Abstract
Avoidance coping and symptoms of posttraumatic stress disorder (PTSD) covary. However, relatively little research has examined the bi-directional relation between these constructs among individuals in treatment for PTSD. The current longitudinal study examined the reciprocal associations between avoidance coping and PTSD symptom severity during and after residential PTSD treatment among a sample of 1,073 military veterans (88.9% male; Mage = 52.39 years) with chronic, treatment-resistant PTSD. Greater avoidance coping at intake predicted more severe PTSD symptoms at discharge, and severity of PTSD symptoms at discharge predicted increased avoidance at follow-up. Conversely, PTSD symptom severity at intake was not related to avoidance coping at discharge, and in turn avoidance coping at discharge was not related to PTSD symptom severity at follow-up. These findings offer a number of important clinical implications including evidence suggesting avoidance may predict poorer treatment response among individuals seeking treatment for chronic PTSD, and that greater end-of-treatment PTSD symptom severity may predict increased avoidance following treatment.
Keywords: Posttraumatic Stress, PTSD, Avoidance, Treatment
Avoidance coping has been defined as efforts to distance oneself from aversive situations or negative emotional reactions (Litman, 2006; Roth & Cohen, 1986). Theoretical models of posttraumatic stress disorder (PTSD) have posited a central role of avoidance in the maintenance of posttraumatic stress symptoms via interfering with processing of the traumatic experience and preventing incorporation of safety learning into these informational networks (e.g., Foa & Kozak, 1986; Keane, Zimering & Caddell, 1985; Resick & Schnicke, 1992). Cross-sectional research suggests that individuals with PTSD are apt to employ avoidance coping strategies (Amir, Kaplan, Efroni, Levine, & Kotler, 1997; Nezu & Carnevale, 1987; Sutker, Davis, Uddo, & Ditta, 1995). Moreover, longitudinal research suggests greater avoidance of thoughts, feelings, or other reminders associated with a traumatic experience predicts later PTSD symptom severity even after accounting for initial symptom levels (Gutner, Rivzi, Monson, & Resick, 2006; Jacobsen et al., 2000; Krause, Kaltman, Goodman, & Dutton, 2008; Pineles et al., 2011). Similarly, general avoidance coping (as opposed to traumatic event-specific avoidance) both prior to (Gil, 2005) and following (Eld, 2003; Marx & Sloan, 2005) exposure to a traumatic event prospectively predicts greater PTSD severity.
Importantly, avoidance coping and PTSD severity appear bi-directionally related. Benotsch and colleagues (2000) assessed Gulf War veterans at approximately 14 and 27 months after returning from deployment. General avoidance coping (trauma-specific) at Time 1 predicted PTSD severity and diagnostic status at Time 2. Additionally, PTSD symptom severity at Time 1 predicted general avoidance coping at Time 2 after controlling for initial levels of avoidance coping. In combination, PTSD symptoms and avoidance coping appear to exert reciprocal influences on each other across the course of recovery from traumatic event exposure, outside the context of treatment.
Relatively little research has examined the interplay between avoidance and PTSD severity during or following treatment, and existing research offers a somewhat inconsistent picture. Models of PTSD treatment are often predicated on the idea that PTSD severity and avoidance coping are bi-directionally related and both should be targeted in treatment (Foa & Kozak, 1986; Orsillo & Batten, 2005; Resick & Schnicke, 1992; Shapiro, 1989). Patients are taught that distress associated with posttraumatic stress reactions to traumatic event exposure is likely to lead to increased use of avoidance as a coping strategy, and such avoidance serves to maintain PTSD. The only study to directly examine avoidance coping as a predictor of response to PTSD treatment included a sample of rape victims who were randomly assigned (in the context of a controlled treatment efficacy trial) to receive either nine weeks of prolonged exposure or eye movement desensitization and reprocessing (Leiner, Kearns, Jackson, Astin, & Rothbaum, in press). Collapsed across groups, rape-related avoidance coping prior to treatment was negatively correlated with post-treatment PTSD symptom severity after accounting for initial symptom levels. That is, patients with PTSD who were more apt to employ avoidant coping strategies were more likely to evince reductions in PTSD symptom severity during treatment. Conversely, in the only other relevant study in this domain, Tiet and colleagues (2006) examined the longitudinal association between traumatic event-specific avoidance coping and PTSD symptom severity among predominantly male veterans diagnosed with PTSD who had attended at least one treatment visit through the Veterans Affairs (VA) Healthcare System in the two months prior to the initial assessment. Cognitive avoidance strategies (e.g., denying the seriousness of the problem, avoiding distressing thoughts or feelings related to the event) at baseline were positively correlated with PTSD symptom severity 10 months later. Moreover, baseline PTSD symptom severity was positively related to behavioral avoidance (e.g., withdrawing from others, engaging in distracting behaviors), but not cognitive avoidance over time. These results suggest greater avoidance may be associated with greater PTSD severity among people receiving treatment.
Multiple aspects of the findings regarding the reciprocal relations between avoidance and PTSD symptom severity among treatment-seeking samples highlight the need for additional research in this area. First, methodological differences across the two studies such as sample characteristics (e.g., traumatic event type, gender composition) and treatment approach (controlled treatment efficacy trial vs. VA outpatient treatment) make drawing general inferences difficult. Second, in the study reported by Tiet and colleagues (2006), assessments were not regularly administered at particular time points during treatment. Although participants all endorsed completing at least one treatment session within the previous two months, they did not necessarily attend treatment sessions during the study. Indeed, participants received a range of 0-25 treatment sessions in the 6 months prior to the follow-up assessment. Accordingly, conclusions regarding the reciprocal relations between avoidance and PTSD severity during treatment based on Tiet and colleagues’ results as well as comparisons between their results and those of Leiner and colleagues (in press) must be considered tentative. Third, the conflicting results described above yield uncertainty regarding how PTSD severity and avoidance coping relate across the course of PTSD treatment. Accordingly, additional research is needed to better understand the relation between PTSD symptom severity and avoidance coping during and after treatment.
The current study sought to build upon extant research by offering a novel approach to examining the bi-directional relation between avoidance coping and PTSD symptom severity during and after treatment for PTSD. First, a standardized assessment strategy was employed (cf., Tiet et al., 2006) wherein avoidance and PTSD severity were measured at intake, treatment discharge, and a four-month follow-up. Examination of data regarding avoidance coping and PTSD symptom severity at follow-up is considered a significant strength of the current design, given that these relations may change following treatment termination. Moreover, the current study was the first to examine relations with general, as opposed to traumatic event-specific, avoidance coping in a treatment-seeking sample. Participants in the current study included veterans with chronic PTSD who did not respond to initial outpatient treatment. Testing the bi-directional relations between avoidance and PTSD symptom severity among individuals with chronic treatment-resistant PTSD yields important and novel insight into how these factors influence one another in a unique sample, thereby extending the currently limited evidence base in this domain. Furthermore, examining these factors in such a sample has the potential to suggest avenues for advancing treatments for this population. Given the treatment-resistant nature of the sample, we expected that PTSD symptom severity and levels of avoidance coping would be fairly stable across time. We further expected that avoidance and PTSD severity would be positively related at each assessment point. In terms of the associations between factors across time, we hypothesized that elevated avoidance at baseline would predict greater PTSD severity at discharge, which would in turn predict greater avoidance at follow-up. This hypothesis is consistent with observations of the relations between these factors outside of the context of treatment (given the treatment-resistant nature of the sample) and theories positing that avoidance interferes with reduction of PTSD symptoms (Benotsch et al., 2000; Foa & Kozak, 1986; Orsillo & Batten, 2005; Resick & Schnicke, 1992; Shapiro, 1989; Tiet et al., 2006). A secondary aim of the study was to conduct a novel examination of how pre-treatment PTSD severity relates to avoidance at discharge, and in turn how avoidance at discharge predicts PTSD severity at follow-up. An absence of evidence in this area precluded hypotheses regarding how baseline PTSD severity would relate to discharge levels of avoidance, but we did expect that discharge avoidance would be positively associated with PTSD severity at follow-up based on prior work (Benotsch et al., 2000).
Method
Sample and Procedures
Participants were 1,073 military veterans admitted to a VA residential rehabilitation program for PTSD between 2000 and 2008 (88.9% male; Mage = 52.39 years, SD = 8.41 years; range = 19 – 80 years). Participants who completed at least one of the primary measures of interest at program intake were included in the study (n = 1073). Participants who completed measures at intake only did not significantly differ from those who returned for either the discharge (n = 717) or follow-up (n = 456) assessments in terms of PTSD symptom severity or avoidance coping at treatment intake. Most participants (78.5%) were exposed to some form of combat with the majority reporting combat experiences in Vietnam (58.5%), followed by the Persian Gulf (19.2%), Iraq (15.8%) and Afghanistan (4.1%); however, not all participants reported the theatre of operations in which they were exposed to combat. Per participant reports, the racial/ethnic composition of the sample was as follows: Caucasian (58.6%), African American (17.4%), Hispanic/Latino/a (14.4%), Mixed Ethnicity (3.7%), Native American/Alaskan Native (2.3%), Asian/Pacific Islander (2.1%), and “Other” (1.5%). Participants were admitted for PTSD treatment at a residential rehabilitation program of a VA Medical Center (Mlength of stay = 66.21 days; SD = 27.9 days). This program admits clinician-referred military veterans with severe PTSD whose symptoms have not been successfully ameliorated with outpatient treatment. Exclusion criteria for enrollment in the program included: (a) substance use within 15 days of the start of treatment, (b) current psychotic symptoms, and (c) medical conditions that would substantially interfere with or prevent participation in residential treatment (i.e., those unable to move about independently). A group format that primarily adopted a cognitive-behavioral orientation was used exclusively in treatment for all individuals. In cases where individuals were admitted to the program more than one time, data were used from the first admission. The 4-month follow-up assessment was administered by mail. Mailings were sent to patients 3 months post treatment discharge and received by program staff by the 4-month post-treatment discharge date. All procedures were approved by the local Institutional Review Board for Human Subjects Research.
Measures
PTSD symptom severity
The PTSD Checklist-Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993) was used to measure PTSD symptom severity at each assessment. The PCL-M consists of 17 items that measure PTSD symptoms as defined by the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition – Text Revision (DSM-IV-TR, American Psychiatric Association, 2000). At each time point, respondents were asked to indicate the degree to which they have been bothered by each symptom within the past month, using a 5-point scale (1 = not at all bothered; 5 = extremely bothered). Items were aggregated into three subscales, which corresponded to the DSM symptom clusters (i.e., re-experiencing, avoidance/numbing, and hyperarousal). Across a number of samples, the PCL-M has shown excellent psychometric properties, as well as strong convergent and divergent validity (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Ruggiero, Del Ben, Scotti, & Rabalais, 2003). Descriptive statistics and internal reliabilities for all scales are included in Table 1.
Table 1. Descriptive Statistics and Reliabilities (Cronbach’s alpha) for PTSD Symptom Severity and Avoidance Coping at All Time-Points.
| Variable | Mean (SD) | Range | Cronbach’s Alpha |
|---|---|---|---|
| Intake | |||
| Avoidance Coping | 12.08 (4.40) | 5.00 – 24.00 | .74 |
| - Denial | 4.24 (1.92) | 1.00 – 8.00 | .70 |
| - Behavioral disengagement | 4.18 (1.85) | 1.00 – 8.00 | .71 |
| - Substance use | 3.67 (2.37) | 1.00 – 8.00 | .96 |
| PTSD symptom severity | 64.78 (10.76) | 22.00 – 85.00 | .89 |
| - Re-experiencing | 17.99 (4.35) | 5.00 – 25.00 | .88 |
| - Avoidance/numbing | 27.16 (4.82) | 9.00 – 35.00 | .76 |
| - Hyperarousal | 19.63 (3.58) | 5.00 – 25.00 | .79 |
| Discharge | |||
| Avoidance Coping | 12.10 (4.91) | 3.00 – 24.00 | .80 |
| - Denial | 4.43 (1.98) | 1.00 – 8.00 | .70 |
| - Behavioral disengagement | 4.33 (2.04) | 1.00 – 8.00 | .75 |
| - Substance use | 3.36 (2.29) | 1.00 – 8.00 | .94 |
| PTSD symptom severity | 58.86 (14.36) | 3.00 – 85.00 | .94 |
| - Re-experiencing | 17.34 (4.57) | 5.00 – 25.00 | .90 |
| - Avoidance/numbing | 23.81 (6.57) | 7.00 – 35.00 | .87 |
| - Hyperarousal | 17.80 (4.52) | 3.00 – 25.00 | .87 |
| Follow-up | |||
| Avoidance Coping | 11.67 (4.23) | 6.00 – 24.00 | .75 |
| - Denial | 4.33 (1.96) | 2.00 – 8.00 | .70 |
| - Behavioral disengagement | 4.13 (1.89) | 1.00 – 8.00 | .77 |
| - Substance use | 3.22 (2.04) | 1.00 – 8.00 | .97 |
| PTSD symptom severity | 60.07 (14.48) | 3.00 – 85.00 | .93 |
| - Re-experiencing | 16.94 (4.76) | 1.00 – 25.00 | .90 |
| - Avoidance/numbing | 25.00 (5.93) | 3.00 – 35.00 | .83 |
| - Hyperarousal | 18.65 (4.27) | 4.00 – 25.00 | .83 |
Avoidance coping
Three scales from a revised version of the 24-item Brief COPE (Carver, 1997) were used to measure avoidance coping: denial, behavioral disengagement, and substance use. Each scale was comprised of 2 items, rated on 4-point Likert scale (1 = I haven’t been doing this at all; 4 = I’ve been doing this a lot), which reflected the frequency with which a particular coping style was used in the past week. The Brief COPE has excellent psychometric properties, and individual subscales and composite scales have demonstrated good construct validity based on their pattern of associations with a wide-range of constructs (Carver, 1997; Carver, Scheier, & Weintraub, 1989). The subscales used to compose the avoidant coping factor were similar to those utilized in previous studies employing the Brief COPE to measure avoidance coping (see Litman [2006] for a review). Table 1 includes descriptive statistics and internal reliabilities for this measure.
Data Analysis
A latent variable (LV) structural modeling approach in Mplus 5.2 (Muthén & Muthén, 1998-2009) was used to construct cross-lagged path models to examine associations over time between PTSD symptom severity and avoidance coping. Such an approach has been used widely to estimate the fit of causal models based on nonexperimental, longitudinal data (Finkel, 1995). Model fit was evaluated using the chi-square goodness-of-fit test (χ2), the comparative fit index (CFI; Bentler, 1990), the Tucker-Lewis index (TLI; Tucker & Lewis, 1973), the root-mean-square error of approximation (RMSEA; Browne & Cudeck, 1993), and the standardized root-mean-square residual (SRMR; Bentler, 1995). Per the recommendations of Hu and Bentler (1999), CFI and TLI values > .95 and RMSEA and SRMR values < .06 indicate a good fitting model. For all models, the maximum-likelihood estimator (MLE) was used, which allows for missing data estimation and assumes that the data under analysis fits a multivariate normal distribution.
Following the recommendations of Bentler (2000) and others (e.g., Mulaik & Millsap, 2000), model fitting procedures proceeded in two stages. First, measurement models for PTSD symptom severity and avoidance coping were fit using data at all three time points simultaneously. That is, at each time point, the three PTSD symptom clusters of re-experiencing, avoidance and numbing, and hyperarousal were used as observed indicators of a PTSD symptom severity LV, and the three subscales of denial, behavioral disengagement, and substance use were used as indicators of an avoidance coping LV. For these models, covariances among all LVs were freely estimated, as were the covariances between residual error terms of analogous indicators over time (e.g., residual variance of denial coping at intake was allowed to covary with the residual variance of denial coping at discharge). For the sake of parsimony and to minimize the number of parameters requiring estimation, we also tested the fit of a measurement model in which analogous factor loadings were constrained to be equal across time (e.g., factor loadings for denial coping at intake, discharge, and follow-up were constrained to be equal).
At the second stage, cross-lagged models were tested in which paths were estimated from the LVs at each time point to the opposite LV at the subsequent time point. For example, causal paths were modeled from PTSD symptom severity at intake to avoidance coping at discharge, and from avoidance coping at intake to PTSD symptom severity at discharge. Estimation of these models began with a fully-saturated model that included auto-regressions from intake to discharge and discharge to follow-up, as well as auto-regressions and cross-lagged paths from intake to follow-up. To improve model parsimony, we subsequently tested the fit of a series of nested models in which paths were either removed or analogous regression coefficients constrained to be equal over time (e.g., cross-lagged paths from PTSD symptom severity at intake to avoidance coping at discharge and PTSD symptom severity at discharge to avoidance coping at follow-up were fixed to be equal). The significance of the decrease in fit across these nested models was evaluated with chi-square likelihood ratio tests.
Results
Descriptive Statistics
Descriptive information for PTSD symptoms and avoidance coping at each time point is presented in Table 1. Paired samples t-tests demonstrated a significant decrease in PTSD symptom severity from intake to follow-up (t = 5.21, p < .001, d = −.25). Examination of this pattern revealed a significant decrease in symptoms from intake to discharge (t = 11.49, p < .001, d = −.47), and a significant increase from discharge to follow-up (t = −4.75, p < .001, d = .24). Avoidance coping also decreased from intake to follow-up (t = 2.89, p < .01, d = −.23). There was no significant change in avoidance coping from intake to discharge (t = 1.74, p = .08, d = −.06), but there was a significant decrease in avoidance coping from discharge to follow-up (t = 4.04, p < .001, d = −.23).
Measurement Models
The initial measurement model consisted of three LVs of PTSD symptom severity (one at each time point) and three LVs of avoidance coping (one at each time point). All covariances between LVs and residual error terms for analogous indicators across time were freely estimated. This model, which allowed analogous factor loadings to differ across time, fit the data well: χ2 (102, N = 1073) = 198.19, CFI = .981, TLI = .972, RMSEA = .030, SRMR = .043. Subsequently, we estimated a model in which analogous factor loadings for each indicator were constrained to be equal over time. This more parsimonious model also fit the data well: χ2 (110, N = 1073) = 222.82, CFI = .978, TLI = .969, RMSEA = .031, SRMR = .052. Across the indicators of PTSD symptom severity, the mean factor loadings at intake, discharge, and follow-up were .75, .86, and .83, respectively. Across the indicators of avoidance coping, the mean factor loadings at intake, discharge, and follow-up were .53, .65, and .56, respectively.
Cross-Lagged Path Models
Fit indices for cross-lagged models of associations between PTSD symptom severity and avoidance coping over time are presented in Table 2. Each model controlled for length of stay in treatment. For Model 1, all cross-lagged and autoregressive paths between the LVs were freely estimated (i.e., a fully cross-lagged model). This model represented a reparameterization of the measurement model such that cross-time covariances were converted to regression estimates in which LVs measured at a common time point were regressed onto the LVs at all previous time points (e.g., PTSD symptom severity and avoidance coping were correlated at follow-up and modeled as being predicted by PTSD symptom severity and avoidance coping at both intake and discharge). This base model fit the data well (see fit indices in Table 2).
Table 2. Fit Indices for Cross-lagged Models of Associations Between PTSD Symptom Severity and Avoidance Coping over Time.
| Model | χ2 (df) | CFI | TLI | RMSEA | SRMR | Δχ2 (Δdf) | p value |
|---|---|---|---|---|---|---|---|
| Model 1 | 245.11 (122) | .976 | .966 | .031 | .050 | -- | -- |
| Model 2 | 245.32 (124) | .976 | .967 | .030 | .050 | 0.21 (2) | .900 |
| Model 3 | 263.30 (126) | .973 | .964 | .032 | .054 | 17.98 (2) | <.001 |
| Model 4 | 258.37 (126) | .974 | .965 | .031 | .056 | 13.05 (2) | <.01 |
| Model 5 | 250.77 (126) | .976 | .967 | .030 | .052 | 5.45 (2) | .066 |
Notes. CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root-Mean-Square Error of Approximation; SRMR = Standardized Root-Mean-Square Residual. Δχ2 (Δdf) = chi-square and degrees of freedom based on likelihood ratio tests. Model 2 was compared to Model 1. All other models were compared to Model 2. Bold indicates the best-fitting model. All models controlled for length of stay in treatment.
In Model 2, we removed the cross-lagged paths from each LV at intake to the opposite LV at the follow-up assessment (i.e., PTSD at intake to avoidance coping at follow-up, and avoidance coping at intake to PTSD at follow-up). This model also fit the data well and did not result in a significant decrease in fit relative to Model 1 [Δχ2 (2) = 0.21, p = .900] and was therefore retained. In Model 3, the autoregressive paths from intake to follow-up for equivalent LVs were removed (i.e., the path from PTSD at intake to PTSD at follow-up, and the path from avoidance coping at intake to avoidance coping at follow-up). This resulted in a significant decrease in fit in comparison with Model 2 [Δχ2 (2) = 17.98, p < .001]; hence, this model was rejected. In Model 4, analogous autoregressive paths for PTSD and avoidance coping were constrained to equality (e.g., the path from PTSD at intake to PTSD at discharge was constrained to be equal to the path from PTSD at discharge to PTSD at follow-up). This resulted in a significant decrease in fit in comparison with Model 2 [Δχ2 (2) = 13.05, p < .01]; thus, Model 4 was also rejected. For Model 5, analogous cross-lagged paths were constrained to equality (e.g., the path from PTSD at intake to avoidance coping at discharge was constrained to be equal to the path from PTSD at discharge to avoidance coping at follow-up). In a nested comparison with Model 2, these model constraints resulted in a significant (trend-level) decrease in fit, Δχ2 (2) = 5.45, p = .066. Although retention of this model may be suggested based on parsimony, a comparison of the analogous cross-lagged paths from the model in which they were not constrained revealed marked differences in the magnitude of the parameter estimates. Thus, Model 5 was rejected in favor of Model 2.
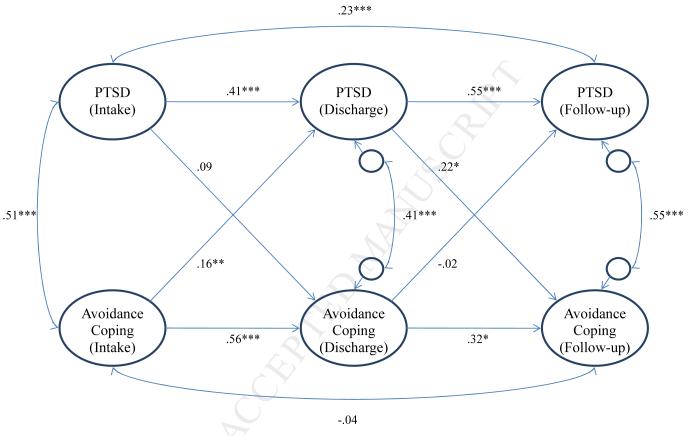
Figure 1 provides the parameter estimates from the best-fitting cross-lagged model (Model 2). The covariate of length of stay in treatment was not associated with PTSD (r = .05, ns) or avoidance coping (r = .06, ns) at intake, PTSD (β = −.02, ns) or avoidance coping (β = .03, ns) at discharge, or avoidance coping at follow-up (β = −.02, ns), but was significantly associated with PTSD at follow-up (β = −.11, p < .05). At intake, PTSD symptom severity and avoidance coping were moderately positively correlated, as were the residuals of these variables at discharge and follow-up (i.e., after controlling for previous levels of each variable). The autoregressive paths indicated that both PTSD symptom severity and avoidance coping were moderately stable and significant from intake to discharge, and from discharge to follow-up (the stability of avoidance coping over the latter timeframe was slightly reduced, but remained significant). Regarding the cross-lagged associations, PTSD symptom severity at intake was not significantly associated with avoidance coping at discharge (controlling for the stability of avoidance coping over this timeframe). However, controlling for the stability of PTSD symptom severity, greater use of avoidance coping at intake was significantly associated with greater severity of PTSD symptoms at discharge. Conversely, from discharge to follow-up, controlling for the stability of PTSD symptom severity over this time period, avoidance coping at discharge was not significantly associated with PTSD symptom severity at follow-up. However, controlling for the stability of avoidance coping, greater severity of PTSD symptoms at discharge was significantly associated with greater use of avoidance coping at follow-up.
Figure 1.
Structural Model of Cross-lagged Associations Between PTSD Symptom Severity and Avoidance Coping across Intake, Discharge and Follow-up. Parameter estimates shown are standardized beta coefficients. *p < .05, **p < .01, ***p < .001. For the sake of parsimony, associations between the model variables and the covariate of length of stay in treatment are not shown here, but are provided in the Results section.
Discussion
Efficacious clinical interventions for PTSD typically teach clients that avoidance and PTSD symptoms are bi-directionally related and seek to simultaneously reduce both of these factors (Foa & Kozak, 1986; Orsillo & Batten, 2005; Resick & Schnicke, 1992; Shapiro, 1989). However, evidence regarding how avoidance and PTSD severity relate to one another across the course of treatment is not clear. The current novel extension to this literature employed a standardized repeated assessment to examine the relation between PTSD severity and general avoidance coping among veterans with chronic PTSD, who had not responded to initial outpatient treatment, during and following residential treatment for PTSD.
We observed several findings that were consistent with hypotheses. Although significant decreases in both PTSD symptom severity and avoidance coping were evidenced from intake to follow-up, overall levels of PTSD symptom severity and avoidance coping did not evince substantial reductions across time (see Table 1). This pattern, consistent with prior work in a similar sample (Boden, Bonn-Miller, Vujanovic, & Drescher, in press), was not surprising given the chronic nature of the PTSD characterizing this treatment-resistant sample of veterans. Also, as predicted, PTSD severity and avoidance coping evidenced medium to large (Cohen, 1992) positive relations when assessed concurrently, and these associations remained significant even after statistically controlling for levels of each, measured at the previous assessment. This pattern is consistent with research documenting comparable cross-sectional relations (Marx & Sloan, 2005; Sutker et al., 1995; Tiet et al., 2006). Taken together, this pattern highlights that within this treatment-resistant sample of veterans with chronic PTSD, avoidance and symptom severity are, on average, relatively stable and interrelated at treatment initiation and discharge, as well as four months post-treatment.
Prospective relations between avoidance and PTSD severity also emerged and were partially consistent with hypotheses. Relatively greater avoidance coping at intake prospectively predicted more severe PTSD at discharge, which in turn prospectively predicted greater avoidance at follow-up. This series of associations was observed after statistically controlling for the stability of both PTSD severity and avoidance coping across time. The pre- to post-treatment link between avoidance and subsequent PTSD severity suggests avoidance coping is an important predictor of treatment response among individuals with chronic PTSD, which is generally consistent with PTSD treatment models (Foa & Kozak, 1986; Resick & Schnicke, 1992; Shapiro, 1989). Interestingly, this pattern is inconsistent with evidence suggesting level of avoidance coping prior to treatment negatively predicts PTSD severity after controlled, evidence-based treatment for rape-related PTSD (Leiner et al., in press). It is possible that elevated levels of avoidance prior to efficacious treatment mark greater room for improvement, and therefore greater treatment-related change may be observed (Leiner et al., in press). In contrast, the treatment-resistant sample studied here did not evince large improvements on average, and therefore greater avoidance pre-treatment predicted greater maintenance of symptom severity, which is consistent with prospective research outside of treatment contexts (Eld, 2003; Gil, 2005; Marx & Sloan, 2005). Accordingly, the present findings suggest that an empirical test is now needed of treatment response as a factor that affects the relation between pre-treatment avoidance and post-treatment PTSD severity. The current pattern of results further demonstrates that relatively elevated PTSD severity at treatment discharge predicts greater avoidance four months post-treatment. These results bolster findings that elevated PTSD symptoms, outside of the context of treatment, predict increased use of avoidant coping strategies (Benotsch et al., 2000).
Taken together, these results suggest relatively elevated pre-treatment avoidance among treatment-resistant veterans with chronic PTSD may maintain PTSD severity during inpatient treatment, and that PTSD severity post-treatment may, in turn, potentiate avoidance coping post-treatment. This pattern is consistent with learning-based accounts of PTSD that suggest people with relatively severe PTSD are likely to adopt avoidant coping strategies, which interfere with recovery from symptomatic reactions to traumatic event exposure (Foa & Kozak, 1986; Keane et al., 1985). Importantly, these inferences should be considered cautiously as the degree to which they apply to non-veterans and people who are suffering from less chronic PTSD is not clear. Examination of these factors among samples with greater representation of women with chronic PTSD and men with less chronic PTSD and greater variability in treatment response is needed.
Pre-treatment PTSD severity did not predict avoidance coping at discharge, which in turn was not associated with PTSD severity at follow-up. It is possible that this pattern is primarily attributable to the chronicity of the PTSD characterizing the sample. Relatively more treatment responsive clients would be expected to evidence greater decreases in avoidance coping during treatments that target avoidance (e.g., Foa & Kozak, 1986; Orsillo & Batten, 2005; Resick & Schnicke, 1992; Shapiro, 1989). The fact that this sample was comprised of treatment-resistant patients who evinced relatively stable levels of PTSD severity and avoidance coping suggests avoidance may not have been greatly influenced regardless of baseline PTSD severity. Although to the best of our knowledge no data have been reported regarding the degree to which pre-treatment PTSD severity predicts change in general avoidance coping during treatment (particularly within a treatment-resistant sample), treatment discharge levels of avoidance would be expected to predict PTSD severity during follow-up (Benotsch et al., 2000). Given independent replication of this pattern, research is needed to elucidate why treatment-discharge levels of avoidance are unrelated to subsequent levels of PTSD symptom severity.
A number of study limitations, in addition to those noted above, warrant consideration. First, confidence in the findings would have been strengthened by the use of a clinical interview to measure PTSD symptom severity. Similarly, although the current study utilized a well-established measure of general avoidance coping, future research would benefit from examining reciprocal associations between PTSD symptom severity and both general and traumatic event-specific avoidance across the course of treatment to determine if distinct patterns emerge across these different types of avoidance. Reliance on retrospective self-report to measure avoidance coping also is a limitation. Real-time assessment of avoidance using measures such as ecological momentary assessment (Kashdan, Breen, & Julian, 2010) and measuring behavioral avoidance in response to controlled stress inductions (Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007) would offer additional insight into the nature of the PTSD-avoidance coping relation. The current study also was unable to address the possible influence of treatment engagement and adherence as well as secondary gain for treatment nonresponse (e.g., retaining PTSD-related service-connected benefits). Given these factors may influence both self-reported PTSD symptom severity and avoidance coping, as well as the interplay between these factors, future research should examine the possible role that these factors play in links between PTSD and avoidance across the course of PTSD treatment. Finally, the current sample was comprised primarily of men with a history of combat exposure, which constrains generalizability of the results.
These limitations notwithstanding, the current findings represent an important contribution to a growing body of work (1) documenting a reciprocal association between PTSD severity and avoidance coping outside the context of treatment and (2) aiming to better understand such patterns during treatment. Results suggest that individuals with chronic, treatment-resistant, PTSD who are apt to employ avoidance coping strategies upon presenting for inpatient treatment may not benefit to the degree that comparable people who avoid relatively less do, and this outcome may predict maintained avoidance coping. As such, tailoring treatments to the level of avoidance coping at treatment initiation may be warranted. Much more research is needed to fully understand how avoidance and PTSD severity relate across the course of treatment for PTSD varying in chronicity. Nonetheless, treatment researchers are now poised to examine the advantages of increasing the degree to which avoidance is targeted in treatment for people with chronic PTSD who endorse particularly high levels of pre-treatment avoidance.
Research supports a bi-directional relation between PTSD and avoidance coping.
This study examined this relation during and following treatment of chronic PTSD.
Avoidance at intake predicted PTSD symptoms at post-treatment.
PTSD symptoms at post-treatment predicted avoidance at follow-up.
Clinical implications and future research directions are discussed.
Acknowledgments
This work was supported, in part, by the following: A VA Clinical Science Research and Development (CSR&D) Career Development Award – 2 (Bonn-Miller) and a VA HSR&D SUD-QUERI grant (RRP 10-192; Bonn-Miller). Christal L. Badour was supported by a NIMH National Research Service Award (F31 MH092994-01). Daniel M. Blonigen was supported by a Career Development Award – 2 from the VA office of Research and Development (Clinical Sciences Research & Development). The expressed views do not necessarily represent those of the Department of Veterans Affairs. The authors would like to thank Dr. Kent D. Drescher at the National Center for PTSD at the VA Palo Alto Health Care System for collecting and providing access to the data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text revision. [Google Scholar]
- Amir M, Kaplan Z, Efroni R, Levine Y, Kotler M. Coping styles in post- traumatic stress disorder (PTSD) patients. Personality and Individual Differences. 1997;23:399–405. doi: 10.1016/S0191-8869(97)80005-0. [Google Scholar]
- Benotsch EG, Brailey K, Vasterling J, Uddo M, Constans JI, Sutker PB. War zone stress, personal and environmental resources, and PTSD symptoms in Gulf War veterans: A longitudinal perspective. Journal of Abnormal Psychology. 2000;109:205–213. doi: 10.1037/0021-843X.109.2.205. [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS structural equations program manual. Multivariate Software; Encino, CA: 1995. [Google Scholar]
- Bentler PM. Rites, wrongs, and gold in model testing. Structural Equation Modeling. 2000;7:82–91. doi: 10.1207/S15328007SEM0701_04. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris C. Psychometric properties of the PCL-checklist. Behavior Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. DOI:10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Vujanovic AA, Drescher KD. A prospective investigation of changes in avoidant and active coping and posttraumatic stress disorder symptoms among military veterans. Journal of Psychopathology and Behavioral Assessment. in press. doi: 10.007/s10862-012-9293-6. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. doi::10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Eld J. The course of PTSD symptoms following military training accidents and brief psychosocial interventions. Personality and Individual Differences. 2003;35:771–783. doi: 10.1016/S0191-8869(02)00282-9. [Google Scholar]
- Finkel S. Causal analysis with panel data. In: Michael L-B, editor. Quantitative Applications in Social Science. Sage; London: 1995. Series Ed. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. doi: 10.1037/0033-2909.99.1.20. [PubMed] [Google Scholar]
- Gil S. Coping style in predicting posttraumatic stress disorder among Israeli students. Anxiety, Stress and Coping. 2005;18:351–359. doi: 10.1080/10615800500392732. [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, Lejuez CW. A laboratory- based study of the relationship between childhood abuse and experiential avoidance among innercity substance users: The role of emotional nonacceptance. Behavior Therapy. 2007;38:256–268. doi: 10.1016/j.beth.2006.08.006. doi: 10.1016/j.beth.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Gutner CA, Rizvi SL, Monson CM, Resick PA. Changes in coping strategies, relationship to the perpetrator, and posttraumatic distress in female crime victims. Journal of Traumatic Stress. 2006;19:813–823. doi: 10.1002/jts.20158. doi: 10.1002/jts.20158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [Google Scholar]
- Jacobsen PB, Sadler IJ, Booth-Jones M, Soety E, Weitzner MA, Fields KK. Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. Journal of Consulting and Clinical Psychology. 2002;70:235–240. doi: 10.1037//0022-006x.70.1.235. doi: 10/1037/0022-006X.70.1.235. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Breen WE, Julian T. Everyday strivings in war veterans with posttraumatic stress disorder: Suffering from a hyper-focus on avoidance and emotion regulation. Behavior Therapy. 2010;41:350–363. doi: 10.1016/j.beth.2009.09.003. doi: 10.1016/j.beth.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, Zimering RT, Caddell JM. A behavioral formulation of posttraumatic stress disorder in Vietnam veterans. Behavior Therapist. 1985;8:9–12. [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Avoidance coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress. 2008;21:83–90. doi: 10.1002/jts.20288. doi: 10.1002/jts.20288. [DOI] [PubMed] [Google Scholar]
- Leiner AS, Kearns MC, Jackson JL, Astin MC, Rothbaum BO. Avoidant coping and treatment outcome in rape-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0026814. in press. doi: 10.1037/a0026814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litman JA. The COPE inventory: Dimensionality and relationships with approach- and avoidance-motives and positive and negative traits. Personality and Individual Differences. 2006;41:273–284. doi: 10.1016/j.paid.2005.11.032. [Google Scholar]
- Marx BP, Sloan DM. Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behaviour Research and Therapy. 2005;43:569–583. doi: 10.1016/j.brat.2004.04.004. doi: 10.1016/j.brat.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Mulaik SA, Millsap RE. Doing the four-step right. Structural Equation Modeling. 2000;7:36–73. doi: 10.1207/S15328007SEM0701_02. [Google Scholar]
- Muthén BO, Muthén LK. Mplus 5.2. Author; Los Angeles, CA: 1998-2008. [Google Scholar]
- Nezu AM, Carnevale GJ. Interpersonal problem solving and coping reactions of Vietnam veterans with posttraumatic stress disorder. Journal of Abnormal Psychology. 1987;96:155–157. doi: 10.1037//0021-843x.96.2.155. doi: 10.1037/0021-843X.96.2.155. [DOI] [PubMed] [Google Scholar]
- Orsillo S, Batten SV. Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification. 2005;29:95–129. doi: 10.1177/0145445504270876. doi: 10.1177/0145445504270876. [DOI] [PubMed] [Google Scholar]
- Pineles SL, Mostoufi SM, Ready CB, Street AE, Griffin MG, Resick PA. Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of Abnormal Psychology. 2011;120:240–246. doi: 10.1037/a0022123. DOI: 10.1037/a0022123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. doi: 10.1037/002-006X.60.5.748. [DOI] [PubMed] [Google Scholar]
- Roth S, Cohen LJ. Approach avoidance and coping with stress. American Psychologist. 1986;41:813–819. doi: 10.1037//0003-066x.41.7.813. doi: 10.1037/0003-066X.41.7.813. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist--Civilian Version. Journal of Traumatic Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. doi:10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Shapiro F. Eye movement desensitization: A new treatment for post-traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry. 1989;20:211–217. doi: 10.1016/0005-7916(89)90025-6. doi: 10.1016/0005-7916(89)90025-6. [DOI] [PubMed] [Google Scholar]
- Sutker PB, Davis JM, Uddo M, Ditta SR. War zone stress, personal resources, and PTSD in Persian Gulf war returnees. Journal of Abnormal Psychology. 1995;104:444–452. doi: 10.1037//0021-843x.104.3.444. doi: 10.1037/0021-843X.104.3.444. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Rosen C, Cavella S, Moos RH, Finney JW, Yesavage J. Coping symptoms, and functioning outcomes of patients with posttraumatic stress disorder. Journal of Traumatic Stress. 2006;19:799–811. doi: 10.1002/jts.20185. doi:10.1002/jts.20185. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. doi: 10.1007/BF02291170. [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD checklist (PCL): Reliability, validity, and diagnostic utility; Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. October, 1993. [Google Scholar]