Primary lymphoma of the pituitary gland is an important diagnosis to consider in patients with seemingly inoperable pituitary tumours.
Introduction
Primary central nervous system lymphoma (PCNSL) is an uncommon form of non-Hodgkin's lymphoma that can affect any part of the brain or spinal cord. The progressive refinement of endocrine tests, as well as improvements in and increasing availability of diagnostic imaging, has led to an increasing number of pituitary masses being diagnosed.1,2 In addition, with the appearance of acquired immunodeficiency syndrome (AIDS) and organ transplantation in the last 30 years, the incidence of central nervous system (CNS) lymphoma is thought to have increased.2 Recent improved survival rates of patients with AIDS have led to a further increase in primary CNS lymphoma (PCNSL), with an estimated 2.5% of patients with AIDS developing PCNSL.3 PCNSL of the pituitary gland is an extremely rare form of this disease. In this article we report the case of an immunocompetent patient who presented with hemianopia and headache secondary to a large primary lymphoma of the pituitary gland which was initially thought to represent an inoperable and incurable tumour. A review of other reported cases is presented to establish common features of the disease.
Case report
A 67-year-old woman presented to the Ophthalmology Department with a left visual field defect and headache. Magnetic resonance imaging revealed a pituitary tumour measuring 3.6 × 3.4 × 2.85 cm (Figure 1), extending inferiorly to occupy the sphenoid sinus. Laboratory testing of endocrine function was normal and a staging computerized tomography scan showed no evidence of disease elsewhere. The past medical history included a T1 N1 MO breast cancer. The initial differential diagnosis for this tumour included metastasis, pituitary adenoma and meningioma. Neurosurgical review of the scans concluded that the appearances were that of an inoperable neoplasm. She was referred to the ENT department for a transnasal, trans-sphenoidal biopsy to gain a tissue diagnosis. During surgery the tumour was found to be filling the sphenoid sinus. In addition to a biopsy, debulking of the tumour was carried out. Postoperatively the patient noticed an immediate improvement in her visual field defect and headache. Histological analysis revealed a diffuse, large, high-grade B-cell pituitary lymphoma (Figure 2). A bone marrow biopsy was normal and the patient was treated with four cycles of chemotherapy and stereotactic radiotherapy. She had a complete response to treatment with no signs of recurrence at 15-month follow-up (Figure 3). Postoperative blood tests showed continued normal pituitary function, requiring no hormone replacement.
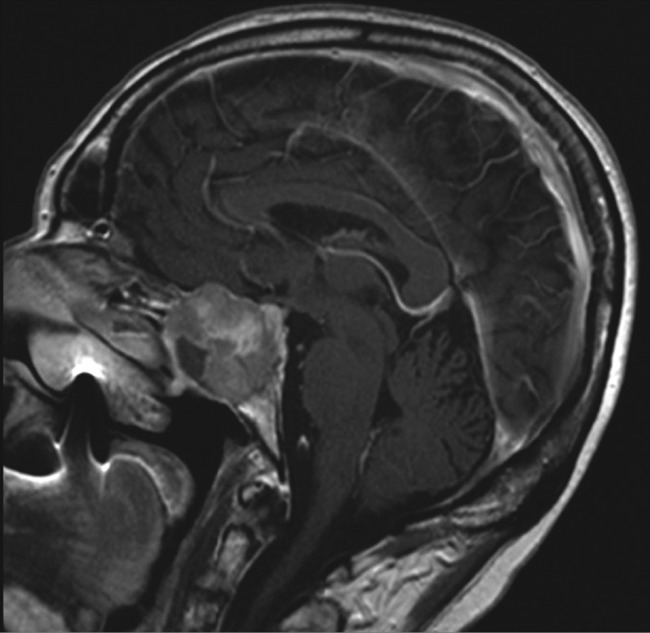
Figure 1.
Magnetic resonance imaging pre-endoscopic transnasal transphenoidal biopsy
Figure 2.
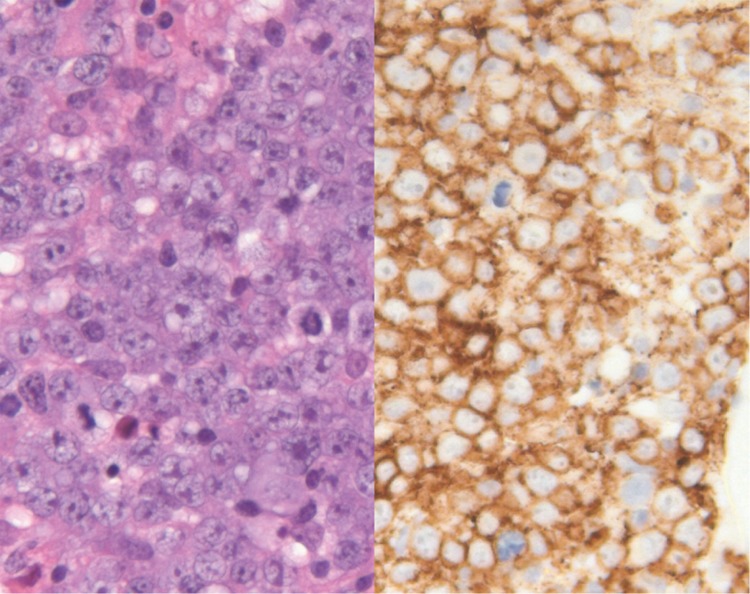
Histopathological specimen of tumour. Left slide shows cellular tumour with large vesicular nuclei, prominent nucleoli and mitotic figures (H&E ×400). Right slide shows positive (brown) membrane staining of the tumour cells with an antibody to CD20 (B lymphocyte marker) (×400)
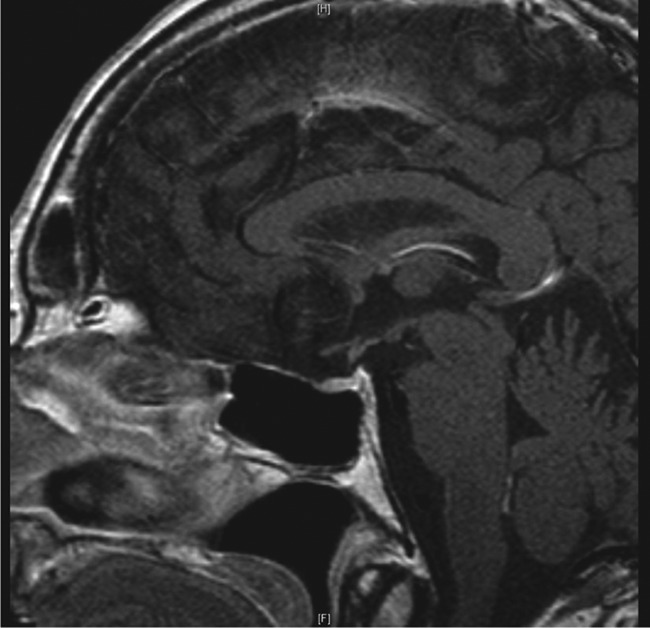
Figure 3.
Magnetic resonance imaging post-treatment
Discussion
Primary pituitary lymphoma (PPL) is a rare tumour of the pituitary gland, although as discussed is now diagnosed more frequently. The exact cause is unknown but several hypotheses have been suggested. These include a possible infectious aetiology, perhaps due to Epstein–Barr virus or another herpes virus with the transformation of folliculostellate cells (thought to be a form of adult stem cell) into lymphoma cells.1
A literature review was performed to search for other reported cases of primary lymphoma of the pituitary gland. A PubMED search was carried out using the MeSH terms (Pituitary Gland OR Pituitary Disease OR Pituitary neoplasm AND Lymphoma). Cases were excluded if the patient was immunosuppressed, or if the lymphoma was widespread. Autopsy studies were not included. This search yielded a total of 27 other reported cases of primary lymphoma of the pituitary gland (Table 1). The majority of these cases were reported in the last 10 years.
Table 1.
Summary of other reported cases of primary lymphoma of the pituitary
| Author and date | Patient | Cell type | Management | Outcome |
|---|---|---|---|---|
| Li et al. (2012)4 | 41♀ | B-cell | Surgical resection | |
| Carrasco et al. (2010)5 | 49 ♀ | B-cell | Biopsy and chemoradiotherapy | No recurrence at four years |
| Hayasaka et al. (2010)6 | 71 ♂ | B-cell | ||
| Bayraktar et al. (2010)7 | 47 ♀ | B-cell | Endoscopic resection, chemotherapy and stem cell transplantation for recurrence | No recurrence at eight months |
| Fadoukhair et al. (2010)8 | 26 ♀ | B-cell | Stereotactic biopsy and steroids | |
| Moshkin et al. (2009)9 | 62 ♂ | B-cell | Endoscopic biopsy with partial tumor resection only | Not stated |
| Quintero Wolfe et al. (2009)10 | 45 ♀ | B-cell | Sublabial transsphenoidal resection and chemotherapy | No recurrence at three months |
| Kozáková et al. (2008)11 | 60 ♀ | B-cell | Neurosurgical intervention | |
| Romeike et al. (2008)12 | 64 ♀ | T-cell | Trans-sphenoidal surgery and chemoradiotherapy | No recurrence at 19 months |
| Rudnik et al. (2007)13 | 37 ♂ | B-cell | Endoscopic resection, chemoradiotherapy and craniotomy for recurrence | No recurrence at four years |
| Liu et al. (2007)14 | 26 ♂ | Mixed cell | Endoscopic biopsy and chemoradiotherapy | Died six months post op (lymphoma) |
| Huang et al. (2005)15 | 47 ♂ | Mixed cell | Trans-sphenoidal pituitary resection and chemoradiotherapy | No recurrence at five months |
| Capra et al. (2004)16 | 14 ♀ | B-cell | Biopsy through right frontal craniotomy and chemotherapy | No recurrence at 10 months |
| Katz et al. (2003)17 | 64 ♀ | B cell | Craniotomy performed after biopsies | |
| Stephens et al. (2002)18 | 79 ♀ | B-cell | Craniotomy performed after biopsies and radiotherapy | Died soon after treatment |
| Kaufmann et al. (2002)19 | 74 ♂ | B-cell | Trans-sphenoidal pituitary resection and radiotherapy | Died soon after treatment |
| Kaufmann et al. (2002)15 | 65 ♂ | B-cell | Trans-sphenoidal pituitary resection, stereotactic radiosurgery, chemotherapy and bone marrow transplantation for recurrence | Died seven months postsurgery (pulmonary failure) |
| Lee et al. (2002)20 | 42 ♂ | MALT | Endoscopic trans-sphenoidal surgery and chemotherapy | No recurrence after six months |
| Landman et al. (2001)21 | 86 ♀: | B-cell | Trans-sphenoidal resection and chemotherapy | died three months after diagnosis |
| Baleydier et al. (2001)22 | 9 ♂ | B-cell | Diagnosis made on lumbar puncture and treated with chemotherapy | No recurrence at one year |
| Silfen et al. (2001)23 | 11 ♂ | Burkitt cell | Biopsy of the lesion and chemotherapy | No recurrence at 17 months |
| Mathiasen et al. (2000)24 | 65 ♂ | B-cell | Endosopic transnasal transsephenoidal and chemotherapy | |
| Au et al. (2000)25 | 82 ♂ | B-cell | Trans-sphenoidal biopsy and palliative radiotherapy | |
| Kuhn et al. (1999)26 | 67 ♀ | T-cell | Sublabial transsphenoidal resection and radiotherapy | |
| Sakakibara et al. (1998)27 | 53 ♂ | T-cell | Transsphenoidal surgery and radiotherapy | |
| Shaw et al. (1997)28 | 73 ♀ | Mixed cell | Transsphenoidal exploration and radiotherapy | No recurrence at 21 months |
| Samaratunga et al. (1997)29 | 66 ♂ | MALT-cell | Endosopic resection and radiotherapy |
MALT, mucosa-associated lymphoid tissue
The incidence of PPL seems to be similar in both men and women and most commonly affects patients in the sixth decade, although cases from all age groups have been reported. Endocrine dysfunction, headache and visual symptoms such as decreased acuity and bitemporal hemianopia are the most common presenting features and may be associated with other cranial nerve palsies. Endocrine dysfunction appears to occur in roughly 50% of the studies reviewed in this study.4,5,8,11,15–17,19,21,23,24,29 Studies of non-functioning pituitary macroadenomas suggest that pituitary dysfunction is present in more than 30%30 which would correlate well with lymphomas. By far the most common lymphoma subtype reported was B-cell (65%), the other cases were made up of mixed cell, T-cell, Burkitt cell and mucosa-associated lymphoid tissue cell types. The majority of reported cases were treated with radiotherapy, chemotherapy or a combination of the two. It was not possible to estimate survival rates from the literature due to limited follow-up.
Conclusion
Otorhinolaryngologists involved in the treatment of pituitary tumours should be aware of this disease as it is increasing in incidence. It is particularly important to consider the diagnosis in cases that are labelled as inoperable.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written informed consent to publish the article was obtained from the patient or next of kin
Guarantor
HSK
Contributorship
HSK performed the surgery, revised the paper and is guarantor and corresponding author. PR performed a literature search, drafted and revised the paper. AMI drafted, revised and submitted the paper. NC drafted and revised the paper.
Acknowledgements
The authors would like to thank Duncan Cundall-Curry and Manish Powari for their help with the images in this article.
References
- 1.Giustina A, Gola M, Doga M, Rosei E Primary lymphoma of the pituitary; an emerging clinical entity. J Clin Endocrinol Metab 2001;86:4567. [DOI] [PubMed] [Google Scholar]
- 2.Eby NL, Eby NL, Grufferman S, et al. Increasing incidence of primary brain lymphoma in the US. Cancer 1988;62:2461–5 [DOI] [PubMed] [Google Scholar]
- 3.Baumgartner JE Primary central nervous system lymphomas: natural history and response to radiation therapy in 55 patients with acquired immunodeficiency syndrome. J Neurosurg 1990;73:206–11 [DOI] [PubMed] [Google Scholar]
- 4.Li Y, Zhang Y, Xu J, Chen N Primary pituitary lymphoma in an immunocompromised patient: a rare clinical entity. J Neurol 2012;259:297–305 Epub 2011 20 September [DOI] [PubMed] [Google Scholar]
- 5.Carrasco CA, Rojas-Z D, Chiorino R, González G Primary pituitary lymphoma in immunocompetent patient: diagnostic problems and prolonged follow-up. Pituitary 2010;10 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Hayasaka K, Koyama M, Yamashita T Primary pituitary lymphoma diagnosis by FDG-PET/CT. Clin Nucl Med 2010;35:205. [DOI] [PubMed] [Google Scholar]
- 7.Bayraktar S, Bassini W, Goodman M Primary pituitary lymphoma: idiopathic anascarca with relapse in bone marrow only. Acta Haematol 2010;123:121–5 [DOI] [PubMed] [Google Scholar]
- 8.Fadoukhair Z, Amzerin M, Ismaili N, et al. Symptomatic hypopituitarism revealing primary suprasellar lymphoma. BMC Endocrinol Disord 2010;10:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moshkin O, Muller P, Scheithauer BW, et al. Primary pituitary lymphoma: a histological, immunohistochemical, and ultrastructural study with literature review. Endocrinol Pathol 2009;20:46–9 [DOI] [PubMed] [Google Scholar]
- 10.Quintero Wolfe S, Hood B, Barker J, Benveniste RJ Primary central nervous system lymphoma mimicking pituitary apoplexy: case report. Pituitary 2009;12:76–9 [DOI] [PubMed] [Google Scholar]
- 11.Kozáková D, Macháleková K, Brtko P, Szépe P, Vanuga P, Pura M Primary B-cell pituitary lymphoma of the Burkitt type: case report of the rare clinic entity with typical clinical presentation. Cas Lek Cesk 2008;147:569–73 [PubMed] [Google Scholar]
- 12.Romeike BFM, Joellenbeck B, Stein H, et al. Precursor T-lymphoblastic lymphoma within a recurrent pituitary adenoma. Acta Neurochirurgica 2008;150:833–6 [DOI] [PubMed] [Google Scholar]
- 13.Rudnik A, Larysz D, Blamek S, et al. Primary pituitary lymphoma. Folia Neuropathol 2007;45:144–8 [PubMed] [Google Scholar]
- 14.Liu JK, Sayama C, Chin SS, Couldwell WT Extranodal NK/T-cell lymphoma presenting as a pituitary mass. Case report and review of the literature. J Neurosurg 2007;107:660–5 [DOI] [PubMed] [Google Scholar]
- 15.Huang YY, Lin SF, Dunn P, Wai YY, Hsueh C, Tsai JS Primary pituitary lymphoma presenting as hypophysitis. Endocr J 2005;52:543–9 [DOI] [PubMed] [Google Scholar]
- 16.Capra M, Wherrett D, Weitzman S, Dirks P, Hawkins C, Bouffet E Pituitary stalk thickening and primary central nervous system lymphoma. J Neurooncol 2004;67:227–31 [DOI] [PubMed] [Google Scholar]
- 17.Katz BJ, Jones RE, Digre KB, Warner JE, Moore KR Panhypopituitarism as an initial manifestation of primary central nervous system non-Hodgkin's lymphoma. Endocrinol Pract 2003;9:296–300 [DOI] [PubMed] [Google Scholar]
- 18.Stephens JW, Morganstein DL, McLaughlin JE, Dorwood N, Vanderpump MP Isolated B-cell lymphoma of the pituitary region: a rare clinical entity. Hosp Med 2002;63:306–7 [DOI] [PubMed] [Google Scholar]
- 19.Kaufmann TJ, Lopes MB, Laws ER Jr, Lipper MH Primary sellar lymphoma: radiologic and pathologic findings in two patients. Am J Neuroradiol 2002;23:364–7 [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JH, Lee HK, Choi CT, Huh J Mucosa-associated lymphoid tissue lymphoma of the pituitary gland: MR imaging features. Am J Neuroradiol 2002;23:838–40 [PMC free article] [PubMed] [Google Scholar]
- 21.Landman RE, Wardlaw SL, McConnell RJ, Khandji AG, Bruce JN, Freda PU Pituitary lymphoma presenting as fever of unknown origin. J Clin Endocrinol Metab 2001;86:1470–6 [DOI] [PubMed] [Google Scholar]
- 22.Baleydier F, Galambrun C, Manel AM, Guibaud L, Nicolino M, Bertrand Y Primary lymphoma of the pituitary stalk in an immunocompetent 9-year-old child. Med Pediatr Oncol 2001;36:392–5 [DOI] [PubMed] [Google Scholar]
- 23.Silfen ME, Garvin JH, Hays AP, et al. Primary central nervous system lymphoma in childhood presenting as progressive panhypopituitarism. J Pediatr Hematol Oncol 2001;23:130–3 [DOI] [PubMed] [Google Scholar]
- 24.Mathiasen RA, Jarrahy R, Cha ST, et al. Pituitary lymphoma: a case report and literature review. Pituitary 2000;2:283–7 [DOI] [PubMed] [Google Scholar]
- 25.Au WY, Kwong YL, Shek TW, Leung G, Ooi C Diffuse large cell B-cell lymphoma in a pituitary adenoma: an unusual cause of pituitary apoplexy. Am J Hematol 2000;63:231–2 [DOI] [PubMed] [Google Scholar]
- 26.Kuhn D, Buchfelder M, Brabletz T, Paulus W Intrasellar malignant lymphoma developing within pituitary adenoma. Acta Neuropathol 1999;97:311–6 [DOI] [PubMed] [Google Scholar]
- 27.Sakakibara Y, Matsuzawa M, Taguchi Y, et al. A case of sellar T cell type malignant lymphoma. No Shinkei Geka 1998;26:53–8 [PubMed] [Google Scholar]
- 28.Shaw JA, Strachan FM, Sawers HA, Bevan JS Non-Hodgkin lymphoma with panhypopituitarism, hyperprolactinaemia and sixth nerve palsy. J R Soc Med 1997;90:274–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Samaratunga H, Perry-Keene D, Apel RL Primary lymphoma of pituitary gland: a neoplasm of acquired malt? Endocrinol Pathol 1997;8:335–41 [DOI] [PubMed] [Google Scholar]
- 30.Ezzat S, Asa SL, Couldwell WT, et al. The prevalence of pituitary adenomas: a systematic review. Cancer 2004;101:613–9 [DOI] [PubMed] [Google Scholar]