Abstract
Background
Low-threshold and out-of-hours services play an important role in the emergency care for people with mental illness. In Norway casualty clinic doctors are responsible for a substantial share of acute referrals to psychiatric wards. This study’s aim was to identify patients contacting the casualty clinic for mental illness related problems and study interventions and diagnoses.
Methods
At four Norwegian casualty clinics information on treatment, diagnoses and referral were retrieved from the medical records of patients judged by doctors to present problems related to mental illness including substance misuse. Also, routine information and relation to mental illness were gathered for all consecutive contacts to the casualty clinics.
Results
In the initial contacts to the casualty clinics (n = 28527) a relation to mental illness was reported in 2.5% of contacts, whereas the corresponding proportion in the doctor registered consultations, home-visits and emergency call-outs (n = 9487) was 9.3%. Compared to other contacts, mental illness contacts were relatively more urgent and more frequent during night time. Common interventions were advice from a nurse, laboratory testing, prescriptions and minor surgical treatment. A third of patients in contact with doctors were referred to in-patient treatment, mostly non-psychiatric wards. Many patients were not given diagnoses signalling mental problems. When police was involved, they often presented the patient for examination.
Conclusions
Most mental illness related contacts are managed in Norwegian casualty clinics without referral to in-patient care. The patients benefit from a wide range of interventions, of which psychiatric admission is only one.
Keywords: After-hours care, Mental health services, Emergency medical services, Primary healthcare, Coercion
Background
Low-threshold and out-of-hours services like casualty clinics, emergency rooms and emergency departments play an important role in the emergency care for people with mental illness [1-3]. In Norway casualty clinic doctors are responsible for 38-63% of acute referrals to psychiatric wards [4-6]. As in many other countries [7-10], overcrowding of emergency wards is a problem. In Norway the casualty clinics’ high share of acute referrals has nourished a popularly held belief that inadequate service provision at casualty clinics contribute to the overload of emergency specialist in-patient services and a high use of coercion [5,11,12]. The need of reducing casualty clinic referrals is a recurrent theme in governmental policy documents [11-13], and there is an ongoing debate regarding alternative organisation of emergency psychiatric care [11,12,14-16].
Currently, Norway has a strict two-tiered healthcare system. General practitioners (GPs) serve as gatekeepers for all secondary care, including psychiatric specialist care. No patients can present themselves directly to a hospital. A patient in need of voluntary or involuntary psychiatric care always has to be assessed by a GP for hospital referral. When in need of emergency care during office-hours, patients contact their regular GP’s surgery directly. Out-of-hours (4.00 pm – 8.00 am, weekends and public holidays) patients have to contact casualty clinics organised by the municipality and staffed by GPs. In the initial contact with the casualty clinics, nurses assess the patients’ needs and initiate the appropriate response. Possible responses are advice from a nurse or different types of contact with a GP, i.e. telephone advice, consultation, home-visit or emergency call-out. In situations where an initial assessment by the GP will delay immediate access to specialist life-supporting treatment vital to the patient’s survival, the patient will be transported directly to a somatic hospital. However, there are no direct transports to psychiatric hospitals. Although casualty clinics are intended to be an emergency service, the majority of contacts are of non-urgent nature [17].
Given the popularly held belief of inadequate service provision at Norwegian casualty clinics, the results of a recent study [6] comparing emergency psychiatric admissions from casualty clinic doctors, regular GPs, doctors in medical hospitals, and doctors from other parts of the secondary services in psychiatry, are rather surprising. There were no significant difference in the proportion of emergency admissions that could have been handled in alternative ways and only small differences were found in the characteristics of patients referred from the different agents. Nevertheless, the same study showed that casualty clinic referrals had significantly more use of police assistance and involuntary care than referrals from other agents [6]. Thus a further focus on the casualty clinics is warranted. The findings also suggest that casualty clinics see patients in a rather serious general condition, and that aggressive behaviour is a problem. They thus resonate with international studies reporting worries over own security as a major issue in out-of-hours primary care [18-23], a worry which often has been associated with the care for mentally disturbed patients [19,21,24,25].
Most studies with relevance for out-of-hours care in Norway have studied a patient population already filtered through primary care [4-6]. Little is known about patients retained in primary care. The presentation rate of mental illness at Norwegian casualty clinics seems to be low [26-28], but these estimates of prevalence are somewhat uncertain as diagnoses from the chapter P of the diagnostic system International Classification for Primary Care 2nd edition (ICPC-2) [29] are used as a proxy for mental illness. This approach has unknown validity. Hence we have limited knowledge of the actual prevalence of Norwegian casualty clinic contacts related to mental illness, the filtering process on the way to specialist psychiatric care, and the treatment these patients are given in out-of-hours primary care. The present study used a cohort design to prospectively identify casualty clinic patients with problems related to mental illness including substance misuse. We investigated which care these patients received at the casualty clinics, to which extent they were referred onwards to specialist services and which diagnoses they were given. We also investigated involvement of the police.
Methods
We used a predefined cohort of seven casualty clinics known as the Watchtowers, whose monthly activity reports are used to monitor emergency primary healthcare activities in Norway [30]. The participating casualty clinics are purposely selected to give a representative sample of Norwegian casualty clinics. The Watchtowers manually record information about all successive contacts to the clinic, including age and gender of the patient, time of contact, priority degree given and first action taken [30]. In this study we added information on the further course of patients’ contact with the casualty clinic. Assessment, initiated treatment, diagnoses and onward referrals are documented by the doctors on call in electronic medical records (EMR). A tailor-made computer program retrieved this information anonymously. The Watchtowers differed in which computer software they used for EMR, and the five users of the dominating software were invited to participate in the study. All the invited clinics consented, but one clinic was later excluded due to lack of local IT-support. The excluded casualty clinics were all rural and had a total population of approximately 38000 inhabitants.
The four participating casualty clinics covered a population of approximately 180000 inhabitants. They ranged from a small rural casualty clinic where the GP on call was supported by a nurse during daytime and evenings, to larger city based casualty clinics with other health personnel and up to three GPs on duty around-the-clock.
Earlier studies have shown seasonal variation in casualty clinic contacts related to substance misuse or mental illness, with July as the most aberrant month [26,31]. This study was therefore performed in winter and spring to enhance the representativeness of the sample. In the period from January throughout May 2010 the regular Watchtower recordings were expanded to include whether the attending nurse considered the contact to be related to mental illness or substance misuse problems. These recordings are henceforth referred to as the Watchtower log.
As Norwegian regulations limits the possibility to trace individual patients through the healthcare system, we had to separately identify patients with contacts related to mental illness or substance misuse problems seen by GPs to obtain information on the GPs contact with the patients. Thus a pop-up window was activated whenever the GP closed a patient’s EMR and if a consultation, home visit or emergency call-out had been recorded for that patient the same day. The window contained a question asking whether today’s contact with the patient was related to mental illness or substance misuse. To remove the window and be able to continue to work with other medical records, the GP had to tick off one of the following statements: ‘no’, ‘yes, substance misuse’, ‘yes, mental illness’ or ‘yes, both mental illness and substance misuse’. During the study period the casualty clinics had information posters about the study on display in their waiting room. The posters included information about the patients’ right to refuse participation. In cases where the patient did not want to participate in the study, the GP would tick off that ‘the patient does not want to participate in the study’. All GP generated responses were recorded in an anonymous log which included information of the patient’s age and gender. This log will henceforth be referred to as the GP generated log.
Unfortunately, the tailor-made computer-program producing the pop-up window stopped working in periods with maintenance of the computer servers and in periods with high activity on the system. Several of the casualty clinics shared servers with local hospitals or regular GPs’ surgeries, thus this interference typically happened during daytime. Altogether this resulted in a substantial loss of GP-registered contacts, especially in the largest casualty clinic where an upgrade of the computer system resulted in the loss of all cases over several weeks. All types of contacts were equally affected independent of their relation to mental illness or substance misuse, and thus no selection bias was introduced.
For contacts judged to be related to mental illness or substance misuse an additional log stored identification of the contacts. At the end of the study period a specifically designed computer program retrieved the EMR text related to these contacts. No information that could directly identify the patient was ever retrieved, and all text was completely anonymous. Based on information available in the text, the following was recorded for each contact: age and gender of the patient, interventions at the casualty clinic beyond standard consultation, onwards referrals, diagnoses given, involvement by the police and reports of dangerous situations. All the casualty clinics used ICPC-2 for diagnoses [29]. Results from this part of the study will be referred to as the extracts from the electronic medical records.
The study was approved by the Regional Committee for Medical Research Ethics and the Norwegian Social Science Data Services. The Ministry of Health and Care Services gave permission to use patient information in the study.
All three data sets were analysed descriptively using SPSS 15.0. Means are quoted as mean ± standard deviation. Group differences were tested with Pearson’s chi-squared test or Student’s t test.
Results
The Watchtower log
During the study period 28527 contacts were recorded at the casualty clinics. The attending nurse judged 715 contacts (2.5%) to be related to mental illness or substance misuse. In contacts related to mental illness or substance misuse 52.6% (n = 361) of the patients were men, compared to 46.2% (n = 12804) for other contacts (p = 0.001). The mental illness or substance misuse patients had a mean age of 38.5 ± 15.0 years, whilst the other patients had a mean age of 33.6 ± 26.2 years (p < 0.001).
Table 1 shows initial contacts to the casualty clinics by period of day, priority grade given, type of primary action taken, and by whether the contact reason was related to substance misuse or mental illness. Contacts related to substance misuse or mental illness differed from other contacts by being more urgent and more frequent during night time. The contacts were frequently handled by nurses only and they resulted less frequently in a consultation with a GP.
Table 1.
Initial contacts by substance misuse/mental illness relatedness and by day distribution, urgency and action taken
| |
Substance misuse/mental illness |
Others |
|
||
|---|---|---|---|---|---|
| n | % | n | % | p-value | |
|
Time of day, n = 28527 |
|
|
|
|
<0.001 |
| 08.00-15.29 |
162 |
22.7 |
10381 |
37.3 |
|
| 15.30-22.59 |
313 |
43.8 |
14121 |
50.8 |
|
| 23.00-07.59 |
240 |
33.6 |
3310 |
11.9 |
|
|
Priority grade, n = 28387 |
|
|
|
|
<0.001 |
| Acute |
31 |
4.6 |
802 |
2.9 |
|
| Urgent |
249 |
36.7 |
8523 |
30.8 |
|
| Not urgent |
398 |
58.7 |
18384 |
66.3 |
|
|
Action taken, n = 28417 |
|
|
|
|
<0.001 |
| Contact with nurse |
|
|
|
|
|
| Telephone advice |
209 |
30.8 |
4949 |
17.8 |
|
| Consultation |
13 |
1.9 |
473 |
1.7 |
|
| Contact with GP |
|
|
|
|
|
| Telephone advice |
78 |
11.5 |
2514 |
9.1 |
|
| Consultation |
314 |
46.2 |
17481 |
63.0 |
|
| Home visit |
9 |
1.3 |
235 |
0.8 |
|
| Emergency call-out |
19 |
2.8 |
499 |
1.8 |
|
| Other | 37 | 5.4 | 1587 | 5.7 | |
Initial patient contacts to triaging nurses in the four casualty clinics (n = 28527) by judged relation to substance misuse or mental illness, and by period of day, assessed priority grade, and type of primary action taken. Group differences were tested with Pearson’s chi-squared test.
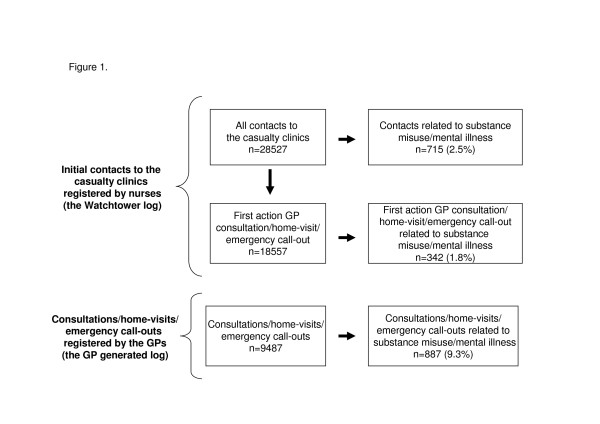
The GP generated log
During the study period 9753 cases were registered in the GP generated log. The GP generated log thus included 52.6% of the initial contacts to the casualty clinic where the nurses had chosen a consultation, home-visit or emergency call-out as first action. In 266 cases (2.7%) the patient refused to participate in the study, thus 9487 cases were available for further analysis. The non-participant group consisted of 48.5% men (n = 129) and the patients had a mean age of 44.7 ± 24.1 years. The non-participating patients did not differ significantly from the participating patients regarding gender (p = 0.628) or age (p = 0.240). For an overview of contacts registered by nurses and GPs available for further analysis, see Figure 1.
Figure 1.
Total number of registered contacts and share with identified relation to substance misuse/mental illness. Share of contacts with identified relation to substance misuse/mental illness in nurse registered initial contacts to the casualty clinics (n = 28527) and GP registered consultations, home-visits and emergency call-outs (n = 9487). GP registered contacts where the patient refused to participate in the study are excluded (n = 266). First action GP consultation/home-visit/emergency call-out are initial contacts where the nurses decided that the patient had to be seen by a GP.
The GPs judged 887 of the eligible contacts (9.3%) to be related to substance misuse or mental illness. The gender distribution differed significantly between the subcategories (p < 0.001), with high proportions of men in subcategories related to substance misuse (Table 2). The patients with contacts related to only substance misuse were younger than the other patients (Table 2). All subgroups related to mental illness or substance misuse had relatively more night time contacts than other types of contacts (p < 0.001) (Table 2).
Table 2.
GP registered contacts by substance misuse/mental illness relatedness, and by gender, age and day period
| |
Total |
Men |
Age |
Time of day |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
|
|
|
|
|
|
08-15.59 |
16-22.59 |
23-07.59 |
|||
| Contact related to | n | % | n | % | mean | SD | n | % | n | % | n | % |
| Substance misuse |
305 |
3.2 |
209 |
68.5 |
34.6 |
15.6 |
56 |
18.4 |
95 |
31.1 |
154 |
50.5 |
| Mental illness |
375 |
3.9 |
147 |
39.2 |
40.0 |
18.3 |
79 |
21.1 |
202 |
53.8 |
94 |
25.1 |
| Substance misuse/mental illness combined |
207 |
2.2 |
123 |
59.4 |
39.1 |
13.6 |
58 |
28.0 |
81 |
39.1 |
68 |
32.9 |
| Other issues |
8600 |
90.7 |
3979 |
46.3 |
43.5 |
22.4 |
2727 |
31.7 |
4680 |
54.4 |
1193 |
13.9 |
| All | 9487 | 100.0 | 4458 | 47.0 | 43.0 | 22.0 | 2920 | 30.8 | 5058 | 53.3 | 1509 | 15.9 |
The GP registered patient contacts in the study period (n = 9487) by whether the contact was related to substance misuse or mental illness, and by share of total, gender and age distribution, and distribution over the day. SD denotes standard deviation.
The extracts from the electronic medical records
Of the 887 contacts where information was retrieved from the EMRs, 20 cases (2.3%) were excluded due to no or uncertain information about the type of contact. Another 14 cases (1.6%) could only be analysed for diagnoses as information was missing on the interventions at the casualty clinic.
The most common interventions at the clinic differed between the subcategories (Table 3). Frequent interventions were laboratory tests, consulting others regarding the case, the administering or prescription of medication, and minor surgical treatment. In general, there were small differences in the interventions described for cases concluded at the casualty clinic compared to cases referred onwards (data not shown).
Table 3.
The most common interventions in GP registered contacts related to substance misuse or mental illness
| |
Total n = 853 |
Substance abuse n = 292 |
Mental illness n = 361 |
Mental illness/ substance abuse n = 200 |
|
||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | n | % | n | % | n | % | n | % | p-value |
| Laboratory tests |
198 |
23.2 |
86 |
29.5 |
78 |
21.6 |
34 |
17.0 |
<0.01 |
| Consulted others regarding treatment |
143 |
16.7 |
32 |
11.0 |
70 |
19.3 |
41 |
20.5 |
<0.01 |
| Given medication |
128 |
15.0 |
35 |
12.0 |
63 |
17.5 |
30 |
15.0 |
0.15 |
| Prescriptions |
113 |
13.2 |
23 |
7.9 |
64 |
17.7 |
26 |
13.0 |
0.001 |
| Minor surgical treatment |
77 |
9.0 |
51 |
17.5 |
15 |
4.2 |
11 |
5.5 |
<0.001 |
| Observation in casualty clinic |
55 |
6.4 |
22 |
7.5 |
17 |
4.7 |
16 |
8.0 |
0.20 |
| Sick leave | 19 | 2.2 | 5 | 1.7 | 11 | 3.0 | 3 | 1.5 | 0.38 |
The most common interventions in GP-contacts related to substance misuse or mental illness at the casualty clinics (n = 853). Only interventions beyond dialogue between the patient and the GP are included. Percentage denotes percentage of all patients in given category. Group differences were tested with Pearson’s chi-squared test.
Half of the patients received all necessary treatment at the casualty clinic (Table 4). Treatment at a specialist level was needed more frequently for patients presenting problems related to substance misuse and mental illness combined compared with patients presenting problems related to only substance misuse or mental illness. A third of patients seen by GPs were referred to in-patient treatment, and many were admitted to other than psychiatric wards. Only one patient was referred to addiction treatment. Of 131 patients admitted to psychiatric services, 50 (38.2%) were admitted involuntarily.
Table 4.
Use of onwards referral in GP registered contacts related to substance misuse or mental illness
| |
Total n = 853 |
Substance abuse n = 292 |
Mental illness n = 361 |
Mental illness/ substance abuse n = 200 |
|
||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | p-value | |
|
No onwards referral |
428 |
50.2 |
154 |
52.7 |
190 |
52.6 |
84 |
42.0 |
0.03 |
|
Onwards referral |
|
|
|
|
|
|
|
|
|
| Out-patient treatment |
121 |
14.0 |
45 |
15.4 |
54 |
15.0 |
22 |
11.0 |
0.33 |
| Somatic services |
49 |
5.7 |
38 |
13.0 |
9 |
2.5 |
2 |
1.0 |
<0.001 |
| Regular GP |
34 |
4.0 |
6 |
2.1 |
20 |
5.5 |
8 |
4.0 |
0.08 |
| Psychiatric services |
31 |
3.6 |
1 |
0.3 |
23 |
6.4 |
7 |
3.5 |
<0.001 |
| Addiction treatment |
1 |
0.1 |
0 |
0.0 |
0 |
0.0 |
1 |
0.5 |
N/A |
| Others |
6 |
0.7 |
0 |
0.0 |
2 |
0.6 |
4 |
2.0 |
N/A |
| In-patient treatment |
290 |
34.0 |
87 |
29.8 |
117 |
32.4 |
86 |
43.0 |
<0.01 |
| Psychiatric wards |
131 |
15.4 |
6 |
2.1 |
78 |
21.6 |
47 |
23.5 |
<0.001 |
| Medical wards |
114 |
13.4 |
53 |
18.2 |
30 |
8.3 |
31 |
15.5 |
0.001 |
| Surgical wards |
31 |
3.6 |
22 |
7.5 |
5 |
1.4 |
4 |
2.0 |
<0.001 |
| Community based wards |
7 |
0.8 |
1 |
0.3 |
3 |
0.8 |
3 |
1.5 |
N/A |
| Other somatic wards |
6 |
0.7 |
4 |
1.4 |
1 |
0.3 |
1 |
0.5 |
N/A |
| Addiction treatment |
1 |
0.1 |
1 |
0.3 |
0 |
0.0 |
0 |
0.0 |
N/A |
| Police custody | 19 | 2.2 | 6 | 2.1 | 4 | 1.1 | 9 | 4.5 | 0.03 |
Onwards referral from the casualty clinics in GP registered contacts related to substance misuse or mental illness (n = 853). The columns add to more than 100% because some patients were referred to several services. Percentage denotes percentage of all patients in given category. Group differences were tested with Pearson’s chi-squared test. N/A marks when Pearson’s chi-squared test was non-applicable due to low expected cell-count.
The police was involved in 148 contacts. In 123 of these (83.1%) the police presented a patient for examination. In the remaining 25 contacts (16.9%) the police was alerted by the casualty clinic staff. The police assisted in 34 admissions to in-hospital treatment, whereof four were to medical and surgical wards, and the remaining 30 were involuntary admissions to psychiatric wards. In 29 of the 30 involuntary psychiatric admissions the patient was presented for examination by the police. Threatening behaviour by patient or relatives was mentioned in 32 of the GP registered contacts related to mental illness or substance misuse. This included one episode where health personnel were physically abused. Police was involved in 17 of the contacts with display of threatening behaviour. In 12 contacts the patient had arrived with the police, and in five contacts the police were alerted by the casualty clinic staff. In eight of the contacts involving threatening behaviour the patient was involuntarily admitted to a psychiatric hospital.
The most commonly used diagnoses varied between the 3 subcategories (Table 5). In addition to reflecting substance abuse, the diagnoses in the substance-misuse-only group were often related to acute injuries like cuts and concussion. Far from all cases had been given diagnoses from the chapter P of ICPC-2. One or more diagnoses from chapter P had been given in 32.1% of cases related to substance misuse only (n = 96), 58.6% of cases related to mental illness only (n = 214) and 70.4% of cases related to both mental illness and substance misuse (n = 143).
Table 5.
The most frequently used diagnoses in GP contacts related to substance misuse or mental illness
|
Substance misuse (n = 299) |
Mental illness (n = 365) |
Mental illness/substance misuse (n = 203) |
||||||
|---|---|---|---|---|---|---|---|---|
| ICPC-code | % | ICPC-code | % | ICPC-code | % | |||
|
P16 |
Acute alcohol abuse |
14.4 |
P76 |
Depressive disorder |
8.8 |
A84 |
Poisoning by medical agent |
11.8 |
|
S18 |
Laceration or cut |
12.0 |
P74 |
Anxiety disorder/anxiety state |
7.7 |
P19 |
Drug abuse |
9.4 |
|
P19 |
Drug abuse |
10.0 |
P99 |
Other psychological disorders |
7.1 |
P99 |
Other psychological disorders |
8.4 |
|
N79 |
Concussion |
5.7 |
P27 |
Fear of mental disorder |
5.5 |
P15 |
Chronic alcohol abuse |
7.9 |
|
A99 |
Unspecified general disease |
5.4 |
P77 |
Suicide or suicide attempt |
5.5 |
P76 |
Depressive disorder |
7.9 |
|
D01 |
Abdominal pain |
4.3 |
A84 |
Poisoning by medical agent |
4.7 |
P16 |
Acute alcohol abuse |
6.4 |
|
N80 |
Head injury other |
4.0 |
P02 |
Acute stress reaction |
4.4 |
P74 |
Anxiety disorder/anxiety state |
6.4 |
|
P15 |
Chronic alcohol abuse |
3.7 |
P73 |
Affective psychosis |
4.4 |
P98 |
Psychosis unspecified |
5.9 |
|
A11 |
Chest pain |
2.3 |
P98 |
Psychosis unspecified |
4.4 |
P77 |
Suicide or suicide attempt |
4.9 |
|
L76 |
Sprain/strain of joint |
2.3 |
P72 |
Schizophrenia |
3.8 |
P02 |
Acute stress reaction |
4.4 |
|
L18 |
Musculoskeletal injury |
2.3 |
A11 |
Chest pain |
3.6 |
P29 |
Unspecified psychological symptom |
3.4 |
| All other diagnoses | 61.2 | All other diagnoses | 66.0 | All other diagnoses | 57.6 | |||
The 11 most commonly used ICPC-2 diagnoses at the casualty clinics for patients presenting problems judged by GPs to be related to mental illness or substance misuse. The columns add to more than 100% because patients were given up to four diagnoses.
Comparison of the casualty clinics
Table 6 shows main characteristics of the individual casualty clinics and sums up key results for each individual casualty clinic. There were marked differences between the casualty clinics in judged urgency level of the initial contacts and number of GP contacts related to mental illness. Other parameters were rather similar, for example share of GP contacts related to substance misuse and share of GP contacts resulting in a referral to in-patient treatment.
Table 6.
Descriptive background information and key results by casualty clinic (A-D)
| A | B | C | D | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Descriptive information |
|
|
|
|
|
|
|
|||||
| Number of municipalities participating in the casualty clinic |
1 |
10 |
1 |
1 |
|
|
|
|||||
| Number of inhabitants 01.01.10 |
18680 |
88997 |
8360 |
67305 |
|
|
|
|||||
| Description of community |
Mostly rural |
Urban and rural |
Rural |
Urban |
|
|
|
|||||
| |
|
|
|
|
|
|
|
|
Total |
|
|
|
|
Key results |
n |
% |
n |
% |
n |
% |
n |
% |
n |
% |
p-value |
|
|
Nurse registered initial contacts |
|
|
|
|
|
|
|
|
|
|
|
|
| Total number of contacts |
5493 |
|
10818 |
|
2456 |
|
9760 |
|
28527 |
|
|
|
| Contacts related to substance misuse or mental illness |
139 |
2.5 |
198 |
1.8 |
32 |
1.3 |
346 |
3.5 |
715 |
2.5 |
<0.001 |
|
| Judged acute or urgent |
43 |
32.3 |
101 |
53.7 |
12 |
38.7 |
124 |
38.0 |
280 |
41.3 |
<0.001 |
|
| Handled by nurse |
38 |
28.6 |
42 |
22.5 |
5 |
16.1 |
137 |
41.8 |
222 |
32.7 |
<0.001 |
|
| Home-visits/emergency call-outs |
7 |
5.3 |
8 |
4.3 |
5 |
16.1 |
8 |
2.4 |
28 |
4.1 |
<0.01 |
|
|
GP registered contacts |
|
|
|
|
|
|
|
|
|
|
|
|
| Total number of contacts |
1486 |
|
3123 |
|
806 |
|
4072 |
|
9487 |
|
|
|
| Contacts related to substance misuse |
40 |
2.7 |
123 |
3.9 |
23 |
2.9 |
119 |
2.9 |
305 |
3.2 |
0.05 |
|
| Contacts related to mental illness |
73 |
4.9 |
138 |
4.4 |
15 |
1.9 |
149 |
3.7 |
375 |
4.0 |
0.001 |
|
| Contacts related to substance use and mental illness combined |
49 |
3.3 |
67 |
2.1 |
12 |
1.5 |
79 |
1.9 |
207 |
2.2 |
<0.01 |
|
|
Extracts from medical records |
|
|
|
|
|
|
|
|
|
|
|
|
| Total number of extracts |
158 |
|
314 |
|
44 |
|
337 |
|
853 |
|
|
|
| Total referrals to in-patient treatment |
46 |
29.1 |
108 |
34.4 |
14 |
31.8 |
122 |
36.2 |
290 |
34.0 |
0.47 |
|
| Admissions to psychiatric ward |
16 |
10.1 |
52 |
16.6 |
3 |
6.8 |
60 |
17.8 |
131 |
15.4 |
0.05 |
|
| Involuntary admissions | 2 | 1.3 | 19 | 6.1 | 2 | 4.5 | 30 | 8.9 | 53 | 6.2 | 0.01 | |
Percent denotes percentage of relevant contacts. Group differences were tested with Pearson’s chi-squared test.
Discussion
In this study the GPs judged 9.3% of their patient contacts to be related to mental illness or substance misuse, and most contacts were handled without referral to in-patient care. A wide range of interventions took place at the casualty clinics and a substantial share of patients received counselling by nurse only. When involved, the police often presented a patient for examination. Less than 70% of relevant patients were given diagnoses reflecting mental illness or substance misuse.
Nearly 40% of initial contacts to the casualty clinics were handled by nurses, and three quarters of GP face-to-face contacts were handled by GPs without in-patient referrals. Thus more than 80% of all casualty clinic contacts were handled within the casualty clinic system by use of ambulatory care. The low rate of referrals to inpatient care was consistent across individual casualty clinics, and occurred despite the higher judged urgency of mental illness or substance misuse contacts compared to other types of contacts. The wide range of interventions reported and specialist referrals used suggest that meeting a generalist in the initial contact with the healthcare system could benefit the patients. Even in the patient group with contacts related to only psychiatry a significant number of patients received or were referred to non-psychiatric treatment. Studies of GPs’ participation in out-of-hours emergency healthcare have observed a switch from hospitalisation to ambulatory care [32-36], and there are indications that when presented with the same emergency cases, specialists tend to admit more patients than generalists do [37-39]. The use of GPs as gatekeepers might optimise the use of available specialist resources both in terms of the general filtering to specialist care and filtering into specific sub-groups of specialist care. However, other study designs are needed to judge the appropriateness of current treatment and referrals at casualty clinics.
Earlier findings of three times more police assistance in emergency psychiatric referrals from casualty clinics compared to referrals from other agents have raised issues about how casualty clinics handle these patients [6]. In this study police involvement was mentioned in 148 out of 853 contacts (17.4%), and when involved, the police frequently presented the patient for examination. These findings probably suggest that the situations are rather accentuated before the patients arrive at the casualty clinic. Higher relative rates of more serious diagnoses at casualty clinics compared to at regular GP’s surgeries [31], combined with high estimated urgency and use of emergency call-outs, further strengthen this impression. If the casualty clinics’ involvement in emergency psychiatric admissions really is a problem, then the most efficient initiatives to reduce their involvement might be to prevent crises from escalating by improving early crisis detection and prevention [40]. Consequently, alternative care provision when the crisis has already escalated, for example crisis resolution teams, will have limited effect on emergency admissions [41,42], although they undoubtedly contribute to better healthcare services for patients not necessarily in need of an emergency admission.
In this study we wanted to mirror the clinical experience of casualty clinic staff, thus the selection of the cohort relied on subjective assessment by nurses and GPs. There was a marked discrepancy of the GP- and nurse-reported shares of contacts related to mental illness. This might partly be due to an awareness effect as the GPs were actively asked about this relation for each contact by a pop-up window, whilst the nurses ticked off a box among others in a standard registration form. The discrepancy might also reflect the limited information available to nurses in the initial assessment of patients compared to the information GPs possess after a face-to-face patient encounter. Less than 70% of patient contacts marked by GPs as related to mental illness or substance misuse were given diagnoses from the chapter P of ICPC-2. Limited validity of routinely set diagnostic codes has previously been reported [43,44], and our findings suggest that the prevalence of mental illness related contacts out-of-hours are underestimated in former Norwegian reports. Our study also identified a substance misuse related group of patients mainly presenting with injuries or intoxications. These patients were rarely given diagnoses from the chapter P of ICPC-2 and would therefore have been missed in earlier studies [26,27,31]. Our findings thus further highlight the need for contextual sensitivity and interpretative caution when studying prevalence by use of routinely set diagnostic codes.
Conclusions
This study shows that substantial triage takes place at the casualty clinics, and that four out of five patients contacting the casualty clinic for mental illness or substance misuse related problems are helped by the casualty clinic staff without further referral to in-patient treatment. Many of the patients needed other than psychiatric specialist care. It is therefore likely that patients in their initial emergency contact benefit from the generalists’ broad range of qualifications, and that thepresence of GP-based casualty clinics may reduce the overload of emergency psychiatric wards, rather than induce it.
Abbreviations
GP: General practitioner; EMR: Electronic medical record.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
IHJ conceived of the study. She collected, analysed and interpreted the data, and she drafted and revised the manuscript. TM helped interpret the data and revised the manuscript critically for important intellectual content. SH contributed to the design of the study and revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Contributor Information
Ingrid H Johansen, Email: ingrid.johansen@uni.no.
Tone Morken, Email: tone.morken@uni.no.
Steinar Hunskaar, Email: steinar.hunskar@isf.uib.no.
Acknowledgements
The authors would like to thank all the participating patients, casualty clinic doctors and nurses.
References
- Larkin GL, Beautrais AL, Spirito A, Kirrane BM, Lippmann MJ, Milzman DP. Mental health and emergency medicine: a research agenda. Acad Emerg Med. 2009;16:1110–1119. doi: 10.1111/j.1553-2712.2009.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazlett SB, McCarthy ML, Londner MS, Onyike CU. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004;11:193–195. [PubMed] [Google Scholar]
- Biancosino B, Vanni A, Marmai L, Zotos S, Peron L, Marangoni C, Magri V, Grassi L. Factors related to admission of psychiatric patients to medical wards from the general hospital emergency department: a 3-year study of urgent psychiatric consultations. Int J Psychiatry Med. 2009;39:133–146. doi: 10.2190/PM.39.2.b. [DOI] [PubMed] [Google Scholar]
- Ruud T, Gråwe RW, Hatling T. Akuttpsykiatrisk behandling i Norge - resultater fra en multisenterstudie. [Emergency psychiatric treatment in Norway – Results form a multi center study.] Report No.: A310/2006. Supported by the Norwegian Directorate of Health. Oslo: SINTEF, 2006. Norwegian.
- Tørrissen T. Tvangsinnleggelser i en akuttpsykiatrisk post. [Involuntary admissions to an acute psychiatric ward.] Tidsskr Nor Laegeforen. 2007;127:2086–2089. Norwegian. English. [PubMed] [Google Scholar]
- Johansen IH, Mellesdal L, Jørgensen HA, Hunskaar S. Admissions to a Norwegian emergency psychiatric ward. A prospective study of patient characteristics and referring agents. Nord J Psychiatry. 2012;66:40–48. doi: 10.3109/08039488.2011.598554. [DOI] [PubMed] [Google Scholar]
- Munk-Jorgensen P. Has deinstitutionalization gone too far? Eur Arch Psychiatry Clin Neurosci. 1999;249:136–143. doi: 10.1007/s004060050078. [DOI] [PubMed] [Google Scholar]
- Jayaprakash N, O'Sullivan R, Bey T, Ahmed SS, Lotfipour S. Crowding and delivery of healthcare in emergency departments: the European perspective. West J Emerg Med. 2009;10:233–239. [PMC free article] [PubMed] [Google Scholar]
- Nishi D, Matsuoka Y, Kawase E, Nakajima S, Kim Y. Mental health service requirements in a Japanese medical centre emergency department. Emerg Med J. 2006;23:468–469. doi: 10.1136/emj.2005.029769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Croudace TJ, Singh S, Harrison G. The Nottingham Acute Bed Study: alternatives to acute psychiatric care. Br J Psychiatry. 1997;170:247–252. doi: 10.1192/bjp.170.3.247. [DOI] [PubMed] [Google Scholar]
- Official Norwegian Report 2011:9. Økt selvbestemmelse og rettssikkerhet. Balansegangen mellom selvbestemmelsesrett og omsorgsansvar i psykisk helsevern. [Increased autonomy and legal protection. The balance between autonomy and care responsibility within mental health care] Ministry of Health and Care Services, Oslo; 2011. Norwegian. [Google Scholar]
- Norwegian Directorate of Health. Allmennlegetjenesten og psykisk helse. [General Practice and Mental Health.] Report No.: 04/2009. Oslo: Norwegian Directorate of Health, 2009. Norwegian.
- Proposal No. 63 to the Government (1997–98) Om opptrappingsplan for psykisk helse 1999–2006. Endringer i statsbudsjettet for 1998. [The escalation plan for mental health 1999–2006. Changes in the governmental budget for 1998] Ministry of Health and Care Services, Oslo; 1998. Norwegian. [Google Scholar]
- Hasselberg N, Grawe RW, Johnson S, Ruud T. An implementation study of the crisis resolution team model in Norway: are the crisis resolution teams fulfilling their role? BMC Health Serv Res. 2011;11:96. doi: 10.1186/1472-6963-11-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grawe RW, Ruud T, Bjorngaard JH. Alternative akuttilbud i psykisk helsevern for voksne. [Alternative emergency interventions in adult mental health care] Tidsskr Nor Laegeforen. 2005;125:3265–3268. Norwegian. English summary. [PubMed] [Google Scholar]
- The Norwegian Council for Mental Health. Frivillighet før tvang. Tiltak for å redusere omfang av tvangsinnleggelser til psykisk helsevern. [Voluntariness before coercion. Initiatives to reduce the number of involuntary admissions to mental health care] The Norwegian Council for Mental Health, Oslo; 2010. Norwegian. [Google Scholar]
- Hansen EH, Zakariassen E, Hunskaar S. Sentinel monitoring of activity of out-of-hours services in Norway in 2007: an observational study. BMC Health Serv Res. 2009;9:123. doi: 10.1186/1472-6963-9-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen IH, Carlsen B, Hunskaar S. Psychiatry out-of-hours: a focus group study of GPs' experiences in Norwegian casualty clinics. BMC Health Serv Res. 2011;11:132. doi: 10.1186/1472-6963-11-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolhurst H, Baker L, Murray G, Bell P, Sutton A, Dean S. Rural general practitioner experience of work-related violence in australia. Aust J Rural Health. 2003;11:231–236. [PubMed] [Google Scholar]
- Tolhurst H, Talbot J, Baker L, Bell P, Murray G, Sutton A, Dean S, Treloar C, Harris G. Rural general practitioner apprehension about work related violence in australia. Aust J Rural Health. 2003;11:237–241. [PubMed] [Google Scholar]
- Magin P, Adams J, Joy E, Ireland M, Heaney S, Darab S. General practitioners' assessment of risk of violence in their practice: results from a qualitative study. J Eval Clin Pract. 2008;14:385–390. doi: 10.1111/j.1365-2753.2007.00874.x. [DOI] [PubMed] [Google Scholar]
- Myerson S. Violence to general practitioners and fear of violence. Fam Pract. 1991;8:145–147. doi: 10.1093/fampra/8.2.145. [DOI] [PubMed] [Google Scholar]
- Hobbs FD. Violence in general practice: a survey of general practitioners' views. BMJ. 1991;302:329–332. doi: 10.1136/bmj.302.6772.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magin P, Adams J, Joy E, Ireland M, Heaney S, Darab S. Violence in general practice: perceptions of cause and implications for safety. Can Fam Physician. 2008;54:1278–1284. [PMC free article] [PubMed] [Google Scholar]
- Joa TS, Morken T. Violence towards personnel in out-of-hours primary care: a cross-sectional study. Scand J Prim Health Care. 2012;30:55–60. doi: 10.3109/02813432.2012.651570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen IH, Morken T, Hunskaar S. Contacts related to psychiatry and substance abuse in Norwegian casualty clinics. A cross-sectional study. Scand J Prim Health Care. 2009;27:180–185. doi: 10.1080/02813430903075473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nossen JP. Hva foregår på legekontorene? Konsultasjonsstatistikk for 2006. [What happens at the GPs’ surgeries? Consultation statistics for 2006.] Report No.: 4/2007. Oslo: The Norwegian Labour and Welfare Administration; 2007. Norwegian.
- Sandvik H, Hunskaar S. Årsstatistikk fra legevakt 2007. [Annual statistics from casualty clinics 2007] Report No.: 5/2009. Bergen: The National Centre for Emergency Primary Health Care, 2009. Norwegian.
- ICPC. http://www.kith.no/templates/kith_WebPage____1186.aspx
- Hansen EH, Hunskaar S. Development, implementation, and pilot study of a sentinel network ("The Watchtowers") for monitoring emergency primary health care activity in Norway. BMC Health Serv Res. 2008;8:62. doi: 10.1186/1472-6963-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen IH, Morken T, Hunskaar S. Contacts related to mental illness and substance abuse in primary health care. A cross-sectional study comparing patients' use of daytime versus out-of-hours primary care in Norway. Scand J Prim Health Care. 2010;28:160–165. doi: 10.3109/02813432.2010.493310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichler K, Imhof D, Moshinsky CC, Zoller M, Senn O, Rosemann T, Huber CA. The provision of out-of-hours care and associated costs in an urban area of Switzerland: a cost description study. BMC Fam Pract. 2010;11:99. doi: 10.1186/1471-2296-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakariassen E, Hunskaar S. Involvement in emergency situations by primary care doctors on-call in Norway - a prospective population-based observational study. BMC Emerg Med. 2010;10:5. doi: 10.1186/1471-227X-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Uden CJ, Winkens RA, Wesseling G, Fiolet HF, van Schayck OC, Crebolder HF. The impact of a primary care physician cooperative on the caseload of an emergency department: the Maastricht integrated out-of-hours service. J Gen Intern Med. 2005;20:612–617. doi: 10.1111/j.1525-1497.2005.0091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibowitz R, Day S, Dunt D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam Pract. 2003;20:311–317. doi: 10.1093/fampra/cmg313. [DOI] [PubMed] [Google Scholar]
- Kool RB, Homberg DJ, Kamphuis HC. Towards integration of general practitioner posts and accident and emergency departments: a case study of two integrated emergency posts in the Netherlands. BMC Health Serv Res. 2008;8:225. doi: 10.1186/1472-6963-8-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coast J, Inglis A, Frankel S. Alternatives to hospital care: what are they and who should decide? BMJ. 1996;312:162–166. doi: 10.1136/bmj.312.7024.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCulloch P, Bowyer J, Fitzsimmons T, Johnson M, Lowe D, Ward R. Emergency admission of patients to general surgical beds: attitudes of general practitioners, surgical trainees, and consultants in Liverpool, UK. J Epidemiol Community Health. 1997;51:315–319. doi: 10.1136/jech.51.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong D, Bird J, Fry J, Armstrong P. Perceptions of psychological problems in general practice: a comparison of general practitioners and psychiatrists. Fam Pract. 1992;9:173–176. doi: 10.1093/fampra/9.2.173. [DOI] [PubMed] [Google Scholar]
- Wierdsma AI, Poodt HD, Mulder CL. Effects of community-care networks on psychiatric emergency contacts, hospitalisation and involuntary admission. J Epidemiol Community Health. 2007;61:613–618. doi: 10.1136/jech.2005.044974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolbjornsrud OB, Larsen F, Elbert G, Ruud T. Kan psykiatriske akutteam redusere bruk av akuttplasser ved sykehus? [Can psychiatric acute teams reduce acute admissions to psychiatric wards?] Tidsskr Nor Laegeforen. 2009;129:1991–1994. doi: 10.4045/tidsskr.09.32187. [DOI] [PubMed] [Google Scholar]
- Jacobs R, Barrenho E. Impact of crisis resolution and home treatment teams on psychiatric admissions in England. Br J Psychiatry. 2011;199:71–76. doi: 10.1192/bjp.bp.110.079830. [DOI] [PubMed] [Google Scholar]
- Hjerpe P, Merlo J, Ohlsson H, Bengtsson Bostrom K, Lindblad U. Validity of registration of ICD codes and prescriptions in a research database in Swedish primary care: a cross-sectional study in Skaraborg primary care database. BMC Med Inform Decis Mak. 2010;10:23. doi: 10.1186/1472-6947-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq E, Van Casteren V, Jonckheer P, Burggraeve P, Lafontaine MF. Electronic Patient Record data as proxy of GPs' thoughts. Stud Health Technol Inform. 2008;141:103–110. [PubMed] [Google Scholar]