Abstract
Background
Despite high rates of post-cardiac surgery depression, studies of depression treatment in this population have been limited.
Objective
To evaluate early cognitive behavioral therapy (CBT) in a home environment in patients recovering from cardiac surgery.
Methods
From July 2006 through October 2009, we conducted a randomized controlled trial and enrolled 808 patients who were screened for depressive symptoms using the Beck Depression Inventory (BDI) in the hospital and one month later. Patients were interviewed using the Structured Clinical Interview for DSM-IV (SCID-I); those who met criteria for clinical depression (n=81) were randomized to CBT (n=45) or usual care (UC; n=36). After completion of the UC period, 25 individuals were offered later CBT (UC+CBT).
Results
Main outcomes (depressive symptoms [BDI] and clinical depression [SCID-I]) were evaluated after 8 weeks using intention-to-treat principles and linear mixed models. In the CBT group compared to the UC group, there was greater decline in BDI scores (β=1.41 [95% CI 0.81–2.02], p = <.001) and greater remission of clinical depression (29 [64%] vs. 9 [25%], number need to treat, 2.5 [95% CI, 1.7–4.9], p < .001). Compared to the early CBT group, (median time from surgery to CBT = 45.5 days) the later UC+CBT group (median time from surgery to CBT = 122 days) also experienced a reduction in BDI scores, but the group x time effect was smaller (β=0.79 [95% CI 0.101.47], p = .03) and remission rates between the two groups did not differ.
Conclusions
Early home CBT is effective in depressed post-cardiac surgery patients. Early treatment is associated with greater symptom reduction than similar therapy given later after surgery.
Introduction
Depression occurs in 15 to 40% of patients who undergo cardiac surgery.1–7 After cardiac surgery, depression is a major cause of mortality; its effects are long-lasting, with deaths increased for up to ten years after surgery.8 In addition to mortality, postoperative depression has been shown to adversely affect surgical recovery and is associated with increased cardiac morbidity and decreased functional status.9
Despite the known deleterious effects of depression in this population, studies designed to treat depression early after cardiac surgery have been limited. Two studies of depression treatment after cardiac surgery have been reported.10,11 Only one study has evaluated the effectiveness of cognitive behavioral therapy (CBT) in this population.10 Further, novel home-based approaches to delivery of CBT for cardiac patients have not been tested systematically, with only a single pilot study of home CBT for heart failure patients reporting non-significant improvements in depressive symptoms when CBT was combined with an exercise component.12 Home-based therapy may be particularly advantageous for postoperative patients, whose recovery may limit their ability to attend traditional site-based programs. The purpose of this study was to evaluate the efficacy of CBT in a home environment among patients recovering from cardiac surgery. The primary aims of the study were 1) to test the effect of a short, eight-week course of early home CBT compared to usual care (UC) on remission of clinical depression and depressive symptom severity and 2) to test early home CBT compared to later home CBT on the same outcomes.
Methods
Sample and Setting
From July 2006 through October 2009, we screened 3,422 patients who underwent cardiac surgery (coronary artery bypass grafting or valve replacement/repair) from five tertiary care hospitals in Los Angeles, CA. Institutional Review Board (IRB) approvals were obtained from all participating sites. A two-step screening protocol was used. First, patients were excluded if they met any of the following criteria : age < 30 years, residing outside of the greater Los Angeles area, presence of cognitive impairment (Mini Mental State Exam [MMSE] < 24) or major comorbid psychiatric condition (schizophrenia, bipolar disorder, substance abuse), and autoimmune disorder or malignancy.
A second screening evaluation occurred within a month after hospital discharge. A trained research nurse called patients at home to reassess depressive symptoms. This time frame was selected because depressive symptoms at this time are more likely to be consistent with clinical depression, rather than a reactive depressive disorder or somatic symptoms related to surgery.13 Patients with BDI scores >10 at either baseline or one month post-discharge or those with a history of depression met the second screening eligibility criteria and were interviewed at home using the Structured Clinical Interview for DSM-IV (SCID-I).14
Inclusion criterion was a diagnosis of major or minor depression on the SCID-I. Major depression was defined as: 1) presenting five or more symptoms (depressed mood, anhedonia, weight change, insomnia/hypersomnia, psychomotor retardation/agitation, fatigue, worthlessness/guilt, indecisiveness, thoughts of death/suicidal ideation), 2) including either depressed mood or anhedonia, 3)symptoms occurring nearly every day in a two-week period, and 3) symptoms significant enough to interfere with daily activities.. Minor depression was defined as meeting the same criteria, but presenting at least two of the above symptoms.
Procedures
Of the 3,422 patients, 1,881 (55%) met initial screening eligibility criteria, and 808 (43%) consented to participate (Figure 1). Patients were approached after surgery and before hospital discharge. After consent, a brief in-hospital screening interview was conducted to assess cognitive function. Individuals with a score of ≥ 24 on the MMSE15 completed a brief questionnaire booklet to obtain baseline measures of sociodemographic (marital and work status) and psychobehavioral characteristics (depressive and anxiety symptoms). Medical records were reviewed to obtain demographic data and to identify co-morbidities (Charlson Comorbidity Index16), pre-existing psychiatric conditions, and current medications. Patients with preoperative depression and those on antidepressants were included in the study.
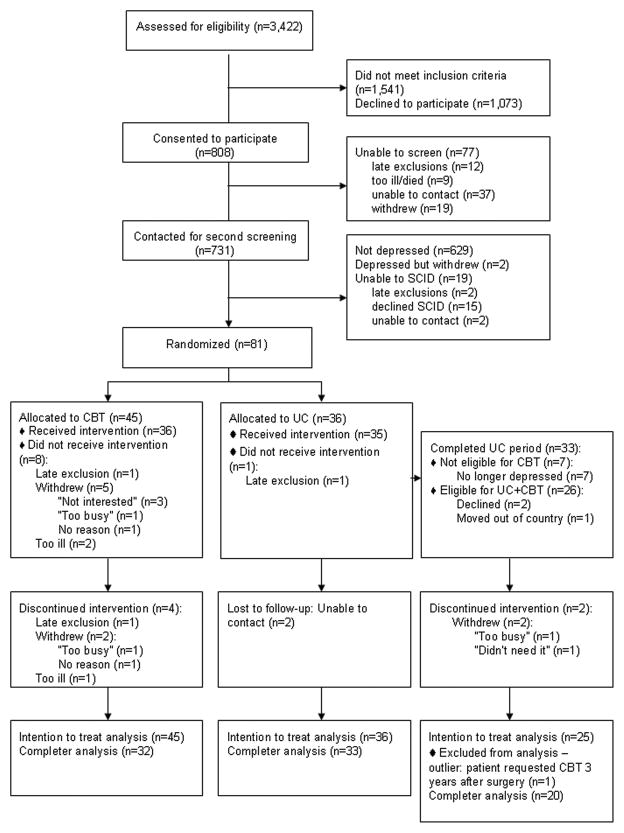
Figure 1.
Flowchart of study participants
Of the 808 patients who consented to participate, 731 (90%) were contacted for the second screening. Nineteen subjects were not interviewed because they declined the interview (15), were unable to be reached (2), or were excluded (2). Eighty-three patients (11.4%) met inclusion criteria for major or minor depression. Diagnoses were confirmed at consensus meetings which included a psychiatrist (M.R.I.) and psychologist. Two patients dropped out before randomization (one withdrew and one moved out of the area), and the remaining patients (n=81) were randomized to the UC Group (n=36) or the CBT group (n=45) using randomization tables for each hospital created by our statistician. After randomization, one participant in each group was excluded when previously unidentified psychiatric conditions (i.e. bipolar disorder) became evident. In addition, in the CBT group five participants withdrew before starting therapy and two withdrew without completing therapy. Among UC participants, after eight weeks, ten did not participate in later therapy because they were no longer depressed (7), moved away (1), or declined therapy (2). Of the 23 who continued in the study, two withdrew without completing therapy.
The UC group received referrals to their primary care providers, along with biweekly follow-up phone calls from study staff for eight weeks (a total of four calls). Phones calls were short (< 15 minutes) and aimed primarily at maintaining ongoing contact. They followed a semi-scripted outline, in which research staff told participants that they were “checking in with them” and reminded them about their enrollment in the study, but did not assess depressive symptoms. Twenty-six participants of the UC group who remained depressed after the 8-week UC condition were offered CBT and comprised the later CBT (UC+CBT) group. One participant was excluded from the analysis because he requested therapy three years after his surgery (outlier). In the early CBT and UC groups, median time from surgery to CBT or UC was 45.5 days (interquartile range = 26.25 days). In the UC+CBT group, median time from surgery to CBT was 122.0.days (interquartile range = 29.0 days).
Intervention
CBT was conducted by four advanced practice nurses, all of whom had expertise in cardiac and/or psychiatric care and completed standardized CBT training (Beck Institute, Philadelphia, PA). Patients participated in an eight week course of therapy, which was selected based on our pilot work, in which all patients had achieved symptom remission after eight weeks.17 The average length of sessions was 50 to 60 minutes; all sessions were face-to-face and occurred at the patient’s home or a location of his/her choosing. All sessions were conducted 1:1 without family members present. Every effort was made to schedule weekly sessions consecutively, unless the participant requested a change. To insure fidelity and consistency of the intervention, therapy nurses used a weekly manual, which included agenda templates and commonly used analysis forms.18 Agenda setting was conducted collaboratively by the nurse and patient at the beginning of each session, with the nurse typically asking, “What do you want talk about today?” Every session included a mood check using the BDI-1, assignment by mutual agreement of some “homework” (i.e. behavioral or cognitive tasks) to reinforce skills learned during the session. Typical topics for each session were: Week 1: Orientation to therapy, goals and expectation of therapy, Week 2: Identifying negative automatic thoughts in difficult situations during the previous week, practice reframing negative thoughts; Weeks 3–6: Continued analysis of negative thoughts, identification of core beliefs, problem-solving, coping strategies, Week 7: Self-therapy guide and relapse prevention, Week 8: Termination, review self-therapy guide, accomplishments of therapy. Postoperative recovery education was not the focus of therapy. However, if patients brought up concerns, such as fatigue, wound care, and diet, therapy nurses answered their questions briefly in a manner consistent with the written discharge instructions they had received and encouraged them to seek advice from their primary care providers and specialists. In addition, therapy nurses coded session activities, which reflected high levels of agreement in weekly activities, and met weekly to insure adherence to the manual and to discuss individual cases. In case conferences, led by a study investigator (L.D.), fidelity to the intervention was insured through assessment and discussion of specific CBT techniques used to address common themes and problems; the study psychiatrist (M.R.I.) was available for consultation
At the end of the initial eight weeks, the presence of clinical depression in the CBT and UC groups was re-evaluated via the SCID-I by a trained research nurse, who was blinded to the treatment group. For the UC+CBT group, SCID-I interviews were repeated at the end of therapy. A suicide protocol was in place and approved by the IRBs at all sites for subjects who became more depressed and expressed suicidal ideation/intention. The protocol consisted of identifying the subject’s location, devising a no-suicide plan and contract with the patient, and contacting the police and/or Psychiatric Mobile Response Team (PMRT) for inpatient treatment.
Instruments
The SCID-I was used to determine presence or absence of clinical depression. It is widely accepted and has been used as a criterion reference in studies evaluating other interviews and questionnaires for the identification of Axis 1 disorders.14 The SCID-I has reported inter-rater agreement of 82% and kappa score of .79 for major depressive disorder.19 It was selected because it allowed screening for excluded conditions, as well as clinical depression. Criteria for major and minor depression in the SCID are consistent with the DSM-IV-R, as described in the Inclusion Criteria..
Depressive symptoms were measured with the Beck Depression Inventory (BDI), a 21-item self-report measure used widely used in cardiac patients.20,21 Used in over 2,000 empirical studies, the BDI has sound internal consistency (i.e., mean Cronbach’s alpha = 0.82) and concurrent validity (i.e. with the Hamilton Rating Scale for Depression (r = .75) for non-psychiatric populations.22 In the current study, internal consistency of the BDI at baseline yielded an α-coefficient of 0.87.
Anxiety, known to be highly comorbid with depression,23 was also assessed. It was measured by the Brief Symptom Inventory (BSI) Anxiety Subscale, a 6-item questionnaire that measures psychological state anxiety symptoms. Each item is rated on a 5-point scale, with higher scores indicative of higher anxiety. The BSI has been used in related cardiac populations,24 and has demonstrated strong internal consistency (Cronbach’s α = .87) and criterion validity with the Speilberger Anxiety Index (r = .70).25 Cronbach’s α in this study was 0.87.
Analysis
All data analyses were conducted with IBM SPSS 19 (IBM, Somers, NY 2010). Baseline characteristics between CBT and UC groups were compared using χ2 analyses and Student’s T-test (Table 1). Comparisons between the CBT and UC groups and between the CBT and UC+CBT groups were completed using linear mixed models with maximum likelihood estimation to assess the association between BDI scores over time. A square root transformation was used on raw BDI scores to fit normality assumptions. The models included a random intercept for each subject, a fixed time factor, group, and the interaction between time and group. Analyses followed intention-to-treat (ITT) principles, in which baseline scores or last BDI scores were imputed for individuals who were excluded or didn’t finish eight weeks of CBT. We tested models adjusting for gender, antidepressant use, history of depression, anxiety scores, BMI, age, statins, employment, and post-operative complications. For comparison of CBT and UC+CBT groups, we also included duration of depressive symptoms (from date of surgery to the start of CBT). Analyses of group differences were unchanged when adjusting for these variables, so results of the simple model are reported. Completer analyses yielded equivalent results, so ITT analyses are reported.
Table 1.
Demographic and Clinical Characteristics
| Characteristics | Cognitive Behavioral Therapy Group (n=45) | Usual Care Group (n=36) | P valuea |
|---|---|---|---|
| No. (%) | No. (%) | ||
| Female | 9 (20.0) | 16 (44.4) | 0.02 |
| Non-Hispanic White | 28 (62.2) | 24 (66.7) | 0.68 |
| > high school education | 35 (77.8) | 25 (71.4) | 0.52 |
| Married or cohabitating | 35 (78.3) | 23 (63.9) | 0.17 |
| Employed | 17 (37.8) | 11 (30.6) | 0.50 |
| Non-Elective Surgery | 19 (42.2) | 18 (51.4) | 0.41 |
| Type of Surgery | |||
| CABG | 32 (71.1) | 23 (63.9) | 0.85 |
| AVR | 6 (13.3) | 6 (16.7) | |
| MVR | 3 (6.7) | 2 (5.6) | |
| CABG & AVR/MVR | 4 (8.9) | 5 (13.9) | |
| Post-op Complications (yes) | 24 (55.8) | 19 (54.3) | 0.89 |
| Type of Depression – baseline | |||
| major | 34 (75.6) | 29 (80.6) | 0.59 |
| minor | 11 (24.4) | 7 (19.4) | |
| History of Depression | 16 (35.6) | 11 (30.6) | 0.64 |
| On antidepressants | 17 (37.8) | 12 (33.3) | 0.68 |
| Mean (SD) | Mean (SD) | ||
| Age (years) | 63.4 (8.4) | 63.9 (11.4) | 0.83 |
| Body Mass Index (kg/m2) | 30.1 (7.3) | 31.2 (10.9) | 0.59 |
| Charlson Comorbidity Index Total Score | 3.5 (2.0) | 4.4 (2.3) | 0.07 |
| Hospital length of stay (days) | 9.1 (5.2) | 10.3 (6.3) | 0.33 |
| Mini Mental Exam Total Score | 27.5 (0.9) | 27.4 (0.9) | 0.46 |
| Number of grafts | 2.4 (1.4) | 2.1 (1.3) | 0.38 |
| Pump time (min) | 92.7 (46.1) | 108.8 (63.7) | 0.21 |
| Cross clamp time (min) | 65.5 (39.0) | 87.7 (63.6) | 0.07 |
| Ejection Fraction | 51.3 (13.8) | 50.5 (14.7) | 0.81 |
| Baseline BDI | 16.8 (9.3) | 15.1 (8.9) | 0.43 |
| Baseline BSI | 9.5 (7.8) | 8.3 (6.8) | 0.54 |
using t tests or χ2 tests
Abbreviations: AVR=aortic valve replacement; BDI=Beck Depression Inventory; BSI = Brief Symptom Inventory; CABG = Coronary artery bypass graft; MVR = mitral valve replacement
Treatment response was examined using three methods. First, we compared changes in the distribution of BDI severity categories (none-minimal = <10, mild = 10–18, moderate = 19–29, severe= >29) from baseline to 8 weeks within UC, CBT, and UC+CBT groups using the McNemar-Bowker test, which extends the McNemar test for symmetry for tables with more than 2 categories.26 Then, we evaluated the distribution of individual changes in depressive symptom severity (i.e. worse, same, or improved) from baseline to post-treatment. Second, between-group differences in the post-test presence of clinical depression was evaluated by χ2 analyses and ITT principles. Lastly, to determine clinical significance, we used the two-step method of Jacobson and Truax.27,28 This method defines clinical significant change as (1) a symptom score that decreased by a reliable amount and not due to chance variation (reliable change index [RCI]) and (2) a post-treatment symptom score in the non-dysfunctional range. Patients with final BDI scores < 10 and an RCI > 1.96) 27,28 were considered to have experienced clinical significant change. Significance levels for all analyses were set at p < .05
RESULTS
A total of 81 patients with clinical depression were randomized (Figure 1). Forty-five individuals were assigned to CBT, and 36 were assigned to UC. There were no statistical differences between CBT and UC groups in age, race/ethnicity, educational level, type of cardiac surgery, or marital or employment status (Table 1). However, the CBT group had fewer women than the UC group (p = .02). There were no statistical differences in history of depression, antidepressant use, anxiety level or other medications between the groups. Sensitivity analysis of CBT and UC groups excluding the individuals who did not receive the allocated intervention yielded similar results. There were no statistical differences between UC participants who elected to have CBT later and those who declined, or between the CBT and the UC+CBT groups.
Cognitive Behavioral Therapy vs. Usual Care
Participants in the CBT group had a significantly greater reduction in depressive symptoms than those in the UC group (Table 2). Linear mixed models analyses indicated a significant group by time interaction effect. BDI scores decreased over time in the CBT group, while BDI scores increased over time in the UC group (β=1.41 [95% CI 0.81–2.02]). In the post-test SCID-I interview, 29 individuals (64%) from the CBT group experienced remission, compared with 9 (25%) from the UC group (p < .001) (Table 3). The number needed to produce one additional treatment response was 2.5 (95% CI: 1.7 – 4.9).
Table 2.
Depressive Symptoms Across Time
| Pairwise Comparison of Means and Standard Deviations | ||||
|---|---|---|---|---|
| Early CBT (n = 45) (mean ± SD) |
Usual Care (n = 36) (mean ± SD) |
Early CBT (n = 45) (mean ± SD) |
Later CBT (n = 25) (mean ± SD) |
|
| Change in BDI scores (Posttest-pretest) | −6.91 (9.9) | 2.03 (9.8)* | −6.91 (9.9) | −5.40 (7.2)** |
| Linear Mixed Models Analysis with Random Intercept | ||||||||
|---|---|---|---|---|---|---|---|---|
| Early CBT vs. Usual Care | Early CBT vs. Later CBT | |||||||
| Parameter | Beta | SE | 95% CI | P | Beta | SE | 95% CI | P |
| Intercept | 3.95 | 0.97 | 3.58 – 4.32 | <.001 | 4.21 | 0.32 | 3.59 – 4.84 | <.001 |
| Time (coded 0,1) | −1.19 | 0.20 | −1.59 – −0.79 | <.001 | −1.85 | 0.20 | --2.26 – −1.45 | <.001 |
| Symptom duration | 0.001 | 0.00 | −0.008 – 0.01 | 0.88 | ||||
| Group: Early (UC = 1; CBT = 0) Later (UC+CBT = 1; CBT = 0) | − 0.23 | 0.28 | −0.79 – 0.33 | 0.42 | − 0.27 | 0.47 | − 1.20 – 0.67 | 0.57 |
| Group X Time | 1.41 | 0.30 | 0.81–2.02 | <.001 | 0.79 | 0.34 | 0.10–1.47 | 0.03 |
| −2 log likelihood | 518.41 | 339.29 | ||||||
p < .001,
p=.07
Abbreviations: CBT = Early Cognitive Behavioral Therapy; UC = Usual Care, UC+CBT = Completed CBT after usual care; SE = Standard Error; CI =Confidence Interval
Table 3.
Distribution of Post-treatment Symptom Severity, Reliability of Change, and Remission
| Outcome | All Patients | ||
|---|---|---|---|
| CBT (n=45) | UC (n=36) | UC+CBT (n=25) | |
| Post-treatment BDI < 10, No. (%) | 30 (66.7%) | 7 (19.4%)b | 11 (44%)d |
| Post-treatment remission by SCID, No. (%) | 29 (64.4%) | 9 (25%)b | 14 (56%) |
| Pre-treatment BDI ≥ 10a | |||
| Outcome | CBT (n=40) | UC (n=28) | UC+CBT (n=20) |
| Post-treatment BDI < 10: Unreliable change, No. (%) | 1 (2.5%) | 0 | 1 (5.0%) |
| Post-treatment BDI < 10: Reliable change, No. (%) | 24 (60%) | 3 (10.7%)b | 5 (25%)c |
| Post-treatment remission by SCID, No. (%) | 27 (67.5%) | 4 (14.3%)b | 10 (50%) |
Using methods of Jacobson and Truax
CBT vs. UC comparison, Fisher’s exact test p<.001
CBT vs. UC+CBT comparison, Fisher’s exact test p=.01
CBT vs. UC+CBT comparison, Fisher’s exact test p=.08
Abbreviations: BDI = Beck Depression Inventory; CBT = Cognitive Behavioral Therapy; UC = Usual Care; SCID = Structured Clinical Interview for Diagnostic and Statistical Manual; UC+CBT = Completed CBT after usual care
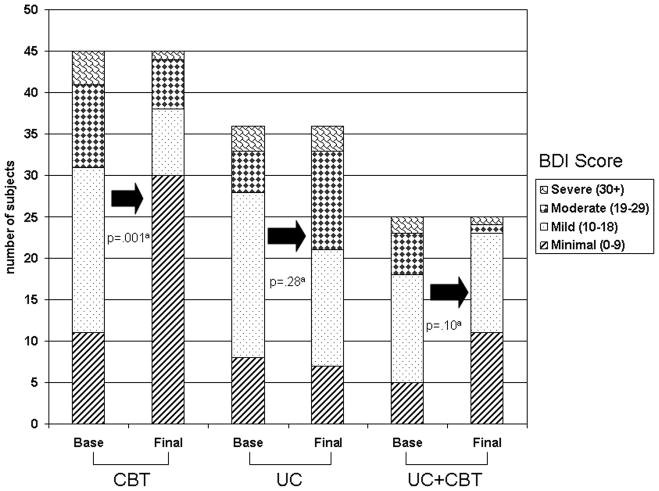
For depressive symptom categories, the CBT group showed a significant decrease in severity of depressive symptoms while the UC group did not (Figure 2). In the CBT group, 14 (7%) at baseline had moderate to severe symptoms compared to 7 (15.6%) after CBT (p = .001). In the UC group, there was no change in the distribution of symptom severity categories from baseline to eight weeks (p = .28). Twenty-two individuals (48%) in the CBT group improved across symptom categories, compared with only 8 (22%) in the UC group (p<.001). Using both RCIs and a cutoff score of BDI < 10, we found that among 68 participants who exceeded the cutoff score at baseline, 24 (60%) of those in the CBT group experienced clinical significant improvement in symptoms compared to only 3 (11%) in the UC group (p<.001) (Table 3). Overall, individuals in the CBT group were more likely to exhibit clinical and significant change compared to both those in the UC group (p < .001).
Figure 2.
Change in BDI Severity within Groups
Abbreviations: CBT = Early Cognitive Behavioral Therapy; UC = Usual Care, UC+CBT = Later CBT completed after usual care;
ap values computed using McNemar-Bowker test.
Early Cognitive Behavioral Therapy vs. Later Cognitive Behavioral Therapy
The early CBT group had a significantly greater reduction in depressive symptoms than those in the later CBT group (UC+CBT), with a significant group by time interaction effect in linear mixed models analysis (Table 2) (β=0.79 [95% CI 0.10–1.47]). However, the magnitude of the effect was smaller than in the CBT vs. UC model. Furthermore, in contrast to the CBT vs. UC comparison, rates of remission of clinical depression were similar between the early CBT and UC+CBT groups (29 [64.4%] vs. 14[56%], p = .33).
For depressive symptom categories, the UC+CBT group showed no change in overall distribution of symptom severity categories over the eight weeks of therapy (p = .10, Figure 2). Using the RCI and a cutoff score of BDI < 10, we found that among 20 participants who exceeded the cutoff score at baseline, only five (25%) of those in the UC+CBT group showed clinical significant improvement in symptoms in contrast to 24 (60%) of those in the early CBT group. Hence, more individuals in the early CBT group experienced clinical and significant change in BDI scores compared to those in the UC+CBT group (p=.01, Table 3).
DISCUSSION
Our findings show for the first time that a brief course of CBT delivered early after cardiac surgery by nurses in the home is effective in improving depression outcomes. Depressive symptoms were sharply reduced and clinical depression remitted more in those receiving early CBT than in those receiving usual care. The decline in depressive symptoms for early CBT was clinically robust and comparable to response rates for antidepressant medications − 51% for antidepressant medications vs. 32% for placebo.29 Using the results of our post-test SCID interviews, early CBT produced a 64% response rate vs. 25% for usual care. Of note, compared to early CBT, CBT performed later (after eight weeks of usual care) was less effective in reducing depressive symptoms, but yielded an equivalent rate of clinical remission.
Several factors may have accounted for the positive outcomes of early CBT treatment. The early timing of therapy may have interrupted new cases of depression at a critical time before they could become entrenched. Other investigators have shown that the duration of untreated major depressive episodes has a negative effect on treatment outcomes.30,31,32,33 It is speculated that untreated symptoms alter the character of the depression itself, yielding it more resistant to treatment.31 Using data from the Canadian Community Health Survey, Patten et al demonstrated that an individual with depressive symptoms of three weeks duration has a 40% probability of recovery over the subsequent six weeks, whereas an individual with symptoms for 23 weeks has substantially less probability of recovery at less than a 5%. Using Patten’s calculator, the CBT and UC+CBT groups, with median durations of symptoms of 6.5 and 16.8 weeks could be expected to show recovery rates of 24% and 8%, respectively.31 Our data exceed these predictions substantially. Our findings provide further evidence that early CBT in cardiac patients with postoperative depression is effective and provides greater symptom relief than delayed treatment. In particular, the success of CBT may arise from its focus on cognitive, behavioral and social dimensions of depression that may become habituated as the duration of symptoms increases.31
A second explanation for our findings is that early CBT may have prevented the exacerbation of pre-existing depressive episodes. This notion is consistent with the symptom relief we found, even in the absence of complete remission. Although we did not find an effect of prior history of depression on treatment outcomes, it is possible that patients who were depressed postoperatively had pre-existing depressive episodes that had not been identified and were untreated or undertreated at enrollment. Further study is needed to explicate more fully the effect of the duration of illness on early CBT outcomes after cardiac surgery.
The smaller number of women enrolled in CBT compared to UC may also have influenced our findings. In the ENRICHD study, women did not respond to CBT as well as men did. It is possible that the greater number of women in our UC group may have contributed disproportionally to the poorer outcomes in that group. Conversely, since the CBT group included more men than women, the lack of women in that group could have contributed to their improved response to CBT. Further study with larger numbers of women in both groups is needed to fully explain the role of gender in response to CBT.
Other factors related to the use of nurses to deliver CBT could have influenced our findings. First, the nurses’ ability to use CBT techniques to guide patients in evaluation of their postoperative medical complaints may have improved outcomes. Although this support was less comprehensive in addressing postoperative cardiac care than that in recent collaboration care models,34 it is possible that the nurses’ support of patient decision-making regarding postoperative recovery enhanced the CBT intervention. While the content of individual therapy sessions was driven by the patient, the CBT intervention was highly structured and focused on thoughts, emotions and behaviors associated with depression; its structure was reinforced by specific training, monitoring of session activities, and weekly case conferences. While it is possible that our positive outcomes were due to the attention patients received from the home visits and not the content of the therapy, a previous study of a home-based psychosocial nursing intervention in cardiac patients does not support that notion.35 In that study, nurses’ visits were ineffective in reducing depressive symptoms. While those nurses were experienced in cardiac care, they received no special training in depression treatment.
Finally, patients generally trust nurses and rate their honesty and ethical standards highly.36 This inherent credibility may have provided a foundation for a strong therapeutic alliance and subsequent CBT effectiveness. In two other studies of nurse case managers, the same benefit may have accrued. However, neither study focused on psychotherapy; nurse case managers were involved primarily in coordination of antidepressant therapy.11,34 Thus, in the current report, the use of nurses for postoperative depression management with CBT is unique.
This is the first study in which nurses have conducted home CBT in patients early after cardiac surgery. In two previous reports of depression treatment after bypass, investigators reported positive results with CBT conducted by clinical psychologists or social workers up to one year after surgery10 and with nurse case-management, which involved coordination of antidepressants and/or referral to a psychologist or psychiatrist.11,37 A third study including patients with CHD also used nurse case-managers, but included coordinated depression treatment and cardiac care34. In the current study compared to previous reports, therapy was initiated earlier and the role of nurses was expanded to encompass both delivery of CBT and support for routine postoperative recovery. Our findings demonstrate that nurses who have received CBT training can intervene successfully in reducing clinical depression and depressive symptoms in cardiac patients.
The current report has several limitations. Our study included a relatively small sample of depressed post-cardiac surgery patients. We included only individuals who met diagnostic criteria for clinical depression. Thus, we were not able to evaluate treatment effectiveness in individuals with depressive symptoms who did not meet these criteria. We had a relatively large attrition rate, with depressed women more likely to drop out than depressed men (p < .05). While other investigators using CBT in randomized studies have reported similar or higher rates of dropout from 30 to 37%,38–40 further study is need to examine gender responses to therapy and to consider practical applications of CBT. Our offer of delayed treatment after completion of the usual care condition may have contributed positively to retention in the UC group. Future studies may be needed to test appropriate measures to limit attrition in this depressed population. We were able to conduct post-test evaluations only and did not include long-term follow-up to evaluate the duration of study effects. Finally, we did not include a cost effectiveness analysis, which would have allowed further evaluation of the study intervention. In summary, the current findings support early CBT for depressed post-cardiac surgery patients. While previous studies have shown that CBT is an effective treatment for depression in this population, the current findings support the unique benefit of CBT administered early in the home environment by nurses. Further study is needed to determine the long-term effects and cost-effectiveness of early home CBT, to explore the relationship of symptom duration to treatment outcome after cardiac surgery, and to evaluate the use of early home CBT delivered by nurses in a wider range of cardiac patients with depressive symptoms.
Summary and Implications.
What’s New?
Early home CBT is effective in reducing depressive symptoms and clinical depression in depressed patients recovering from cardiac surgery
Early treatment is associated with greater symptom reduction than similar therapy given later after surgery
First study in which nurses conducted cognitive behavioral therapy in depressed patients recovering from cardiac surgery
Acknowledgments
Supported by NINR R01NR009228
Funding/Support: This research was supported by a grant from the National Institute of Nursing Research (NINR) (R01NR009228) to Dr. Doering. This study also received support from the Inflammatory Biology Core of the UCLA Older Americans Independence Center, NIH/NIA Grant P30-AG028748.
Role of the Sponsor: The NINR had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Dr. Doering had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Doering, Irwin, Nyamathi
Acquisition of data: Doering, Chen, Cross, Magsarili, Irwin
Analysis and interpretation of data: Doering, Irwin, Chen, Cross,
Drafting of the manuscript: Doering, Irwin, Chen, Cross, Nyamathi
Critical revision of the manuscript for important intellectual content: Doering, Irwin, Chen, Cross, Nyamathi, Magsarili
Statistical analysis: Doering, Irwin, Chen
Obtained funding: Doering, Irwin
Administrative, technical, or material support: Doering, Irwin, Chen, Cross, Nyamathi, Magsarili
Study supervision: Doering, Irwin, Nyamathi, Magsarili
Trials Registration: clinicaltrials.gov Identifier: NCT00522717
Conflicts of Interest and Financial Disclosures: None
Financial Disclosures: None reported.
Disclaimer: This report’s contents are solely the responsibility of the authors and do not necessarily represent the official views of NINR or the National Institutes of Health.
Additional Contributions: We thank our collaborators at our recruitment sites: Cedars-Sinai Medical Center; Kaiser Permanente Medical Center-Sunset, Los Angeles; West Los Angeles Veterans Administration Medical Center; Long Beach Memorial Medical Care; and Ronald Reagan UCLA Medical Center. We are also grateful to all the volunteers and nurses who participated in the study.
Contributor Information
Lynn V. Doering, University of California, Los Angeles, School of Nursing, Los Angeles, CA.
Belinda Chen, University of California, Los Angeles, School of Nursing, Los Angeles, CA.
Rebecca Cross, California State University, Fullerton, School of Nursing, Fullerton, CA.
Marise C. Magsarili, Kaiser Permanente Medical Center, Los Angeles, CA.
Adey Nyamathi, University of California, Los Angeles, School of Nursing Los Angeles, CA.
Michael R. Irwin, Cousins Center for Psychoneuroimmunology, UCLA Semel Institute for Neuroscience and Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA.
References
- 1.Stroobant N, Vingerhoets G. Depression, anxiety, and neuropsychological performance in coronary artery bypass graft patients: a follow-up study. Psychosomatics. 2008;49(4):326–331. doi: 10.1176/appi.psy.49.4.326. [DOI] [PubMed] [Google Scholar]
- 2.Baker RA, Andrew MJ, Schrader G, Knight JL. Preoperative depression and mortality in coronary artery bypass surgery: preliminary findings. ANZ J Surg. 2001;71(3):139–142. doi: 10.1046/j.1440-1622.2001.02055.x. [DOI] [PubMed] [Google Scholar]
- 3.Borowicz L, Jr, Royall R, Grega M, Selnes O, Lyketsos C, McKhann G. Depression and cardiac morbidity 5 years after coronary artery bypass surgery. Psychosomatics. 2002;43(6):464–471. doi: 10.1176/appi.psy.43.6.464. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal JA, Lett HS, Babyak MA, et al. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362(9384):604–609. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 5.Burg MM, Benedetto MC, Rosenberg R, Soufer R. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med. 2003;65(1):111–118. doi: 10.1097/01.psy.0000038940.33335.09. [DOI] [PubMed] [Google Scholar]
- 6.Tully PJ, Baker RA, Knight JL. Anxiety and depression as risk factors for mortality after coronary artery bypass surgery. J Psychosom Res. 2008;64(3):285–290. doi: 10.1016/j.jpsychores.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Connerney I, Shapiro PA, McLaughlin JS, Bagiella E, Sloan RP. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet. 2001;358(9295):1766–1771. doi: 10.1016/S0140-6736(01)06803-9. [DOI] [PubMed] [Google Scholar]
- 8.Connerney I, Sloan RP, Shapiro PA, Bagiella E, Seckman C. Depression is associated with increased mortality 10 years after coronary artery bypass surgery. Psychosom Med. 2010;72(9):874–881. doi: 10.1097/PSY.0b013e3181f65fc1. [DOI] [PubMed] [Google Scholar]
- 9.Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111(3):271–277. doi: 10.1161/01.CIR.0000152102.29293.D7. [DOI] [PubMed] [Google Scholar]
- 10.Freedland KE, Skala JA, Carney RM, et al. Treatment of Depression After Coronary Artery Bypass Surgery: A Randomized Controlled Trial. Arch Gen Psychiatry. 2009;66(4):387–396. doi: 10.1001/archgenpsychiatry.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rollman BL, Belnap BH, LeMenager MS, et al. Telephone-Delivered Collaborative Care for Treating Post-CABG Depression. JAMA: The Journal of the American Medical Association. 2009;302(19):2095–2103. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gary RA, Dunbar SB, Higgins MK, Musselman DL, Smith AL. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. Journal of Psychosomatic Research. 2010;69(2):119–131. doi: 10.1016/j.jpsychores.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pirraglia PA, Peterson JC, Williams-Russo P, Gorkin L, Charlson ME. Depressive symptomatology in coronary artery bypass graft surgery patients. International Journal of Geriatric Psychiatry. 1999;14(8):668–680. doi: 10.1002/(sici)1099-1166(199908)14:8<668::aid-gps988>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 14.Segal DL, Hersen M, Van Hasselt VB. Reliability of the Structured Clinical Interview for DSM-III-R: an evaluative review. Compr Psychiatry. 1994;35(4):316–327. doi: 10.1016/0010-440x(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 15.Folstein MF, Folsltein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Disease. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Doering LV, Cross R, Vredevoe D, Martinez-Maza O, Cowan MJ. Infection, depression, and immunity in women after coronary artery bypass: a pilot study of cognitive behavioral therapy. Altern Ther Health Med. 2007;13(3):18–21. [PubMed] [Google Scholar]
- 18.Beck AT. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- 19.Riskind JH, Beck AT, Berchick RJ, Brown G, Steer RA. Reliability of DSM-III diagnoses for major depression and generalized anxiety disorder using the structured clinical interview for DSM-III. Arch Gen Psychiatry. 1987;44(9):817–820. doi: 10.1001/archpsyc.1987.01800210065010. [DOI] [PubMed] [Google Scholar]
- 20.Frasure-Smith N, Lesperance F, Juneau M, Talajic M, Bourassa MG. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61(1):26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. [Google Scholar]
- 22.Richter P, Werner J, Heerlein A, Kraus A, Sauer H. On the validity of the Beck Depression Inventory. A review. Psychopathology. 1998;31(3):160–168. doi: 10.1159/000066239. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychol Med. 2008;38(3):365–374. doi: 10.1017/S0033291707002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKinley S, Moser DK, Dracup K. Treatment-seeking behavior for acute myocardial infarction symptoms in North America and Australia. Heart Lung. 2000;29(4):237–247. doi: 10.1067/mhl.2000.106940. [DOI] [PubMed] [Google Scholar]
- 25.Abu Ruz ME, Lennie TA, Riegel B, McKinley S, Doering LV, Moser DK. Evidence that the brief symptom inventory can be used to measure anxiety quickly and reliably in patients hospitalized for acute myocardial infarction. J Cardiovasc Nurs. 2010;25(2):117–123. doi: 10.1097/JCN.0b013e3181b56626. [DOI] [PubMed] [Google Scholar]
- 26.Bowker AH. A test for symmetry in contingency tables. J Am Stat Assoc. 1948;43(244):572–574. doi: 10.1080/01621459.1948.10483284. [DOI] [PubMed] [Google Scholar]
- 27.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 28.Seggar LB, Lambert MJ, Hansen NB. Assessing clinical significance: Application to the beck depression inventory. Behavior Therapy. 2002;33(2):253–269. [Google Scholar]
- 29.Williams JW, Jr, Mulrow CD, Chiquette E, Noel PH, Aguilar C, Cornell J. A systematic review of newer pharmacotherapies for depression in adults: evidence report summary. Ann Intern Med. 2000;132(9):743–756. doi: 10.7326/0003-4819-132-9-200005020-00011. [DOI] [PubMed] [Google Scholar]
- 30.Shapiro RW, Keller MB. Initial 6-month follow-up of patients with major depressive disorder. A preliminary report from the NIMH collaborative study of the psychobiology of depression. J Affect Disord. 1981;3(3):205–220. doi: 10.1016/0165-0327(81)90023-9. [DOI] [PubMed] [Google Scholar]
- 31.Patten SB. A major depression prognosis calculator based on episode duration. Clin Pract Epidemiol Ment Health. 2006;2:13. doi: 10.1186/1745-0179-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okuda A, Suzuki T, Kishi T, et al. Duration of untreated illness and antidepressant fluvoxamine response in major depressive disorder. Psychiatry Clin Neurosci. 2010;64(3):268–273. doi: 10.1111/j.1440-1819.2010.02091.x. [DOI] [PubMed] [Google Scholar]
- 33.de Diego-Adeliño J, Portella MJ, Puigdemont D, Pérez-Egea R, Álvarez E, Pérez V. A short duration of untreated illness (DUI) improves response outcomes in first-depressive episodes. Journal of Affective Disorders. 2010;120(1–3):221–225. doi: 10.1016/j.jad.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 34.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Frasure-Smith N, Lespérance F, Prince RH, et al. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. The Lancet. 1997;350(9076):473–479. doi: 10.1016/S0140-6736(97)02142-9. [DOI] [PubMed] [Google Scholar]
- 36.Jones JM. [Accessed Feb 23, 2011, 2011];Nurses Top Honesty and Ethics List for 11th Year. 2010 http://www.gallup.com/poll/145043/nurses-top-honesty-ethics-list-11-year.aspx.
- 37.Rollman BL, Belnap BH, LeMenager MS, Mazumdar S, Schulberg HC, Reynolds CF., III The Bypassing the Blues Treatment Protocol: Stepped Collaborative Care for Treating Post-CABG Depression. Psychosom Med. 2009;71(2):217–230. doi: 10.1097/PSY.0b013e3181970c1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crane C, Williams JM. Factors Associated with Attrition from Mindfulness-Based Cognitive Therapy in Patients with a History of Suicidal Depression. Mindfulness (N Y) 2010;1(1):10–20. doi: 10.1007/s12671-010-0003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Richards DA, Borglin G. Implementation of psychological therapies for anxiety and depression in routine practice: two year prospective cohort study. J Affect Disord. 2011;133(1–2):51–60. doi: 10.1016/j.jad.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 40.Grant K, McMeekin E, Jamieson R, Fairfull A, Miller C, White J. Individual Therapy Attrition Rates in a Low-Intensity Service: A Comparison of Cognitive Behavioural and Person-Centred Therapies and the Impact of Deprivation. Behav Cogn Psychother. 2011:1–5. doi: 10.1017/S1352465811000476. [DOI] [PubMed] [Google Scholar]