
- American Academy of Pediatrics. Council on Pediatric Practice. AAP . Standards of Child Care. Evanston, IL: 1967. Pediatric records and a “medical home; pp. 77–79. [Google Scholar]
- American Academy of Pediatrics. Medical Homes Initiatives for Children with Special Health Care Needs Project Advisory Committee The medical home. Pediatrics. 2002;110:184–186. [Google Scholar]
- Antonelli R, McAllister JW, Popp J. Making care coordination a critical component of the pediatric health system: A multidisciplinary framework. The Commonwealth Fund. 2009 pub. no. 1277. http://www.commonwealthfund.org/Content/Publications/Fund-Reports/2009/May/Making-Care-Coordination-a-Critical-Component-of-the-Pediatric-Health-System.aspx.
- Bodenheimer T. Coordinating care - a perilous journey through the health care system. The New England Journal of Medicine. 2008;358(10):1064. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- Brooten D, Youngblut JM. Nurse dose as a concept. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2006;38(1):94–99. doi: 10.1111/j.1547-5069.2006.00083.x. [DOI] [PubMed] [Google Scholar]
- Brooten D, Youngblut J, Deatrick J, Naylor M, York R. Patient problems, advanced practice nurse (APN) interventions, time, and contacts among five patient groups. Journal of Nursing Scholarship. 2003;35(1):73–79. doi: 10.1111/j.1547-5069.2003.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant-Lukosius D, Dicenso A, Browne G, Pinelli J. Advanced practice nursing roles: Development, implementation and evaluation. Journal of Advanced Nursing. 2004;48(5):519–529. doi: 10.1111/j.1365-2648.2004.03234.x. doi:10.1111/j.1365-2648.2004.03234.x. [DOI] [PubMed] [Google Scholar]
- Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646. doi: 10.1542/peds.2009-1658. doi:10.1542/peds.2009-1658. [DOI] [PubMed] [Google Scholar]
- Cady R. Time-motion study of standard clinic RN telephone triage and APN care coordination for children with special health care needs. Department of Laboratory Medicine and Pathology, School of Medicine, University of Minnesota; Minneapolis: 2011. Unpublished manuscript. [Google Scholar]
- Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, Srivastava R. Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538. doi: 10.1542/peds.2010-0910. doi:10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grupp-Phelan J, Lozano P, Fishman P. Health care utilization and cost in children with asthma and selected comorbidities. The Journal of Asthma: Official Journal of the Association for the Care of Asthma. 2001;38(4):363–373. doi: 10.1081/jas-100001492. [DOI] [PubMed] [Google Scholar]
- Gupta VB, O’Connor KG, Quezada-Gomez C. Care coordination services in pediatric practices. Pediatrics. 2004;113(Supplement 4):1517–1521. [PubMed] [Google Scholar]
- McAllister JW, Presler E, Cooley WC. Practice-based care coordination: A medical home essential. Pediatrics. 2007;120(3):e723–33. doi: 10.1542/peds.2006-1684. doi:10.1542/peds.2006-1684. [DOI] [PubMed] [Google Scholar]
- McDonald KM, Sundaram V, Bravata DM. Care coordination. In: Shojania KG, McDonald KM, Wachter RM, Owens DK, editors. Closing the quality gap: A critical analysis of quality improvement strategies. Agency for Healthcare Research and Quality; Rockville, MD: 2007. [PubMed] [Google Scholar]
- Minnesota Department of Health Health Care Homes. 2011 Retrieved from http://www.health.state.mn.us/healthreform/homes.
- Nageswaran S, Silver EJ, Stein RE. Association of functional limitation with health care needs and experiences of children with special health care needs. Pediatrics. 2008;121(5):994–1001. doi: 10.1542/peds.2007-1795. doi:10.1542/peds.2007-1795. [DOI] [PubMed] [Google Scholar]
- National Association of Pediatric Nurse Practitioners Position statement on Pediatric Healthcare/Medical Home: Key issues on delivery, reimbursement, and leadership. Journal of Pediatric Health Care. 2009;23:23A–24A. [Google Scholar]
- National Research Council . Crossing the quality chasm: A new health system for the 21st century. National Academies Press; Washington, DC: 2001. Retrieved from http://www.nap.edu. [PubMed] [Google Scholar]
- Neff JM, Sharp VL, Muldoon J, Graham J, Myers K. Profile of medical charges for children by health status group and severity level in a washington state health plan. Health Services Research. 2004;39(1):73–89. doi: 10.1111/j.1475-6773.2004.00216.x. doi:10.1111/j.1475-6773.2004.00216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Archives of Pediatrics & Adolescent Medicine. 2005;159(1):10–17. doi: 10.1001/archpedi.159.1.10. doi:10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- Office of the Legislative Council, US House of Representatives Compilation of Patient Protection and Affordable Care Act; 111th Congress 2d Session; May 2010; Print 111-1. [Google Scholar]
- Orszag PR, Emanuel EJ. Health care reform and cost control. The New England Journal of Medicine. 2010;363(7):601–603. doi: 10.1056/NEJMp1006571. doi:10.1056/NEJMp1006571. [DOI] [PubMed] [Google Scholar]
- Palfrey JS. How health care reform can benefit children and adolescents. The New England Journal of Medicine. 2009;361(17):e34. doi: 10.1056/NEJMp0908051. doi:10.1056/NEJMp0908051. [DOI] [PubMed] [Google Scholar]
- Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the united states. JAMA : The Journal of the American Medical Association. 2007;297(24):2755–2759. doi: 10.1001/jama.297.24.2755. doi:10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- Ruel J, Motyka C. Advanced practice nursing: A principle-based concept analysis. Journal of the American Academy of Nurse Practitioners. 2009;21(7):384–392. doi: 10.1111/j.1745-7599.2009.00415.x. doi:10.1111/j.1745-7599.2009.00415.x. [DOI] [PubMed] [Google Scholar]
- Safriet BJ. The Future of Nursing: Leading Change, Advancing Health. Institute of Medicine; 2011. Federal options for maximizing the value of advanced practice nurses in providing quality, cost-effective health care. Retrieved from http://www.iom.edu/~/media/Files/Activity%20Files/Workforce/Nursing/Federal%20Options%20for%20Maximizing%20the%20Value%20of%20Advanced%20Practice%20Nurses.pdf. [Google Scholar]
- Sia C, Tonniges TF, Osterhus E, Taba S. History of the medical home concept. Pediatrics. 2004;113:1473–1478. [PubMed] [Google Scholar]
- Stein RE, Jessop DJ. Functional status II(R). A measure of child health status. Medical Care. 1990;28(11):1041–1055. doi: 10.1097/00005650-199011000-00006. [DOI] [PubMed] [Google Scholar]
- Tennant PW, Pearce MS, Bythell M, Rankin J. 20-year survival of children born with congenital anomalies: A population-based study. Lancet. 2010;375(9715):649–656. doi: 10.1016/S0140-6736(09)61922-X. doi:10.1016/S0140-6736(09)61922-X. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . The national survey of children with special health care needs chartbook 2005-2006. U.S.: USDHHS, Health Resources and Services Administration, Maternal and Child Health Bureau; Rockville, Maryland: 2008. Retrieved from http://mchb.hrsa.gov/cshcn05/ [Google Scholar]
- Wise PH, Huffman LC, Brat G. A critical analysis of care coordination strategies for children with special health care needs. Agency for Healthcare Research and Quality; Rockville, MD: 2007. No. Technical Review No. 14. AHRQ Publication No. 07-0054.). Rockville (MD) [PubMed] [Google Scholar]