Abstract
Objective
To ascertain whether a parent education program based on Satter’s division of responsibility in feeding children (DOR) is effective in enhancing parent/child feeding interactions for children with an overweight/obese parent. The primary hypothesis was that the intervention would decrease parental pressure to eat.
Methods
Sixty-two families with a child aged 2–4 years with at least one overweight/obese parent were randomly allocated using a cluster design to either the DOR intervention or a control group. The control group focused on increasing family consumption of healthy foods and activity levels, and enhancing child sleep duration. The primary outcome was parent pressure on their child to eat.
Results
The DOR intervention was superior to the control group in reducing pressure to eat. Two moderators of pressure to eat were found: disinhibition of eating and hunger. DOR group parents irrespective of disinhibition levels lowered pressure to eat whereas control group parents with low disinhibition increased pressure to eat. There were similar findings for hunger. Gender moderated restrictive feeding with DOR parents lowering restriction more than the control group in girls only.
Conclusion
The DOR intervention was more effective in reducing parent pressure to eat and food restriction (in girls only) than the control group.
Keywords: child feeding problems, pressure to eat, restrictive feeding, responsive feeding, Satter method
The increase in US childhood overweight/obesity over the past 20-years across all income and ethnic groups in the USA 1,2 underlines the need for early prevention programs to reduce the increasingly prevalent and costly medical comorbidities associated with overweight.3 To date, however, prevention programs which are often implemented in school settings have met with only moderate success 4 perhaps because the family environment continues to reinforce maladaptive behaviors. At the family level parent feeding practices, such as taking excessive control over their child’s eating, appear to contribute to childhood overweight. 5,6 It is hypothesized that these parental behaviors interfere with the child’s perception of hunger and satiety leading to loss of control over eating and eventually to overweight.
Family studies suggest that restrictive feeding by the parent is related to childhood overweight although the majority of these studies are cross-sectional.6,7 Laboratory studies also suggest that restrictive feeding is associated with childhood overweight. For example, when children have restricted access to a specific food they tend to eat more of that food in a later test, although this finding was for girls but not boys.8 On the other hand if children are pressured to eat a healthy food, in this case by making play contingent on consuming a particular food, their preference for that food will diminish in subsequent tests.9 Observational studies also demonstrate the importance of parental behavior on children’s feeding. For example, higher rates of parent food offers, presentations, and prompts, all measures of pressure to eat, were associated with higher caloric intake in young children in a laboratory setting.10 Another study found that higher rates of parental prompts to eat and food offers were associated with higher child relative weights.11 It can be argued that parental control over their child’s eating is simply a reaction to their child’s feeding problems. However, a prospective study from birth to 7 years of age found that parental attributes at infancy predicted over-control at 7-years.12 Such attributes included: Parental body dissatisfaction, parental eating disorders, minority status and parents being born outside the United States. This study indicates that parental over-control of their child’s feeding is not simply a reaction to an existing feeding problem.
Thus parent behaviors particularly restricting food choices are risk factors for overweight. However, to determine whether changing these behaviors affect weight gain in young children, i.e. are causal risk factors, an evidence-based intervention to reduce parental over-control during mealtimes is first needed. A child development-based feeding relationship model, Division of Responsibility, formalized by Satter 13,14 has been used to foster optimal feeding practices. The American Academy of Pediatrics recommends the model during child health supervision visits 15 However, this model has not been tested in a controlled trial, hence it is unclear whether it actually reduces parent attempts to control their child’s eating. The aim of this study was to compare, in a randomized trial, an intervention based on the Satter model which is aimed at reducing parental interference during feeding, to a control group adapted from the “We Can” program developed by the National Institutes of Health which is aimed at enhancing family nutrition and activity levels.16 The children involved in the study were at risk for overweight or obesity because at least one parent was overweight or obese.
METHODS
Design
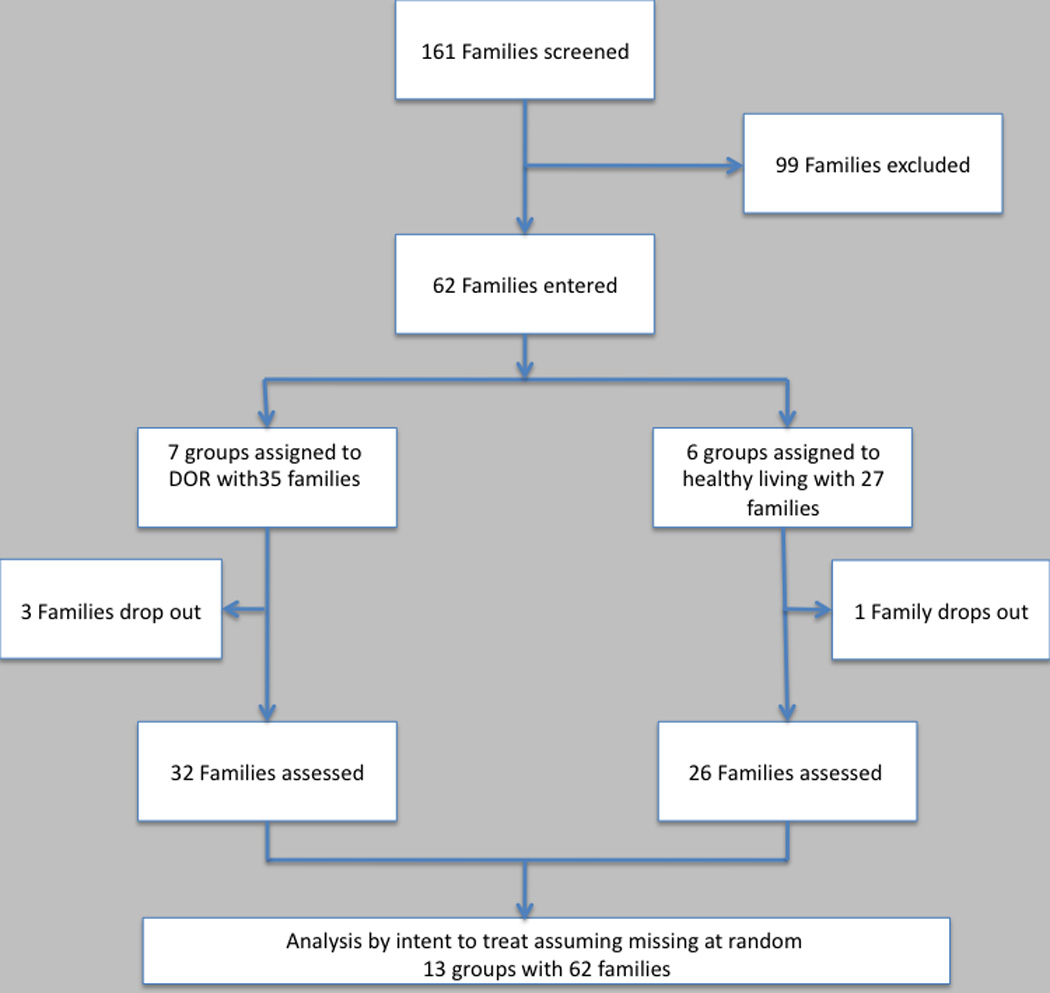
A cluster design was used in which participants were allocated in the order in which they were entered to the study to a small group. The group was then randomized to one of the two interventions (see Figure 1). Each group met weekly for five sessions, each session lasting about 1-hour. Both parents were invited to the groups but usually only one parent attended. Children were not involved directly in the study because the study was aimed at changing parent behaviors.
Figure 1.
Participants
The participants were 62 families with a child aged 2–4 years. At least one parent was overweight/obese with a Body Mass Index (BMI) greater than 28 kg/M2. Participants were recruited from several sources including: Pre-schools, mothers clubs, Santa Clara County WIC clinics, and internet sources such as Craig’s list and the study website. All parents had to speak and understand English in order to complete the assessments and take part in the interventions. Parent exclusions were ongoing serious illness such as cancer, or serious psychiatric illness such as schizophrenia, uncontrolled bipolar disorder, mental retardation, that would prevent participation in the assessments or interventions. Children’s exclusions included: Serious physical illness or related treatments that would affect feeding or weight including a history of feeding aversion, failure to thrive, prematurity below 37-weeks associated with prolonged hospitalization, ongoing need for nutritional supplementation; serious current developmental problems including any that might interfere with self-feeding or require additional parental feeding support (e.g., developmental delay, autism).
Parents were told that we were studying the comparative effectiveness of two different methods that may help to prevent childhood overweight. The study was approved by the Stanford University Institutional Review Board. All potential participants signed a consent form.
Interventions
Three therapists treated groups in both conditions to reduce therapist bias. The therapists were clinical psychology graduate students with experience as therapists. They read the treatment manuals, which were then discussed with them in several preliminary sessions ensuring mastery of the content and procedures. Each therapist then role-played situations likely to arise in both interventions. When they reached a satisfactory level of expertise they began leading groups. Each group session was audited (by WSA) the therapists were supervised in weekly sessions that included an expert (CD) in the DOR intervention. Feedback to the therapists was provided from the previous sessions recordings.
Division of Responsibility (DOR) intervention
The DOR program was based on the Satter model13,14 in which parents take responsibility for providing and serving food, maintaining a regular schedule of meals and snacks, and deciding where food is to be served including family meals, during which the child serves him or herself depending on age and skills. The child’s responsibilities are to decide whether or not to eat and how much to eat. The primary principle is that crossing parent or child boundaries leads to feeding problems. The intervention incorporates behavior change principles such as self-monitoring of behavior and progress, and making changes in small steps.
Control group
The ‘We Can’ program16 which has been tested in a number of community settings focuses on changing parental behaviors to increase the consumption of healthy foods by increasing intake of vegetables, decreasing fats and sweetened beverages, and increasing family exercise and decreasing TV and computer time. Results from nine sites suggest that the program is effective in changing attitudes and behaviors and no safety concerns were noted. In the light of recent findings concerning the relation between short sleep time and overweight, attention was also paid to regular and sufficient sleep,17,18 this is an addition to the original program. Because the original program targeted older children and their families the content, particularly activity levels and types and introduction of healthy foods, was adapted for the age group involved in this study. Behavior change procedures were also incorporated in this intervention. Hence, this group controls for the therapy mode, parental involvement and information and practice with behavior change procedures focused on the family and toddler involved in the study, similar to the DOR intervention, but does not target specific feeding behaviors such as pressure to eat and food restriction.
Outcome measures
The primary outcome measure was pressure to eat. Secondary outcome measures were food restriction and satisfaction with treatment. Both pressure to eat and food restriction were assessed using the Child Feeding Questionnaire (CFQ).19 The CFQ was developed to assess two broad categories of factors, (i) parent perceptions and concerns about their child’s risk of obesity and (ii) parent use of child feeding practices, particularly pressure to eat and food restriction.19 Responses range from unconcerned to extremely concerned on a five point Likert scale. Satisfaction with treatment was assessed using the Client Satisfaction Questionnaire (CSQ). The CSQ consists of 8 items each rated on a 4-point scale forming a global score. The internal consistency and reliability of the questionnaire is high as is its validity. 20
Descriptive variables were collected at baseline. Because children were not involved in this study the children’s ages were verified from their birth certificates. Parent birthplace, age, ethnicity and race, were collected and parent BMI measured using a balance beam scale that was calibrated daily. Other baseline data collected for descriptive purposes and to investigate possible moderators of outcome included the Three Factor Eating Questionnaire (TFEQ) used to assess parent dietary restraint, hunger and disinhibition of eating because these variables have been associated with children’s eating behaviors8,12. Disinhibition represents responses to food cues, with high disinhibition often associated with binge eating. Hunger refers to the parent’s habitual level of hunger, with high levels of hunger associated with lessened ability to control eating. The TFEQ consists of 36 items with a Yes/No format. 21 It has good internal consistency, and test-retest reliability over a one-month period is .90. A revised version of the Stanford Child Feeding Questionnaire (SCFQ-R) was used to assess parent/child feeding behaviors. This questionnaire was revised for this study from a previous version by removing items not applicable to the present study. 17 It consists of 62 questions about child/parent interactions and behaviors regarding feeding with a 7-point response scale ranging from Never (0) to Always. The questionnaire comprises 7 factors across parent behaviors, child behaviors, and meal patterns. For this study we chose to retain factors significantly correlated with the outcomes. Two child behavior factors which account for 55.4% of the variance were selected: Picky eating (38.7% of the variance) consisting of responses to 8 items such as “How difficult is it to get your child to eat new foods?” “Is your child a picky eater?” This subscale has been validated against observed behaviors22 Mealtime tantrums (16.7% of the variance) consisting of responses to two items “If your child wants something to eat and you say no how often does s/he become upset?” “How often does this cause a tantrum?” This subscale shows good test/retest reliability. Temperament style was assessed using the Child Behavior Questionnaire (CBQ) 23 developed by Rothbart to evaluate temperament in preschool and early school-age children. For this study temperament as perceived by the parent was assessed as the mean of 4 dimensions that have been related to childhood overweight24 (Anger/Frustration, Activity, Approach Anticipation, Impulsivity) using a 7-point range from “extremely untrue of your child” to “extremely true of your child.” The scales have good internal consistency with coefficient alphas ranging from 0.63 to 0.92, with a mean of 0.74. The scales are also relatively stable across periods as long as two years and have moderate to high levels of parental agreement. Temperament was assessed because it has been associated with child overweight in a previous studies.17,24 Therapist fidelity to the two treatment conditions was assessed by one of the investigators (wsa) auditing all audiotapes of the group sessions. A global score was used based on a 0–5 Likert scale from low to high fidelity.
Data analysis
A baseline comparison of treatment groups was used to determine the success of randomization; we utilized t-tests (for continuous variables) and chi-squared tests (for categorical variables). Spearman correlations were used to examine relationships between baseline behaviors and outcome measures. Because randomization occurred at the group level, analysis techniques were selected to appropriately model the data. Thus linear mixed modeling was employed where the group was the second level model, with the parent as the first level model. Baseline values were controlled for by using the baseline measure as a covariate. Effect sizes were calculated using Cohen’s d, correcting for cluster intraclass correlations. Analysis was by intent-to-treat. In addition a moderator analysis was performed. A moderator is a baseline variable that interacts with an outcome variable where the moderator divides the treatment group into two subgroups with different outcomes i.e., greater or lesser responsiveness to treatment. Exploratory moderator analysis using the methodology of Kraemer et al.25 suggests that all baseline (pre-randomization) measures (see Table 1) be considered as potential moderators. Moderators were determined for both outcome measures: parental pressure to eat and food restriction controlling for the baseline measure and using treatment, moderator, and interaction as the independent measures.
Table 1.
Baseline characteristics of the sample by intervention (N=61)
| DOR Program | Control group | |
|---|---|---|
| Paternal BMI | 29.2 (6.4) | 30.5 (6.0) |
| Paternal Age (years) | 38.2 (8.5) | 37.0 (7.6) |
| Maternal BMI | 32.8 (7.2) | 32.1 (8.1) |
| Maternal age (years) | 35.6 (6.1) | 38.4 (6.6) |
| Child age (months) | 40.5 (11.8) | 39.47 (10.0) |
|
Child Gender Male Female |
21 (64%) 12 (36%) |
14 (58%) 11 (42%) |
|
Paternal Ethnicity Not Hispanic Hispanic |
26 (84%) 5 (16%) |
16 (67%) 7 (33%) |
|
Paternal Race Native American Asian Black Pacific Islander Caucasian More than 1 race Did not answer |
0 (0%) 3 (9%) 3 (9%) 0 (0%) 21 (58%) 5 (15%) 1 (3%) |
1 (4%) 3 (12%) 1 (4%) 1 (4%) 15 (42%) 0 (0%) 4 (16%) |
| Parental disinhibitiona | 10.2 (3.1) | 8.9 (3.9) |
| Parental hungera | 7.8 (2.7) | 7.6 (3.7) |
| Parental restrainta | 7.5 (4.3) | 7.1 (3.7) |
| Child temperamentb | 59.2 (8.0) | 60.0 (8.8) |
| Child picky eatingc | 2.5 (1.3) | 2.5 (1.4) |
| Child mealtime tantrumsc | 3.3 (1.6) | 2.9 (1.7) |
| Parental pressure to eatd | 2.2 (1.0) | 2.6 (0.8) |
| Parental food restrictiond | 2.9 (0.8) | 2.8 (0.8) |
Three factor eating Questionnaire (possible range for disinhibition 0–16, hunger 0–14, restraint 0–21)
Child Behavior Questionnaire (possible range 4–91)
Stanford Child Feeding Questionnaire-R (possible range 0–7)
Child Feeding Questionnaire (possible range 0–5)
RESULTS
Demographics and baseline findings
Figure 1 shows the flow of participants into the study. Sixty-two families were entered, 35 to the DOR intervention and 27 to the control group. One family (3.7%) dropped out of the control intervention and three (8.5%) from the DOR intervention leaving 59 families who were assessed at end-of-treatment. On average fathers ages were (± SD) 37.6 ± 8.0 years and mothers ages averaged 36.8±6.4 years, with BMI’s of 29.8± 6.2 and 35.3 ± 7.6 respectively. Baseline characteristics by group are presented in Table 1. There were no statistically significant differences between treatment groups on any parent or child baseline variable. Hence, randomization appeared successful. Pressure to eat at baseline was correlated with the child’s temperament r=0.29, p<.05 and with picky eating r=0.54, p<.001. Food restriction at baseline was correlated with mealtime tantrums r=0.34, p<.01
Pressure to eat
The primary outcome, parent pressure on their child to eat, decreased significantly more in the DOR intervention than in the control group at end of treatment (F [1,10] = 26.0, p < 0.001) with a NNT=2 i.e. the number of families needed to treat to prevent one additional bad outcome. Two parent variables from the TFEQ moderated pressure to eat, namely disinhibition of eating and hunger. DOR parents irrespective of disinhibition scores decreased pressure to eat (low disinhibition parents decreased by 67%, high disinhibition parents by 59%) whereas parents with low disinhibition scores in the control group increased pressure to eat (low disinhibition parents increased by 33%, high disinhibition parents decreased by 33%) F(1,53)=7.5 p=.008. There was a similar pattern for hunger. DOR parents lowered pressure to eat irrespective of hunger levels (low hunger parents decreased by 57%, high hunger parents by 63%) whereas parents with low hunger in the control group increased pressure to eat (low hunger parents increased by 31%, high hunger parents decreased by36%) F(1,53)=4.1 p=.047.
Food restriction
Change in level of food restriction was not significantly different between the two groups. However, child gender moderated food restriction with parents of male children hardly decreasing food restriction (DOR males decreased by 20%, control males no change) whereas parents of female children decreased food restriction in the DOR intervention by 117% compared to the control group which decreased by19% F(1,50)=5.1 p=.029.
Therapist fidelity and client satisfaction
Mean therapist fidelity scores derived from auditing session tapes were 4.1± 1.2 for the DOR group and 4.3±1.3 for the control group on a 0–5 scale. Client satisfaction was not significantly different between the two groups at end of treatment.
DISCUSSION
In this randomized study of children with an overweight/obese parent an intervention aimed at improving child feeding practices was compared to a group focused on increasing physical activity and consumption of healthy foods. The first intervention was based on Satter’s model, the division of responsibilities between parents and children relating to feeding, whereas the control group was adapted from the NIH “We Can” program. The DOR intervention was superior to the control group in reducing parent pressure on their child to eat. A moderator analysis revealed that parents with low disinhibition and hunger, somewhat increased pressure on their child to eat in the control group. Hence, there is evidence that promoting consumption of healthy foods led to decrements in positive feeding practices. This may arise from parents pressuring their children to eat healthy foods. The two treatments appeared equally acceptable to the participating parents.
Gender also moderated outcome with parents of girls reducing food restriction more in the DOR group than in the control group. Parents of boys were not affected. It may be that parents are more focused on their female children’s eating patterns in line with the greater concern about female weight and shape.26,27
The main limitation of this study is the relatively small sample size, which may have minimized differences between the two treatments. A second limitation is the reliance on parent reporting of behavior change. For example, pressure to eat assessed by parent report is associated with reductions in intake28 whereas direct observations suggest that prompts to eat (an indication of parent pressure) are associated with increased caloric intake.10 Future research could strengthen these findings by incorporating direct observation of parent-child interactions during mealtime. A final limitation is that data on income and socioeconomic status were not collected for this study.
A recent Institute of Medicine policy statement 29 suggested that health and education professionals providing guidance to parents of young children and those working with young children should be trained and educated and have the right tools to increase children’s healthy eating and counsel parents about their children’s diet. Similarly, an expert panel selected from 15 organizations proposed four stages of obesity care; the first brief counseling delivered in a health care office with subsequent stages requiring more time and resources.30 This study suggests that the DOR program based on the Satter model13,14 may be an effective intervention, if brief physician counseling does not result in appropriate changes, to enable parents to enhance their management of child feeding in children at risk for overweight or obesity. Physician counseling could be based on the principles underlying the DOR intervention.
CONCLUSION
The DOR intervention based on the Satter developmental model of feeding was more effective in reducing parent pressure on their child to eat and restrictive feeding in girls than the control group. However, a larger longer-term study will be needed to establish whether modifying restrictive feeding and pressure to eat reduces the risk of overweight. The study also provides a note of caution that efforts to increase consumption of healthy foods in toddlers should include counseling to parents to model eating such foods and not to pressure children to eat them.
Table 2.
Estimated Means (standard errors) for the outcome variables by treatment group.
| DOR Intervention |
Healthy Living Intervention |
Baseline adjusted mean difference ‘DOR- Healthy Living (95% CI) |
t- value |
P | Effect size |
|
|---|---|---|---|---|---|---|
| Pressure to Eat | 1.6 (.10) | 2.4 (.12) | −.771 (−1.11 to −.435) | −5.10 | p<.001 | .88 |
| Food Restriction | 2.4 (.12) | 2.8 (.15) | −.338 (−.74 to .07) | −1.82 | NS | .44 |
| Client Satisfaction Questionnairea | 27.1 (.7) | 25.6 (.9) | 1.55 (−.74 to 3.85) | 1.36 | NS | .34 |
Scores range from 0–32
Acknowledgments
This study was supported in part by a grant HD055637 from the National Institute of Child Health and Development.
Footnotes
The authors have no conflict of interest regarding this paper.
REFERENCES
- 1.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Ogden CL, Yanovski JA, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91:1020–1026. doi: 10.3945/ajcn.2009.28589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: An updated systematic review of the literature. Obesity. 2009;18:S27–S35. doi: 10.1038/oby.2009.429. [DOI] [PubMed] [Google Scholar]
- 4.Summerbell C, Walters E, Edmunds L, Kelly S, Brown T, Campbell K. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD001871.pub2. Art No CD 001871. [DOI] [PubMed] [Google Scholar]
- 5.DiSantis KI, Hodges EA, Johnson SL, Fisher JO. The role of responsive feeding in overweight during infancy. Int J Obes (Lond) 2011;35:480–492. doi: 10.1038/ijo.2011.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hurley KM, Cross MB, Hughes SO. A systematic review of responsive feeding and child obesity in high income countries. J Nutr. 2011;141:495–501. doi: 10.3945/jn.110.130047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faith MS, Scanlon K, Birch LL, Francis LA, Sherry B. Parent-child feeding strategies and their relationship to child eating and weight status. Obes Res. 2004;12:1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- 8.Fisher JO, Birch LL. Restricting access to foods and children's eating. Appetite. 1999 Jun;32(3):405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- 9.Birch LL, Birch D, Marlin DW, Kramer L. Effects of instrumental consumption on children's food preference. Appetite. 1982;3:125–134. doi: 10.1016/s0195-6663(82)80005-6. [DOI] [PubMed] [Google Scholar]
- 10.Drucker RR, Hammer LD, Agras WS, Bryson S. Can mothers influence their child's eating behavior? Dev Behav Pediatr. 1999;20:88–92. doi: 10.1097/00004703-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Klesges RC, Coates TJ, Brown G, Sturgeon-Tillich J, Moldenhauer-Klesges LM, Holzer B, Woolfrey J, Vollmer J. Parental influences on children's eating behavior and relative weight. J Appl Behav Anal. 1983;16:371–378. doi: 10.1901/jaba.1983.16-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duke RE, Bryson S, Hammer LD, Agras WS. The relationship between parental factors at infancy and parent reported control of children's eating at age 7. Appetite. 2004;43:247–252. doi: 10.1016/j.appet.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Satter E. The feeding relationship: Problems and interventions. J Pediatr. 1990;117:S181–S189. doi: 10.1016/s0022-3476(05)80017-4. [DOI] [PubMed] [Google Scholar]
- 14.Satter E. The feeding relationship. J Am Diet Assoc. 1986;86:352–356. [PubMed] [Google Scholar]
- 15.Hagan JF, Shaw JS, Duncan PM, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children and Adolescents. Third edition. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 16.NHLBI. We Can! Progress report. Curriculum implementations by intensive sites. Washington, D.C.: National Institutes of Health; 2007. [Google Scholar]
- 17.Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. J Pediatr. 2004;145:20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 18.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–733. doi: 10.1016/j.pcl.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birch LL, Grimm-Thomas K, Markey CN, Sawyer R, Johnson MB. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs, and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 20.Larsen DL, Attkisson CC, Hargreaves WA. Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 21.Stunkard AJ, Messick S. The three factor eating questionnaire to measure dietary restraint, disinhibition, and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 22.Jacobi C, Agras WS, Bryson S, Hammer LD. Behavioral validation, precursors, and concomitants of picky eating in chldhood. J Am Academy Child Adolesc Psychiatry. 2003;42:76–84. doi: 10.1097/00004583-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The Childrens Behavior Questionnaire. Child Dev. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- 24.Mascola AJ, Agras WS. Perceived temperament and risk for development of overweight in children. Curr Nutr Food Science. 2006;2:15–22. [Google Scholar]
- 25.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 26.Agras WS, Bryson S, Hammer LD, Kraemer HC. Childhood risk factors for thin body preoccupation and social pressure to be thin. J Am Acad Child & Adol Psychiatry. 2007;46:171–178. doi: 10.1097/chi.0b013e31802bd997. [DOI] [PubMed] [Google Scholar]
- 27.Presnell K, Bearman SK, Stice E. Risk factors for body dissatisfaction in adolescent boys and girls: A prospective study. Int JEat Disord. 2003;36:389–401. doi: 10.1002/eat.20045. [DOI] [PubMed] [Google Scholar]
- 28.Ventura AK, Birch LL. Does parenting affect children's eating and weight status? Int J Behav NutrPhys Activity. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Early Childhood Obesity Prevention Policies. Institute of Medicine; 2011. [Google Scholar]
- 30.Barlow SE. Expert Committee Recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Supplement):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]


