Abstract
Many published studies that examined the effect of lead exposure on neurobehavioral performances were conducted in confined manufacturing environment with low to moderate blood lead levels as a marker of exposure. This study was conducted in a general environmental setting with very low exposure intensity and blood lead levels. The objective of the study was to determine the effect of very low blood lead levels (below 10 μg/dl) on the neurobehavioral performances of policemen in Kota Bharu, Kelantan. The study, conducted between August 25th and October 20th 2001, was cross-sectional in design and comprised of 89 policemen working in Kota Bharu district. The lead concentration of venous blood was determined using graphite furnace absorption spectrometer. We assessed neurobehavioral performances using the WHO Neurobehavioral Core Test Battery (NCTB). The mean blood lead concentration was 2.5 + 1.0 mg/dl. Among the seven tests performed, the positive effect of blood lead on Benton visual retention was not significant after controlling for the confounding effect of smoke-dose. This study suggested that very low blood lead levels have no significant effects on the neurobehavioral performances. Therefore, more studies with blood lead levels below the recommended environmental limit of 10 mg/dl, as recommended by Centers for Disease Control (CDC), be conducted in order to justify that limit.
Keywords: blood lead level, lead poisoning, neurobehavioral performances, policemen, environmental health
Introduction
Lead poisoning has been a recognized health hazard for more than 2,000 years. Hippocrates and Nikander noted characteristic features of lead toxicity, including anemia, colic, neuropathy, nephropathy, sterility and coma, in ancient times, as well as by Ramazzini and Hamilton in the modern era(1).
Lead serves no useful biologic function in the body (2). The ideal blood lead level is 0 mg/dl (3). Over the past several years, there was increasing concern over the health effects of low-level lead exposure. In October of 1991, the recommended level for safe limit was lowered from 25 mg/dl to 10 mg/dl (4). This limit is now being challenged, despite it being universally accepted as a safety level (5). An association between blood lead level below 10 mg/dl and cognitive function of middle-age and elderly men has also been reported (6).
Lead poisoning is insidious, because at blood lead concentration under 45 mg/dl, symptoms are not always overt. Thus, neurological damage may unknowingly occur in children and subsequently emerge as lower IQ scores, as learning difficulties or behavioral problems (5). In adults, neurological damage may enhance ageing-related cognitive function loss (7). Children with lower IQ and adults with early cognitive function loss are serious public health burdens as the life expectancy of the world population is increasing. The dependency ratio may increase in the future. Therefore, more evidences are needed to prove that the current safety limit is truly safe or otherwise.
We had the opportunity to examine the possible effects of very low blood lead levels on neurobehavioral performances of a group of policemen in Kota Bharu, Kelantan using WHO Neurobehavioral Core Test Battery (NCTB) (8). The WHO NCTB was chosen as a tool for testing because it has been validated as a standardized neuropsychological test battery, trans-culturally feasible and sensitive enough to detect neurobehavioral impairment (8, 9). We hypothesized that at very low blood lead levels, there would be no significant changes in neurobehavioral performances.
Materials and Methods
Study Design
The study was a cross-sectional design and focused on lead exposure in the general environmental setting. Enrollment of subjects began on 25th August 2001 through to 20th October 2001. The current report focuses on neurobehavioral performances of 89 policemen in Kota Bharu district.
The study was funded by the Universiti Sains Malaysia’s short-term research grant (No. 304/PPSP/6131177). The study protocol was reviewed and approved by the Research and Ethics Committee, School of Medical Sciences, Universiti Sains Malaysia. Participation in the study was voluntary and all participants provided written informed consents.
Sample Size
We estimated the sample size using the single mean formula with 95% confidence interval. We used standard deviation of mean simple reaction time from the Venezuelan study (10). We set the precision at 13%. The calculated sample size was 100.
Recruitment of Study Subjects
The subjects were selected through simple random sampling from a sampling frame consisting of all eligible policemen working in Kota Bharu district. We obtained the initial list comprising of 185 policemen from Kelantan’s Contingent Police Headquarters. We set the inclusion and exclusion criteria as follows: male policemen working in Kota Bharu and available during data collection (25th August – October 20th 2001) would be included. We excluded those having history of head trauma with loss of consciousness, recent exposure (within two weeks) to other neurotoxic agents such as organophosphates or organic solvents, and chronic medical illnesses such as diabetes mellitus, thyrotoxicosis, anxiety, nervous system diseases, or past psychiatric illnesses.
From 185 policemen, 162 (87.6 %) were males and 23 (12.4 %) females. Since we restricted the study to males, 162 were considered eligible to join the study. We randomly selected 100 of them to join the study and 93 % participated.
Data Collection
Data collection was completed at the Police Contingent Headquarters Office in Kota Bharu. Upon registration, we explained the purpose of the study and took written informed consents from the subjects. Then their heights and weights were measured using SECA weighing scale with height, to the nearest weight (0.1 kg) and height (0.5 cm). The self-administered questionnaire, which was validated by Ariza in 2001 (11), and consisting of demography (14 questions), chemical exposure (4 questions), and subjective symptoms (36 questions) were completed. We administered the WHO (NCTB) in standard order beginning with the easiest to the most difficult test as recommended by the WHO NCTB module (8). The order of the tests was as follows: Profile of Mood States (POMS), Simple Reaction Time (SRT), Digit Span, Santa Ana Manual Dexterity, Digit Symbol, Benton Visual Retention and Pursuit Aiming II.
Three ml of venous blood was withdrawn from the antecubital fossa vein of each subject using a 5 ml syringe. Prior to that, the puncture site was cleaned with ready packed alcohol swab soaked with 70% isopropyl alcohol. The blood was immediately put into a 5 ml polypropylene tube containing lithium heparin as anti-coagulant. The blood was mixed by shaking the tube thoroughly to prevent clotting. Subsequently, the blood specimens were packed into a cool box for delivery to the National Poison Center (PRN), USM, Penang on the same day using the Pos Courier express. Blood specimens were received by PRN in the next morning and stored in the refrigerator until the analysis was done.
Laboratory Methods for Blood Lead Analysis
We analyzed blood lead concentration at the PRN using Graphite Furnace Atomic Absorption Spectrometry (GFAAS) for the determination of lead in whole blood. GFAAS analyses were performed with a Perkin-Elmer“ Model 6000, equipped with Zeeman background correction and a transversely heated graphite tube (THGT) providing stabilized temperature program furnace (STPF) conditions, in which nearly isothermal conditions were achieved within the graphite atomizer as a requirement for efficient atomization. The detection limit of GFAAS during the analysis was 0.0081 mg/dl (12).
For calibration purposes, the stock solution (Perkin-Elmer pure multi-element Atomic Spectroscopy Standard) was used. We prepared and run five working standard solutions (0.5, 1.5, 2.0, 3.0 and 5.0 mg/dl). The correlation coefficient for calibration was almost 1 (0.99997) and reslopes were programmed for every 10 samples being run. We verified the analytical accuracy and precision of the test procedure using Whole Blood Standards from Lyphochek as reference material (12).
Each blood sample was run in duplicate with three injections for each duplicate to ensure accuracy. The mean blood lead level of the duplicate was used as the blood lead level for each subject.
Exposure Assessment
Environmental monitoring of lead in air (ambient lead) was obtained to calculate the exposure level. Alam Sekitar Malaysia Bhd. (ASMA), the responsible agency for air quality monitoring in Malaysia, collected and analyzed air samples using two Continuous Air Monitoring Station (CAMS) in Kota Bharu. Throughout the study period, six air samples were obtained and analyzed for lead concentration.
Statistical Analysis
The primary goal of analysis was to examine the correlation and effects of blood lead levels on neurobehavioral performances of policemen using Stata version 7 (13). We set the level of significance at 0.05. After data clearing (from 93 participated, 4 did not complete the WHO NCTB as they have an emergency call from their units while attending the session), 89 subjects were eligible for data analysis.
Means (SD) and percentages were calculated for scaled and categorical data, respectively. Correlation coefficients were computed for smoke-dose, age, education, blood lead level, and each of the seven test scores. Each of the raw test scores of WHO NCTB was regressed onto the blood lead level using simple linear regression.
We then performed multiple linear regressions for each of the WHO NCTB test scores controlling for smoke-dose, age and education.
Results
This study was completed with a high participation rate (93%). Seven subjects did not turned up because of several reasons. One was involved in a road accident, 2 retired before the end of data collection and another 4 were emergency call. The 89 male policemen were predominantly Malays (93.3 %) with mean age of 41 years (Table 1). More than half of them (52%) were chronic smokers. The subjects were likely to be overweight (BMI = 27 kgm−2). The mean blood lead level was 2.5 ± 1.0 mg/dl.
Table 1 :
Sociodemographic characteristics and blood lead level in 89 male policemen in Kota Bharu, Kelantan, 25th August – 20th October 2001
| Variable | Mean | (SD) | No. | (%) |
|---|---|---|---|---|
| Race | ||||
| Malay | 83 | (93.3) | ||
| Other | 6 | (6.7) | ||
| Age (yr) | 41.1 | (5.1) | ||
| Duration of employment (yr) | 16.8 | (4.7) | ||
| Education (yr) | 10.1 | (1.7) | ||
| BMIa (kgm−2) | 27.0 | (7.3) | ||
| Smoker | 47 | (52.8) | ||
| No. of cigarette/day | 18.6 | (3.7) | ||
| Duration of smoking (yr) | 18.3 | (7.7) | ||
| Blood lead (μg/dl) | ||||
| 2.5 | (1.0) |
Body Mass Index = weight (kg) / height2 (m2)
Blood lead and smoke-dose was significantly and positively correlated with Benton visual retention (Pearson’s r = 0.231, p = <0.05 and Pearson’s r = 0.247, p < 0.05, respectively) (Table 2). In simple linear regression, blood lead has a significant positive effect on Benton visual retention (b = 0.25, p = 0.03, CI = 0.021 and 0.47) (Table 3). However, after controlling for smoke-dose, the effect was not significant (b = 0.20, p = 0.10).
Table 2 :
Correlation between smoke-dose, age, education, blood lead level and test scores in 89 male policemen in Kota Bharu, Kelantan, 25th August – 20th October 2001
| Age | Education | Lead | SRTc (mean) | SRT (SD) | Digit-span forward | Digit-span backward | Santad | Santaa | Ten-anxf | hostility | Farigue | depression | vigor | confuse | Digit symbol | Bentong | Aimingh | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Smoke-dosea | rb: 0.105 | r: −0.195 | r: −0.243* | r: −0.001 | r: −0.018 | r: 0.039 | r: 0.148 | r: −0.103 | r: −0.083 | r: −0.006 | r: −0.076 | r: 0.052 | r: −0.018 | r: 0.001 | r: 0.047 | r: −0.230* | r: −0.247* | r: −0.173 |
| Age | r: −0.244** | r: −0.244* | r: 0.028 | r: 0.107 | r: −0.056 | r: −0.073 | r: 0.018 | r: −0.288** | r: −0.147 | r: −0.061 | r: −0.049 | r: −0.002 | r: −0.048 | r: −0.014 | r: −0.100 | r: −0.244* | r: −0.067 | r: −0.219* |
| Education | r: −0.031 | r: −0.151 | r: −0.137 | r: −0.124 | r: −0.102 | r: 0.152 | r: 0.023 | r: 0.070 | r: 0.059 | r: −0.027 | r: 0.043 | r: −0.200 | r: 0.029 | r: 0.185 | r: −0.092 | r: −0.118 | ||
| Lead | r: −0.114 | r: −0.088 | r: −0.068 | r: 0.078 | r: 0.084 | r: 0.078 | r: 0.066 | r: 0.112 | r: 0.053 | r: 0.061 | r: 0.051 | r: 0.008 | r: 0.051 | r: 0.231* | r: −0.176 |
Smoke-dose = number of cigarettes per day x duration of smoking (yr) x 365
Pearson’s correlation Cofficient
Simple Reaction Time
Santa Ana preferred hand
Santa Ana non-preferred hand
Tension-anxiety
Benton Visual Retention
Pursuit Aiming (correct dot) II
P <0.05
P <0.01
Table 3 :
Linear regression analysis of mean blood lead level on neurobehavioral test scores in 89 policemen in Kota Bharu, Kelantan, 25th August – 20th October 2001
| Test | ß | SE | P-value | 95% Confidence Interval | |
|---|---|---|---|---|---|
| POMSa | |||||
| Tension-anxiety | 0.28 | 0.44 | 0.54 | −0.61 | 1.15 |
| Hostility | 0.66 | 0.63 | 0.30 | −0.59 | 1.92 |
| Fatigue | 0.21 | 0.42 | 0.62 | −0.63 | 1.05 |
| Depression | 0.45 | 0.78 | 0.57 | −1.11 | 2.00 |
| Vigor | 0.21 | 0.43 | 0.63 | −0.65 | 1.06 |
| Confusion | 0.03 | 0.41 | 0.94 | −0.77 | 0.83 |
| Psychomotor speed and attention | |||||
| Mean SRTb | −0.00 | 0.00 | 0.29 | −0.01 | 0.00 |
| SD SRT | 0.05 | 0.01 | 0.94 | −1.36 | 2.20 |
| Auditory memory and learning | |||||
| Digit-span forward | −0.12 | 0.19 | 0.53 | −0.48 | 0.24 |
| Digit-span backward | 0.11 | 0.15 | 0.47 | −0.18 | 0.41 |
| Santa Ana Manual dexterity | |||||
| Pegboard, dominant hand | 0.44 | 0.53 | 0.43 | −0.66 | 1.53 |
| Pegboard, non-dominant hand | 0.06 | 0.57 | 0.92 | −1.05 | 1.16 |
| Perceptual motor speed | |||||
| Digit symbol | 0.42 | 0.89 | 0.64 | −1.36 | 2.20 |
| Visual memory | 0.25 | 0.12 | 0.03* | 0.02 | 0.48 |
| Benton visual retention | 0.20 | 0.12 | 0.10Ø | −0.03 | 0.43 |
| Motor steadiness | |||||
| Pursuit aiming (no. correct) | 0.55 | 3.61 | 0.88 | −6.64 | 7.73 |
| Pursuit aiming (total attempted) | 3.09 | 4.10 | 0.46 | −3.08 | 11.25 |
Profile of Mood state
Simple Reaction Time
Controlling for smoke-dose; R2=0.09
P <0.05
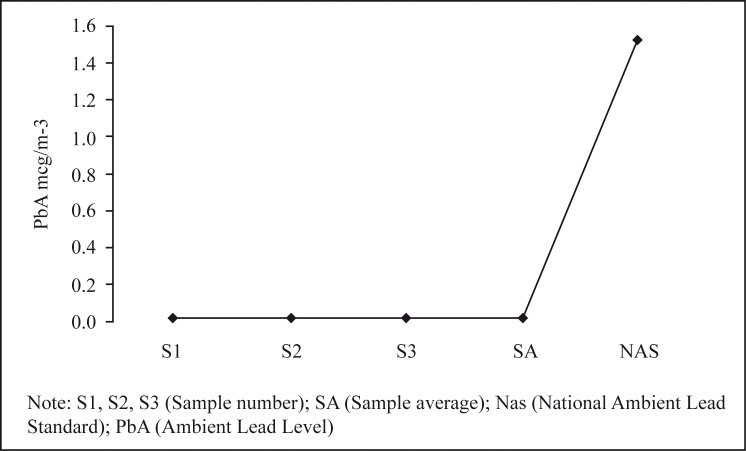
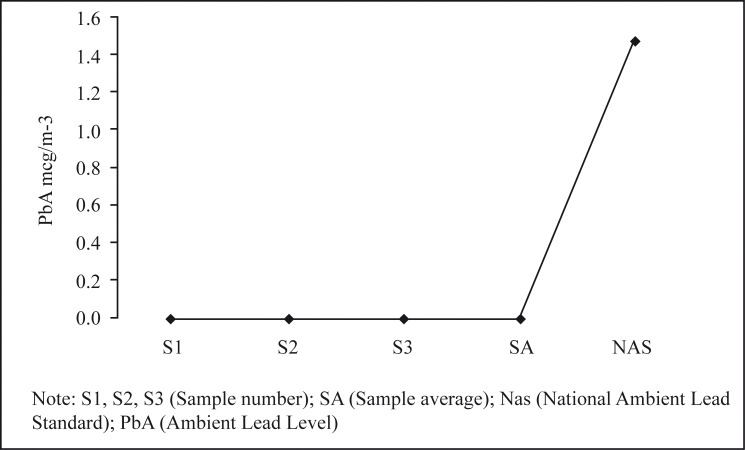
As shown in Figure 1 and 2, the atmospheric lead levels at Maktab Sultan Ismail Kota Bharu and Pengkalan Chepa were far below the National Ambient Lead Standard of 1.5 mg per m3. These two sites represent the residential and industrial area in Kota Bharu, respectively.
Figure 1 :
Comparison of ambient lead levels measured by Continuous Air Monitoring Station at Maktab Sultan Ismail, Kota Bharu, Kelantan and the National Ambient Lead Standard, 25th August – 20th October 2001
Figure 2 :
Comparison of ambient lead levels measured by Continuous Air Monitoring Station at Pengkalan Chepa, Kota Bharu, Kelantan and the National Ambient Lead Standard, 25th August – 20th October 2001
Discussion
Lead has been demonstrated to cause sub-clinical neurotoxicity (14). Since the central nervous system has little capacity for repair, the alteration caused by sub-clinical neurotoxicity can be permanent and irreversible (14). Therefore, recognition of the sub-clinical changes is vital for betterment of primary prevention effort.
We used the WHO NCTB to detect sub-clinical neurobehavioral changes because the neurobehavioral changes were found to be consistently sensitive to the effect of chemicals such as lead (15). Many studies have shown that several cognitive domains were affected by lead exposure (16). These include memory deficit (17–19), poor reaction time (7, 19–21), changes in mood profile (10, 17–19, 22, 23), impaired perceptual motor speed (19, 20), Benton visual retention (10, 20) and eye-hand coordination (18, 19).
However, most of the above studies examined the neurobehavioral performances in confined manufacturing environments with blood lead levels much higher than the safety limit set by CDC (4). Since this safety limit is currently being challenged (5), we conducted the study in a group of policemen working in the general environment with very low environmental lead exposures (below the safety limit) with the aim of further challenging the current safety limit.
Among the seven tests conducted, Benton visual retention was significantly and positively correlated with blood lead. We could not explain this biologically non-plausible contradiction since other studies have shown reverse relationships (10, 20). We also found that smoke-dose was positively correlated with Benton visual retention as well as significantly correlated with blood lead level, thus raising the possibility of a confounding effect. The relationship between blood lead level and Benton visual retention was not significant after controlling for smoke-dose. Our study has failed to detect any mood changes (10, 22, 23) due to very low exposure to lead.
Previous studies using much smaller sample sizes were able to show significant relationship between exposure and neurobehavioral outcomes (10, 20, 22–26). Therefore, the negative finding reported by our study was not due to a low study power but rather due to the subtle effect of very low blood lead levels on neurobehavior that could not be detected by using the WHO NCTB.
This study suggested that at blood lead levels of 2.5 mg per dl and below there were no significant changes in the neurobehavioral performances of policemen. Therefore, more studies, especially electrophysiological studies, be conducted in exposed workers with blood lead levels below 10 mg per dl in order to justify the current safe limits.
Acknowledgments
The authors wish to thank the Department of Community Medicine, Research and Ethics Committee, School of Medical Sciences, Universiti Sains Malaysia, Kota Bharu Kelantan, and the Biomedical and Health Sciences Committee of Universiti Sains Malaysia, for reviewing and approving the study and the USM short term research grant (No. 304 /PPSP/6131177), the National Poison Center, Universiti Sains Malaysia, Penang for analyzing the blood samples, Alam Sekitar Malaysia Sdn. Bhd. for ambient lead sampling and analysis, and the Police Contingent Headquarters, Kota Bharu, Kelantan for participation in the study. We would also like to thank Mr. Kamarudin Hussin, Research Assistant, for secretarial assistance.
References
- 1.Editorial. Lead in the modern workplace. Am J Public Health. 1990;80:907–8. doi: 10.2105/ajph.80.8.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan AH, Khan A, Ghani F, Khurshid M. Low level lead exposure and blood lead levels in children: a cross-sectional survey. Arch Environ Health. 2001;56:501–5. doi: 10.1080/00039890109602898. [DOI] [PubMed] [Google Scholar]
- 3.Elaine W. Health Effect from Human Exposure to Lead. Workshop: Analytical Method for Blood Lead Measurement. National Meeting of the American Association for Clinical Chemistry (AACC) Chicago IL: AACC; 1996. [Google Scholar]
- 4.CDC. Preventing Lead Poisoning in Young Children: A statement by the Centers for Disease Control. Atlanta, Georgia: US Department of Health and Human Services, Public Health Service; 1991. [Google Scholar]
- 5.Gavaghan H. Lead, unsafe at any level. Bull World Health Organ. 2002;80:82. [PMC free article] [PubMed] [Google Scholar]
- 6.Payton M, Riggs K, Spiro A, Weiss T, Hu H. Relations on bone and blood lead levels to cognitive function in the VA normative aging study. Neurotoxicol Teratol. 1998;20:19–27. doi: 10.1016/s0892-0362(97)00075-5. [DOI] [PubMed] [Google Scholar]
- 7.Bleecker M, Lindren K, Ford D. Differential contribution of current and cumulative indices of lead dose to neuropsychological performances by age. Neurology. 1997;48:639–45. doi: 10.1212/wnl.48.3.639. [DOI] [PubMed] [Google Scholar]
- 8.WHO. Operational Guide for the WHO Neurobehavioral Core Test Battery. Geneva: WHO Office of Occupational Health; 1986. [Google Scholar]
- 9.Anger WK, Cassitto MG, Liang Y, Amador R, Hooisma J, Chrislip DW, Mergler D, Keifer M, Hortnagl J, Fournier L, Dudek B, Zsogon E. Comparison of performance from three continents on the WHO-recommended neurobehavioral core test battery. Environ Res. 1993;62:125–47. doi: 10.1006/enrs.1993.1097. [DOI] [PubMed] [Google Scholar]
- 10.Maizlish NA, Parra G, Feo O. Neurobehavioural evaluation of Venezuelan workers exposed to inorganic lead. Occup Environ Med. 1995;52:408–14. doi: 10.1136/oem.52.6.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ariza AR. A Study of Neurobehavioral Effects of Long-Term Exposure to Organophosphates in Male Tobacco-Growing Farmers in Bachok, Kelantan. Master of Community Medicine (USM), unpublished dissertation 2001.
- 12.Yen CC, Chen WK, Hu CC, Wei BL, Chung C, Kuo SC. Lead determination in whole blood by graphite furnace atomic absorption spectrometry. At Spectrosc. 1997;18:64–9. [Google Scholar]
- 13.Stata Corp. Statistical Software: Release 70 College Station. Texas: Stata Corporation; 2001. [Google Scholar]
- 14.Landrigan PJ, Graham DG, Thomas RD. Strategies for the prevention of environmental neurotoxic illness. Environ Res. 1993;61:157–63. doi: 10.1006/enrs.1993.1060. [DOI] [PubMed] [Google Scholar]
- 15.Anger WK, Cassitto MG. WHO NCTB and other neurobehavioural test batteries. Envion Res. 1993;60:84–6. [Google Scholar]
- 16.Balbus –Kornfeld J, Stewart W, Bolla K, Schwartz B. Cumulative exposure to inorganic lead and neurobehavioural test performance in adults: an epidemiological review. Occup Environ Med. 1995;52:2–12. doi: 10.1136/oem.52.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitchell CS, Shear MS, Bolla KI, Schwartz BS. Clinical evaluation of 58 organolead manufacturing workers. Occup Environ Med. 1996;38:372–77. doi: 10.1097/00043764-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Linz DH, Barrett ET, Pflaumer JE, Keith R. Neuropsychologic and postural sway improvement after CA ++-EDTA chelation for mild lead intoxication. J Occup Med. 1992;34:639–41. [PubMed] [Google Scholar]
- 19.Schwartz BS, Bolla KI, Stewart W, Ford DP, Agnew J, Frumkin H. Decrements in neurobehavioral performances associated with mixed exposure to organic and inorganic lead. Am J Epidemiol. 1993;137:1006–21. doi: 10.1093/oxfordjournals.aje.a116757. [DOI] [PubMed] [Google Scholar]
- 20.Hogstedt C, Hane M, Agrell A, Bodin L. Neuropsychological test results and symptoms among workers with well-defined long term exposure to lead. Br J Indust Med. 1983;40:99–105. doi: 10.1136/oem.40.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stollery BT, Broadbent D, Banks HA, Lee W. Short term prospective study of cognitive functioning in lead workers. Br J Indust Med. 1991;48:739–49. doi: 10.1136/oem.48.11.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker E, Feldman R, White R, Harley J, Niles C, Dinse G, Berkey C. Occupational lead neurotoxicity: a behavioral and electrophysiological evaluation, a study design and year one result. Br J Indust Med. 1984;41:352–61. doi: 10.1136/oem.41.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baker EL, Feldman RG, White RA, Harley JP, Niles CA, Dinse GE, Berkey CS. Occupational lead neurotoxicity: a behavioural and electrophysiological evaluation. Br J Indust Med. 1985;42:507–16. doi: 10.1136/oem.41.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yokoyama K, Araki S, Aono H. Reversibility of psychological performance in subclinical lead absorption. Neurotoxicology. 1988;9:405–10. [PubMed] [Google Scholar]
- 25.Pasternak G, Becker CE, Lash A, Bowler R, Estrin D. Cross-sectional study of lead exposed cohort. Clin Toxicol. 1989;27:37–51. doi: 10.3109/15563658909038568. [DOI] [PubMed] [Google Scholar]
- 26.Jeyaratnam J, Boey KW, Ong CN, Chia CB, Phoon WO. Neuropsychological studies among workers exposed to lead. Br J Indust Med. 1986;43:374–80. doi: 10.1136/oem.43.9.626. [DOI] [PMC free article] [PubMed] [Google Scholar]