Abstract
Prostate cancer is the most commonly diagnosed cancer among men in developed countries.1 One in six males in the US2 and one in nine males in the UK3 will develop the disease at some point during their lifetime. Despite advances in prostate cancer screening, more than a quarter million men die from the disease every year1 due primarily to treatment-resistance and metastasis. Colloidal nanotechnologies can provide tremendous enhancements to existing targeting/treatment strategies for prostate cancer to which malignant cells are less sensitive. Here, we show that antiandrogen gold nanoparticles – multivalent analogues of antiandrogens currently used in clinical therapy for prostate cancer – selectively engage two distinct receptors, androgen receptor (AR), a target for the treatment of prostate cancer, as well as a novel G-protein coupled receptor, GPRC6A, that is also upregulated in prostate cancer. These nanoparticles selectively accumulated in hormone-insensitive and chemotherapy-resistant prostate cancer cells, bound androgen receptor with multivalent affinity, and exhibited greatly enhanced drug potency versus monovalent antiandrogens currently in clinical use. Further, antiandrogen gold nanoparticles selectively stimulated GPRC6A with multivalent affinity, demonstrating that the delivery of nanoscale antiandrogens can also be facilitated by the transmembrane receptor in order to realize increasingly selective, increasingly potent therapy for treatment-resistant prostate cancers.
Androgen deprivation therapy (ADT) is currently recommended for the treatment of advanced/metastatic prostate cancer.4 Nonsteroidal antiandrogens such as flutamide (Eulexin®), bicalutamide (Casodex®), and nilutamide (Nilandron®) are some of the most commonly prescribed ADT drugs and diminish androgenic effects by competitively inhibiting androgen-androgen receptor binding associated with prostate cancer growth, division, and survival. While most advanced or metastatic prostate cancers initially respond well to ADT, malignant cells that survive 2–3 years will typically enter an antiandrogen-resistant5 (i.e. castration-resistant) state and subsequently exhibit chemotherapy-resistance as well.6 Without further intervention, median survival following this period is just 18–24 months. Increasingly selective and potent drugs are urgently needed to treat these prostate cancers.
Nanoscale drug conjugates can provide improved targeting selectivity for prostate cancer treatments via multivalent ligand display (augmented affinity and avidity) and size-dependent passive accumulation;7 they can also realize increasing potency through high drug loading capacity and enhanced intracellular transport rates (endocytosis versus passive diffusion).8 Langer, Farokhzad, and Lippard have shown that PLGA nanoparticles targeted with aptamers toward prostate-specific membrane antigen can deliver platinum prodrug chemotherapeutics to prostate cancer cells with substantially greater drug potency than untargeted carriers or cisplatin alone.9, 10 Folate-targeted lipid nanoparticles have also been applied in gene therapy11 and RNA interference12 for prostate cancer in vivo. Katti and Kannan have shown that gold nanoparticles targeted with bombesin peptides directed toward gastrin-releasing peptide receptor (overexpressed on prostate cancer cells) selectively target prostate cancer cells in vitro/vivo with multivalent affinity and can provide enhanced contrast for x-ray computed tomography (CT) imaging.13 Neoadjuvant administration of gold nanoparticles has been further shown to sensitize prostate cancer cells towards external beam radiation therapy14 and to facilitate in vivo laser photothermal ablation therapy in animal models of prostate cancer.15
We hypothesized that derivatives of commercially-available antiandrogen chemotherapeutics could serve as combined targeting and therapeutic agents for tissue-selective drug delivery of nanoscale drug carriers to prostate cancers expressing membrane androgen receptor16, 17 and/or a recently deorphaned androgen-sensing G protein-coupled receptor, GPRC6A,18 involved in increased prostate cancer risk, growth, and poor survival. We found that antiandrogen gold nanoparticles selectively target and engage both androgen receptor and GPRC6A with multivalent affinity and facilitate cell death in antiandrogen treatment-resistant prostate cancer cells at substantially lower concentrations than their corresponding free drugs. Per ligand, antiandrogen gold nanoparticles bound androgen receptor with affinity 5- to 11-times greater than free antiandrogens, and per particle, bound androgen receptor with affinity superior to endogenous androgens, providing opportunities for further increased treatment efficacy via drug co-conjugation, laser photothermal ablation, radiotherapy sensitization, and imaging-based treatment guidance/monitoring.8, 19
Gold nanoparticles (AuNPs, 29 ± 4 nm diameter, Figure 1a) were synthesized by Turkevich/Frens reduction of chloroauric acid and conjugated with a mixed self-assembled monolayer of 5% thiol PEGylated antiandrogen and 95% thiolated poly(ethylene glycol) stabilizer (PEG-SH, 5 kDa). Antiandrogen ligands used in these studies were employed to reflect structural homology between antiandrogens in clinical use with α- and β-Bicalutamide (α-Bic, β-Bic; Figure 1a) both bearing an aromatic α-anilide ring characteristic of flutamide, bicalutamide, and nilutamide, as well as a five-membered imidazolidinedione ring characteristic of nilutamide and the H-bonded structure of bicalutamide and/or the active metabolite of flutamide. β-Bic contains an additional β-aromatic ring characteristic of bicalutamide which binds the hydrophobic pocket formed by helix 12 residues on androgen receptor and confers it enhanced potency20 (Figure 1b). Antiandrogen ligands were synthesized by Cu(I)-catalyzed Huisgen cycloaddition (i.e. click, azide-alkyne coupling) with PEGylated lipoic acid. Thiol anchoring groups were used to enable stable Au surface bond formation and PEG stabilizer/spacer groups were employed to sterically stabilize the subsequent nanoparticle constructs in physiological media and to resist protein adsorption and/or diminish immunogenic response. α-Bic- and β-Bic-AuNPs contained 2.25 ± 0.02 × 103 and 1.56 ± 0.08 × 103 antiandrogen ligands per particle, respectively (See Supplementary Information for detailed experimental methods; Scheme S1, Figure S1).
Figure 1. Multivalent antiandrogen gold nanoparticles for the treatment of castration-resistant prostate cancer.
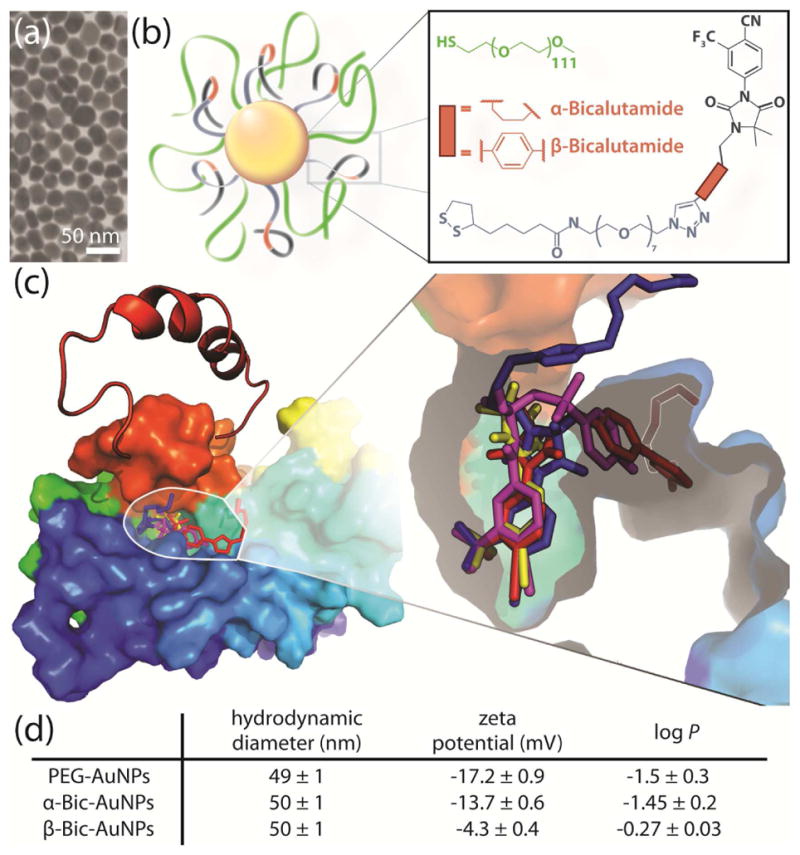
a, Electron micrographs of the as-synthesized 29 ± 4 nm diameter gold nanoparticles. b, Illustration of the antiandrogen nanoconjugates with receptor binding groups shown in gray/red. c, Molecular docking of the antiandrogen ligands with androgen receptor showing outward orientation of the thiol PEGylated nanoparticle linker groups and maintenance of contact points within the androgen receptor binding pocket by the bicalutamide ligand (β-Bic, red) and its β ring-deficient analogue (α-Bic, blue), as compared to their precursor drugs bicalutamide (magenta) and its nilutamide analogue (yellow). d, Physiochemical properties of the antiandrogen gold nanoparticles.
α-Bic and β-Bic AuNPs were found to be 50 ± 1 nm in hydrodynamic diameter, which recent studies by Chan and coworkers indicate to the be within the optimal size range for both tumor accumulation and cellular internalization of AuNPs21, 22 (Figure 1d). PEGylated control nanoparticles were found to be 49 ± 1 nm. The octanol:water partition coefficient of α-Bic- and β-Bic-AuNPs was found to be −1.4 ± 0.2 and −0.27 ± 0.03, respectively, both below that expected from an intravenously administered drug (1.92) with acceptable pharmacokinetics.23
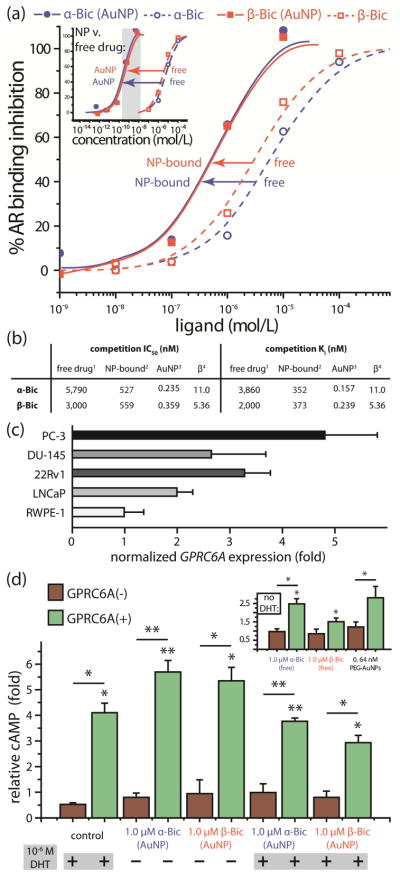
Molecular docking of the antiandrogen ligands with androgen receptor (AR) show that the contact points of their parent drugs within the AR binding pocket are maintained by the ligands and that their thiol PEGylated linker groups face outward to enable accessibility by nanoparticle-bound ligands (Figure 1c).24 Receptor binding competition with radiolabeled androgen (Figure 2a) shows that the AR binding inhibition constant (Ki) of α-Bic and β-Bic is enhanced 11- and 5.4-fold per drug molecule, respectively, when displayed as a multivalent construct, with total nanoparticle AR binding affinity exceeding that of its endogenous hormone dihydroxytestosterone (DHT, 0.28 – 2 nM v. 0.16 – 0.24 nM nanoparticles)20, 25 and yielding, to the best of our knowledge, the highest reported nanoparticle Ki for a non-steroidal antiandrogen (Figure 2a inset, Figure 2b). Free α-Bic- and β-Bic bound AR with affinities comparable to those previously reported for bicalutamide26. Because membrane AR (mAR) binds antibodies16 and endogenous androgens27 for intracellular AR, and because antiandrogens can diminish the effects of androgenic mAR stimulation,28 these data suggest that antiandrogen gold nanoparticles can selectively target mAR which is preferentially overexpressed by human prostate cancer cells and whose expression levels correlate with poor prognosis (Gleason score)29 and total AR levels16 found in 80–90% of all prostate cancers.30
Figure 2. Antiandrogen gold nanoparticles selectively engage androgen receptor (AR) and G protein-coupled receptor GPRC6A targets.
a, AR binding competition between radiolabeled androgen and nanoparticle-bound antiandrogens (solid) or free antiandrogens (dashed) showing multivalency-enhanced AR binding affinity (Ki) from the nanoparticle constructs. Nanoparticle-bound antiandrogens displaced [3H]androgen from AR with 5.4–11 fold greater per-ligand affinity than an equivalent concentration of free antiandrogens. Inset, Nanoparticle and free drug concentrations. b, Half maximal inhibitory concentration (IC50) and binding inhibition constant (Ki) for free1 and nanoparticle-bound2 antiandrogens, nanoparticles3, and their corresponding (per-drug-molecule) multivalency-enhanced values (β4). c, Upregulated GPRC6A mRNA expression levels measured from various prostate cancer cell lines relative to non-malignant RWPE-1 prostate cells (See Supporting Information). d, Androgen-competitive downstream production of cyclic adenosine monophosphate (cAMP) second messenger accumulated in response to overnight stimulation of GPRC6A signal transduction by α-Bic-and β-Bic-AuNPs in an AR−/GPRC6A− and AR−/GPRC6A+ transfected cell line. Inset, Fold-change in GPRC6A signal transduction (cAMP accumulation) in response to GPRC6A stimulation by nanoparticle-equivalent concentrations of free α-Bic/β-Bic and PEGylated control nanoparticles showing significantly lower GPRC6A engagement/stimulation by free α-Bic (2.3-fold, P=0.003), β-Bic (3.5-fold, P=0.03), and PEGylated gold nanoparticles (2.0-fold v. α-Bic-AuNPs, P=0.06; 1.9-fold v. β-Bic-AuNPs, P=0.15) relative to their respective particle constructs. cAMP levels from PEG-AuNPs were comparable to those observed from DHT-abrogated α-Bic/β-Bic-AuNPs indicating antiandrogen ligand-enhanced GPRC6A engagement. Note that GPRC6A is a promiscuous receptor for androgenic ligands and that the cell lines in (d) are AR null. DHT, dihydrotestosterone. Grayscale area in (a) denotes the lower and upper limits previously reported for AR’s endogenous high affinity ligand, dihydrotestosterone (DHT). Error bars represent SEM. P for individual values relative to untreated controls or as indicated; *P<0.05, **P<0.01.
GPRC6A31 is a membrane-associated C family G protein-coupled receptor recently discovered32 through genomic homology search. We have previously shown that GPRC6A senses androgens and is a positive regulator of testosterone and a negative regulator of estrogen production in mice;18 its expression was also found to contribute to prostate cancer growth, malignancy, and poor survival in animal models of prostate cancer.18 Polymorphism at the GPRC6A gene locus was recently associated with significantly altered susceptibility to prostate cancer in a genome-wide association study among Japanese men (P=1.6 × 10−12).18, 33 Here, we found that GPRC6A overexpression strongly correlates malignant phenotype across several prostate cell lines (Figure 2c). Although Pi et al. recently found that androgens selectively stimulate GPRC6A and subsequently promote prostate cancer cell growth,34 we hypothesized that high affinity antiandrogens and multivalent antiandrogen gold nanoparticles may similarly engage GPRC6A, albeit with subsequently diminished cell growth (vide supra) rather than agonist-induced proliferation. Downstream production of the second messenger, cyclic adenosine monophosphate (cAMP), accumulated in response to stimulated GPRC6A signal transduction, was assessed using an established AR−/GPRC6A− and AR−/GPRC6A+ transfected cell line (See Supplementary Information).34 α-Bic- and β-Bic-AuNPs significantly stimulated GPRC6A in an androgen-competitive manner (Figure 2d), eliciting cAMP production at low μM ligand (sub-nM AuNP) concentrations. GPRC6A stimulation by α-Bic- and β-Bic-AuNPs was 2.0- and 1.9-fold greater than that by an equivalent or greater concentration of PEGylated-AuNPs (P=0.06 & 0.15, respectively) and was 2.3- and 3.5-fold greater than their nanoparticle-equivalent concentrations of free antiandrogen ligands (P=0.003 & 0.03, respectively) (Figure 2d inset). GPRC6A stimulation by PEG-AuNPs was nearly equivalent to that observed from testosterone-abrogated α-Bic- and β-Bic-AuNPs, indicating GPRC6A ligand-enhanced activity from antiandrogen-AuNPs. Together, these data show that antiandrogen gold nanoparticles can selectively engage GPRC6A with multivalent affinity and can do so in a manner independent of AR/mAR expression (Figure 2d).
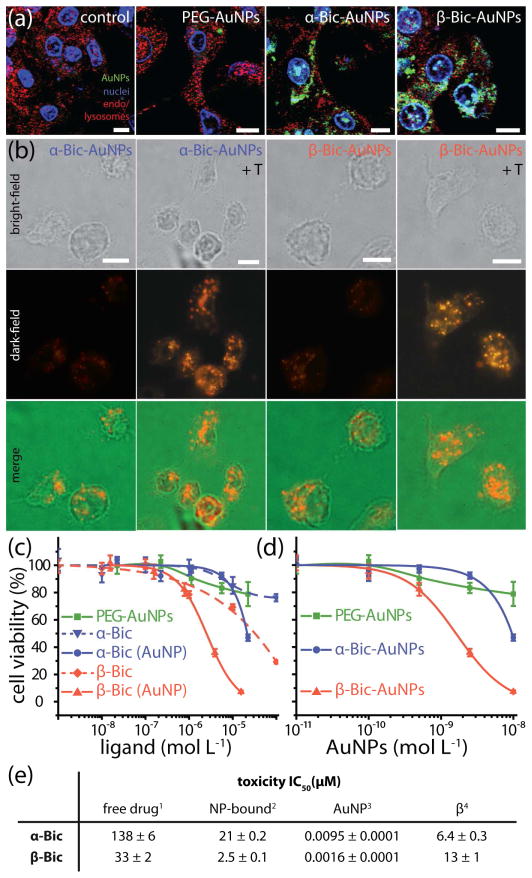
Binding/uptake selectivity of the antiandrogen gold nanoparticles was assessed in a membrane-AR+ and GPRC6A+ prostate carcinoma cell line27 whose response to chemotherapy and antiandrogen therapy reflects that of castration-resistant prostate cancer,6 DU-145 (Figure 3a). Fluorescently-labeled antiandrogen gold nanoparticles exhibited high intracellular accumulation in DU-145 cells and localized in a manner similar to that reported for AR,35 while PEGylated nanoparticles exhibited no significant accumulation. Uptake and localization patterns of both targeted and untargeted nanoparticles in an AR null36 squamous cell carcinoma cell line showed only non-specific cell surface binding (Supplementary Figure S2). We hypothesized that androgen-stimulated upregulation of AR in DU-145,37 and correspondingly increased mAR expression,16 may augment antiandrogen nanoparticle accumulation in prostate cancer cells. Particle uptake/localization was imaged using cardioid immersion optical dark-field scattering microscopy which can achieve sensitivity orders of magnitude higher than conventional fluorescence-based methods.8, 19 Testosterone (T, 10−6 M) stimulation of DU-145 had no effect on PEGylated nanoparticle accumulation (Supplementary Information Figure S3), but significantly increased α-Bic- and β-Bic-AuNP accumulation. These findings are consistent with previous reports demonstrating 1.5–2 fold upregulation of androgen receptor expression following testosterone stimulation in DU-14537 and concomitant increases in membrane-AR traslocation16 (Figure 3b). These imaging data show that antiandrogen gold nanoparticles selectively accumulate in antiandrogen treatment-resistant AR+/GPRC6A+ prostate cancer cells and can also do so in an AR-/mAR-dependent manner.
Figure 3. Antiandrogen gold nanoparticles selectively accumulate in chemotherapy- and antiandrogen-resistant prostate cancer cells expressing membrane-androgen receptor (mAR) and G protein-coupled receptor GPRC6A and induce cell death with multivalency-enhanced drug potency.
a, Confocal fluorescence images of selective antiandrogen nanoparticle intracellular localization (green) in mAR+/GPRC6A+ DU-145 prostate cancer cells. Endo/lysosomes were labeled with dextran (red) and nuclei were stained with DAPI (blue). b, Optical dark-field scattering microscopy of DU-145 cells showing augmented antiandrogen gold nanoparticle accumulation in response to androgen-stimulated mAR-upregulation by testosterone (T, 10−6 M). Note that images in (a) and (b) were obtained using different instruments. c, Dose-dependent cell viability (%) of antiandrogen treatment-resistant DU-145 prostate cancer cells incubated with free antiandrogens and ligand-equivalent concentrations of antiandrogen gold nanoparticles (24 h). d, Total nanoparticle concentrations represented in c. e, Figures of merit for cytotoxicity of the free drug1, nanoparticle-bound ligand2, and multivalent nanoparticle 3, as well as the multivalency enhancement factor β4 exhibiting 6.4- and 13-fold enhanced potency per drug molecule. Scale bars represent 10 μm. Error bars represent SD.
Cytotoxicity of the antiandrogen nanoparticles and their ligands to chemotherapy- and antiandrogen-resistant6 mAR+/GPRC6A+ DU-145 prostate carcinoma cells was investigated by tetrazolium assay (24 h, See Supporting Information). AuNP-bound α-Bic- and β-Bic induced half maximal cytotoxicity (IC50) at 21 and 2.5 μM ligand concentrations, respectively, exhibiting per-molecule potency 6.4- and 13-fold greater than their corresponding free drugs, respectively (Figure 3c–e). Free α-Bic- and β-Bic cytotoxicity was comparable to that previously reported for bicalutamide and OH-flutamide with DU-145,38 while nanoparticle-equivalent concentrations of PEGylated gold nanoparticles exhibited no significant toxicity over therapeutically-relevant antiandrogen-AuNP concentrations. Unlike androgenic GPRC6A agonists which we have previously shown induce cell proliferation,34 antiandrogen-AuNPs stimulate GPRC6A while diminishing cell proliferation (Fig 3c–e) and also maintaining antagonist activity toward androgen receptor (Fig 2a, b). Together, these data correlate selective AR and GPRC6A engagement (vide infra) with enhanced drug potency and cell death by antiandrogen gold nanoparticles.
In summary, we found that antiandrogen gold nanoparticles selectively engaged two distinct receptors involved in prostate cancer growth and progression. These particles selectively accumulated in castration- and chemotherapy-resistant prostate cancer cells and induced cell death at nanomolar particle concentrations, and enhanced the potency of antiandrogens currently in clinical use by roughly one order of magnitude. Further, antiandrogen gold nanoparticles antagonized androgen receptor with multivalent affinity and selectively engaged a newly discovered transmembrane G-protein coupled receptor, GPRC6A, involved in prostate carcinogenesis and disease risk. These platforms provide opportunities for increasingly potent and selective therapy for treatment-resistant prostate cancers and may exhibit further enhanced therapeutic efficacy via drug co-conjugation, image-based treatment guidance/monitoring, concurrent laser photothermal ablation therapy, and/or high-Z enhanced radiotherapy.
Supplementary Material
Acknowledgments
This work was supported by the U.S. National Institutes of Health (1U01CA151802-01, MAE; R01CA131217, AKO; R01-AR37308, LDQ). The authors also thank Dr. Jian Hui Wu for providing the apo homology model of AR.
ABBREVIATIONS
- α-Bic
α-Bicalutamide ligand
- β-Bic
β-Bicalutamide ligand
- ADT
androgen deprivation therapy
- AR
androgen receptor
- AuNP
gold nanoparticle
- cAMP
cyclic adenosine monophosphate
- DAPI
4′,6-diamidino-2-phenylindole
- DHT
dihydrotestosterone
- IC50
half maximal concentration
- mAR
membrane androgen receptor
- PEG
poly(ethylene glycol)
- T
testosterone
Footnotes
Author Disclosures
The authors declare no competing financial interests other than those disclosed. L.D.Q. is a consultant to Amgen, KAI Pharmaceuticals and Shire; he has also been a paid speaker for Amgen.
Antiandrogen ligand synthesis; nanoparticle synthesis, conjugation, and characterization; docking methods, cell culture/in vitro analysis, radioligand binding, GPRC6A expression/stimulation, and imaging methods. This material is available free of charge via the Internet at http://pubs.acs.org.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Ward E, Brawley O, Jemal A. Cancer Statistics, 2011. CA Cancer J Clin. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 3.Statistics on the risk of developing cancer. [accessed 7 December, 2011];Cancer Research UK. http://info.cancerresearchuk.org/cancerstats/incidence/risk/
- 4.Chen Y, Clegg NJ, Scher HI. Anti-androgens and androgen-depleting therapies in prostate cancer: new agents for an established target. Lancet Oncol. 2009;10:981–991. doi: 10.1016/S1470-2045(09)70229-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Attar RM, Takimoto CH, Gottardis MM. Castration-Resistant Prostate Cancer: Locking Up the Molecular Escape Routes. Clin Cancer Res. 2009;15:3251–3255. doi: 10.1158/1078-0432.CCR-08-1171. [DOI] [PubMed] [Google Scholar]
- 6.Borsellino N, Belldegrun A, Bonavida B. Endogenous Interleukin 6 Is a Resistance Factor for cis-Diamminedichloroplatinum and Etoposide-mediated Cytotoxicity of Human Prostate Carcinoma Cell Lines. Cancer Res. 1995;55:4633–4639. [PubMed] [Google Scholar]
- 7.Dreaden EC, Mwakwari SC, Sodji QH, Oyelere AK, El-Sayed MA. Tamoxifen-Poly(ethylene glycol)-Thiol Gold Nanoparticle Conjugates: Enhanced Potency and Selective Delivery for Breast Cancer Treatment. Bioconjugate Chem. 2009;20:2247–2253. doi: 10.1021/bc9002212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dreaden EC, Alkilany AM, Huang X, Murphy CJ, El-Sayed MA. The Golden Age: Gold Nanoparticles for Biomedicine. Chem Soc Rev. 2012;41:2740–2779. doi: 10.1039/c1cs15237h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhar S, Gu FX, Langer R, Farokhzad OC, Lippard SJ. Targeted delivery of cisplatin to prostate cancer cells by aptamer functionalized Pt(IV) prodrug-PLGA–PEG nanoparticles. Proc Natl Acad Sci USA. 2008;105:17356–17361. doi: 10.1073/pnas.0809154105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhar S, Kolishetti N, Lippard SJ, Farokhzad OC. Targeted delivery of a cisplatin prodrug for safer and more effective prostate cancer therapy in vivo. Proc Natl Acad Sci USA. 2011 doi: 10.1073/pnas.1011379108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hattori Y, Maitani Y. Folate-linked nanoparticle-mediated suicide gene therapy in human prostate cancer and nasopharyngeal cancer with herpes simplex virus thymidine kinase. Cancer Gene Ther. 2005;12:796–809. doi: 10.1038/sj.cgt.7700844. [DOI] [PubMed] [Google Scholar]
- 12.Xue HY, Wong HL. Solid Lipid–PEI Hybrid Nanocarrier: An Integrated Approach To Provide Extended, Targeted, and Safer siRNA Therapy of Prostate Cancer in an All-in-One Manner. ACS Nano. 2011;5:7034–7047. doi: 10.1021/nn201659z. [DOI] [PubMed] [Google Scholar]
- 13.Chanda N, Kattumuri V, Shukla R, Zambre A, Katti K, Upendran A, Kulkarni RR, Kan P, Fent GM, Casteel SW, Smith CJ, Boote E, Robertson JD, Cutler C, Lever JR, Katti KV, Kannan R. Bombesin functionalized gold nanoparticles show in vitro and in vivo cancer receptor specificity. Proc Natl Acad Sci USA. 2010;107:8760–8765. doi: 10.1073/pnas.1002143107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roa W, Zhang X, Guo L, Shaw A, Hu X, Xiong Y, Gulavita S, Patel S, Sun X, Chen J, Moore R, Xing JZ. Gold nanoparticle sensitize radiotherapy of prostate cancer cells by regulation of the cell cycle. Nanotechnol. 2009;20:375101. doi: 10.1088/0957-4484/20/37/375101. [DOI] [PubMed] [Google Scholar]
- 15.Stern JM, Stanfield J, Kabbani W, Hsieh JT, Cadeddu JA. Selective Prostate Cancer Thermal Ablation With Laser Activated Gold Nanoshells. J Urology. 2008;179:748–753. doi: 10.1016/j.juro.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Pedram A, Razandi M, Sainson RCA, Kim JK, Hughes CC, Levin ER. A conserved mechanism for steroid receptor translocation to the plasma membrane. J Biol Chem. 2007;282:22278–22288. doi: 10.1074/jbc.M611877200. [DOI] [PubMed] [Google Scholar]
- 17.Hatzoglou A, Kampa M, Kogia C, Charalampopoulos I, Theodoropoulos PA, Anezinis P, Dambaki C, Papakonstanti EA, Stathopoulos EN, Stournaras C, Gravanis A, Castanas E. Membrane Androgen Receptor Activation Induces Apoptotic Regression of Human Prostate Cancer Cells in Vitro and in Vivo. J Clin Endocrinol Metab. 2005;90:893–903. doi: 10.1210/jc.2004-0801. [DOI] [PubMed] [Google Scholar]
- 18.Pi M, Quarles LD. GPRC6A regulates prostate cancer progression. Prostate. 2011;72:399–409. doi: 10.1002/pros.21442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dreaden EC, Mackey MA, Huang X, Kang B, El-Sayed MA. Beating cancer in multiple ways using nanogold. Chem Soc Rev. 2011;40:3391–3404. doi: 10.1039/c0cs00180e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bohl CE, Gao W, Miller DD, Bell CE, Dalton JT. Structural basis for antagonism and resistance of bicalutamide in prostate cancer. Proc Natl Acad Sci USA. 2005;102:6201–6206. doi: 10.1073/pnas.0500381102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang W, Kim BYS, Rutka JT, Chan WCW. Nanoparticle-mediated cellular response is size-dependent. Nat Nanotechnol. 2008;3:145–150. doi: 10.1038/nnano.2008.30. [DOI] [PubMed] [Google Scholar]
- 22.Perrault SD, Walkey C, Jennings T, Fischer HC, Chan WCW. Mediating Tumor Targeting Efficiency of Nanoparticles Through Design. Nano Lett. 2009;9:1909–1915. doi: 10.1021/nl900031y. [DOI] [PubMed] [Google Scholar]
- 23.Obach RS, Lombardo F, Waters NJ. Trend Analysis of a Database of Intravenous Pharmacokinetic Parameters in Humans for 670 Drug Compounds. Drug Metab Dispos. 2008;36:1385–1405. doi: 10.1124/dmd.108.020479. [DOI] [PubMed] [Google Scholar]
- 24.Zhou J, Liu B, Geng G, Wu JH. Study of the impact of the T877A mutation on ligand-induced helix-12 positioning of the androgen receptor resulted in design and synthesis of novel antiandrogens. Proteins. 2010;78:623–637. doi: 10.1002/prot.22592. [DOI] [PubMed] [Google Scholar]
- 25.He Y, Yin D, Perera M, Kirkovsky L, Stourman N, Li W, Dalton JT, Miller DD. Novel nonsteroidal ligands with high binding affinity and potent functional activity for the androgen receptor. Euro J Med Chem. 2002;37:619–634. doi: 10.1016/s0223-5234(02)01335-1. [DOI] [PubMed] [Google Scholar]
- 26.Kirkovsky L, Mukherjee A, Yin D, Dalton JT, Miller DD. Chiral Nonsteroidal Affinity Ligands for the Androgen Receptor. 1 Bicalutamide Analogues Bearing Electrophilic Groups in the B Aromatic Ring1. J Med Chem. 2000;43:581–590. doi: 10.1021/jm990027x. [DOI] [PubMed] [Google Scholar]
- 27.Papadopoulou N, Charalampopoulos I, Anagnostopoulou V, Konstantinidis G, Foller M, Gravanis A, Alevizopoulos K, Lang F, Stournaras C. Membrane androgen receptor activation triggers down-regulation of PI-3K/Akt/NF-kappaB activity and induces apoptotic responses via Bad, FasL and caspase-3 in DU145 prostate cancer cells. Mol Cancer. 2008;7 doi: 10.1186/1476-4598-7-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu S, Papadopoulou N, Gehring EM, Nasir O, Dimas K, Bhavsar S, Föller M, Alevizopoulos K, Lang F, Stournaras C. Functional membrane androgen receptors in colon tumors trigger pro-apoptotic responses in vitro and reduce drastically tumor incidence in vivo. Mol Cancer. 2009;8:1–14. doi: 10.1186/1476-4598-8-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kampa M, Kogia C, Theodoropoulos PA, Anezinis P, Charalampopoulos I, Papakonstanti EA, Stathopoulos EN, Hatzoglou A, Stournaras C, Gravanis A, Castanas E. Activation of membrane androgen receptors potentiates the antiproliferative effects of paclitaxel on human prostate cancer cells. Mol Cancer Ther. 2006;5:1342–1351. doi: 10.1158/1535-7163.MCT-05-0527. [DOI] [PubMed] [Google Scholar]
- 30.Heinlein CA, Chang C. Androgen Receptor in Prostate Cancer. Endocr Rev. 2004;25:276–308. doi: 10.1210/er.2002-0032. [DOI] [PubMed] [Google Scholar]
- 31.Schuh-Huerta SM, Pera RAR. Reproductive biology: Bone returns the favour. Nature. 2011;472:46–47. doi: 10.1038/472046a. [DOI] [PubMed] [Google Scholar]
- 32.Wellendorph P, Bräuner-Osborne H. Molecular cloning, expression, and sequence analysis of GPRC6A, a novel family C G-protein-coupled receptor. Gene. 2004;335:37–46. doi: 10.1016/j.gene.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 33.Takata R, Akamatsu S, Kubo M, Takahashi A, Hosono N, Kawaguchi T, Tsunoda T, Inazawa J, Kamatani N, Ogawa O, Fujioka T, Nakamura Y, Nakagawa H. Genome-wide association study identifies five new susceptibility loci for prostate cancer in the Japanese population. Nat Genetics. 2010;42:751–754. doi: 10.1038/ng.635. [DOI] [PubMed] [Google Scholar]
- 34.Pi M, Parrill AL, Quarles LD. GPRC6A Mediates the Non-genomic Effects of Steroids. J Biol Chem. 2010;285:39953–39964. doi: 10.1074/jbc.M110.158063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whitaker HC, Hanrahan S, Totty N, Gamble SC, Waxman J, Cato ACB, Hurst HC, Bevan CL. Androgen Receptor Is Targeted to Distinct Subcellular Compartments in Response to Different Therapeutic Antiandrogens. Clin Cancer Res. 2004;10:7392–7401. doi: 10.1158/1078-0432.CCR-04-0388. [DOI] [PubMed] [Google Scholar]
- 36.Virolainen E, Vanharanta R, Carey TE. Steroid hormone receptors in human squamous carcinoma cell lines. Int J Cancer. 1984;33:19–25. doi: 10.1002/ijc.2910330105. [DOI] [PubMed] [Google Scholar]
- 37.Alimirah F, Chen J, Basrawala Z, Xin H, Choubey D. DU-145 and PC-3 human prostate cancer cell lines express androgen receptor: Implications for the androgen receptor functions and regulation. FEBS Lett. 2006;580:2294–2300. doi: 10.1016/j.febslet.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 38.Kreis W, Budman DR, Calabro A. A reexamination of PSC 833 (Valspodar) as a cytotoxic agent and in combination with anticancer agents. Cancer Chemother Pharmacol. 2001;47:78–82. doi: 10.1007/s002800000191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.