Abstract
Inflammation is a hallmark of stroke pathology. The cytokines, tumor necrosis factor (TNF), interleukin (IL)-1, and IL-6, modulate tissue injury in experimental stroke and are therefore potential targets in future stroke therapy. The effect of these cytokines on infarct evolution depends on their availability in the ischemic penumbra in the early phase after stroke onset, corresponding to the therapeutic window (<4.5 hours), which is similar in human and experimental stroke. This review summarizes a large body of literature on the spatiotemporal and cellular production of TNF, IL-1, and IL-6, focusing on the early phase in experimental and human stroke. We also review studies of cytokines in blood and cerebrospinal fluid in stroke. Tumor necrosis factor and IL-1 are upregulated early in peri-infarct microglia. Newer literature suggests that IL-6 is produced by microglia, in addition to neurons. Tumor necrosis factor- and IL-1-producing macrophages infiltrate the infarct and peri-infarct with a delay. This information is discussed in the context of suggestions that neuronal sensitivity to ischemia may be modulated by cytokines. The fact that TNF and IL-1, and suppossedly also IL-6, are produced by microglia within the therapeutic window place these cells centrally in potential future stroke therapy.
Keywords: focal cerebral ischemia, interleukin-1, interleukin-6, penumbra, therapeutic window, tumor necrosis factor
Introduction
Tumor necrosis factor (TNF), interleukin (IL)-1, and IL-6 are potent, inflammatory cytokines, and potential targets in future stroke therapy. All three cytokines are able to modulate the size of the ischemic damage in experimental stroke (focal cerebral ischemia) in rodents, and their levels increase in cerebrospinal fluid (CSF) and blood after ischemic stroke in humans (Allan et al, 2005; Simi et al, 2007; McCoy and Tansey, 2008; Whiteley et al, 2009). There is evidence that TNF and IL-1 in the stroke-lesioned rodent brain are produced by resident microglia, intrathecal macrophages, and infiltrating, monocyte-derived macrophages (Buttini et al, 1994; Davies et al, 1999; Lambertsen et al, 2005; Clausen et al, 2008), whereas IL-6 in addition is produced by neurons (Suzuki et al, 1999, 2009). Although TNF, IL-1, and IL-6 are also among the best investigated cytokines in CSF and blood in human stroke patients, we still know very little about their availability and mechanism of action in human brain in the early phase, up till 4 to 6 hours, after induction of experimental stroke, corresponding to the therapeutic window in human stroke (Ginsberg, 2008). Before considering if and how to target these cytokines in patients with stroke, a minimal requirement therefore is to know the availability, including the cellular production, of these cytokines in the ischemic territory in the early phase after stroke onset in rodents and ideally also in the human brain.
The finding that TNF, IL-1, and IL-6 increase many-fold (up to 40- to 60-fold) in the brain within the first 24 hours after experimental stroke (Hill et al, 1999; Lambertsen et al, 2005; Clausen et al, 2005, 2008) has contributed to the view that their effects on infarct evolution critically depend on a pronounced, many-fold increase in cytokine levels in the ischemic territory. However, as will be discussed in this review, the time profile for the evolution of the infarct does not match the increases in cytokine messenger RNA (mRNA) and protein productions, if these many-fold increases in cytokine levels should determine the evolution of the infarct. In the case of permanent (ischemic) strokes, the infarct has accordingly almost attained its final volume several hours before the cytokine production reaches its maximum. However, TNF, IL-1, and IL-6 are extremely potent molecules and along with their pro-forms they are present in low pg/mg protein levels also in normal brain parenchyma in both humans and rodents (Breder et al, 1993; Gahring et al, 1996; Hillhouse et al, 1998; Gregersen et al, 2000; Vitkovic et al, 2000; Lambertsen et al, 2002, 2005; Clausen et al, 2005). Further, evidence is accumulating that glutamate, which is released into the synaptic cleft in the first minutes after stroke onset (Dirnagl et al, 1999), can increase the sensitivity of primarily neurons to cytokines (Cardenas et al, 2002; Pradillo et al, 2005; Gardoni et al, 2011). Knowing the cellular production of TNF, IL-1, and IL-6 in normal brain, and knowing the time profile and the cellular sources of these cytokines within, and the possibilities of their transport into the ischemic territory, in the early phase after stroke onset is crucial to understand the mechanisms by which these cytokines interact with the potentially salvageable neurons in the ischemic ‘penumbra'. The purpose of this review is to clarify the association between the in situ production and total availability of TNF, IL-1, and IL-6 and the evolution of the infarct in experimental stroke in the rodent, and to clarify the association between TNF, IL-1, and IL-6 in CSF and blood, and stroke severity, infarct size, and clinical outcome in human stroke. Based on the evidence that TNF, IL-1, and in part also IL-6 are microglial derived, at the time of and in the early phase after stroke, we finally discuss the role of microglial-derived cytokines in determining the fate of the potentially salvageable neurons in the ischemic ‘penumbra' and point to future research questions/hypotheses.
Infarct Evolution and Therapeutic Window in Experimental and Human Stroke
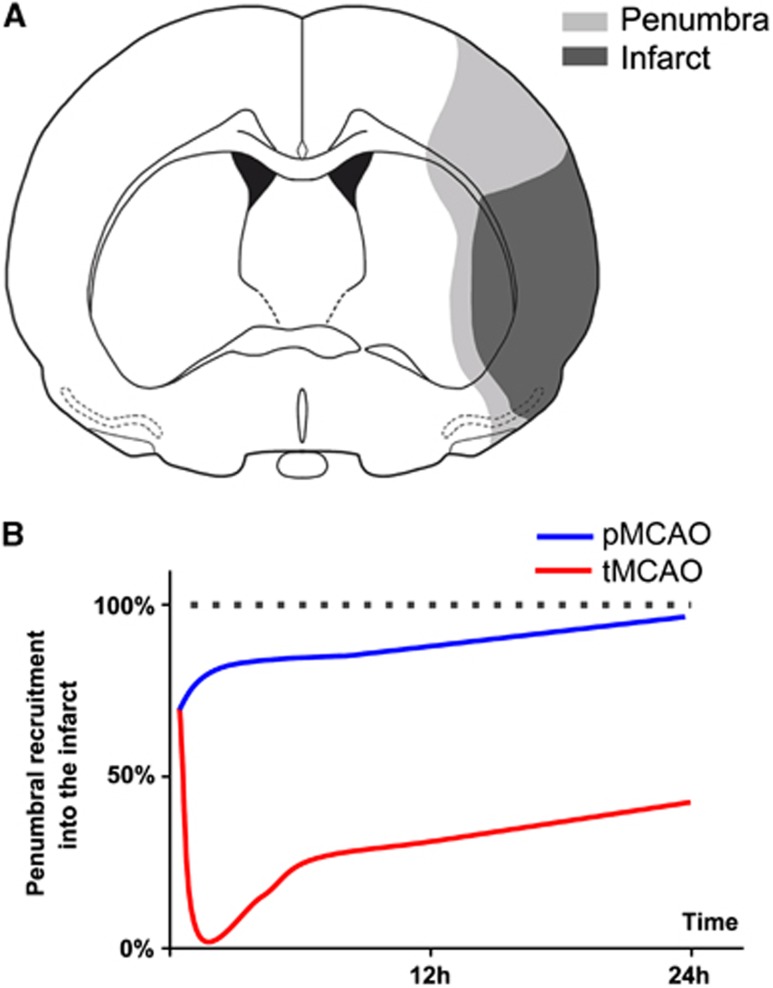
The ‘penumbra' is originally defined as the tissue immediately surrounding the infarct core in which there is reduced blood flow, impaired neuronal functionality, but preserved structural integrity, but which can be recruited into the developing infarct (Astrup et al, 1981), if therapeutic strategies that counteract, inhibit or block deleterius events fail (Ginsberg, 2008). According to the original definition, which is based on studies in the rat, the penumbra is a highly dynamic region, which temporarily may expand, but nevertheless regresses in conjunction with the maturation of the infarct (Figures 1A and 1B). As the penumbra can, in principle, only be visualized by in vivo imaging techniques, although its exact identification in brain sections using histologic techniques are impossible, we will in this review only use the term ‘penumbra', when a ‘context-related' definition of the penumbra is provided. Otherwise, we will use the broader term ‘peri-infarct', which in addition to the penumbra comprises the tissue further away from the developing infarct (Sommer, 2010), tissue which is affected by the stroke, but unlikely to die and to be recruited into the infarct. The ‘ischemic territory' consists of both the infarct and peri-infarct.
Figure 1.
Dynamics of the recruitment of the penumbra into the infarct in experimental stroke. (A) Schematic presentation of the penumbra and infarct early within the acute phase, when the penumbra may still be recruited into the infarct, if the ischemic process is not counteracted by, e.g., reperfusion or neuroprotective intervention. The penumbra is given as the mismatch between the area of reduced protein synthesis and the area of reduced ATP levels exactly 1 hour after proximal middle cerebral artery occlusion (MCAO) in a C57Bl/6 mouse, and is drawn from coronal brain sections shown in Figure 1 in Hata et al (2000b). (B) Graphic presentation illustrating the difference in the recruitment of the penumbra into the infarct after transient MCAO (tMCAO) and permanent MCAO (pMCAO) in the mouse. The dotted line represents the total infarct volume. The vertical distance between the dotted line, and the blue and red line, respectively, represents the size of the penumbra after pMCAO and tMCAO. At 24 hours, the penumbra has been completely recruited into the infarct after pMCAO, but not after tMCAO, in which case the penumbra initially expands due to the reperfusion, whereafter it gradually regresses. As above, the penumbra is defined as the percent mismatch between the area of reduced protein synthesis and the area of reduced ATP levels, starting 1 hour after MCAO, at which time the penumbra is similar in tMCAO and pMCAO. The graph is reconstructed from data in Hata et al (2000a, 2000b).
Infarct Evolution in Experimental Stroke
The most commonly used stroke models are the models of permanent and transient middle cerebral artery occlusion (MCAO) in the rodent, which mirror thrombo-embolic occlusion of the middle cerebral artery in humans. Transient MCAO (tMCAO) mirrors occlusion of the middle cerebral artery followed by reperfusion, which can be either spontaneous or assisted, as when reperfusion is achieved after successful recanalization therapy in patients. Both stroke models are highly invasive, and may or may not involve craniectomy, which should be taken into consideration when evaluating cytokine responses to the stroke. The largest difference between models is, however, the difference between permanent MCAO (pMCAO) and tMCAO (Hossmann, 2012). Although reperfusion attenuates infarction if instituted rapidly after arterial occlusion, it provides fast access for leukocytes into the infarct core and penumbra, which raises questions about the potential additional contribution of leukocyte-derived cytokines in modulating infarct evolution.
Several groups have worked on bridging the gap between the penumbra as originally defined by the use of in vivo imaging techniques and flow studies, and molecular definitions of the penumbra in tissue sections (Hossmann, 1996, 2012; Back et al, 2004; Sharp et al, 2011; Hoehn et al, 2001; Weinstein et al, 2004; Ginsberg, 2008). There is consensus that what corresponds best to the penumbra at the molecular level is (1) areas of suppressed protein synthesis but preserved ATP content, and (2) areas of heat shock protein 70 induction in neurons (Hossmann, 1996; del Zoppo et al, 2011). By recording the area of reduced protein synthesis and the area of reduced ATP levels in parallel sections from the same mice, the Hossmann group, in a series of elegant experiments, showed that the dynamics of the penumbra—defined as the area of suppressed cortical protein synthesis but preserved ATP—was different after pMCAO and tMCAO (Hata et al, 2000a, 2000b; Hossmann, 2012). After pMCAO, this area rapidly regressed from close to 30% of the final infarct volume after 1 hour of ischemia to ∼18% at 6 hours, and to 5% after 24 hours of ischemia, when the edge of the area of reduced protein synthesis and ATP depletion exactly matched the borders of the histologically defined infarct (Figures 1A and 1B; Hata et al, 2000a). In comparison, after 60 minutes of tMCAO, the penumbra initially increased, as a result of the reperfusion, whereafter it was gradually recruited into the infarct, to eventually regress to a few percent of the final infarct volume 3 days after tMCAO (Figure 1B; Hata et al, 2000b).
Taken together, this suggests that the penumbra is smaller and recruited more rapidly into the infarct after pMCAO than after tMCAO (Figure 1B; Hata et al, 2000a, 2000b). This is in line with other studies in rodents, including high-resolution magnetic resonance imaging-based studies, showing that the recruitment of the potentially salvageable penumbral tissue into the infarct happens most rapidly in the early phase after stroke (Hoehn et al, 2001; Weinstein et al, 2004; Liu et al, 2010). In a recent opinion paper (Hossmann, 2012), it was emphasized that pMCAO and tMCAO have different pathophysiologies, where the condition induced by pMCAO reflects the situation in patients with stroke, who do not qualify for recanalization therapy, and who constitute the majority of stroke patients. The tMCAO model allows us to study stroke pathophysiology under the best possible conditions for successful therapeutic intervention, corresponding to patients with stroke that either show spontaneous reperfusion or are successfully treated with recanalization treatment within 1 hour after stroke onset, which is a small minority of patients (Hossmann, 2012).
Interestingly, it has emerged that also the injury within the infarct core develops in a more dynamic way than the imaging studies originally suggested. This has lead to the concept of the infarct core as consisting of ‘multiple mini-cores' associated with multiple ‘mini-penumbras', which over time coalesce to form a solid infarct (del Zoppo et al, 2011), a pattern which is also depicted in stainings for neuronal heat shock protein 70 production and microglial activation (Lehrmann et al, 1997; Lambertsen et al, 2005; Hughes et al, 2010).
Infarct Evolution and Therapeutic Window in Human Stroke
As outlined above, the concept of the penumbra being tissue at risk that is potentially salvageable and therefore the target in stroke therapy has been developed in rodents under controlled conditions and invasive methods. The transfer of this concept, however, to the clinical situation with human stroke patients using modern imaging techniques has proven to be extremely challenging (Heiss and Sobesky, 2008). Positron emission tomography using ligands (e.g., 11C-flumazenil) that allow the discrimination between tissue with and without morphologic destruction or measurements of oxygen supply and blood flow are still the golden standards to identify potentially salvageable brain tissue (Heiss and Sobesky, 2008). Positron emission tomography studies have severe limitations due to invasion and radiation exposure for the patients and require such complex logistics that this technique is available only in few specialized centers. The magnetic resonance imaging-based method that determines the ‘mismatch' between perfusion-weighted and diffusion-weighted images (PWI–DWI mismatch) is the only widely used possibility to determine penumbral tissue in stroke patients (Back et al, 2004; Rivers et al, 2006; Heiss and Sobesky, 2008; Liu et al, 2010). Using this method, it was shown in 14 patients who underwent serial imaging analysis from ∼7 hours to until 42 days after stroke that also in humans the lesion size increases rapidly (<70 hours) to its maximal size (Schwamm et al, 1998). Thus, similar to the situation in mice and rats, the recruitment of penumbral tissue into the infarct is a rapid process also in humans, which thereby underscores the significance of the ‘time is brain' concept (Ginsberg, 2008; Lo, 2008). At the moment, the only approved pharmacological therapy for ischemic stroke is the recanalization of the occluded artery by intravenous (i.v.) administration of recombinant tissue plasminogen activator, allowing reperfusion and thereby access of blood-borne leukocytes and cytokines into the ischemic territory. Because of the limited time window (<4 to 6 hours after stroke) and several severe risk factors, such as hemorrhage, this therapy is only applied in <10% of all stroke patients (Huang et al, 2006), thereby emphasizing the need for additional neuroprotective strategies. Furthermore, it appears that early inflammatory events may be required for recovery at later time points (Lo, 2008), so inhibiting or blocking cytokine responses might interfere with tissue recovery.
Infarct Modifying Effect of Early Stroke Cytokines
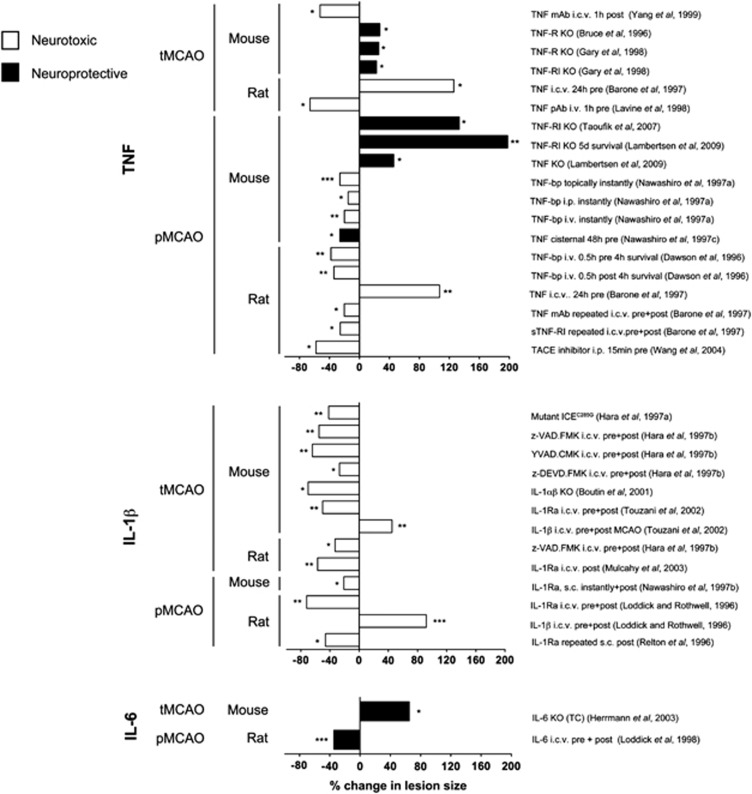
TNF is probably the most extensively studied cytokine in experimental stroke. Tumor necrosis factor can both exacerbate and counteract infarct evolution in rodents (Figure 2 and Table 1A). Tumor necrosis factor exists in a transmembrane and a soluble form, which both signal through surface membrane receptors TNF-RI (TNF-p55R) and TNF-RII (TNF-p75R; Kriegler et al, 1988). In experimental stroke, administration of neutralizing antibodies to TNF or of TNF-binding protein (TNF-bp, soluble (s) TNF-RI, sTNF-p55R) has protective effects (Figure 2 and Table 1A). Although the results of intervention studies thereby indicate a pathologic role of TNF, studies of TNF-deficient mice suggest that TNF is neuroprotective (Bruce et al, 1996; Gary et al, 1998; Taoufik et al, 2007; Lambertsen et al, 2009), an effect which appears to be mediated via TNF-RI (Figure 2 and Table 1A). Importantly, these observations corroborate the idea that the evolution of the infarct and, thus, the survival of ischemic neurons is modulated by the TNF, which is already present in the neural tissue at stroke onset.
Figure 2.
Effect of therapeutic or genetic manipulation of tumor necrosis factor (TNF), interleukin (IL)-1β, or IL-6 bioavailability on infarct size in experimental stroke. Graphic presentation of studies showing a neuroprotective (black) or neurotoxic (white) effect of therapeutic intervention or genetic manipulation of TNF, IL-1β, or IL-6 or their receptors in rodents after transient MCAO (tMCAO) or permanent MCAO (pMCAO). Data are presented as the percent difference in total infarct volume between the experimental and the control group, giving rise to an increase (bars directed to the right) or a decrease (bars directed to the left) in lesion size. Unless stated data were obtained from studies using 24-hour post-surgery survival. Further details on doses and experimental settings are given in Tables 1A, 1B, 1C. bp, binding protein; i.c.v., intracerebroventricular; i.p., intraperitoneal; i.v., intravenous; KO, knock out; mAb, monoclonal antibody; pAb, polyclonal antibody. *P<0.05, **P<0.01, ***P<0.001.
Table 1A. Studies on the neuroprotective or neurotoxic effect of TNF in experimental stroke.
| Ischemia model | Strain | Intervention | Results | Effect of TNF | Reference |
|---|---|---|---|---|---|
| Mouse | |||||
| Distal pMCAO (electrocoagulation) | BALB/c | Intracisternal injection of 0.5 μg TNF 48 hours before occlusion | Intracisternal administration decreased infarct volume | Neuroprotective | Nawashiro et al (1997c) |
| Distal pMCAO (electrocoagulation) | BALB/c | i.p. or i.v. injection of 3 mg/kg TNF-bp immediately after occlusion | TNF-bp decreased infarct volume in a dose-dependent manner in all experiments | Neurotoxic | Nawashiro et al (1997a) |
| Distal pMCAO (electrocoagulation) | BALB/c | Topic administration of 3 mg/kg TNF-bp immediately and 1 hour after occlusion | TNF-bp decreased infarct volume at 1 hour, 24 hours and 2 weeks | Neurotoxic | Nawashiro et al (1997b) |
| Distal pMCAO (electrocoagulation) | TNF-KO, C57BL/6, B6129 TNF-RI-KO, TNF-RII-KO, TNF-RI/RII-KO, C57x129 TNF-KO → TNF-KO TNF-KO → C57BL/6 C57BL/6 → TNF-KO C57BL/6 → C57BL/6 | — | TNF-KO displayed larger infarcts compared with C57BL/6 and B6129 at 24 hours and 5 days TNF-RI-KO displayed larger infarcts compared with TNF-RII-KO, TNFRI/RII-KO, and C57x129 TNF-KO → TNF-KO and C57BL/6 → TNF-KO displayed larger infarcts compared with TNF-KO → C57BL/6 and C57BL/6 → C57BL/6 | Neuroprotective | Lambertsen et al (2009) |
| Distal pMCAO (electrocoagulation) | TNF-RI-KO C57BL/6 | — | TNF-RI-KO displayed larger infarcts compared with control at 24 hours, but not at 3 and 6 hours | Neuroprotective | Taoufik et al (2007) |
| Distal tMCAO (1 hour, filament) | TNF-RI/RII-KO, C57BL/6(B6), B6x129F | — | TNF-RI/RII-KO displayed larger infarcts compared with C57BL/6 and B6x129F | Neuroprotective | Bruce et al (1996) |
| Distal tMCAO (1 hour, filament) | TNF-RI-KO, TNF-RII-KO, TNF-RI/RII-KO, C57BL/6 | — | TNF-RI-KO and TNF-RI/RII-KO mice display larger infarcts compared with TNF-RII-KO and C57BL/6 | Neuroprotective | Gary et al (1998) |
| Distal tMCAO (1 hour, filament) | CD-1 | i.c.v. injection of 300 μg/kg anti-TNF-Ab 1 hour after occlusion | Anti-TNF-Ab decreased infarct volume | Neurotoxic | Yang et al (1998, 1999) |
| Rat | |||||
| Distal tMCAO (80 and 160 minutes) | SHR | 2.5 pmol TNF pre-treatment 24 hours before occlusion | TNF increased infarct volume | Neurotoxic | Barone et al (1997) |
| Distal pMCAO (occluded and cut) | SHR | 2.5 and 25 pmol TNF pre-treatment 24 hours before occlusion 10 μg TNF mAb or 12.5 μg sTNF-RI, 30 minutes before and 3 and 6 hours after occlusion | TNF increased infarct volumes in a dose-related manner. This was reversed by injection of 60 pmol TNF mAb TNF mAb and sTNF-RI reduced infarct volumes | Neurotoxic | Barone et al (1997) |
| Distal pMCAO (thromboembolic) | SD | 30 mg/kg TACE-inhibitor (DHP-067517), 15 minutes before and 6 hours after occlusion | TACE-inhibitor decreased infarct volume | Neurotoxic | Wang et al (1994) |
| Proximal tMCAO (1 hour, filament) | SD | i.v. injection of 0.36 mg/kg anti-TNF Ab 1 hour before occlusion | Anti-TNF-Ab reduced infarct volume | Neurotoxic | Lavine et al (1998) |
| Distal pMCAO (electrocoagulation) | SHR | i.v. injection of 1 mg/kg TNF-bp 30 minutes pre- or post- occlusion | TNF-bp reduced infarct volumes | Neurotoxic | Dawson et al (1996) |
Ab, antibody; i.c.v., intracerebroventricular; i.p., intraperitoneal; i.v., intravenous; KO, knock out; pMCAO, permanent middle cerebral artery occlusion; rh, recombinant human; s.c., subcutaneous; SD, sprague dawley; SHR, spontaneously hypertensive rats; tMCAO, transient middle cerebral artery occlusion; TNF, tumor necrosis factor; TNF-bp, TNF-binding protein; TNF-RI, TNF receptor I; TNF-RII, TNF receptor II; WT LM, wild-type littermates.
Unlike TNF, IL-1 has a clearly defined pathologic effect (Figure 2 and Table 1B). Interleukin-1 occurs in two forms, IL-1α and IL-1β, of which IL-1β, which is a secreted protein, is the one that is best investigated in experimental stroke (Allan et al, 2005). Both forms of IL-1 signal through the IL-1 receptor type I (IL-1RI), an effect, which is competitively blocked by the naturally occurring IL-1 receptor antagonist (IL-1Ra; Dinarello, 1994). Several independent studies have shown that administration of recombinant human IL-1Ra (rhIL-1Ra), neutralizing antibodies against IL-1 (Yamasaki et al, 1995; Loddick and Rothwell, 1996; Boutin et al, 2001; Touzani et al, 2002) or therapeutic inhibition of IL-1-converting enzyme (or caspase-1), which cleaves pro-IL-1β into the secreted bioactive IL-1β (Dinarello, 1994; Schielke et al, 1998), results in large decreases in infarct volume (up to 60% to 70%) after MCAO in mice and rats (Figure 2 and Table 1B). Similarly, mice deficient in IL-1 or in IL-1-converting enzyme show large decreases in infarct size, whereas intracerebroventricular (i.c.v.) injection of IL-1β increases infarct size (Figure 2 and Table 1B). In combination, these studies have paved the way for safety trials of treatment with rhIL-1Ra (Anakinra (Kineret)) in stroke patients (Emsley et al, 2005). Ongoing pharmacokinetic studies show that experimentally effective concentrations of rhIL-1Ra (Anakinra) given within the therapeutic window can be achieved in stroke patients (Galea et al, 2011).
Table 1B. Studies on the neuroprotective or neurotoxic effect of IL-1β in experimental stroke.
| Ischemia model | Strain | Intervention | Results | Effect of IL-1β | Reference |
|---|---|---|---|---|---|
| Mouse | |||||
| Distal pMCAO (electrocoagulation) | BALB/c | s.c. injection of 100 mg/kg IL-1Ra, immediately and 4 hours after surgery | IL-1Ra decreased infarct volume | Neurotoxic | Nawashiro et al (1997b) |
| Proximal tMCAO (30 minutes, filament) | IL-1β-KO IL-1α-KO IL-1αβ-KO C57BL/6 | i.c.v. injection of rhIL-1Ra 30 minutes before surgery and 40 minutes after tMCAO | IL-1αβ-KO mice displayed smaller infarct volumes than C57BL/6 No change in IL-1β-KO or IL-1α-KO rhIL-1Ra reduced infarct volume in C57BL/6 and IL-1α-KO mice but not in IL-1β-KO or IL-1αβ-KO mice | Neurotoxic | Boutin et al (2001) |
| Proximal tMCAO (2 hours, filament) | SV-129 | i.c.v. injection of ICE-like protease inhibitors (2 × 40 or 2 × 120 ng z-VAD.FMK, 2 × 200 ng YVAD.CMK, 2 × 120 ng z-DEVD.FMK) 15 minutes before surgery and again immediately after reperfusion or 45 minutes before surgery and again immediately after reperfusion | ICE-like protease inhibitors reduced infarct volumes | Neurotoxic | Hara et al (1997b) |
| Proximal tMCAO (3 hours, filament) | ICE-KO | — | ICE-KO mice displayed smaller infarct volumes than control mice | Neurotoxic | Hara et al (1997a) |
| Proximal tMCAO (30 minutes, filament) | IL-1RI-KO C57xSV129 | i.c.v. injection of 2 × 2.5 μg rhIL-1Ra and 2 × 2.5 ng IL-1β, respectively, 10 minutes before and 40 minutes after occlusion | rhIL-1Ra reduced infarct volume in C57xSV129 mice and IL-1β increased infarct volume in IL-1RI-KO and C57xSV129 mice | Neurotoxic | Touzani et al (2002) |
| Proximal tMCAO (1 hour, filament) | IL-1αβ-KO WT LM | — | IL-1αβ-KO mice displayed smaller infarct volumes than C57BL/6 | Neurotoxic | Ohtaki et al (2003) |
| Rat | |||||
| Proximal pMCAO (electrocoagulation) | SD | i.c.v. injection of 2 to 10 μg rhIL-1Ra (30 minutes before, at the time of pMCAO, and 30 minutes after pMCAO) and 2 × 2.5 ng IL-1β (30 minutes and 2 hours after pMCAO) | IL-1β treatment increased infarct volumes and body temperatures, whereas IL-1Ra treatment significantly reduced infarct volumes | Neurotoxic | Loddick and Rothwell (1996) |
| Proximal pMCAO (filament) | Wistar | i.v. injection of rhIL-1Ra at the time of occlusion followed by 3 s.c. injections during the first 24 hours after surgery | rhIL-1Ra-treated rats displayed improved neurological score and had fewer necrotic neurons and fewer leukocytes in the ischemic territory | Neurotoxic | Garcia et al (1995) |
| Proximal pMCAO (electrocoagulation) | SD | s.c. injection of 5 × 100 mg/kg rhIL-1Ra (0, 4, 8, 12, and 18 hours after pMCAO) | IL-1Ra reduced infarct volume | Neurotoxic | Relton et al (1996) |
| Proximal tMCAO (2 hours, filament) | SD | i.c.v. injection of ICE-like protease inhibitors (2 × 27 ng or 2 × 80 ng z-VAD.FMK) 15 minutes before surgery and again 10 minutes after reperfusion | ICE-like protease inhibitors reduced infarct volume | Neurotoxic | Hara et al (1997b) |
| Proximal tMCAO (1 hour, filament) | Wistar | i.c.v. injection of 10 mg rhIL-1β and 10 μg anti-IL-1β neutralizing Ab immediately after reperfusion | rhIL-1β administration increased brain edema formation and infarct size, whereas i.c.v. administration of anti-IL-1β attenuated the increase in brain water content and decreased infarct size | Neurotoxic | Yamasaki et al (1995) |
| Proximal tMCAO (1 hour, filament) | SD | i.c.v. injection of 2 × 10 μg rhIL-1Ra immediately after occlusion and again at the time of reperfusion | rhIL-1Ra-treated rats displayed decreased infarct volumes at 24 and 48 hours | Neurotoxic | Mulcahy et al (2003) |
Ab, antibody; ICE, interleukin-1β-converting enzyme; i.c.v., intracerebroventricular; IL, interleukin; IL-1RI, IL-1 receptor I; i.v., intravenous; KO, knock out; pMCAO, permanent middle cerebral artery occlusion; rh, recombinant human; s.c., subcutaneous; SD, sprague dawley; SHR, spontaneously hypertensive rats; tMCAO, transient middle cerebral artery occlusion; WT LM, wild-type littermates.
There are only few reports on the role of IL-6 in experimental stroke (Figure 2 and Table 1C). However, although i.c.v. injection of rhIL-6 reduces infarct size in rats and gerbils (Matsuda et al, 1996; Loddick et al, 1998), initial studies on IL-6-deficient mice suggested that IL-6 has no impact on infarct evolution after neither severe nor mild tMCAO (Clark et al, 2000). This lack of effect on infarct size, however, was most likely due to hypothermia in IL-6-deficient mice as a later study showed increased infarct size and reduced survival in IL-6-deficient mice when controlled for hypothermia (Figure 2 and Table 1C). These results suggest that IL-6 is neuroprotective, as also shown in in vitro studies (Biber et al, 2008), and that infarct evolution is modulated by the IL-6 present in the neural tissue at stroke onset, as is the case for TNF.
Table 1C. Studies of neurotoxic and neuroprotective effects of IL-6 in experimental stroke.
| Ischemia model | Strain | Intervention | Results | Effect of IL-6 | Reference |
|---|---|---|---|---|---|
| Mouse | |||||
| Proximal tMCAO (45 minutes, 2 hours, filament) | IL-6-KO IL-6+/− WT LM | — | IL-6 deficiency had no effect on infarct volume | No effect | Clark et al (2000) |
| Proximal tMCAO (1 hour, filament) | IL-6-KO C57BL/6 | — | IL-6-KO mice had increased infarcts when body temperature was controlled to C57BL/6 levels | Neuroprotective | Herrmann et al (2003) |
| Rat | |||||
| Proximal pMCAO (electrocoagulation) | SD | i.c.v. injection of 2 × 50 or 2 × 500 ng rhIL-6 30 minutes before and again 15 minutes after pMCAO | rhIL-6 reduced infarct volumes | Neuroprotective | Loddick et al (1998) |
i.c.v., intracerebroventricular; IL-6, interleukin-6; KO, knock out; pMCAO, permanent middle cerebral artery occlusion; rh, recombinant human; SD, sprague dawley; tMCAO, transient middle cerebral artery occlusion; WT LM, wild-type littermates.
Cytokines in Experimental Stroke
As mentioned in the introduction, TNF, IL-1, and IL-6 are extremely potent molecules and are present, along with their pro-forms and encoding mRNAs, in low levels also in normal brain. This is important, especially in the case of mRNA level changes, which, when using quantitative PCR analysis, typically are reported as fold-changes compared with baseline. The in situ hybridization technique, which is used to localize the ‘cellular site of' the cytokine mRNA synthesis, and the immunocytochemical technique, which indicates the ‘location' of the actual cytokine, unfortunately often have insufficient sensitivity to detect the baseline expression of cytokines. We have in Tables 2A, 2B, 2C and Figure 3 only included studies in which the cytokine of interest has been detected either using more than one technique and/or using appropriate specificity controls (Saper and Sawchenko, 2003; Lambertsen et al, 2009). Furthermore, if we found that some studies were covered by other studies, these were not included. In addition, a few studies not highlighted in the tables have been included in the text if, e.g., special dissections have been used.
Table 2A. Temporal profile of TNF mRNA and protein in experimental stroke.
| Ischemia model | Strain | Method | Time profile and cellular synthesis | Reference |
|---|---|---|---|---|
| Mouse | ||||
| Proximal tMCAO (1 hour, suture) | BALB/c | RT-PCR | Elevated TNF mRNA from 6 to 48 hours. Peak expression at 24 hours (0.5 hours, and 1 hour during tMCAO and 1, 3, 6, 12, 24, and 48 hours) | Ohtaki et al (2004) |
| Immuno | Cells observed at 1 hour and again from 12 to 48 hours. Expression by MAP2+ and NF200+ neurons, CNP+ oligodendrocytes and F4/80+ microglia/macrophages | |||
| Proximal pMCAO (filament) | C57BL/6 | RPA | Elevated TNF mRNA from 4 to 96 hours. Peak expression at 10 to 18 hours (1, 4, 10, 18, and 96 hours) | Hill et al (1999) |
| Proximal tMCAO (2 hours, filament) | C57BL/6 | RPA | Elevated TNF mRNA from 4 to 96 hours. Peak expression at 10 to 18 hours (1, 4, 10, 18, and 96 hours) | Hill et al (1999) |
| Distal pMCAO (electrocoagulation) | C57BL/6x129 | ISH | Cells observed from 6 to 24 hours. Peak numbers at 12 hours. Expression by GFAP− microglia/macrophage-like cells (6, 12, 24, 48 hours, 5, 10 days) | Gregersen et al (2000) |
| Western blot | Elevated TNF from 2 to 48 hours (2, 12, 48 hours, 5 days) | |||
| Distal pMCAO (electrocoagulation) | C57BL/6x129 BalB/C SJL | ISH | Peak numbers at 12 hours. Expression by GFAP−cells (12, 24 hours) | Lambertsen et al (2002) |
| Immuno | Peak numbers at 24 hours. CD11b+ microglia-macrophages (12, 24 hours) | |||
| Distal pMCAO (electrocoagulation) | BoyJ Chimeric BoyJ | Flow | Cells observed from 6 to 24 hours. Elevated numbers at 12 hours, peak numbers at 24 hours. Expression in TCRβ−, GFAP−, Gr1−, CD11b+CD45+ microglia and macrophages (6, 12, 24 hours) and in control cortex | Clausen et al (2008) |
| Immuno | Expression investigated only at 24 hours. CD11b+ microglia/macrophages | |||
| Distal pMCAO (electrocoagulation) | SJL | Real-time RT-PCR | Elevated TNF mRNA from 4 hours–5 days. Peak expression at 12 hours (30 minutes, 1, 2, 4, 6, 12, 24 hours, 2, 5, 10 days) | Lambertsen et al (2005) |
| ISH | Cells observed from 4 to 24 hours. Peak numbers at 12 hours. Expression in GFAP− microglial-macrophage-like cells | |||
| Immuno | Cells observed from 4 hours–2 days. Peak numbers at 24 hours. Expression in CD11b+ microglial-macrophage-like cells | |||
| Distal pMCAO (electrocoagulation) | C57BL/6 Chimeric C57BL/6 | Real-time RT-PCR | Elevated TNF mRNA from 6 hours. Peak expression at 12 hours (1, 2, 4, 6, 12, and 2 hours) | Lambertsen et al (2009) |
| ISH | Cells observed from 4 hours. NeuN− microglia/macrophage-like cells (4, 6, 12, and 24 hours) | |||
| Immuno | Cells observed at 4–24 hours. Expression in NeuN−, Mac-1+ microglia/macrophages (6, 12, and 24 hours) | |||
| Flow | Cells observed from 6 to 24 hours. Elevated numbers at 24 hours. Expression in TCRβ−, GFAP−, Gr1−, CD11b+CD45dimGFP− microglia and CD11b+CD45highGFP+ macrophages (6, 12, and 24 hours) | |||
| Rat | ||||
| Proximal pMCAO (electrocoagulation) | SHR | ISH | Cells observed from 30 minutes, increased numbers from 3 to 6 hours, reduced numbers from 8 hours–2 days. Microglial/macrophage morphology. Cellular morphology changes from ramified at 3 hours to round at 8 hours (30 minutes, 1, 3, 6, 8 hours, 1, 2, 4, and 6 days) | Buttini et al (1996) |
| RT-PCR | TNF mRNA increased at 30 minutes, peak expression at 3 hours (30 minutes, 1, 3, 6, 8 hours, 1, 2, 4 days) | |||
| Immuno | Cells observed at 30 minutes. Otherwise similar to ISH. Colocalization of GSI-B4+ microglia/macrophages from 6 hours | |||
| Western blot | Increased levels at 3 hours. Peak levels from 8 hours to1 day | |||
| Proximal tMCAO (2 hours, suture) | SD | Real-time RT-PCR | Elevated TNF mRNA from 3 to 24 hours. Peak expression at 6 hours. Leukocyte entry from 6 hours (3, 6, 12, 24, and 72 hours) | Berti et al (2002) |
| Distal tMCAO (160 minutes, occlusion) | SHR | Northern blot | Elevated TNF mRNA from 1 hour. Peak expression at 3 hours (1, 3, 6, 12, 24, 48, and 120 hours) | Wang et al (1994) |
| Proximal pMCAO | SD | mRNA array RT-PCR | Elevated TNF mRNA from 3 hours. Peak expression at 6 hours, decreased at 12 hours, rebound at 3 days (3, 6, 12, 24, 72, and 168 hours) | Kim et al (2002) |
| Proximal pMCAO (occluded and cut) | SHR, WKY, Fisher | Northern blot | Elevated TNF mRNA from 1 hour. Peak expression at 12 hours (1, 3, 6, 12, 24 hours, and 5 days) | Liu et al (1994) |
| Immuno | Cells first observed at 6 hours. Nervefibres observed from 6 to 12 hours and 1 day. Macrophages observed at 5 days | |||
CD, cluster of differentiation; CNP, 2′,3′-cyclic nucleotide-3′-phosphodiesterase; flow, flow cytometry; GFAP, glial fibrillary acidic protein; GFP, green fluorescence protein; GSI-B4, Griffonia simplicifolia isolectin-B4; immuno, immunohistochemistry; ISH, in situ hybridization; MAP2, microtubule-associated protein-2; NF, neurofilament; pMCAO, permanent middle cerebral artery occlusion; RPA, RNAse protection assay; RT-PCR, reverse transcription polymerase chain reaction; SD, sprague dawley; SHR, spontaneously hypertensive rats; tMCAO, transient middle cerebral artery occlusion; TNF, tumor necrosis factor; WKY, Wistar-Kyoto.
Time for tMCAO are time point after reperfusion. Time in parenthesis indicates the time points investigated in the study, except the baseline corresponding to the time ‘0', which is not indicated.
Table 2B. Temporal profile of IL-1β mRNA and protein in experimental stroke.
| Ischemia model | Strain | Method | Time profile and cellular synthesis | Reference |
|---|---|---|---|---|
| Mouse | ||||
| Distal pMCAO (electrocoagulation) | SJL | Real-time RT-PCR | Elevated IL-1β mRNA from 2 to 24 hours. Peak expression at 12 and 24 hours (0.5, 1, 2, 4, 6, 12, 24 hours, and 5 days) | Clausen et al (2005) |
| In situ | Macrophage-like cells observed in cortical layers I/II from 30 hours. Microglial-like cells in ischemic cortex from 2 to 24 hours. Perivascular aggregates at 24 hours (0.5, 1, 2, 4, 6, 12, 24 hours, and 5 days) | |||
| Distal pMCAO (electrocoagulation) | BoyJ Chimeric BoyJ | Flow Immuno | Cells observed from 6 to 24 hours. Elevated numbers at 12 hours, peak numbers at 24 hours. Expression in CD11b+CD45+ microglia/macrophages (6, 12, 24 hours) and in control cortex | Clausen et al (2008) |
| Proximal pMCAO (filament) | C57BL/6 | RPA | Elevated IL-1β mRNA from 10 hours. Peak expression at 18 hours (4, 10, 18, and 96 hours) | Hill et al (1999) |
| Proximal tMCAO (2 hours, filament) | C57BL/6 | RPA | Elevated IL-1β mRNA from 10 hours. Peak expression at 10 hours (4, 10, 18, and 96 hours) | Hill et al (1999) |
| Rat | ||||
| Proximal tMCAO (2 hours, suture) | SD | Real-time RT-PCR | Elevated IL-1β mRNA from 3 to 72 hours. Peak expression at 6 and 24 hours (3, 6, 12, 24, and 72 hours) | Berti et al (2002) |
| Distal pMCAO | SHR | Northern blot | Elevated IL-1β mRNA 1 hour–2 days. Peak expression 6 hours (1, 3, 6, 12, 24 hours and 2, 5 days) | Wang et al (1994) |
| Proximal pMCAO (electrocoagulation) | SD | ISH | Cells with microglial-like nuclei observed from 15 minutes. Peak numbers/expression at 3 hours. High numbers of macrophage-like cells in the meninges at 1 hour (0.25, 1, 3, 6, 18 hours, 2, 5 days) | Buttini et al (1994) |
| Proximal pMCAO (electrocoagulation) | SD | Immuno | Macrophage-like cells observed in meninges from 1 to 2 hours. No such cells observed in sham-operated rats. Microglial-like cells in ischemic cortex from 6 hours (0.5, 1, 2, 6, 24, and 48 hours) | Davies et al (1999) |
| Distal pMCAO (occluded and cut) | SHR F-344, WKY | Northern blot | Elevated IL-1β mRNA from 6 hours. Peak expression at 12 hours (1, 6, 12, 24 hours, and 5 days) | Liu et al (1993) |
| Distal pMCAO (occluded and cut) | SHR | Real-time RT-PCR | Elevated IL-1β mRNA from 6 hours. Peak expression at 6 hours (1, 3, 4, 6, 8, 12, 24 hours, 2, 5 days) | Wang et al (2000) |
CD, cluster of differentiation; F-344, Fisher-344; flow, flow cytometry; IL-1β, interleukin-1β; immuno, immunohistochemistry; ISH, in situ hybridization; pMCAO, permanent middle cerebral artery occlusion; RPA, RNAse protection assay; RT-PCR, reverse transcription polymerase chain reaction; SD, sprague dawley; SHR, spontaneously hypertensive rats; tMCAO, transient middle cerebral artery occlusion; WKY, Wistar-Kyoto.
Time for tMCAO are time point after reperfusion. Time in parenthesis indicate the time points investigated in the study, except the baseline corresponding to the time ‘0', which is not indicated.
Table 2C. Temporal profile of IL-6 mRNA and protein in experimental stroke.
| Ischemia model | Strain | Method | Time profile and cellular synthesis | Reference |
|---|---|---|---|---|
| Mouse | ||||
| Proximal pMCAO (filament) | C57BL/6 | RPA | Elevated IL-6 mRNA from 10 hours. Peak expression at 18 hours (4, 10, 18, and 96 hours) | Hill et al (1999) |
| Proximal tMCAO (2 hours, filament) | C57BL/6 | RPA | Elevated IL-6 mRNA from 10 hours. Peak expression at 18 hours (4, 10, 18, and 96 hours) | Hill et al (1999) |
| Rat | ||||
| Proximal tMCAO (2 hours, suture) | SD | Real-time RT-PCR | Elevated IL-6 mRNA from 3 to 72 hours. Peak expression at 6 hours (3, 6, 12, 24, and 48 hours) | Berti et al (2002) |
| PMCAO (occluded and cut) | SHR | Northern blot | Elevated IL-6 mRNA from 3 hours. Peak expression at 12 hours (1, 3, 6, 12, 24 hours, and 5 days) | Wang et al (1995) |
| Proximal pMCAO Proximal tMCAO (1.5 hours, suture) | SD SD | Bioactivity assay Western blot Immuno | Elevated IL-6 from 2 hours. Peak expression at 24 hours (2, 8, and 24 hours) Elevated at 24 hours. (24 hours) Eleveted IL-6 from 3.5 hours. Peak expression at 12 to 24 hours (3.5, 12, 24, and 48 hours) | (Loddick et al, 1998; Suzuki et al, 1999) |
IL-6, interleukin-6; immuno, immunohistochemistry; pMCAO, permanent middle cerebral artery occlusion; RPA, RNAse protection assay; RT-PCR, reverse transcription polymerase chain reaction; SD, sprague dawley; SHR, spontaneously hypertensive rats; tMCAO, transient middle cerebral artery occlusion.
Time for tMCAO is time point after reperfusion. Time in parenthesis indicate the time-points investigated in the study, except the baseline corresponding to the time ‘0', which is not indicated.
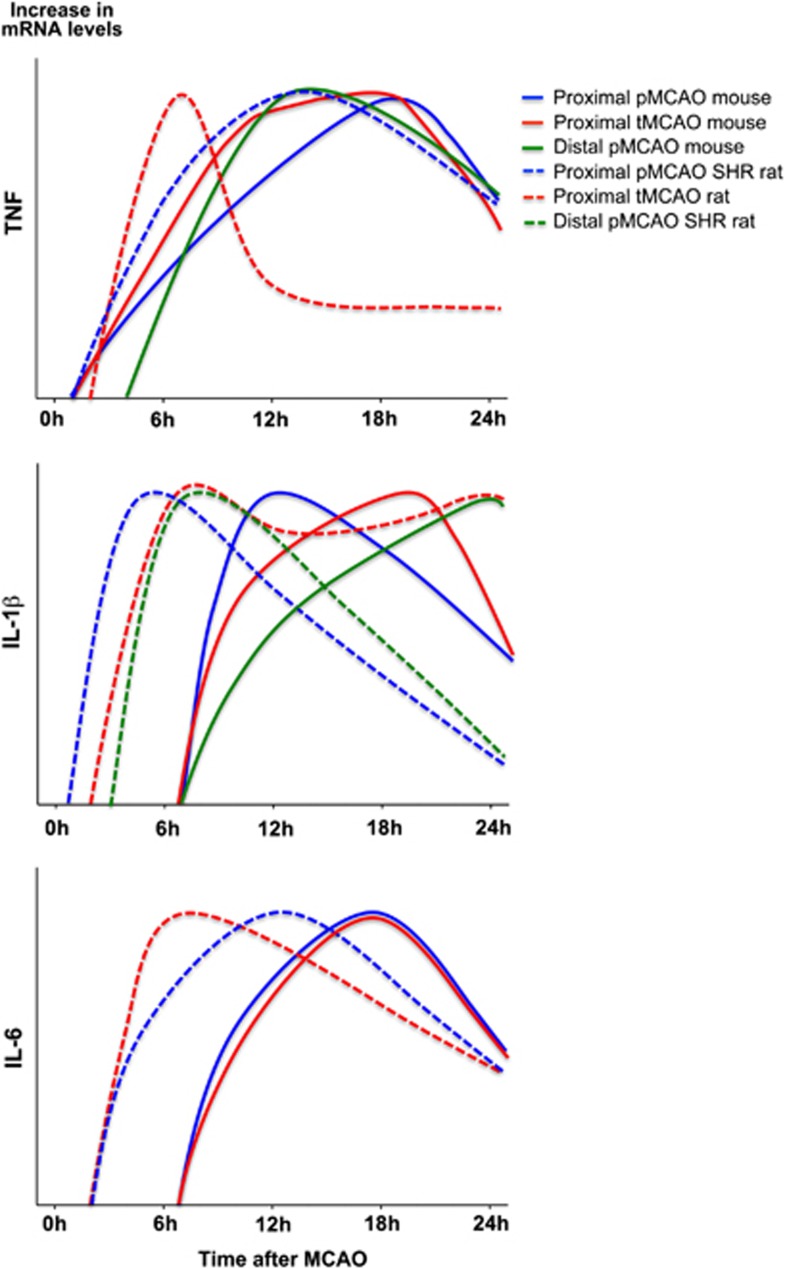
Figure 3.
Temporal cytokine messenger RNA (mRNA) profile in experimental stroke. Graphic presentations of the temporal mRNA profiles of tumor necrosis factor (TNF), interleukin (IL)-1β, and IL-6 mRNA in the acute phase (<4 to 6 hours) and up till 24 hours after permanent MCAO (pMCAO) and transient MCAO (tMCAO) in mice (solid lines) and rats (dotted lines). Data are presented as relative increases in mRNA levels on an abitrary y axis and the peak time of expression after surgery on the x axis. Data for TNF were obtained from: solid blue and red (Hill et al, 1999); solid green (Lambertsen et al, 2009); and dotted blue (Liu et al, 1994) and red (Berti et al, 2002). Data for IL-1β were obtained from: solid blue and red (Hill et al, 1999); solid green (Clausen et al, 2005); dotted blue (Wang et al, 1994); dotted red (Berti et al, 2002); and dotted green (Wang et al, 2000). Data for IL-6 were from: solid blue and red (Hill et al, 1999), dotted blue (Wang et al, 1995); and dotted red (Berti et al, 2002).
Cytokine Synthesis in the Ischemic Territory
TNF is induced in low levels (up till four- to fivefold compared with baseline) within the early phase after stroke onset (<4 to 6 hours), with the earliest increase in mRNA expression observed from 30 minutes to 6 hours after both tMCAO and pMCAO in mice and rats (Figure 3, Table 2A and Supplementary Table 1). In the mouse, increased TNF protein is observed 4 hours after pMCAO, when single TNF immunoreactive cells are detected in the peri-infarct (Table 2A; Lambertsen et al, 2005). This is corroborated by ELISA data reporting on increased TNF in samples of cortex and striatum 1 hour after tMCAO in spontaneously hypertensive rats (Adibhatla and Hatcher, 2007). Peak levels of TNF mRNA and protein are reached from 12 to 24 hours, and TNF remains elevated for days after both tMCAO and pMCAO in the mouse (Figure 3, Table 2A, and Supplementary Table 1). In the rat, however, there is evidence that peak levels of TNF mRNA are reached earlier after tMCAO than after pMCAO (Figure 3; Liu et al, 1994; Wang et al, 1994; Berti et al, 2002), and TNF mRNA remains elevated for hours and days after stroke (Figure 3 and Table 2A). However, interpretations are additionally complicated by the use of different rat strains in different studies (Table 2A). Based on their results, Buttini et al (1996) and Wang et al (1994) suggested that spontaneously hypertensive rats have a TNF time profile different from normotensive rats. This was, however, not supported by findings by Liu et al (1994), who reported on comparable TNF profiles after pMCAO in spontaneously hypertensive rats, Wistar-Kyoto and Fisher-344 rats (Table 2A). Comparable time profiles of TNF production have also been reported for C57BL/6, SJL, BALB/c, and C57x129 mice after pMCAO; however, the magnitude of the TNF response was different (Lambertsen et al, 2002). In all strains, the TNF mRNA+ and TNF+ cells were diffusely distributed in the peri-infarct at both 12 and 24 hours after stroke onset (Table 2A; Lambertsen et al, 2002).
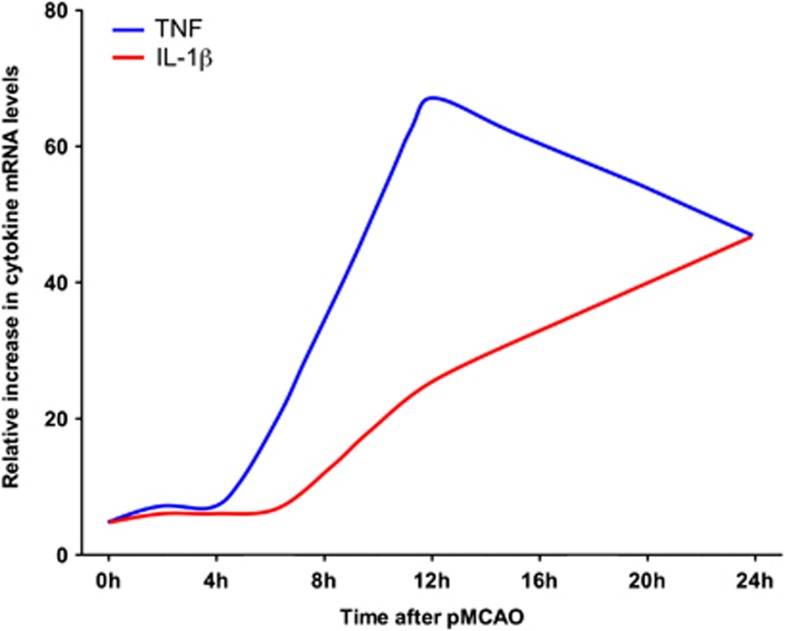
Small increases in IL-1β have been observed as soon as 1 to 2 hours after tMCAO and pMCAO in the rat, where it remains elevated up till 24 hours after tMCAO but not after pMCAO (Figure 3 and Table 2B). The ischemia-induced increase in IL-1β mRNA appears slightly delayed compared with the increase in TNF mRNA after both tMCAO and pMCAO in the mouse (Figures 3 and 4), but continues to increase through 12 and 24 hours after tMCAO and distal pMCAO, to decline toward baseline levels at day 5 (Table 2B and Supplementary Table 1). Very interestingly, in situ hybridization studies performed on tissues from mice and rats after pMCAO (Buttini et al, 1994; Clausen et al, 2005) have detected scattered IL-1β mRNA+ cells in the peri-infarct down to 1 to 2 hours after stroke onset. Of additional interest, the same studies reported on aggregates and perivascular infiltrates of intensely labeled IL-1β mRNA+ cells in the peri-infarct from 12 hours and even more so at 24 hours after the stroke. Both studies also reported on IL-1β mRNA+ macrophage-like cells in the meninges and the superficial cortical layers corresponding to the ischemic territory, during the first post-surgical hour. A similar phenomenon was reported by Davies et al (1999), who, in addition to the IL-1β+ macrophage-like cells in the meninges 1 to 2 hours after pMCAO in the rat, reported on numerous IL-1β+ microglial-like cells in the ischemic territory from 6 to 24 and 48 hours (Table 2B). Although, tempting to speculate that the meningeal infiltration might be ascribed to the craniectomy, which was performed in all three studies, it was specifically reported that IL-1β mRNA+ and IL-1β+ cells were absent from the meninges in the sham-operated animals (Buttini et al, 1994; Davies et al, 1999; Clausen et al, 2005).
Figure 4.
Temporal profile of tumor necrosis factor (TNF) and interleukin (IL)-1β messenger RNA (mRNA) upregulation after permanent MCAO (pMCAO) in mice. Graphic presentation of the temporal mRNA profile of TNF and IL-1β in the same ischemic hemispheres from mice subjected to pMCAO. Data are presented as relative increases in cytokine mRNA levels compared with unmanipulated controls, and have been obtained from Clausen et al (2005) and Lambertsen et al (2009). Note both increase in cytokine levels in the early phase (<4 to 6 hours) after MCAO, and the different profiles of TNF mRNA and IL-1β mRNA expression through 12 and 24 hours after MCAO. Although, only the TNF mRNA level, but not the IL-1β mRNA level, was significantly elevated compared with unmanipulated control and sham-operated mice in the early phase, cells expressing low levels of IL-1β mRNA were observed to be present the ischemic territory from 2 hours after MCAO (Clausen et al, 2005).
There are only few studies on the time profile and cellular production of IL-6 after experimental stroke, and to our knowledge no studies exploring the expression of both mRNA and protein in the same studies. Interleukin-6 mRNA has been shown to be significantly increased as soon as 3 hours and to peak 12 hours after pMCAO in the rat, and remains elevated at 24 hours (Figure 3 and Table 2C).
The striking finding from reviewing the above literature is that the increases in cytokine mRNA and protein levels are at most moderate in the therapeutic window (<4.5 hours; Figures 3 and 4). Even small increases in cytokine levels may, however, have profound effects on infarct evolution if released at the site of the ischemic neurons.
Microglia Produce TNF and IL-1β in the Early Phase and at the Time of MCAO
Studies of the cellular source(s) of TNF in the earliest phase, from minutes to 4 to 6 hours, after MCAO are limited to a few studies (Table 2A), one of them being Buttini et al (1996), who reported on a primarily microglial origin of TNF mRNA 30 minutes after pMCAO in the rat and a mixed microglial-macrophage origin in the later phase (Table 2A). These findings were subsequently reproduced in the mouse, in a series of studies showing a predominantly microglial origin of TNF in the early phase after pMCAO, and a more mixed microglial-macrophage origin from 12 to 24 hours after pMCAO in the mouse (Gregersen et al, 2000; Lambertsen et al, 2002, 2005, 2009; Clausen et al, 2008), although other studies have pointed to an ependymal, astroglial, and even neuronal TNF synthesis (Table 2A and Supplementary Table 1). The repeated lack of observation of neuronal TNF mRNA in situ hybridization signal in several independent well-controlled studies from our laboratory emphasizes that neuronal TNF production is negliable compared with the amount of TNF produced by microglia and macrophages after pMCAO in the mouse (Gregersen et al, 2000; Lambertsen et al, 2002, 2005, 2009). The predominant microglial-macrophage origin of TNF receives support from flow cytometry studies, showing that both microglia and macrophages, but not granulocytes, produce TNF after pMCAO in the stroke-lesioned mouse brain (Clausen et al, 2008; Lambertsen et al, 2009). Importantly, these studies also point to microglia as the source of the TNF present in the brain at stroke onset (Table 2A).
Regarding IL-1β, Buttini et al (1994), Clausen et al (2005, 2008), and Davies et al (1999) have convincingly shown that the main sources of IL-1β in rats and mice subjected to MCAO are microglia and macrophages (Table 2A), but apparently different subsets of microglia and macrophages than those producing TNF as demonstrated in flow cytometry studies (Clausen et al, 2008). Further, it appears that the microglia respond to the ischemic event by increasing their production of both IL-1β and TNF. This goes well hand-in-hand with flow cytometry results, that also point to a microglial origin of the IL-1β and TNF present in the normal brain (Clausen et al, 2008; Lambertsen et al, 2009; Tables 2A and 2B). In agreement with the histologic demonstration of perivascular infiltrates of IL-1β, but not TNF, producing cells in the later phase after MCAO, the proportion of IL-1β-producing macrophages is higher than of TNF-producing macrophages (Clausen et al, 2008). Further, as is the case for TNF, there is no evidence that granulocytes should be major producers of IL-1β (Clausen et al, 2008). In our laboratory, it has not been possible to reproduce reports on IL-1β immunoreactivity in astrocytes and endothelial cells in stroke-lesioned rats (Supplementary Table 1) and in our mouse model (Clausen et al, 2005, 2008).
There is, so far, very little information on IL-1α expression after experimental stroke. Interleukin-1α was recently shown to be upregulated in microglia in the peri-infarct 4 and 24 hours after tMCAO in the mouse (Luheshi et al, 2012). Further, there are, to our knowledge, no in situ hybridization studies of the expression of IL-6 mRNA after MCAO. Interleukin-6 immunoreactivity has been shown to increase in microglia and cortical neurons from 3.5 hours after pMCAO in rats (Suzuki et al, 1999; Table 2C).
Cytokines in Human Stroke
In humans, acute stroke has been shown to result in increased levels of TNF, IL-1β, and IL-6 in CSF and blood (Maas and Furie, 2009) and, so far, in the case of TNF also in the brain (Sairanen et al, 2001; Dziewulska and Mossakowski, 2003). These cytokines can be measured not only in serum or plasma but also are associated with a changed expression of numerous inflammatory genes in blood cells and, as shown recently, also in cells of the bone marrow (Denes et al, 2011; Sharp et al, 2011). These findings have lead to studies of stroke markers with the aim to improve diagnosis, prognosis, and therapy in stroke patients (Jickling and Sharp, 2011; Sharp et al, 2011). As TNF, IL-1β, and IL-6 can modulate infarct evolution in experimental stroke these cytokines have also attracted considerable interest as putative markers of stroke severity and neurologic outcome (Emsley et al, 2003, 2007; Jickling and Sharp, 2011).
Postmortem Studies
Because of the constraints with brain tissue from patients that did not survive an ischemic condition, the studies performed rely exclusively on the use of immunohistochemical methods. In two independent studies it was shown that TNF immunoreactivity is rapidly (<1 day) induced by stroke also in humans (Sairanen et al, 2001; Dziewulska and Mossakowski, 2003), thereby confirming animal studies (Table 3). However, the studies are contradictory with respect to the cellular source of TNF. Whereas Sairanen et al (2001) predominantly describe early TNF immunoreactivity in neurons and at later time points in astrocytes and infiltrating leukocytes, Dziewulska and Mossakowski (2003) show the most intense TNF immunoreactivity in microglia and conclude that these cells are the major source of TNF in human stroke. In an earlier study, TNF immunoreactivity was investigated in brains of stroke patients who died at later time points (up to around 30 days; Tomimoto et al, 1996). In this study, TNF immunoreactivity was predominantly found in microglia, with very few TNF+ astrocytes. The reason for these discrepancies are unclear, the results by Dziewulska and Mossakowski (2003), however, are consistent with the reports that limit early TNF production in stroke-lesioned rodent brain to microglia. According to our knowledge, TNF is yet the only cytokine that has been studied by immunohistochemical methods in post-mortem human stroke tissue.
Table 3. Time profile and cellular synthesis of TNF, IL-1β, and IL-6 in human stroke.
| Stroke severity and sample size | Time point(s) after stroke | Cytokine analysis | Time profile | Cellular synthesis and/or correlation between cytokine levels and stroke severity/outcome | Reference(s) |
|---|---|---|---|---|---|
| Postmortem studies in brain tissue | |||||
| Severe | 1–82 days | TNFa | TNF+ cells observed in all ischemic brains. Maximal numbers observed from 3 days | Primarily microglia-macrophages, but also neurons, astrocytes, and endothelial cells | Dziewulska and Mossakowski (2003) |
| Severe, 16 patients | 15 hours–18 days | TNFa | TNF+ cells from 0 to 6 days to 18 days, peak dependent on cell type | TNF+ neurons, peak days 2–3, gone from day 6, TNF+ invading blood cells from day 3, TNF+ astrocytes from 0 to 6 days to 14 days | Sairanen et al (2001) |
| Severe, 13 patients, including 2 cases of hemorrhage | 4 hours–15 months | TNFa | TNF+ cells from 30 hours, gone at 15 months | Predominantly microglia-macrophages, less in astrocytes and neurons | Tomimoto et al (1996) |
| CSF studies | |||||
| 30 Patients; small infarcts (n=17), large infarcts (n=13), 18 controls | CSF taken at 0–3, 7–9, 21–26 days and 3 months after stroke | TNF, IL-1β, and IL-6b | TNF only increased in patients with white matter damage 3 months after stroke. Elevated IL-1β in severe cases. Peak days 2–3. Increased IL-6, peak days 2–3 | Correlation of IL-6, but not TNF and IL-1β, with poor | Tarkowski et al (1995, 1997) |
| 23 Patients | CSF taken within 24 hours | TNFb | Elevated TNF within 24 hours | Correlation of TNF with lesion size and poor outcome | Zaremba and Losy (2001) |
| 231 Patients, no information on severity | CSF taken within 24 hours from 81 patients only | TNF and IL-6b | Elevated TNF and IL-6 in patients that deteriorated | Correlation of IL-6, but not TNF, with early worsening | Vila et al (2000) |
| 95 Patients, severe (n=44), mild–moderate (n=51), 25 controls | CSF taken within 6 hours | TNF, IL-1, and IL-6b | Elevated IL-1, IL-6, and TNF. IL-6 higher in severe stroke compared with mild and moderate | Correlation of IL-6 with lesion size and poor outcome at 1 month | Beridze et al (2011) |
| Peripheral blood studies | |||||
| 19 Patients within 4 hours | Blood taken at >1, 3, and 10 days | TNF, IL-1β, IL-6, serumb | IL-6 went up rapidly, peaked at 10 hours till 3 days, baseline at 10 days. No changes for IL-1β and TNF | Correlation of IL-6 with lesion size and poor outcome | Fassbender et al (1994) |
| 45 Patients within 72 hours, 40 controls | Blood taken in 1 day (n=35), 48 hours (n=7), −72 hours (n=3) | TNF, IL-1β, IL-6 in serumc | Elevated IL-6, but not IL-1β and TNF, compared with controls | No correlation of IL-6 with lesion size | Ormstad et al (2011) |
| 66 Patients within 20 hours, 32 controls | Blood taken at admission (6 to 29 hours after stroke) | TNF, IL-1β, IL-6 in serumb | Elevated TNF, IL-1β, and IL-6, compared with controls | Inverse correlation of IL-6 with lesion size and poor outcome | Sotgiu et al (2006) |
| 41 Patients within 24 hours, 40 controls | Blood taken at admission, 2, 4, 7, and 10 days | TNF in serumb | TNF was increased compared with controls at 4, 7, and 10 days, peak level day 7 | No correlation of TNF with lesion size and poor outcome | Intiso et al (2003) |
| 231 Patients within 24 hours | Blood taken at admission | TNF and IL-6 in plasmab | Elevated TNF and IL-6 in patients that deteriorated | Correlation of IL-6, but not TNF, with early worsening | Vila et al (2000; see also above) |
| 23 Patients within 24 hours | Blood taken at admission | TNF in serumb | Elevated TNF at 24 hours | Correlation of TNF with lesion size and poor outcome | Zaremba and Losy (2001) |
| 11 Patients, 9 controls | Blood taken at 4, 8, 12, 24, 48, and 72 hours, and 7 and 12 days, and 3 and 12 months | IL-6 in serumd | Elevated IL-6 in the first few hours, peak IL-6 between 3 and 7 days, and correlated with infections | Correlation of early IL-6 with lesion size and poor outcome | Waje-Andreassen et al (2005) |
| 42 Patients within 12 hours, 39 controls | Blood taken at admission, 1, 3, 7, and 14 days | IL-6 in serumb | No elevation of IL-6 up to 3 days after stroke, but elevated levels thereafter with peak at 3 days | Correlation of peak IL-6 with poor outcome. Higher IL-6 in patients with territorial compared with lacunar infarcts | Perini et al (2001) |
| 37 Patients within 12 hours | Blood taken at admission, 1, 5 to 7 days after stroke | IL-6 in plasmab | No information provided | Correlation of peak IL-6 with lesion size and poor outcome | Smith et al (2004) |
| 30 Patients within 3 days | Blood taken at 0–3, 7–9, 21–26 days, and 3 months | IL-1βb, IL-6d in serum | Slight elevation of IL-6 but not IL-1β at day 1 and thereafter. Less IL-6 in serum compared with CSF | No correlation of IL-6 with lesion size | Tarkowski et al (1995; see also above) |
| 18 Patients within 24 hours, 25 controls | Blood taken at admission and 24 hours after tPA therapy | TNF, IL-1β, IL-6 in plasmab | Elevated IL-1β and IL-6 compared with controls and before tPA therapy | Correlation of TNF, IL-1β, and IL-6 with poor outcome | Mazzotta et al (2004) |
| 16 Patients within 6 hours, MRI controlled study | Blood taken at admission, and at 12 and 24 hours | TNF, IL-6 in serumb | No elevation of TNF or IL-6 | Correlation of IL-6 and TNF with PWI values of lesion size | Montaner et al (2003) |
| 113 Patients, 43 controls | Blood taken at admission | TNF, IL-6 in plasmab | Significant elevation of IL-6 and TNF | Correlation of IL-6 and TNF with early deterioration and poor outcome | Castellanos et al (2002) |
CSF, cerebrospinal fluid; IL, interleukin;MRI, magnetic resonance imaging; PWI, perfusion-weighted image; TNF, tumor necrosis factor.
Assay type:
Immuno;
ELISA;
Bio-Plex human cytokine array;
Bio- and immuno assays.
Cytokines in cerebrospinal fluid
More studies have measured cytokine levels in CSF of stroke patients assuming a central origin of these cytokines and little leakage from blood into CSF (Table 3). In an elegant prospective study by Tarkowski et al (1997), TNF levels (next to IL-8, granulocyte-macrophage colony-stimulating factor, and IL-10) were measured in CSF from stroke patients 0 to 3, 7 to 9, 21 to 26 days, and 3 months after stroke. In this study, TNF levels were only increased compared with neurologically normal controls when looking at stroke patients with white matter damage 3 months after the insult (Tarkowski et al, 1997). These results have been challenged by Zaremba and Losy (2001), who detected elevated levels of TNF in CSF that was sampled within 24 hours after stroke, and further showed that CSF levels of TNF correlated with stroke severity and neurologic outcome (Zaremba and Losy, 2001). Knowing whether or not this study only consisted of patients with white matter lesions might be instrumental to understand the reason for the differences in TNF levels in CSF (Zaremba and Losy, 2001). Even though elevated TNF levels were found in CSF of stroke patients that deterioated also by Vila et al (2000), TNF levels did not correlate with early worsening, thereby challenging the results by Zaremba and Losy (2001; Table 3). This study, however, did not include healthy controls, which hamper the direct comparison with the other studies (Vila et al, 2000). Recent studies have shown that TNF levels were elevated in CSF 6 hours after stroke in patients compared with controls, irrespective of stroke severity, however, TNF neither correlated with lesion size or neurologic outcome (Beridze et al, 2011).
To our knowledge, there are only three reports on IL-1β levels in CSF from stroke patients (Table 3). Whereas Tarkowski et al (1995) attribute increased IL-1β to major stroke cases, elevated IL-1β levels in CSF have also been observed in patients with small infarcts (Sun et al, 2009). Beridze et al (2011) also detected elevated IL-1β levels in CSF 6 hours after the stroke irrespective of its severity but here IL-1β levels did not correlate with lesion size or outcome (Table 3). In comparison, more studies have investigated IL-6 levels in stroke patients (Table 3). In several studies, IL-6 levels were elevated in CSF of stroke patients, and further correlated with stroke severity (Table 3). This gains support from very recent studies showing a positive correlation between IL-6 levels in CSF at 6 hours and the lesion size at 24 hours (Beridze et al, 2011). The levels of IL-6 increases within 24 hours after stroke and increases are more pronounced in the case of gray matter lesions (Table 3 and Supplementary Table 2). In a more recent study, IL-6 levels were not changed in a population of patients with small infarcts, which again might indicate that IL-6 in the CSF is a marker of severe lesions (Sun et al, 2009) of especially the gray matter (Beridze et al, 2011).
Although the reviewed studies are mostly restricted to one time point, it is potentially interesting that the cytokine that is most consistently found to be increased in the CSF from stroke patients is IL-6, which may be produced by both microglia and neurons in stroke.
Cytokines in Blood
The analysis of cytokines in peripheral samples may or may not reflect central cytokine production. In comparison to the situation in the CSF, there are contrasting reports on stroke-induced changes in the level of TNF in serum and plasma. Some studies have reported that TNF levels remain unchanged after stroke, whereas others report on increased TNF levels albeit with different peak times and contradictory results with regard to a correlation between peripheral TNF levels and stroke severity (Table 3). In one magnetic resonance imaging-based study, no significant elevations of serum TNF levels were observed in the first 24 hours, although a correlation between TNF levels and the PWI signal was observed (Montaner et al, 2003).
There is a general agreement that IL-6 levels increase in serum or plasma from stroke patients during the first week after the insult (Table 3 and Supplementary Table 2), i.e., in all studies where peripheral IL-6 levels were measured IL-6 levels were elevated compared with control subjects (Supplementary Table 2). Less agreement, however, has been reached on the time point of peak IL-6 levels and the correlation between IL-6 levels and the final infarct volume. High IL-6 levels, which range from a few hours till 1 day after the insult, have been described in Table 3. Others describe IL-6 peak levels at 3 days (Perini et al, 2001) or some time during the first week (Smith et al, 2004). It appears that early IL-6 levels correlate with stroke severity (lesion size), PWI signal, and patient outcome (Fassbender et al, 1994; Perini et al, 2001; Castellanos et al, 2002; Montaner et al, 2003; Smith et al, 2004; Waje-Andreassen et al, 2005), although one study observed the opposite (Sotgiu et al, 2006). In 66 stroke patients, an inverse relationship between early IL-6 levels, lesion size, and final patient outcome was observed, indicating that early IL-6 is neuroprotective rather than a marker of disease progression (Sotgiu et al, 2006).
Although the importance of IL-1β in experimental stroke is undisputed, it generally is not observed at elevated levels in serum or plasma from stroke patients (Fassbender et al, 1994; Tarkowski et al, 1995; Emsley et al, 2007), which is likely due to its localized role (Emsley et al, 2007). The only exception is one report that shows modestly elevated serum levels of IL-1β in a small group of patients compared with healthy controls (Mazzotta et al, 2004). The importance of IL-1β in stroke, however, is underlined by a rapid upregulation of its natural antagonist IL-1Ra in brain ischemia (Emsley et al, 2007) and the potential use of IL-1Ra as a new treatment for stroke patients (Mulcahy et al, 2003; Emsley et al, 2005).
Taken together, there is little homogeneity in the data on peripheral cytokines in human stroke. A lack of homogeneity also exists between studies of lipopolysaccharide-induced release of cytokines (IL-1β, TNF, and IL-6) from whole blood cells drawn from stroke patients. Whereas Ferrarese et al (1999) found that blood cells from stroke patients released significantly higher cytokine levels, the opposite was described by Emsley et al (2007), who observed less cytokine release from blood cells from stroke patients. Moreover, it is becoming clear that systemic inflammation and thereby cytokine levels may be elevated before and influence stroke susceptability and outcome (McColl et al, 2009). Further, the large heterogeneity of human stroke should be taken into consideration when evaluating findings of stroke-induced changes in peripheral cytokines (Maas and Furie, 2009). In conclusion, significant information about peripheral cytokine responses in human stroke is still lacking, especially in the early phase (<4 to 6 hours) after the stroke (Table 3 and Supplementary Table 2).
Comparing Systemic Cytokine Responses in Human and Experimental Stroke
Our understanding of the role of systemic cytokines in human stroke is furthermore hampered by the fact that experimental stroke studies almost exclusively investigated the central cytokine response, leaving a gap of information concerning the systemic immune response in animals (Herrmann et al, 2003; Offner et al, 2009). There are only few studies that have in detail analyzed the systemic cytokine profile in response to experimental stroke. Increased IL-6 levels have been observed in plasma starting from 2 hours of reperfusion (3 hours after stroke onset) and in the brain from 24 hours (Chapman et al, 2009), whereas other studies have shown an increase of TNF levels in serum at 6 and 24 hours after MCAO (Chang et al, 2011), and provided evidence of higher release of IL-6 and TNF from stimulated splenocytes and blood cells at 6 and 24 hours, respectively (Chang et al, 2011; Offner et al, 2009). Interestingly, IL-1β was not detected systemically suggesting that this cytokine was only expressed in the ischemic brain (Offner et al, 2009). Chang and colleagues furthermore showed that the treatment with cocaine- and amphetamine-regulated transcript peptides reduced the infarct size and the cytokine response both centrally and systemically, indicating that the systemic cytokine response parallels the events in the brain (Chang et al, 2011). Although there are results pointing toward the systemic cytokines as potential target in stroke therapy, it should not be forgotten that one of the major clinical problems is post-stroke immunosuppression. A further dampening of systemic immune functions may therefore not be advisable (Denes et al, 2011).
Cytokine Receptors and Cytokine Signaling in Experimental Stroke
A detailed understanding of how cytokines influence the balance of the ischemic neurons between neuroprotection and neurotoxicity is still missing. As there are several excellent recent reviews on the presumed signaling mechanisms (Allan et al, 2005; McCoy and Tansey, 2008; Suzuki et al, 2009), we will mainly focus on neuronal expression of cytokine receptors in brain ischemia. Neurons express both TNF-Rs and IL-1Rs, and IL-6R (Allan et al, 2005; McCoy and Tansey, 2008; Suzuki et al, 2009), however, baseline expression may, as has been estimated for the IL-1RI, be limited to very few receptors per cell (Dinarello, 1994), which makes it difficult to study their expression in tissue sections. Nevertheless, it appears that the TNF-RI is increased in both neurons and non-neuronal cells from 4 to 6 hours and up till 5 days after pMCAO (Botchkina et al, 1997; Lambertsen et al, 2007) and tMCAO (Yin et al, 2004) in mice and rats. The TNF-RII is upregulated from 24 hours after pMCAO in the rat (Botchkina et al, 1997), at which time point it in the mouse is expressed in high levels by microglia and macrophages, consistent with that also the increase of TNF-RII mRNA is higher than that of TNF-RI mRNA (Lambertsen et al, 2007). This could reflect that the TNF-RI, besides a role in normal neuronal function (Botchkina et al, 1997), have a role for neuroprotection after experimental stroke (Figure 2). The TNF-RII to a larger extent appears to be involved in inflammatory responses, although neuroprotection though TNF-RII has been reported (Fontaine et al, 2002; Marchetti et al, 2004).
Both TNF-Rs can be cleaved from the cell surface as sTNF-RI and sTNF-RII and function as decoy molecules for TNF (Kohno et al, 1990; Nophar et al, 1990). Thus, increasing the cleavage of TNF-RI is an important step in reducing activation of TNF-RI-mediated apoptotic signaling in spinal cord neurons (Bartsch et al, 2010). Although cleavage is mediated by TNF alpha converting enzyme (TACE) in normal central nervous system, it is mediated by ADAM8 under pathologic conditions (Bartsch et al, 2010). Interestingly, ischemic tolerance induction in vitro depends on TACE-mediated TNF-release, which leads to upregulation of glutamate transporters (Romera et al, 2004), whereas, ischemic preconditioning involves upregulation of TACE and TNF-signaling through TNF-RI (Cardenas et al, 2002; Pradillo et al, 2005). Tumor necrosis factor signaling in ischemic neurons in vivo is still unclear. However, it appears that the pleiotrophic effect of TNF in experimental stroke (Figure 2 and Table 1A) can mainly be attributed to the binding of TNF to the TNF-RI, which through stepwise recruitment and activation of signaling molecules, leads to neuroprotection or apoptosis (McCoy and Tansey, 2008). Neuroprotection via TNF-RI can also be attributed to increases in calcium-binding proteins and Mn-superoxide dismutase in neurons (Mattson et al, 1997; Ginis et al, 2002).
Binding of IL-1 to IL-1RI leads to recruitment of a co-receptor accessory protein, which is essential to IL-1RI signaling (Greenfeder et al, 1995; Cullinan et al, 1998; Lang et al, 1998). Interestingly, N-methyl-D-aspartate-R activation increases the interaction between IL-1RI and the glutamate recepter GluN2b subunit of N-methyl-D-Aspartate-R (Gardoni et al, 2011). Interleukin-1β also potentiates N-methyl-D-Aspartate-R-mediated increases of intracellular calcium and neuronal death by Src tyrosine kinase activation in vitro (Viviani et al, 2003). Taken together, this could provide a mechanism by which ischemia could sensitize neurons to IL-1β. Further, there is evidence that IL-1 can signal independently of the IL-1RI, suggesting that there may be other functional, yet unknown, IL-1Rs in the brain (Parker et al, 2002; Touzani et al, 2002). Besides IL-1RII, both soluble receptors, sIL-1RI and sIL-1RII, act as decoy receptors (Allan et al, 2005; Fogal and Hewett, 2008). Interleukin-1Ra has been shown to be induceable in primary microglial cultures (Pinteaux et al, 2006), and to be rapidly upregulated after experimental stroke and inhibiting its function enhances infarct size (Boutin et al, 2001; Loddick et al, 1996). As previously discussed, administration of IL-1Ra by various routes is protective in stroke models (Figure 2 and Table 1B), making IL-1Ra the most widely studied putative neuroprotector (Banwell et al, 2009; Galea et al, 2011).
IL-6 exerts its function through binding to the IL-6R, which has no signaling properties by itself. However, ligand binding allows the formation of gp130/gp130 homodimers that associates with Janus-associated kinases, activates signal transducer and activator of transcription and mitogen-activated protein kinase signaling pathways (Heinrich et al, 2003; Kamimura et al, 2003; Ernst and Jenkins, 2004; Bauer et al, 2007). Unlike sTNF-R and sIL-1R, the sIL-6R does not have any decoy properties, but instead activates the ubiquitously expressed gp130 like the membrane-bound form of IL-6R (Scheller and Rose-John, 2006). This mechanism is called trans-signaling and contributes to explain that IL-6 has numerous effects in many different cell types, despite the limited expression of the IL-6R (Scheller and Rose-John, 2006). Brain neurons express IL-6R, whereas glial cells, including microglia, require sIL-6R to respond to IL-6 (Suzuki et al, 2009). In contrast to the IL-6 there is so far no evidence that the levels of IL-6R change after MCAO (Suzuki et al, 2005). Although the mechanisms behind the apparently neuroprotective effect of IL-6 in stroke (Figure 2 and Table 1C) have not yet been ressolved, we have shown that IL-6 upregulates the expression and function of the neuronal adenosine A1 receptor (Biber et al, 2008). This upregulation appears to be crucial for the protective effect of IL-6, as IL-6 is not protective in neurons lacking adenosine A1 receptors (Moidunny et al, 2010). Furthermore, as IL-6 inhibits IL-l synthesis (Schindler et al, 1990) and stimulates the production of the IL-1Ra and sTNF-RI (Tilg et al, 1994), these actions may also contribute to the neuroprotective effects of IL-6.
Discussion
From the literature reviewed here, it is clear that modulating the function of TNF, IL-1, or IL-6 in experimental stroke has significant effects on infarct evolution, after both pMCAO and tMCAO, and across different species and strains (Figure 2). This finding, and in particular the robustness of the finding, indicates that these cytokines also influence infarct evolution in human stroke. Due to the narrow therapeutic window, the few-fold increases in cytokine levels in the early phase after stroke onset (<4 to 6 hours), and even the low baseline levels of cytokines present at stroke onset, are the cytokines that can directly act on the ischemic neurons, and must therefore be the cytokines that are important for the evolution of the infarct. This is particularly clear in the case of pMCAO where the penumbra is recruited into the infarct within the first few hours after stroke onset (Figures 1A and 1B). Evidence that the low baseline levels of cytokines influence infarct evolution is also provided by the findings of increased infarct sizes in TNF- and TNF-RI-deficient mice (Bruce et al, 1996; Gary et al, 1998; Taoufik et al, 2007; Lambertsen et al, 2009) and IL-6-deficient mice (Herrmann et al, 2003), and of reduced infarct sizes in IL-1α/β-deficient mice (Boutin et al, 2001), findings obtained by several independent laboratories (Figure 2). Nevertheless, as these results have been obtained using transgenics with embryonic deletions, which could lead to gestational adaptations of neurons, and compensatory changes of other cytokine systems, key findings should be re-investigated using mice with cell-specific or conditional cytokine deletions.
An obvious question is if the effect of cytokines in general, or of individual cytokines, depends on the model used, pMCAO or tMCAO? At present there is no clear answer to this question. Using the wording by Hossmann (2012), ‘In promptly reversed transient ischemia as after mechanical occlusion', blood-borne cells and cytokines have fast access to the infarct core and the penumbra. Although, there are no studies that have directly compared leukocyte kinetics after pMCAO and tMCAO, it is obvious from the literature that larger numbers of leukocytes accumulate faster in the ischemic territory after tMCAO (Gelderblom et al, 2009) than after pMCAO (Clausen et al, 2008). Grossly, 1% to 2% of myeloid cells were macrophages in the hemispheres from perfused, unmanipulated central nervous system in these studies. This percentage had at 12 hours increased to, respectively, 5% and 20%, and at 24 hours to, respectively, 25% and close to 30%, of the total number of myeloid cells, after pMCAO (Clausen et al, 2008) and tMCAO (Gelderblom et al, 2009). Although, the model used by Gelderblom et al (2009) is a model for proximal tMCAO compared with the distal pMCAO model used by Clausen et al (2008), these percentages appear representative for previously published work on leukocyte entry into the stroke-lesioned brain (Zhang et al, 1997; Lehrmann et al, 1997; Gregersen et al, 2000; Lambertsen et al, 2009). Consistent with that macrophages infiltrate the ischemic territory with a delay after pMCAO, we in our recent studies of the effect of microglial- versus macrophage-derived TNF, found that the neuroprotective TNF in pMCAO is produced by microglia and not macrophages (Lambertsen et al, 2009). However, this finding clearly leaves open the possibility that macrophage-derived TNF might influence infarct evolution after tMCAO. Indeed, such effect will depend on the cytokine and on its production by the macrophages after they have infiltrated the neural parenchyma. The best evidence that systemic cytokines influence infarct evolution is provided by experimental stroke studies, showing that i.v., subcutaneous, or intraperitoneal treatment of the experimental animal with cytokine or cytokine antagonist at the time of, or after MCAO, reduces the size of the infarct (Dawson et al, 1996; Relton et al, 1996; Nawashiro et al, 1997a, 1997b; Lavine et al, 1998; Wang et al, 2004) (Figure 2). Recently, it was also shown that IL-1α is contained in platelets, and that it modifies endothelial cell adhesion molecule expression in vitro, thereby putatively facilitating leukocyte extravasation (Thornton et al, 2010). Taken together, systemic administration of cytokines or cytokine-antagonists still holds promise as a treatment option in acute stroke therapy, taking into consideration the therapeutic window.
Although the available information on IL-6 in experimental stroke, argue against a pathogenic role of IL-6 in stroke (Suzuki et al, 2009), it was nevertheless surprising that there was so little data on its production in experimental stroke. The importance of this question is emphasized by the finding that IL-6 is the cytokine, which is most consistently found to be increased in the CSF from stroke patients. Although, there is data suggesting that IL-6 is produced in both neurons and non-neuronal cells after MCAO in rats (Suzuki et al, 1999, 2009), IL-6 is also produced by microglia in other models of neurologic disease (Nakanishi et al, 2007; Cho et al, 2011). At present, it is therefore difficult to know whether the increased IL-6 in CSF after a stroke in the human, reflects release of IL-6 into the CSF from dying neurons or if IL-6 is produced by microglia. In the lack of technology that allows molecular modeling (e.g., imaging, nuclear magnetic resonance spectroscopy) of cytokines and their receptors in human stroke, we still depend on information from studies of postmortem human brain tissue. Although, studies of postmortem human brain tissue are far from trivial, and may not necessarily reflect the situation in stroke survivors, we therefore still need well-controlled studies to be performed on the in situ production of IL-6. In fact, we would argue the same for IL-1, whose cellular production also remains undetermined in postmortem human stroke tissue, and even for TNF, as the results from the available immunohistochemical reports are contradictory (Table 3).
In the peripheral nervous system, it is generally accepted that cytokines released from inflammatory cells regulate neuronal sensitivity to stimulation. Any tissue damage and the subsequent release of inflammatory mediators cause a transient hypersensitivity of the pain-sensing system of the affected area, a phenomenon called inflammatory pain. An injection of TNF, IL-1, or IL-6 causes rapidly (within minutes) hyperalgesia in numerous animal models (Thacker et al, 2007). This rapid effect is explained by numerous direct effects of these cytokines on nociceptive neurons, such as changes in ion-currents, enhancement of transient receptor potential channel activity, and increases in glutamatergic effects (St Pierre et al, 2009). Several lines of evidence indicate that, at least for IL-1 and TNF, similar effects are also observed in central nervous system neurons (Viviani et al, 2003; Gardoni et al, 2011). These and other results have led to the hypothesis that the direct sensitization by IL-1 of cortical neurons to glutamatergic input may contribute to the known detrimental effects of IL-1 in stroke (Fogal and Hewett, 2008). In comparison, cortical neurons respond to IL-6 with a rapid upregulation of adenosine A1 receptors, which results in decreased electrical excitability and decreased sensitivity toward glutamate (Biber et al, 2008; Moidunny et al, 2010). This could potentially also occur in the stroke-lesioned brain where an upregulation of adenosine A1 receptors would most likely increase survival of penumbral neurons.
The findings discussed here show the limitations of focussing on one cytokine only, which is part of a dynamic network. Upcoming reports based on the use of transgenics with conditional and cell-specific deletion of cytokines will provide insight into these questions. Furthermore, as we now have evidence that microglia is a diverse cell population with regard to cytokine production (Clausen et al, 2008), it should be clarified what regulates microglial production of early stroke cytokines or if different subsets microglia are destined to respond by producing different cytokines. Possibly, the more general issue about cellular cytokine production can be reduced to that microglia just produce much higher levels of, e.g., TNF and IL-1 than any other cell in the neural parenchyma, while sub-threshold produced cytokines still matters, and modulate neuronal sensitivity to, in this context, ischemia. What should also be considered is that cytokines, despite their importance, only constitute a single stratum of a multi-layered immune system. Removing a single cytokine may therefore not solely modify the production of other cytokines, but also modify the production of other immune mediators and alter the sensitivity of neuronal and non-neuronal cells to these mediators. To model cytokine effects on the neuronal network at the genomic and proteomic level, in the penumbra in the early phase after experimental stroke, using models for both pMCAO and tMCAO, could be instrumental to pave the way for new strategies for inhibiting detrimental effects and promoting beneficial effects of key inflammatory cytokines in stroke.
Acknowledgments
We thank Ms Tanja Hass Nielsen for the artwork, and Dr Bettina Clausen for giving permission to use her original IL-1β mRNA data in Figure 4.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Journal of Cerebral Blood Flow & Metabolism website (http://www.nature.com/jcbfm)
The work reported here has been supported in part by grants from the Lundbeck Foundation to Dr Kate Lykke Lambertsen (5539) and Dr Bente Finsen (2201), from the Novo Nordic Foundation (R153-A-12550) and the Danish Medical Research Council (22-04-0638) to Dr Kate Lykke Lambertsen, and by grants from the German Research Council (DFG, FOR1336) and EU FP7 ‘MoodInflame' to Dr Knut Biber.
Supplementary Material
References
- Adibhatla RM, Haatcher JF. Secretory phospholipase A2 IIA is up-regulated by TNF-α and IL-1α/β after transient focal cerebral ischemia in rat. Brain Res. 2007;1134:199–205. doi: 10.1016/j.brainres.2006.11.080. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Allan SM, Tyrrell PJ, Rothwell NJ. Interleukin-1 and neuronal injury. Nat Rev Immunol. 2005;5:629–640. doi: 10.1038/nri1664. [DOI] [PubMed] [Google Scholar]
- Astrup J, Siesjo BK, Symon L. Thresholds in cerebral ischemia - the ischemic penumbra. Stroke. 1981;12:723–725. doi: 10.1161/01.str.12.6.723. [DOI] [PubMed] [Google Scholar]
- Back T, Hemmen T, Schuler OG. Lesion evolution in cerebral ischemia. J Neurol. 2004;251:388–397. doi: 10.1007/s00415-004-0399-y. [DOI] [PubMed] [Google Scholar]
- Banwell V, Sena ES, Macleod MR. Systematic review and stratified meta-analysis of the efficacy of interleukin-1 receptor antagonist in animal models of stroke. J Stroke Cerebrovasc Dis. 2009;18:269–276. doi: 10.1016/j.jstrokecerebrovasdis.2008.11.009. [DOI] [PubMed] [Google Scholar]
- Barone FC, Arvin B, White RF, Miller A, Webb CL, Willette RN, Lysko PG, Feuerstein GZ. Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke. 1997;28:1233–1244. doi: 10.1161/01.str.28.6.1233. [DOI] [PubMed] [Google Scholar]
- Bartsch JW, Wildeboer D, Koller G, Naus S, Rittger A, Moss ML, Minai Y, Jockusch H. Tumor necrosis factor-alpha (TNF-alpha) regulates shedding of TNF-alpha receptor 1 by the metalloprotease-disintegrin ADAM8: evidence for a protease-regulated feedback loop in neuroprotection. J Neurosci. 2010;30:12210–12218. doi: 10.1523/JNEUROSCI.1520-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer S, Kerr BJ, Patterson PH. The neuropoietic cytokine family in development, plasticity, disease and injury. Nat Rev Neurosci. 2007;8:221–232. doi: 10.1038/nrn2054. [DOI] [PubMed] [Google Scholar]
- Beridze M, Sanikidze T, Shakarishvili R, Intskirveli N, Bornstein NM. Selected acute phase CSF factors in ischemic stroke: findings and prognostic value. BMC Neurol. 2011;11:41. doi: 10.1186/1471-2377-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berti R, Williams AJ, Moffett JR, Hale SL, Velarde LC, Elliott PJ, Yao C, Dave JR, Tortella FC. Quantitative real-time RT-PCR analysis of inflammatory gene expression associated with ischemia-reperfusion brain injury. J Cereb Blood Flow Metab. 2002;22:1068–1079. doi: 10.1097/00004647-200209000-00004. [DOI] [PubMed] [Google Scholar]
- Biber K, Pinto-Duarte A, Wittendorp MC, Dolga AM, Fernandes CC, Von Frijtag Drabbe Kunzel J, Keijser JN, de Vries R, Ijzerman AP, Ribeiro JA, Eisel U, Sebastiao AM, Boddeke HW. Interleukin-6 upregulates neuronal adenosine A1 receptors: implications for neuromodulation and neuroprotection. Neuropsychopharmacology. 2008;33:2237–2250. doi: 10.1038/sj.npp.1301612. [DOI] [PubMed] [Google Scholar]
- Botchkina GI, Meistrell ME, III, Botchkina IL, Tracey KJ. Expression of TNF and TNF receptors (p55 and p75) in the rat brain after focal cerebral ischemia. Mol Med. 1997;3:765–781. [PMC free article] [PubMed] [Google Scholar]
- Boutin H, LeFeuvre RA, Horai R, Asano M, Iwakura Y, Rothwell NJ. Role of IL-1alpha and IL-1beta in ischemic brain damage. J Neurosci. 2001;21:5528–5534. doi: 10.1523/JNEUROSCI.21-15-05528.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breder CD, Tsujimoto M, Terano Y, Scott DW, Saper CB. Distribution and characterization of tumor necrosis factor-alpha-like immunoreactivity in the murine central nervous system. J Comp Neurol. 1993;337:543–567. doi: 10.1002/cne.903370403. [DOI] [PubMed] [Google Scholar]
- Bruce AJ, Boling W, Kindy MS, Peschon J, Kraemer PJ, Carpenter MK, Holtsberg FW, Mattson MP. Altered neuronal and microglial responses to excitotoxic and ischemic brain injury in mice lacking TNF receptors. Nat Med. 1996;2:788–794. doi: 10.1038/nm0796-788. [DOI] [PubMed] [Google Scholar]
- Buttini M, Appel K, Sauter A, Gebicke-Haerter PJ, Boddeke HW. Expression of tumor necrosis factor alpha after focal cerebral ischaemia in the rat. Neuroscience. 1996;71:1–16. doi: 10.1016/0306-4522(95)00414-9. [DOI] [PubMed] [Google Scholar]
- Buttini M, Sauter A, Boddeke HW. Induction of interleukin-1 beta mRNA after focal cerebral ischaemia in the rat. Brain Res Mol Brain Res. 1994;23:126–134. doi: 10.1016/0169-328x(94)90218-6. [DOI] [PubMed] [Google Scholar]
- Cardenas A, Moro MA, Leza JC, O'Shea E, Davalos A, Castillo J, Lorenzo P, Lizasoain I. Upregulation of TACE/ADAM17 after ischemic preconditioning is involved in brain tolerance. J Cereb Blood Flow Metab. 2002;22:1297–1302. doi: 10.1097/01.WCB.0000033968.83623.D0. [DOI] [PubMed] [Google Scholar]
- Castellanos M, Castillo J, García MM, Leira R, Serena J, Chamorro A, Dávalos A. Inflammation-mediated damage in progressing lacunar infarctions: a potential therapeutic target. Stroke. 2002;33:982–987. doi: 10.1161/hs0402.105339. [DOI] [PubMed] [Google Scholar]
- Chang L, Chen Y, Li J, Liu Z, Wang Z, Chen J, Cao W, Xu Y. Cocaine- and amphetamine-regulated transcript modulates peripheral immunity and protects against brain injury in experimental stroke. Brain Behav Immun. 2011;25:260–269. doi: 10.1016/j.bbi.2010.09.017. [DOI] [PubMed] [Google Scholar]
- Chapman KZ, Dale VQ, Denes A, Bennett G, Rothwell NJ, Alland SM, McColl BW. A rapid and transient response precedes brain inflammation after experimental stroke. J Cereb Blood Flow Metab. 2009;29:1764–1768. doi: 10.1038/jcbfm.2009.113. [DOI] [PubMed] [Google Scholar]
- Cho SH, Sun B, Zhou Y, Kauppinen TM, Halabisky B, Wes P, Ransohoff RM, Gan L. CX3CR1 modulates microglial activation and protects against plaque-independent cognitive deficits in a mouse model of Alzheimer's disease. J Biol Chem. 2011;286:32713–32722. doi: 10.1074/jbc.M111.254268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark WM, Rinker LG, Lessov NS, Hazel K, Hill JK, Stenzel-Poore M, Eckenstein F. Lack of interleukin-6 expression is not protective against focal central nervous system ischemia. Stroke. 2000;31:1715–1720. doi: 10.1161/01.str.31.7.1715. [DOI] [PubMed] [Google Scholar]
- Clausen BH, Lambertsen KL, Babcock AA, Holm TH, Dagnaes-Hansen F, Finsen B. Interleukin-1beta and tumor necrosis factor-alpha are expressed by different subsets of microglia and macrophages after ischemic stroke in mice. J Neuroinflammation. 2008;5:46. doi: 10.1186/1742-2094-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clausen BH, Lambertsen KL, Meldgaard M, Finsen B. A quantitative in situ hybridization and polymerase chain reaction study of microglial-macrophage expression of interleukin-1beta mRNA following permanent middle cerebral artery occlusion in mice. Neuroscience. 2005;132:879–892. doi: 10.1016/j.neuroscience.2005.01.031. [DOI] [PubMed] [Google Scholar]
- Cullinan EB, Kwee L, Nunes P, Shuster DJ, Ju G, McIntyre KW, Chizzonite RA, Labow MA. IL-1 receptor accessory protein is an essential component of the IL-1 receptor. J Immunol. 1998;161:5614–5620. [PubMed] [Google Scholar]
- Davies CA, Loddick SA, Toulmond S, Stroemer RP, Hunt J, Rothwell NJ. The progression and topographic distribution of interleukin-1beta expression after permanent middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab. 1999;19:87–98. doi: 10.1097/00004647-199901000-00010. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Martin D, Hallenbeck JM. Inhibition of tumor necrosis factor-alpha reduces focal cerebral ischemic injury in the spontaneously hypertensive rat. Neurosci Lett. 1996;218:41–44. doi: 10.1016/0304-3940(96)13116-5. [DOI] [PubMed] [Google Scholar]
- del Zoppo GJ, Sharp FR, Heiss WD, Albers GW. Heterogeneity in the penumbra. J Cereb Blood Flow Metab. 2011;31:1836–1851. doi: 10.1038/jcbfm.2011.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denes A, McColl BW, Leow-Dyke SF, Chapman KZ, Humphreys NE, Grencis RK, Allan SM, Rothwell NJ. Experimental stroke-induced changes in the bone marrow reveal complex regulation of leukocyte responses. J Cereb Blood Flow Metab. 2011;31:1036–1050. doi: 10.1038/jcbfm.2010.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinarello CA. The interleukin-1 family: 10 years of discovery. FASEB J. 1994;8:1314–1325. [PubMed] [Google Scholar]
- Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–397. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- Dziewulska D, Mossakowski MJ. Cellular expression of tumor necrosis factor a and its receptors in human ischemic stroke. Clin Neuropathol. 2003;22:35–40. [PubMed] [Google Scholar]
- Emsley HC, Smith CJ, Gavin CM, Georgiou RF, Vail A, Barberan EM, Illingworth K, Scarth S, Wickramasinghe V, Hoadley ME, Rothwell NJ, Tyrrell PJ, Hopkins SJ. Clinical outcome following acute ischaemic stroke relates to both activation and autoregulatory inhibition of cytokine production. BMC Neurol. 2007;7:5. doi: 10.1186/1471-2377-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emsley HC, Smith CJ, Georgiou RF, Vail A, Hopkins SJ, Rothwell NJ, Tyrrell PJ. A randomised phase II study of interleukin-1 receptor antagonist in acute stroke patients. J Neurol Neurosurg Psychiatry. 2005;76:1366–1372. doi: 10.1136/jnnp.2004.054882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emsley HC, Smith CJ, Gavin CM, Georgiou RF, Vail A, Barberan EM, Hallenbeck JM, del Zoppo GJ, Rothwell NJ, Tyrrell PJ, Hopkins SJ. An early and sustained peripheral inflammatory response in acute ischaemic stroke: relationships with infection and atherosclerosis. J Neuroimmunol. 2003;139:93–101. doi: 10.1016/s0165-5728(03)00134-6. [DOI] [PubMed] [Google Scholar]
- Ernst M, Jenkins BJ. Acquiring signaling specificity from the cytokine receptor gp130. Trends Genet. 2004;20:23–32. doi: 10.1016/j.tig.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Fassbender K, Schmidt R, Mossner R, Daffertshofer M, Hennerici M. Pattern of activation of the hypothalamic-pituitary-adrenal axis in acute stroke. Relation to acute confusional state, extent of brain damage, and clinical outcome. Stroke. 1994;25:1105–1108. doi: 10.1161/01.str.25.6.1105. [DOI] [PubMed] [Google Scholar]
- Ferrarese C, Mascarucci P, Zoia C, Cavarretta R, Frigo M, Begni B, Sarinella F, Frattola L, De Simoni MG. Increased cytokine release from peripheral blood cells after acute stroke. J Cereb Blood Flow Metab. 1999;19:1004–1009. doi: 10.1097/00004647-199909000-00008. [DOI] [PubMed] [Google Scholar]
- Fogal B, Hewett SJ. Interleukin-1beta: a bridge between inflammation and excitotoxicity. J Neurochem. 2008;106:1–23. doi: 10.1111/j.1471-4159.2008.05315.x. [DOI] [PubMed] [Google Scholar]
- Fontaine V, Mohand-Said S, Hanoteau N, Fuchs C, Pfizenmaier K, Eisel U. Neurodegenerative and neuroprotective effects of tumor necrosis factor (TNF) in retinal ischemia: opposite roles of TNF receptor 1 and TNF receptor 2. J Neurosci. 2002;22:RC216. doi: 10.1523/JNEUROSCI.22-07-j0001.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gahring LC, Carlson NG, Kulmar RA, Rogers SW. Neuronal expression of tumor necrosis factor alpha in the murine brain. Neuroimmunomodulation. 1996;3:289–303. doi: 10.1159/000097283. [DOI] [PubMed] [Google Scholar]
- Galea J, Ogungbenro K, Hulme S, Greenhalgh A, Aarons L, Scarth S, Hutchinson P, Grainger S, King A, Hopkins SJ, Rothwell N, Tyrrell P. Intravenous anakinra can achieve experimentally effective concentrations in the central nervous system within a therapeutic time window: results of a dose-ranging study. J Cereb Blood Flow Metab. 2011;31:439–447. doi: 10.1038/jcbfm.2010.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia JH, Liu KF, Relton JK. Interleukin-1 receptor antagonist decreases the number of necrotic neurons in rats with middle cerebral artery occlusion. Am J Pathol. 1995;147:1477–1486. [PMC free article] [PubMed] [Google Scholar]
- Gardoni F, Boraso M, Zianni E, Corsini E, Galli CL, Cattabeni F, Marinovich M, Di Luca M, Viviani B. Distribution of interleukin-1 receptor complex at the synaptic membrane driven by interleukin-1beta and NMDA stimulation. J Neuroinflammation. 2011;8:14. doi: 10.1186/1742-2094-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gary DS, Bruce-Keller AJ, Kindy MS, Mattson MP. Ischemic and excitotoxic brain injury is enhanced in mice lacking the p55 tumor necrosis factor receptor. J Cereb Blood Flow Metab. 1998;18:1283–1287. doi: 10.1097/00004647-199812000-00001. [DOI] [PubMed] [Google Scholar]
- Gelderblom M, Leypoldt F, Steinbach K, Behrens D, Choe CU, Siler DA, Arumugam TV, Orthey E, Gerloff C, Tolosa E, Magnus T. Temporal and spatial dynamics of cerebral immune cell accumulation in stroke. Stroke. 2009;40:1849–1857. doi: 10.1161/STROKEAHA.108.534503. [DOI] [PubMed] [Google Scholar]
- Ginis I, Jaiswal R, Klimanis D, Liu J, Greenspon J, Hallenbeck JM. TNF-alpha-induced tolerance to ischemic injury involves differential control of NF-kappaB transactivation: the role of NF-kappaB association with p300 adaptor. J Cereb Blood Flow Metab. 2002;22:142–152. doi: 10.1097/00004647-200202000-00002. [DOI] [PubMed] [Google Scholar]
- Ginsberg MD. Neuroprotection for ischemic stroke: past, present and future. Neuropharmacology. 2008;55:363–389. doi: 10.1016/j.neuropharm.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfeder SA, Nunes P, Kwee L, Labow M, Chizzonite RA, Ju G. Molecular cloning and characterization of a second subunit of the interleukin 1 receptor complex. J Biol Chem. 1995;270:13757–13765. doi: 10.1074/jbc.270.23.13757. [DOI] [PubMed] [Google Scholar]
- Gregersen R, Lambertsen K, Finsen B. Microglia and macrophages are the major source of tumor necrosis factor in permanent middle cerebral artery occlusion in mice. J Cereb Blood Flow Metab. 2000;20:53–65. doi: 10.1097/00004647-200001000-00009. [DOI] [PubMed] [Google Scholar]
- Hara H, Fink K, Endres M, Friedlander RM, Gagliardini V, Yuan J, Moskowitz MA. Attenuation of transient focal cerebral ischemic injury in transgenic mice expressing a mutant ICE inhibitory protein. J Cereb Blood Flow Metab. 1997a;17:370–375. doi: 10.1097/00004647-199704000-00002. [DOI] [PubMed] [Google Scholar]
- Hara H, Friedlander RM, Gagliardini V, Ayata C, Fink K, Huang Z, Shimizu-Sasamata M, Yuan J, Moskowitz MA. Inhibition of interleukin 1beta converting enzyme family proteases reduces ischemic and excitotoxic neuronal damage. Proc Natl Acad Sci USA. 1997b;94:2007–2012. doi: 10.1073/pnas.94.5.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hata R, Maeda K, Hermann D, Mies G, Hossmann KA. Dynamics of regional brain metabolism and gene expression after middle cerebral artery occlusion in mice. J Cereb Blood Flow Metab. 2000a;20:306–315. doi: 10.1097/00004647-200002000-00012. [DOI] [PubMed] [Google Scholar]
- Hata R, Maeda K, Hermann D, Mies G, Hossmann KA. Evolution of brain infarction after transient focal cerebral ischemia in mice. J Cereb Blood Flow Metab. 2000b;20:937–946. doi: 10.1097/00004647-200006000-00006. [DOI] [PubMed] [Google Scholar]
- Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F. Principles of interleukin (IL)-6-type cytokine signaling and its regulation. Biochem J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiss WD, Sobesky J. Comparison of PET and DW/PW-MRI in acute ischemic stroke. Keio J Med. 2008;57:125–131. doi: 10.2302/kjm.57.125. [DOI] [PubMed] [Google Scholar]
- Herrmann O, Tarabin V, Suzuki S, Attigah N, Coserea I, Schneider A, Vogel J, Prinz S, Schwab S, Monyer H, Brombacher F, Schwaninger M. Regulation of body temperature and neuroprotection by endogenous interleukin-6 in cerebral ischemia. J Cereb Blood Flow Metab. 2003;23:406–415. doi: 10.1097/01.WCB.0000055177.50448.FA. [DOI] [PubMed] [Google Scholar]
- Hill JK, Gunion-Rinker L, Kulhanek D, Lessov N, Kim S, Clark WM, Dixon MP, Nishi R, Stenzel-Poore MP, Eckenstein FP. Temporal modulation of cytokine expression following focal cerebral ischemia in mice. Brain Res. 1999;820:45–54. doi: 10.1016/s0006-8993(98)01140-8. [DOI] [PubMed] [Google Scholar]
- Hillhouse EW, Kida S, Iannotti F. Middle cerebral artery occlusion in the rat causes a biphasic production of immunoreactive interleukin-1beta in the cerebral cortex. Neurosci Lett. 1998;249:177–179. doi: 10.1016/s0304-3940(98)00392-9. [DOI] [PubMed] [Google Scholar]
- Hoehn M, Nicolay K, Franke C, van der Sanden B. Application of magnetic resonance to animal models of cerebral ischemia. J Magn Reson Imaging. 2001;14:491–509. doi: 10.1002/jmri.1213. [DOI] [PubMed] [Google Scholar]
- Hossmann KA. Pathophysiology and therapy of experimental stroke. Cell Mol Neurobiol. 1996;26:1057–1083. doi: 10.1007/s10571-006-9008-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossmann KA.2012The two pathophysiologies of focal brain ischemia: implications for translational stroke research J Cereb Blood Flow Metabdoi: 10.1038/jcbfm.2011.186 [DOI] [PMC free article] [PubMed]
- Huang P, Chen CH, Yang YH, Lin RT, Lin FC, Liu CK. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: way to endeavor. Cerebrovasc Dis. 2006;22:423–428. doi: 10.1159/000094994. [DOI] [PubMed] [Google Scholar]
- Hughes JL, Beech JS, Jones PS, Wang D, Menon DK, Baron JC. Mapping selective neuronal loss and microglial activation in the salvaged neocortical penumbra in the rat. Neuroimage. 2010;49:19–31. doi: 10.1016/j.neuroimage.2009.08.047. [DOI] [PubMed] [Google Scholar]
- Intiso D, Stampatore P, Zarrelli MM, Guerra GL, Arpaia G, Simone P, Tonali P, Beghi E. Incidence of first-ever ischemic and hemorrhagic stroke in a well-defined community of southern Italy, 1993 to 1995. Eur J Neurol. 2003;10:559–565. doi: 10.1046/j.1468-1331.2003.00648.x. [DOI] [PubMed] [Google Scholar]
- Jickling GC, Sharp FR. Blood biomarkers of ischemic stroke. Neurotherapeutics. 2011;8:349–360. doi: 10.1007/s13311-011-0050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamimura D, Ishihara K, Hirano T. IL-6 signal transduction and its physiological roles: the signal orchestration model. Rev Physiol Biochem Pharmacol. 2003;149:1–38. doi: 10.1007/s10254-003-0012-2. [DOI] [PubMed] [Google Scholar]
- Kim YD, Sohn NW, Kang C, Soh Y. DNA array reveals altered gene expression in response to focal cerebral ischemia. Brain Res Bull. 2002;58:491–498. doi: 10.1016/s0361-9230(02)00823-7. [DOI] [PubMed] [Google Scholar]
- Kohno T, Brewer MT, Baker SL, Schwartz PE, King MW, Hale KK, Squires CH, Thompson RC, Vannice JL. A second tumor necrosis factor receptor gene product can shed a naturally occurring tumor necrosis factor inhibitor. Proc Natl Acad Sci USA. 1990;87:8331–8335. doi: 10.1073/pnas.87.21.8331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriegler M, Perez C, DeFay K, Albert I, Lu SD. A novel form of TNF/cachectin is a cell surface cytotoxic transmembrane protein: ramifications for the complex physiology of TNF. Cell. 1988;53:45–53. doi: 10.1016/0092-8674(88)90486-2. [DOI] [PubMed] [Google Scholar]
- Lambertsen KL, Clausen BH, Babcock AA, Gregersen R, Fenger C, Nielsen HH, Haugaard LS, Wirenfeldt M, Nielsen M, Dagnaes-Hansen F, Bluethmann H, Faergeman NJ, Meldgaard M, Deierborg T, Finsen B. Microglia protect neurons against ischemia by synthesis of tumor necrosis factor. J Neurosci. 2009;29:1319–1330. doi: 10.1523/JNEUROSCI.5505-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambertsen KL, Clausen BH, Fenger C, Wulf H, Owens T, Dagnaes-Hansen F, Meldgaard M, Finsen B. Microglia and macrophages express tumor necrosis factor receptor p75 following middle cerebral artery occlusion in mice. Neuroscience. 2007;144:934–949. doi: 10.1016/j.neuroscience.2006.10.046. [DOI] [PubMed] [Google Scholar]
- Lambertsen KL, Gregersen R, Finsen B. Microglial-macrophage synthesis of tumor necrosis factor after focal cerebral ischemia in mice is strain dependent. J Cereb Blood Flow Metab. 2002;22:785–797. doi: 10.1097/00004647-200207000-00004. [DOI] [PubMed] [Google Scholar]
- Lambertsen KL, Meldgaard M, Ladeby R, Finsen B. A quantitative study of microglial-macrophage synthesis of tumor necrosis factor during acute and late focal cerebral ischemia in mice. J Cereb Blood Flow Metab. 2005;25:119–135. doi: 10.1038/sj.jcbfm.9600014. [DOI] [PubMed] [Google Scholar]
- Lang D, Knop J, Wesche H, Raffetseder U, Kurrle R, Boraschi D, Martin MU. The type II IL-1 receptor interacts with the IL-1 receptor accessory protein: a novel mechanism of regulation of IL-1 responsiveness. J Immunol. 1998;161:6871–6877. [PubMed] [Google Scholar]
- Lavine SD, Hofman FM, Zlokovic BV. Circulating antibody against tumor necrosis factor-alpha protects rat brain from reperfusion injury. J Cereb Blood Flow Metab. 1998;18:52–58. doi: 10.1097/00004647-199801000-00005. [DOI] [PubMed] [Google Scholar]
- Lehrmann E, Christensen T, Zimmer J, Diemer NH, Finsen B. Microglial and macrophage reactions mark progressive changes and define the penumbera in the rat neocortex and striatum after transient midddle cerebral artery occlusion. J Comp Neurol. 1997;386:41–476. [PubMed] [Google Scholar]
- Liu S, Levine SR, Winn HR. Targeting ischemic penumbra: part I - from pathophysiology to therapeutic strategy. J Exp Stroke Transl Med. 2010;3:47–55. doi: 10.6030/1939-067x-3.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T, Clark RK, McDonnell PC, Young PR, White RF, Barone FC, Feuerstein GZ. Tumor necrosis factor-alpha expression in ischemic neurons. Stroke. 1994;25:1481–1488. doi: 10.1161/01.str.25.7.1481. [DOI] [PubMed] [Google Scholar]
- Liu T, McDonnell PC, Young PR, White RF, Siren AL, Hallenbeck JM, Barone FC, Feurstein GZ.1993Interleukin-1 beta mRNA expression in ischemic rat cortex Stroke 241746–1750.discussion 1750–1751 [DOI] [PubMed] [Google Scholar]
- Lo EH. A new penumbra: transitioning from injury into repair after stroke. Nat Med. 2008;14:497–500. doi: 10.1038/nm1735. [DOI] [PubMed] [Google Scholar]
- Loddick SA, Rothwell NJ. Neuroprotective effects of human recombinant interleukin-1 receptor antagonist in focal cerebral ischaemia in the rat. J Cereb Blood Flow Metab. 1996;16:932–940. doi: 10.1097/00004647-199609000-00017. [DOI] [PubMed] [Google Scholar]
- Loddick SA, Turnbull AV, Rothwell NJ. Cerebral interleukin-6 is neuroprotective during permanent focal cerebral ischemia in the rat. J Cereb Blood Flow Metab. 1998;18:176–179. doi: 10.1097/00004647-199802000-00008. [DOI] [PubMed] [Google Scholar]
- Luheshi NM, Kovács KJ, Lopez-Castejon G, Brough D, Denes A. Interleukin-1α expression precedes Il-1β after ischemic injury and is localised to areas of focal neuronal loss and penumbral tissues. J Neuroinflamm. 2012;8:186. doi: 10.1186/1742-2094-8-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas MB, Furie KL. Molecular biomarkers in stroke diagnosis and prognosis. Biomark Med. 2009;3:363–383. doi: 10.2217/bmm.09.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchetti L, Klein M, Schlett K, Pfizenmaier K, Eisel UL. Tumor necrosis factor (TNF)-mediated neuroprotection against glutamate-induced excitotoxicity is enhanced by N-methyl-D-aspartate receptor activation. Essential role of a TNF receptor 2-mediated phosphatidylinositol 3-kinase-dependent NF-kappa B pathway. J Biol Chem. 2004;279:32869–32881. doi: 10.1074/jbc.M311766200. [DOI] [PubMed] [Google Scholar]
- Matsuda S, Wen TC, Morita F, Otsuka H, Igase K, Yoshimura H, Sakanaka M. Interleukin-6 prevents ischemia-induced learning disability and neuronal and synaptic loss in gerbils. Neurosci Lett. 1996;204:109–112. doi: 10.1016/0304-3940(96)12340-5. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Goodman Y, Luo H, Fu W, Furukawa K. Activation of NF-kappaB protects hippocampal neurons against oxidative stress-induced apoptosis: evidence for induction of manganese superoxide dismutase and suppression of peroxynitrite production and protein tyrosine nitration. J Neurosci Res. 1997;49:681–697. doi: 10.1002/(SICI)1097-4547(19970915)49:6<681::AID-JNR3>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Mazzotta G, Sarchielli P, Caso V, Paciaroni M, Floridi A, Gallai V. Different cytokine levels in thrombolysis patients as predictors for clinical outcome. Eur J Neurol. 2004;11:377–381. doi: 10.1111/j.1468-1331.2004.00798.x. [DOI] [PubMed] [Google Scholar]
- McColl BW, Allan SM, Rothwell NJ. Systemic infection, inflammation and acute ischemic stroke. Neuroscience. 2009;158:1049–1061. doi: 10.1016/j.neuroscience.2008.08.019. [DOI] [PubMed] [Google Scholar]
- McCoy MK, Tansey MG. TNF signaling inhibition in the CNS: implications for normal brain function and neurodegenerative disease. J Neuroinflammation. 2008;5:45. doi: 10.1186/1742-2094-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moidunny S, Dias RB, Wesseling E, Sekino Y, Boddeke HW, Sebastiao AM, Biber K. Interleukin-6-type cytokines in neuroprotection and neuromodulation: oncostatin M, but not leukemia inhibitory factor, requires neuronal adenosine A1 receptor function. J Neurochem. 2010;114:1667–1677. doi: 10.1111/j.1471-4159.2010.06881.x. [DOI] [PubMed] [Google Scholar]
- Montaner J, Rovira A, Molina CA, Arenillas JF, Ribó M, Chacón P, Monasterio J, Alvarez-Sabín J. Plasmatic level of neuroinflammatory markers predict the extent of diffusion-weighted image lesions in hyperacute stroke. J Cereb Blood Flow Metab. 2003;23:1403–1407. doi: 10.1097/01.WCB.0000100044.07481.97. [DOI] [PubMed] [Google Scholar]
- Mulcahy NJ, Ross J, Rothwell NJ, Loddick SA. Delayed administration of interleukin-1 receptor antagonist protects against transient cerebral ischaemia in the rat. Br J Pharmacol. 2003;140:471–476. doi: 10.1038/sj.bjp.0705462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakanishi M, Niidome T, Matsuda S, Akaike A, Kihara T, Sugimoto H. Microglia-derived interleukin-6 and leukaemia inhibitory factor promote astrocytic differentiation of neural stem/progenitor cells. Eur J Neurosci. 2007;25:649–658. doi: 10.1111/j.1460-9568.2007.05309.x. [DOI] [PubMed] [Google Scholar]
- Nawashiro H, Martin D, Hallenbeck JM. Inhibition of tumor necrosis factor and amelioration of brain infarction in mice. J Cereb Blood Flow Metab. 1997a;17:229–232. doi: 10.1097/00004647-199702000-00013. [DOI] [PubMed] [Google Scholar]
- Nawashiro H, Martin D, Hallenbeck JM. Neuroprotective effects of TNF binding protein in focal cerebral ischemia. Brain Res. 1997b;778:265–271. doi: 10.1016/s0006-8993(97)00981-5. [DOI] [PubMed] [Google Scholar]
- Nawashiro H, Tasaki K, Ruetzler CA, Hallenbeck JM. TNF-alpha pretreatment induces protective effects against focal cerebral ischemia in mice. J Cereb Blood Flow Metab. 1997c;17:483–490. doi: 10.1097/00004647-199705000-00001. [DOI] [PubMed] [Google Scholar]
- Nophar Y, Kemper O, Brakebusch C, Englemann H, Zwang R, Aderka D, Holtmann H, Wallach D. Soluble forms of tumor necrosis factor receptors (TNF-Rs). The cDNA for the type I TNF-R, cloned using amino acid sequence data of its soluble form, encodes both the cell surface and a soluble form of the receptor. EMBO J. 1990;9:3269–3278. doi: 10.1002/j.1460-2075.1990.tb07526.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Offner H, Vandenbark AA, Hurn PD. Effect of experimental stroke on peripheral immunity: CNS ischemia induces profound immunosuppression. Neuroscience. 2009;158:1098–111. doi: 10.1016/j.neuroscience.2008.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtaki H, Takaki A, Yin L, Dohi K, Nakamachi T, Matsunaga M, Horai B, Asano M, Iwakura Y, Shoida S. Suppression if oxidative stress after transient focal ischemia in interleukin-1 knock out mice. Acta Neurochir Suppl. 2003;86:191–194. doi: 10.1007/978-3-7091-0651-8_41. [DOI] [PubMed] [Google Scholar]
- Ohtaki H, Yin L, Nakamachi T, Dohi K, Kudo Y, Makino R, Shioda S. Expression of tumor necrosis factor alpha in nerve fibers and oligodendrocytes after transient focal ischemia in mice. Neurosci Lett. 2004;368:162–166. doi: 10.1016/j.neulet.2004.07.016. [DOI] [PubMed] [Google Scholar]
- Ormstad H, Aass HC, Lund-Sorensen N, Amthor KF, Sandvik L. Serum levels of cytokines and C-reactive protein in acute ischemic stroke patients, and their relationship to stroke lateralization, type, and infarct volume. J Neurol. 2011;258:677–685. doi: 10.1007/s00415-011-6006-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker LC, Luheshi GN, Rothwell NJ, Pinteaux E. IL-1 beta signaling in glial cells in wildtype and IL-1RI deficient mice. Br J Pharmacol. 2002;136:312–320. doi: 10.1038/sj.bjp.0704715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perini F, Morra M, Alecci M, Galloni E, Marchi M, Toso V. Temporal profile of serum anti-inflammatory and pro-inflammatory interleukins in acute ischemic stroke patients. Neurol Sci. 2001;22:289–296. doi: 10.1007/s10072-001-8170-y. [DOI] [PubMed] [Google Scholar]
- Pinteaux E, Rothwell NJ, Boutin H. Neuroprotective action of endogenous interleukin-1 receptor antagonist (IL-1ra) are mediated by glia. Glia. 2006;53:551–556. doi: 10.1002/glia.20308. [DOI] [PubMed] [Google Scholar]
- Pradillo JM, Romera C, Hurtado O, Cardenas A, Moro MA, Leza JC, Davalos A, Castillo J, Lorenzo P, Lizasoain I. TNFR1 upregulation mediates tolerance after brain ischemic preconditioning. J Cereb Blood Flow Metab. 2005;25:193–203. doi: 10.1038/sj.jcbfm.9600019. [DOI] [PubMed] [Google Scholar]
- Relton JK, Martin D, Thompson RC, Russell DA. Peripheral administration of Interleukin-1 Receptor antagonist inhibits brain damage after focal cerebral ischemia in the rat. Exp Neurol. 1996;138:206–213. doi: 10.1006/exnr.1996.0059. [DOI] [PubMed] [Google Scholar]
- Rivers CS, Wardlaw JM, Armitage PA, Bastin ME, Carpenter TK, Cvoro V, Hand PJ, Dennis MS. Persistent infarct hyperintensity on diffusion-weighted imaging late after stroke indicates heterogeneous, delayed, infarct evolution. Stroke. 2006;37:1418–1423. doi: 10.1161/01.STR.0000221294.90068.c4. [DOI] [PubMed] [Google Scholar]
- Romera C, Hurtado O, Botella SH, Lizasoain I, Cardenas A, Fernandez-Tome P, Leza JC, Lorenzo P, Moro MA. In vitro ischemic tolerance involves upregulation of glutamate transport partly mediated by the TACE/ADAM17-tumor necrosis factor-alpha pathway. J Neurosci. 2004;24:1350–1357. doi: 10.1523/JNEUROSCI.1596-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sairanen T, Carpen O, Karjalainen-Lindsberg ML, Paetau A, Turpeinen U, Kaste M, Lindsberg PJ. Evolution of cerebral tumor necrosis factor-alpha production during human ischemic stroke. Stroke. 2001;32:1750–1758. doi: 10.1161/01.str.32.8.1750. [DOI] [PubMed] [Google Scholar]
- Saper CB, Sawchenko PE. Magic peptides, magic antibodies: guidelines for appropriate controls for immunohistochemistry. J Comp Neurol. 2003;465:161–163. doi: 10.1002/cne.10858. [DOI] [PubMed] [Google Scholar]
- Scheller J, Rose-John S. Interleukin-6 and its receptor: from bench to bedside. Med Microbiol Immunol. 2006;195:173–183. doi: 10.1007/s00430-006-0019-9. [DOI] [PubMed] [Google Scholar]
- Schielke GP, Yang GY, Shivers BD, Betz AL. Reduced ischemic brain injury in interleukin-1 beta converting enzyme-deficient mice. J Cereb Blood Flow Metab. 1998;18:180–185. doi: 10.1097/00004647-199802000-00009. [DOI] [PubMed] [Google Scholar]
- Schindler R, Mancilla J, Endres S, Ghorbani R, Clark SC, Dinarello CA. Correlations and interactions in the production of interleukin-6 (IL-6), IL-1, and tumor necrosis factor (TNF) in human blood mononuclear cells: IL-6 suppresses IL-1 and TNF. Blood. 1990;75:40–47. [PubMed] [Google Scholar]
- Schwamm LH, Koroshetz WJ, Sorensen AG, Wang B, Copen WA, Budzik R, Rordorf G, Buonanno FS, Schaefer PW, Gonzalez RG. Time course of lesion development in patients with acute stroke: serial diffusion- and hemodynamic-weighted magnetic resonance imaging. Stroke. 1998;29:2268–2276. doi: 10.1161/01.str.29.11.2268. [DOI] [PubMed] [Google Scholar]
- Sharp FR, Jickling GC, Stamova B, Tian Y, Zhan X, Liu D, Kuczynski B, Cox CD, Ander BP. Molecular markers and mechanisms of stroke: RNA studies of blood in animals and humans. J Cereb Blood Flow Metab. 2011;31:1513–1531. doi: 10.1038/jcbfm.2011.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simi A, Tsakiri N, Wang P, Rothwell NJ. Interleukin-1 and inflammatory neurodegeneration. Biochem Soc Trans. 2007;35:1122–1126. doi: 10.1042/BST0351122. [DOI] [PubMed] [Google Scholar]
- Smith CJ, Emsley HC, Gavin CM, Georgiou RF, Vail A, Barberan EM, del Zoppo GJ, Hallenbeck JM, Rothwell NJ, Hopkins SJ, Tyrrell PJ. Peak plasma interleukin-6 and other peripheral markers of inflammation in the first week of ischaemic stroke correlate with brain infarct volume, stroke severity and long-term outcome. BMC Neurol. 2004;4:2. doi: 10.1186/1471-2377-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommer C.2010Histology and infarct volume determination Rodent Models of Stroke Vol. 47(Dirnagl U, ed)Springer New York Dordrecht Heidelberg London: Humana Press; 213–226. [Google Scholar]
- Sotgiu S, Zanda B, Marchetti B, Fois ML, Arru G, Pes GM, Salaris FS, Arru A, Pirisi A, Rosati G. Inflammatory biomarkers in blood of patients with acute brain ischemia. Eur J Neurol. 2006;13:505–513. doi: 10.1111/j.1468-1331.2006.01280.x. [DOI] [PubMed] [Google Scholar]
- St Pierre M, Reeh PW, Zimmermann K. Differential effects of TRPV channel block on polymodal activation of rat cutaneous nociceptors in vitro. Exp Brain Res. 2009;196:31–44. doi: 10.1007/s00221-009-1808-3. [DOI] [PubMed] [Google Scholar]
- Sun Y, Lu CJ, Lin CH, Wen LL. Interleukin-1beta is increased in the cerebrospinal fluid of patients with small infarcts. Eur J Neurol. 2009;16:858–863. doi: 10.1111/j.1468-1331.2009.02609.x. [DOI] [PubMed] [Google Scholar]
- Suzuki S, Tanaka K, Nogawa S, Nagata E, Ito D, Dembo T, Fukuuchi Y. Temporal profile and cellular localization of interleukin-6 protein after focal cerebral ischemia in rats. J Cereb Blood Flow Metab. 1999;19:1256–1262. doi: 10.1097/00004647-199911000-00010. [DOI] [PubMed] [Google Scholar]
- Suzuki S, Tanaka K, Suzuki N. Ambivalent aspects of interleukin-6 in cerebral ischemia: inflammatory versus neurotrophic aspects. J Cereb Blood Flow Metab. 2009;29:464–479. doi: 10.1038/jcbfm.2008.141. [DOI] [PubMed] [Google Scholar]
- Suzuki S, Yamashita T, Tanaka K, Hattori H, Sawamoto K, Okano H, Suzuki N. Activation of cytokine signaling through leukemia inhibitory factor receptor (LIFR)/gp130 attenuates ischemic brain injury in rats. J Cereb Blood Flow Metab. 2005;25:685–693. doi: 10.1038/sj.jcbfm.9600061. [DOI] [PubMed] [Google Scholar]
- Taoufik E, Valable S, Muller GJ, Roberts ML, Divoux D, Tinel A, Voulgari-Kokota A, Tseveleki V, Altruda F, Lassmann H, Petit E, Probert L. FLIP(L) protects neurons against in vivo ischemia and in vitro glucose deprivation-induced cell death. J Neurosci. 2007;27:6633–6646. doi: 10.1523/JNEUROSCI.1091-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarkowski E, Rosengren L, Blomstrand C, Wikkelso C, Jensen C, Ekholm S, Tarkowski A. Early intrathecal production of interleukin-6 predicts the size of brain lesion in stroke. Stroke. 1995;26:1393–1398. doi: 10.1161/01.str.26.8.1393. [DOI] [PubMed] [Google Scholar]
- Tarkowski E, Rosengren L, Blomstrand C, Wikkelso C, Jensen C, Ekholm S, Tarkowski A. Intrathecal release of pro- and anti-inflammatory cytokines during stroke. Clin Exp Immunol. 1997;110:492–499. doi: 10.1046/j.1365-2249.1997.4621483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thacker MA, Clark AK, Marchand F, McMahon SB. Pathophysiology of peripheral neuropathic pain: immune cells and molecules. Anesth Analg. 2007;105:838–847. doi: 10.1213/01.ane.0000275190.42912.37. [DOI] [PubMed] [Google Scholar]
- Thornton P, McColl MW, Greenhalgh A, Denes A, Allan SM, Rothwell NJ. Platelet interleukin-1α drives cerebrovascular inflammation. Blood. 2010;115:3632–3639. doi: 10.1182/blood-2009-11-252643. [DOI] [PubMed] [Google Scholar]
- Tilg H, Trehu E, Atkins MB, Dinarello CA, Mier JW. Interleukin-6 (IL-6) as an anti-inflammatory cytokine: induction of circulating IL-1 receptor antagonist and soluble tumor necrosis factor receptor p55. Blood. 1994;83:113–118. [PubMed] [Google Scholar]
- Tomimoto H, Akiguchi I, Wakita H, Kinoshita A, Ikemoto A, Nakamura S, Kimura J. Glial expression of cytokines in the brains of cerebrovascular disease patients. Acta Neuropathol. 1996;92:281–287. doi: 10.1007/s004010050519. [DOI] [PubMed] [Google Scholar]
- Touzani O, Boutin H, LeFeuvre R, Parker L, Miller A, Luheshi G, Rothwell N. Interleukin-1 influences ischemic brain damage in the mouse independently of the interleukin-1 type I receptor. J Neurosci. 2002;22:38–43. doi: 10.1523/JNEUROSCI.22-01-00038.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vila N, Castillo J, Davalos A, Chamorro A. Proinflammatory cytokines and early neurological worsening in ischemic stroke. Stroke. 2000;31:2325–2329. doi: 10.1161/01.str.31.10.2325. [DOI] [PubMed] [Google Scholar]
- Vitkovic L, Bockaert J, Jacque C. ‘Inflammatory' cytokines: neuromodulators in normal brain. J Neurochem. 2000;74:457–471. doi: 10.1046/j.1471-4159.2000.740457.x. [DOI] [PubMed] [Google Scholar]
- Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL, Marinovich M. Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci. 2003;23:8692–8700. doi: 10.1523/JNEUROSCI.23-25-08692.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waje-Andreassen U, Krakenes J, Ulvestad E, Thomassen L, Myhr KM, Aarseth J, Vedeler CA. IL-6: an early marker for outcome in acute ischemic stroke. Acta Neurol Scand. 2005;111:360–365. doi: 10.1111/j.1600-0404.2005.00416.x. [DOI] [PubMed] [Google Scholar]
- Wang X, Feuerstein GZ, Xu L, Wang H, Schumacher WA, Ogletree ML, Taub R, Duan JJ, Decicco CP, Liu RQ. Inhibition of tumor necrosis factor-alpha-converting enzyme by a selective antagonist protects brain from focal ischemic injury in rats. Mol Pharmacol. 2004;65:890–896. doi: 10.1124/mol.65.4.890. [DOI] [PubMed] [Google Scholar]
- Wang X, Li X, Currie RW, Willette RN, Barone FC, Feuerstein GZ. Application of real-time polymerase chain reaction to quantitate induced expression of interleukin-1beta mRNA in ischemic brain tolerance. J Neurosci Res. 2000;59:238–246. doi: 10.1002/(sici)1097-4547(20000115)59:2<238::aid-jnr10>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Wang X, Yue TL, Barone FC, White RF, Gagnon RC, Feuerstein GZ. Concomitant cortical expression of TNF-alpha and IL-1 beta mRNAs follows early response gene expression in transient focal ischemia. Mol Chem Neuropathol. 1994;23:103–114. doi: 10.1007/BF02815404. [DOI] [PubMed] [Google Scholar]
- Wang X, Yue TL, Young PR, Barone FC, Feuerstein GZ. Expression of interleukin-6, c-fos, and zif268 mRNAs in rat ischemic cortex. J Cereb Blood Flow Metab. 1995;15:166–171. doi: 10.1038/jcbfm.1995.18. [DOI] [PubMed] [Google Scholar]
- Weinstein PR, Hong S, Sharp FR. Molecular identification of the ischemic penumbra. Stroke. 2004;35:2666–2670. doi: 10.1161/01.STR.0000144052.10644.ed. [DOI] [PubMed] [Google Scholar]
- Whiteley W, Jackson C, Lewis S, Lowe G, Rumley A, Sandercock P, Wardlaw J, Dennis M, Sudlow C. Inflammatory markers and poor outcome after stroke: a prospective cohort study and systematic review of interleukin-6. PLoS Med. 2009;6:e1000145. doi: 10.1371/journal.pmed.1000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamasaki Y, Matsuura N, Shozuhara H, Onodera H, Itoyama Y, Kogure K.1995Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats Stroke 26676–680.discussion 681 [DOI] [PubMed] [Google Scholar]
- Yang GY, Gong C, Qin Z, Liu XH, Lorris Betz A. Tumor necrosis factor alpha expression produces increased blood-brain barrier permeability following temporary focal cerebral ischemia in mice. Brain Res Mol Brain Res. 1999;69:135–143. doi: 10.1016/s0169-328x(99)00007-8. [DOI] [PubMed] [Google Scholar]
- Yang GY, Gong C, Qin Z, Ye W, Mao Y, Bertz AL. Inhibition of TNFalpha attenuates infarct volume and ICAM-1 expression in ischemic mouse brain. Neuroreport. 1998;9:2131–2134. doi: 10.1097/00001756-199806220-00041. [DOI] [PubMed] [Google Scholar]
- Yin L, Ohtaki H, Nakamachi T, Kudo Y, Makino R, Shioda S. Delayed expressed TNFR1 co-localize with ICAM-1 in astrocyte in mice brain after transient focal ischemia. Neurosci Lett. 2004;370:30–35. doi: 10.1016/j.neulet.2004.07.083. [DOI] [PubMed] [Google Scholar]
- Zaremba J, Losy J. Early TNF-alpha levels correlate with ischaemic stroke severity. Acta Neurol Scand. 2001;104:288–295. doi: 10.1034/j.1600-0404.2001.00053.x. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Chopp M, Powers C. Temporal profile of microglial response following transient (2 hours) middle cerebral artery occlusion. Brain Res. 1997;744:189–198. doi: 10.1016/S0006-8993(96)01085-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.