Abstract
Objectives
To document any consistent clinical findings in a large cohort of patients with whiplash associated disorder.
Design
Four-year observational study.
Setting
Large orthopaedic medicolegal practice in the UK.
Participants
1025 consecutive cases of chronic whiplash associated disorder.
Main outcome measures
Observational study of the clinical features of whiplash associated disorder: detailed examination
Results
Three consistent clinical features: neck pain; reduced cervical spine range of motion; and myofascial-entheseal dysfunction. With regards to the myofascial-entheseal dysfunction there were trigger points in the upper, middle or lower trapezius; with or without enthesopathy in the lower or middle trapezius.
Conclusions
On the basis of this large observational experience we propose a clinically-based definition of chronic whiplash associated disorder: a painful syndrome following acceleration-deceleration injury with neck stiffness; and myofascial-entheseal dysfunction.
Introduction
Chronic whiplash associated disorder is a challenging and apparently heterogeneous entitity. In 1995 the Quebec Task Force published their systematic review of whiplash injuries and defined whiplash associated disorder mechanistically as an acceleration-deceleration mechanism of energy transfer to the neck.1 One of the problems is that the clinical findings in whiplash injuries do not appear consistent. The question is whether this is because this is a heterogeneous group of patients and problems; or because as clinicians we have thus far been unable to fully characterize the condition.
Increasingly, the role of enthesopathy, myofascial pain and trigger points in musculoskeletal pain generation is being recognized; and are presently the subject of a great deal of clinical and basic science study: both in terms of the general and specific (regional) issues. Thus far, a Pubmed search does not reveal any clinical investigation of the role of myofascial-entheseal dysfunction in whiplash injury: hence initially the general concepts of myofascial-entheseal dysfunction and parallels with regional myofascial-entheseal dysfunction which had been characterized were necessary.
We have previously elucidated the role of enthesopathy and dysfunction of the musculo-fascial unit in chronic sporting soft-tissue problems.2,3 The basic science work of Benjamin et al.4 on the enthesis has enabled clinicians to better characterize chronic soft-tissue problems which have previously been largely misunderstood. Thus, dysfunction of the entheseal-myo-fascial unit is now recognized as key in conditions that were previously considered to have an acute inflammatory component, such as tennis elbow (lateral epicondylitis),4 golfer's elbow (medial epicondylitis)4 and in chronic athletic groin pain (osteitis pubis).3 It is now clear that enthesopathy has a role in all of these conditions. Entheses are specialized attachments of myofascial units to bone and are sites of stress concentration, and hence are prone to microtrauma and chronic inflammation:4 this is termed enthesopathy (Table 1). Enthesopathy can sometimes be visualized on gadolinium enhanced MRI scanning once the correct protocol has been devised,2,3 and MRI-positive enthesopathy is usually seen in more severely affected cases.2,3
Table 1.
Enthesopathy clinical features
|
The trapezius muscle is a large diamond-shaped superficial muscle which attaches in the midline from the occiput through to the mid-thoracic spine, and laterally to the scapula and lateral clavicle; and with upper, middle and lower components. The muscle is the commonest site of myofascial dysfunction with trigger points in the human body;5 and enthesopathy is also known to be a clinical issue. Whilst there have been, as far as we are aware, no clinical studies of the trapezius in a large series of whiplash patients: trapezius abnormalities in this patient group are well-documented. 6,7 This observational study aimed initially only to document any totally consistent clinical findings in whiplash injury; but in the second phase of the study we then sought to characterize the ubiquitous myofascial-entheseal dysfunction which was documented in the first phase; and indeed which has been observed by others on a basic science level.6,7
Methods
Between 2009 and 2012, the authors examined 1000 patients with whiplash injury, according to the Quebec Task force mechanistic definition, with chronic symptoms (over six months duration) (Table 2). We documented the circumstances of the accident, progression of symptoms and treatment and clinical features.
Table 2.
Inclusion criteria for 1000 cases
|
In the 1000 patients examined, there were indeed consistent findings, of reduced range of cervical spine movement; and myofascial-entheseal dysfunction. For the second phase of the study we sought to document the nature of the myofascial-entheseal dysfunction in 25 consecutive cases.
There were three solely consistent features in all 1025 patients: acceleration-deceleration injury to cervical spine; reduced range of cervical spine movement; and dysfunction of the trapezius muscle with or without enthesopathy.
In 2012 we then documented the specifics of the myofascial-entheseal dysfunction in twenty-five consecutive cases, specifically with regards to myo-fascial dysfunction of the trapezius; the presence or absence of enthesopathy; and the site of the problem (upper, middle or lower trapezius).
Results for case series
Mean age 42 years
44% male, 56% male
- Mean range of global cervical spine movement restriction 9.2 %
- Range 5–15%
- Enthesopathy (see Table 1)
- middle and lower parts of trapezius
- At scapular attachment
- 48%
Figure 1.
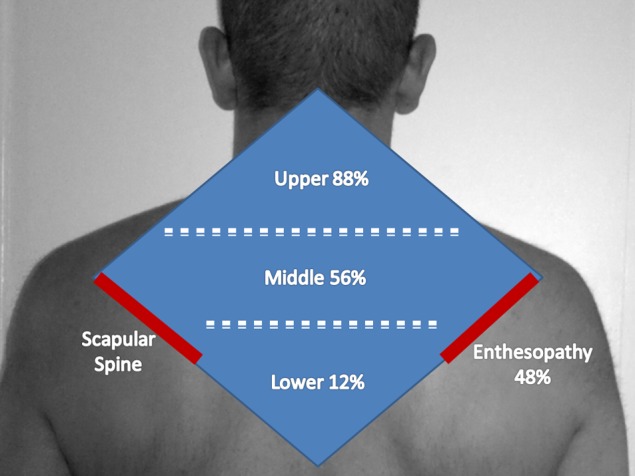
Myofascial-entheseal dysfunction in chronic whiplash injury
Table 3.
Myofascial-entheseal dysfunction site
| Upper | 88% |
| Middle | 56% |
| Lower | 12% |
Discussion
The Quebec Task force mechanistic definition of whiplash associated disorder is useful, simple but also clinically ambiguous. Chronic whiplash injuries are difficult to treat and assess for many reasons, but we suggest the lack of a consistent and all-encompassing clinically-based definition is a major factor. The trapezius muscle has been implicated in basic science work on whiplash injury6–7 but appears thus far to have been overlooked from a clinical perspective. The muscle is known to be the commonest site of myofascial dysfunction,5 and its anatomy correlates with the symptoms of whiplash: neck pain/headaches-upper part; shoulder/scapular pain-middle part; and scapular/thoracic radiation-lower part.
The authors Yoganandan and Pintar and colleagues have extensively researched the kinematics and biomechanics of this injury.8,9 Their biomechanical, cadaveric and computer-model research has provided an important biomechanical insight into the nature of whiplash injury. Thus, in the first phase of a whiplash injury the upper cervical spine-head undergoes flexion while the lower cervical spine is in extension, and there is a reverse curvature of the head-neck complex. Initially the head lags behind and then ‘catches up’ with the neck. In the second phase of whiplash injury, the entirety of the head and neck is under an extension force, with a resultant single extension curvature. The lower cervical facet joints undergo compression and sliding: such that there is generalized sliding; with more compression posteriorly; resulting in a ‘pinching’ mechanism. It is our impression that the cervical facet joint injury is at least in part responsible for the neck stiffness that we have consistently observed in these patients.
The trapezius muscle has upper, middle and lower components; and all three areas are a relatively common source of myofascial pain with trigger points.5 Enthesopathy may affect the middle and lower parts of the muscle.5 Clinically, enthesopathy may be defined as: tender enthesis; pain on passive stretching; and pain on resisted muscle movement.2,3 The present study demonstrates that myofascial-entheseal dysfunction and enthesopathy is a consistent clinical features in chronic whiplash injuries. On the basis of our re-analysis of the available evidence of whiplash kinematics in light of the present study, we hypothesize that during the whiplash mechanism there is eccentric loading of the trapezius unit with microtrauma to the trapezius unit; and it is our impression that the trapezius is especially vulnerable during the transition between the first and second phases of the whiplash mechanism.
In the current paper, we have sought to document the consistent clinical findings in a large consecutive series of chronic whiplash cases; and the only totally consistent findings are reduced range of motion and dysfunction of the trapezius muscle. It appears that the role of the trapezius muscle has, thus far, largely been overlooked by clinicians in the whiplash syndrome. We suggest that this maybe partly due to the relatively recent identification of enthespathy and myfascial dysfunction as common sources of musculoskeletal pain. However, from a basic science perspective, trapezius abnormalities have been clearly demonstrated in whiplash patients.6,7 Clearly there are a multitude of other potential pain sources in whiplash injuries, but we suggest that logical treatment of chronic whiplash injuries should in the first instance target the neck stiffness and myofascial-entheseal dysfunction which appears to be ubiquitous.
The detailed analysis of the myofascial-entheseal dysfunction documents that the combination of myofascial dysfunction with trigger points and enthesopathy is a consistent finding in whiplash injuries. In our analysis, the upper trapezius is the usual site of myofascial dysfunction, with or without dysfunction in the lower and middle parts of the muscle. Trapezius enthesopathy was present in the middle and lower parts of the muscle at the scapular insertion in almost half of the whiplash patients. Interestingly, we did not observe any cases of enthesopathy of the attachment of the upper trapezius into the lateral clavicle in this patient cohort. Neither were we able to disinter midline trapezius enthesopathy from myofascial or facet joint dysfunction. The last decade has seen great advances in the understanding of the enthesis and enthesopathy,2–4 but the trapezius entheses have not been fully characterized. It is our hypothesis that the ‘enthesis organ’4 of the middle and lower trapezius at the scapular attachment is damaged during eccentric loading of the trapezius; and that the scapular attachment is particularly prone to stress concentration. This hypothesis can be tested in the future through basic science and imaging studies.
Whilst the present observational study demonstrates that myofascial-entheseal dysfunction is ubiquitous in chronic whiplash injury, it is clear that there are a range of potential pain sources in these patients. Other factors may include changes in cerebral blood flow,10 biopsychosocial factors11 and altered nociception.
We suggest the following clinical definition of chronic whiplash injury: a syndrome of pain following acceleration-deceleration injury, with reduced range of cervical spine movement and myofascial-entheseal dysfunction. Moreover, we suggest that rehabilitation should target these clinical abnormalities.
DECLARATION
Competing interests
None declared
Funding
None
Ethical approval
This is an observational study of a longstanding medicolegal practice, and clearly neither the medicolegal process nor patient management has been affected in any way by this study: hence no ethical approval has been sought
Guarantor
QMKB
Contributorship
Both authors have assessed all participants in this study; hence all listed authors are contributors. Both authors have contributed equally to this paper and have given permission for their names to be included as co-authors.
Acknowledgments
Annamma Bismil, Nursing Sister, ExpertOrthopaedics.Com
Reviewer
Kamran Abbasi
References
- 1.Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on whiplash-associated disoders: redefining ‘whiplash’ and its management. Spine 1995;20(8 Suppl):1S–73S [PubMed] [Google Scholar]
- 2.Schilders E, Bismil Q, Robinson P, O'Connor PJ, Gibbon WW, Talbot JC Adductor-related groin pain in competitive athleles: the role of MRI and entheseal pubic cleft injections. The Journal of Bone and Joint Surgery (American) 2007;89:2173–2178 [DOI] [PubMed] [Google Scholar]
- 3.Schilders E, Talbot JC, Robinson P, Dimitrakopoulou A, Gibbon WW, Bismil Q Adductor-related groin pain in recreational athletes: role of the adductor enthesis, magnetic resonance imaging, and entheseal pubic cleft injections. J Bone Joint Surg Am 2009;91:2455–60 [DOI] [PubMed] [Google Scholar]
- 4.Benjamin M, Toumi H, Ralphs JR, Bydder G, Best TM, Milz S Where tendons and ligaments meet bone: attachment sites (‘entheses’) in relation to exercise and/or mechanical load. Journal of Anatomy 2006;208:471–490 doi: 10.1111/j.1469-7580.2006.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Travell JG, Simons DG Myofascial Pain and Dysfunction. The Trigger Point Manual. Vol 2 Baltimore, Md: Williams & Wilkins; 1992:168–185 [Google Scholar]
- 6.Nederhand MJ, IJzerman MJ, Hermens HJ, Baten CT, Zilvold G Cervical muscle dysfunction in the chronic whiplash associated disorder grade II (WAD-II). Spine (Phila Pa 1976) 2000;25:1938–43 [DOI] [PubMed] [Google Scholar]
- 7.Gerdle B, Lemming D, Kristiansen J, Larsson B, Peolsson M, Rosendal L Biochemical alterations in the trapezius muscle of patients with chronic whiplash associated disorders (WAD)–a microdialysis study. Eur J Pain. 2008;12:82–93 Epub 2007 Apr 24 [DOI] [PubMed] [Google Scholar]
- 8.Stemper BD, Yoganandan N, Gennarelli TA, Pintar FA Localized cervical facet joint kinematics under physiological and whiplash loading. J Neurosurg Spine 2005;3:471–6 [DOI] [PubMed] [Google Scholar]
- 9.Cusick JF, Pintar FA, Yoganandan N Whiplash syndrome: kinematic factors influencing pain patterns. Spine (Phila Pa 1976) 2001;26:1252–8 [DOI] [PubMed] [Google Scholar]
- 10.Linnman C, Appel L, Söderlund A, et al. ‘Chronic whiplash symptoms are related to altered regional cerebral blood flow in the resting state’. Eur. J Pain 2009;12:65–70 [DOI] [PubMed] [Google Scholar]
- 11.Ferrari R, Schrader H ‘The late whiplash syndrome: a biopsychosocial approach’. J. Neurol. Neurosurg. Psychiatr 2001;70:722–6 doi:10.1136/jnnp.70.6.722 PMC 1737376.PMID 11385003 [DOI] [PMC free article] [PubMed] [Google Scholar]


