Abstract
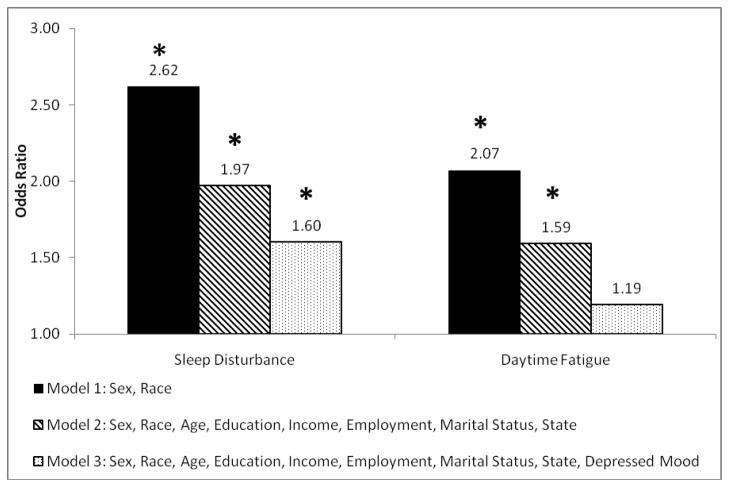
Perceived discrimination is a potential cause of racial and ethnic disparities in health. Disturbed sleep may serve as a mechanism linking perceived racism with health consequences. The current study investigates data from 7,148 adults from Michigan and Wisconsin who participated in the 2006 Behavioral Risk Factor Surveillance System. Hierarchical logistic regression analyses explored associations between perceived racial discrimination and self-reported sleep disturbance and daytime fatigue. Sleep Disturbance and Daytime Fatigue were reported in 19% and 21% of the sample, respectively. Black/African-American respondents (21%) report perceiving worse experience compared to people of other races when seeking health care at higher rates than Non-Hispanic White respondents (3%). Results from logistic regression models show that perceived racial discrimination is associated with increased risks of sleep disturbance (OR=2.62, p<.0001) and daytime fatigue (OR=2.07, p<.0001). After adjustment for all covariates, perceived discrimination remains a significant predictor of sleep disturbance (OR=1.60, p=.04). The interaction between perceived racism and race (Black/African-American vs. Non-Hispanic White) was non-significant. This population-based research adds to the growing body of data suggesting that perceived racism may impact health via its influence on sleep-wake behaviors.
In recent years, increasing attention has been drawn to health disparities between racial groups across many domains of health, particularly in comparing Non-Hispanic White and Black/African-American individuals (Freid, Prager, MacKay, & Xia, 2003; Levine et al., 2001; Piffath, Whiteman, Flaws, Fix, & Busht, 2001). A number of factors have been shown to play a role in these inequalities, including socioeconomic factors (Pickett & Pearl, 2001; Williams & Jackson, 2005; Williams, Neighbors, & Jackson, 2003), social environment (Williams & Collins, 2001), access to healthcare and other services (Smedley, Stith, & R., 2002; Weinick, Zuvekas, & Cohen, 2000), and psychosocial risk factors, including exposure to racial discrimination (Williams, et al., 2003).
Racial discrimination may negatively impact health by increasing exposure to chronic psychosocial stress, which has been implicated in a number of chronic health conditions (McEwen, 1998, 2007; McEwen & Seeman, 1999). Sleep disturbance, as a consequence of psychosocial stress, has been studied less extensively, though recent findings support the claim that stress in the social environment may negatively impact sleep (Aanes, Hetland, Pallesen, & Mittelmark, 2011; Geiger-Brown, Trinkoff, & Rogers, 2011; Grandner et al., 2010; Grandner, Patel, Hale, & Moore, 2010; Hale & Do, 2007; Hill, Burdette, & Hale, 2009; Patel, Grandner, Xie, Branas, & Gooneratne, 2010; Runeson, Lindgren, & Wahlstedt, 2011).
Many previous studies have shown that sleep disturbance (short sleep duration, long sleep duration, and/or poor sleep quality) is an independent predictor of mortality (Gallicchio & Kalesan, 2009; Grandner, Patel, Hale, et al., 2010; Kripke, Garfinkel, Wingard, Klauber, & Marler, 2002; Kripke, Langer, Elliott, Klauber, & Rex, 2011), including all-cause and disease-specific mortality. Large population-based studies have reported significant associations between sleep disturbance and many other negative health outcomes, including obesity, cardiovascular disease, heart attack, stroke, diabetes, depression, and substance abuse (Anic, Titus-Ernstoff, Newcomb, Trentham-Dietz, & Egan, 2010; Grandner, Patel, Gehrman, Perlis, & Pack, 2010; Hairston et al., 2010; Lyytikainen, Lallukka, Lahelma, & Rahkonen, 2010; Nielsen, Danielsen, & Sorensen, 2010; van Cauter & Leproult, 2010; Watanabe, Kikuchi, Tanaka, & Takahashi, 2010). Important determinants of sleep disturbance have included socioeconomic factors such as income, education, employment status, and marital status (Grandner, Patel, Gehrman, Xie, et al., 2010). These relationships interact with race to produce differential outcomes (Grandner, Patel, Gehrman, Xie, et al., 2010; Patel et al., 2010). This suggests that although patterns relating sleep disturbance to socioeconomic status were found, there are other race-related factors that play a role in these relationships.
Few previous studies have investigated whether perceived racial discrimination results in disturbed sleep. One study used a path analytic approach to explore the role of perceived racism in subjective and polysomnographic sleep outcomes (Thomas, Bardwell, Ancoli-Israel, & Dimsdale, 2006). Perceived racism was associated with less slow wave sleep (Stage 4 in particular) and more daytime fatigue. Additionally, this study found that those who identified more strongly with their ethnicity had longer sleep latencies. A study in Latinos found that sleep disturbance mediated the relationship between perceived racism and depressed mood (Steffen & Bowden, 2006). This evidence suggests that perceived racism may be related to sleep disturbance, which may, in turn, lead to other negative health consequences.
The present study explored how perceived racism relates to sleep disturbance and daytime fatigue. Previous studies that measured discrimination have not operationalized discrimination in a more specific setting. Accordingly, the present study evaluated perceived racial discrimination (treatment versus people of other races) in the healthcare setting, which provided the added benefit of being more directly relatable to health outcomes, and may also reflect institutionalized racism.
Our hypotheses were that perceived racism was an independent predictor of (1) sleep disturbance and (2) daytime fatigue. Furthermore, we investigated whether demographics, socioeconomic factors and depressed mood play a role in this relationship.
Method
Participants
We use data from the 2006 Behavioral Risk Factor Surveillance System (BRFSS)(Centers for Disease Control, 2007) for this analysis. The BRFSS is an annual, state-based, random-digit-dialed telephone interview survey of adults aged ≥18 years from all over the United States conducted by the Centers for Disease Control and Prevention. It is the world’s largest telephone survey, designed to monitor health-related behaviors in the general population. For the present analyses, data from Michigan and Wisconsin were included, since these were the only two states to collect both sleep and racism variables. The overall response rate (completed interviews relative to total eligible households) was 35.5% in Michigan and 48.7% in Wisconsin. The completion rate (number of interviews completed relative to the number of interviews completed, terminated, and/or refused) was 76.9% in Michigan and 79.5% in Wisconsin. All participants were treated in accordance with the principles expressed in the Declaration of Helsinki.
To increase generalizability of results, each participant was assigned a weight to be used in analysis. Thus, even though the sample is, by the nature of the sampling scheme, not representative of the general population, all analyses are adjusted so that biases in the sample do not contaminate results. The process of determining participant weighting is discussed in more detail in the BRFSS documentation. In brief, each weight is calculated using a combination of: (1) a weight which accounts for differences in the basic probability of selection among subsets of regions delineated by combinations of area code and telephone prefix, (2) a weight which adjusts for noncoverage and nonresponse, forcing the sum of all weighted frequencies to equal population estimates for that region, based on age, sex, and race/ethnicity, (3) the number of residential telephone lines in the participant’s home, and (4) the number of adults in the participant’s household. Thus, although the sample that was aggregated is not representative of the general population, each participant’s weight assures that all results are maximally generalizable, accounting for any noncoverage and/or nonresponse based on geographic region, as well as sociodemographic categories of age, sex and ethnicity.
Measures
Two states (Michigan and Wisconsin) collected data on perceived racism as part of the 2006 BRFSS. The current analyses utilized this data. Perceived racism was assessed with the question, “Within the past 12 months when seeking health care, do you feel your experiences were worse than, the same as, or better than for people of other races?” Response choices were dichotomized as either “Worse” (including “Worse than other races” and “Worse than some races, better than others”) and “Same” or “Better” (including “The same as other races” and “Better than other races”).
Participants also answered a question on Sleep Disturbance: “Over the last 2 weeks, how many days have you had trouble falling asleep or staying asleep or sleeping too much?” and Daytime Fatigue: “Over the last 2 weeks, how many days have you felt tired or had little energy?” Answers for both questions ranged from 0–14. However, the distributions were bimodal, with peaks at 0 and 14. Because of the non-normal distribution, these variables cannot be assessed as continuous variables without violating the assumptions of the statistical methods employed. Because the distribution is bimodal, linear transformations cannot be applied, and using absolute value would not be consistent with the hypotheses. Thus, Sleep Disturbance and Daytime Fatigue were dichotomized into those who report complaints ≥6 days and those who report complaints <6 days. This is consistent with other classification approaches where a frequency of three or more events per week has been used to denote abnormality (Jansson-Frojmark & Linton, 2008).
Covariates used to adjust for socioeconomic factors included age, sex, race/ethnicity (Non-Hispanic White vs. Black/African-American), education (less than high school, high school graduate, some college, college graduate), income level (<$10,000 pre-tax income per year, $10,000–$15,000, $15,000–$20,000, $20,000–$25,000, $25,000–$35,000, $35,000–$50,000, $50,000–$75,000, >$75000), marital status (married, never married, part of an unmarried relationship, divorced, separated, widowed), and employment (employed, self-employed, retired, student, homemaker, unemployed <1 year, unemployed >1 year, unable to work). Previous analyses of these data at the national level (including states other than Michigan and Wisconsin) have found that education, gender, employment and income are significant predictors of sleep complaint in this sample (Grandner, Patel, Gehrman, Xie, et al., 2010). Depressed mood was measured with the item, “Over the last 2 weeks, how many days have you felt down or depressed” which was assessed as a continuous variable.
Statistical Analyses
Complete-case analysis was implemented for both Sleep Disturbance and Daytime Fatigue; thus, only participants who provided complete data were included for each analysis. Of those with Sleep Disturbance and Daytime Fatigue responses, only 62 participants were excluded. Missing data analysis demonstrated that the missing group did not differ from those retained for analysis on any indicator except age, where those excluded were somewhat older than the rest of the sample (mean 68 vs. 51 years old, p<.05). To determine whether state (Michigan vs. Wisconsin) played a role in results, we assessed state differences in variables of interest and included state as a covariate and explored State*Racism and State*Race/Ethnicity*Racism interactions.
We estimated a series of logistic regression models for each of our two dichotomous outcomes of Sleep Disturbance and Daytime Fatigue. All sampling was weighted appropriately for representativeness, using weighting scores specifically developed for BRFSS 2006 (Centers for Disease Control, 2007). The odds ratios (ORs) and 95% confidence intervals (CIs) were estimated among groups relative to a preselected reference. Analyses were performed using STATA software Version 11 (StataCorp, College Station, TX). All statistical tests were two-tailed. Statistical significance was set at the p< 0.05 level. The reference for the Perceived Racism variable was the group that reported being treated the “Same or Better” so that the effect of perceived racism can be studied. Other variables studied included Education (reference = college graduate), Income (reference = >$75,000), Race/Ethnicity (separate dichotomous variables for Black/African-American or Non-Hispanic White), Employment (reference = Employed), and Depressed mood. A total of three separate models were tested: (1) Racism + Race/Ethnicity + Sex; (2) Racism + Race/Ethnicity + Sex + Age + Education + Income + Employment; (3) Racism + Race/Ethnicity + Sex + Age + Education + Income + Employment + Depression. We selected these models in order to examine perceived racism adjusting only for race/ethnicity and sex, and relative to sociodemographic covariates, with and without depressed mood.
As a post-hoc analysis, we explored Employment*Race/Ethnicity*Racism and Sex*Racism interactions, to determine whether the relationship between perceived racism and sleep-related outcomes depended on sex or employment status.
Results
Subject Characteristics
Characteristics of the sample are reported in Table 1. Prior to applying weights, the sample was majority female (60% among Non-Hispanic Whites and 68% among Black/African-Americans). Sleep Disturbance and Daytime Fatigue were reported in approximately 20% of the sample (19% and 21%, respectively), which is consistent with rates of reports of these complaints from the larger, national 2006 BRFSS sample (Grandner et al., 2009; Grandner, Patel, Gehrman, Xie, et al., 2010) and does not represent a difference between the Non-Hispanic White and Black/African-American groups. Perceived racism was reported by a minority of Non-Hispanic Whites (3%), and seven times as many Black/African-American (21%) participants; this represented a significant difference (p<0.001).
Table 1.
Characteristics of the Sample
| Variable | All (N=7093) | Non-Hispanic White (N=6469) | Black/African-American (N=624) | P |
|---|---|---|---|---|
| Age | ||||
| Mean (Standard Deviation) | 50.9 (15.6) | 51.3 (15.6) | 47.5 (15.2) | 0.02 |
| Sleep Disturbance | ||||
| Yes (%) | 18.86 | 18.36 | 24.04 | 0.47 |
| Daytime Fatigue | ||||
| Yes (%) | 21.33 | 20.93 | 25.48 | 0.72 |
| Perceived Racism | ||||
| Worse (%) | 4.78 | 3.25 | 20.67 | <0.001 |
| Sex | ||||
| Female (%) | 60.59 | 59.92 | 67.63 | 0.44 |
| Education | ||||
| Less than High School (%) | 5.85 | 5.15 | 13.14 | 0.002 |
| High School Graduate (%) | 31.71 | 31.78 | 30.93 | |
| Some College (%) | 30.31 | 30.16 | 31.89 | |
| College Graduate (%) | 32.13 | 32.91 | 24.04 | |
| Income | ||||
| < $10,000 (%) | 3.09 | 2.63 | 7.85 | <0.001 |
| $10,000–$15,000 (%) | 4.54 | 4.14 | 8.65 | |
| $15,000–$20,000 (%) | 5.94 | 5.38 | 11.7 | |
| $20,000–$25,000 (%) | 9.25 | 8.55 | 16.51 | |
| $25,000–$35,000 (%) | 15.49 | 15.38 | 16.67 | |
| $35,000–$50,000 (%) | 17.86 | 18.24 | 13.94 | |
| $50,000–$75,000 (%) | 19.77 | 20.44 | 12.82 | |
| $75,000 + (%) | 24.07 | 25.24 | 11.86 | |
| Employment | ||||
| Employed (%) | 54.41 | 55.08 | 47.44 | <0.001 |
| Self-Employed (%) | 7.6 | 7.73 | 6.25 | |
| Unemployed <1 Year (%) | 2.02 | 1.86 | 3.69 | |
| Unemployed >1 Year (%) | 2.06 | 1.70 | 5.77 | |
| Homemaker (%) | 6.82 | 7.08 | 4.17 | |
| Student (%) | 1.89 | 1.76 | 3.21 | |
| Retired (%) | 20.46 | 20.82 | 16.67 | |
| Unable to Work (%) | 4.75 | 3.97 | 12.82 | |
| Marital Status | ||||
| Married | 64.83% | 67.16% | 43.36% | <0.001 |
| Divorced | 8.97% | 8.55% | 12.84% | |
| Widowed | 5.23% | 5.27% | 4.89% | |
| Separated | 1.06% | 0.88% | 2.66% | |
| Never Married | 16.96% | 15.28% | 32.41% | |
| Unmarried | 2.94% | 2.85% | 3.85% | |
| Depressed Mood | ||||
| Mean (Standard Deviation) | 1.25 (2.92) | 1.20 (2.86) | 1.71 (3.46) | 0.10 |
We compared the N=62 respondents with missing data for the Sleep Disturbance or Daytime Fatigue items to those included in the study. Those missing sleep-related items were generally older (mean age 66 vs. 46); no other group differences were noted. This represents exclusion of <1% or participants. Although a geographic comparison is outside of the scope of the present study, we examined differential response rates in Michigan and Wisconsin and found that these states represented statistically different cohorts. Overall, the Michigan group was more likely to be Black/African-American (13% vs. 4%), more likely to report racism (6% vs. 4%), more likely to report sleep disturbance (19% vs. 16%), less likely to be employed (55% vs. 64%), and more likely to earn an income in the highest (30% vs. 25%) and lowest (4% vs. 1%) category (less likely to be in the middle of the distribution). However, no significant state*racism or state*race*racism interactions were significant.
To determine whether Non-Hispanic White and Black/African-American groups should be analyzed separately, a Race*Racism interaction explored whether the relationship between Racism and either Sleep Disturbance or Daytime Fatigue differed by race. This interaction was not statistically significant (Reference=Non-Hispanic White/Same or Better; Black/African-American/Worse OR = 0.81 (0.33–2.03), p>0.1 for Sleep Disturbance and OR = 0.78 (0.33–1.85), p>0.1 for Daytime Fatigue, see Tables 2 and 3). Thus, Black/African-American and Non-Hispanic White groups were analyzed together for the primary analyses. However, post hoc analyses explored whether the effects were maintained when groups were stratified into Non-Hispanic White (n=6,462) and Black/African-American (622) groups.
Table 2.
Odds Ratios (and 95% Confidence Intervals) for Sleep Disturbance Using Logistic Regression Across Models*
| Independent Variables | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | OR (95%CI) | P | ||
| Race (ref=White) | Black/African- American | 0.93 (0.68–1.29) | 0.667 | 0.62 (0.43–0.89) | 0.009 | 0.70 (0.48–1.02) | 0.061 |
| Racism (ref=Same) | Worse | 2.62 (1.80–3.81) | <0.001 | 1.97 (1.34–2.89) | <0.001 | 1.60 (1.03–2.49) | 0.036 |
| Sex (ref=Male) | Female | 1.56 (1.32–1.83) | <0.001 | 1.47 (1.23–1.74) | <0.001 | 1.44 (1.19–1.73) | <0.001 |
| Age | (Continuous) | 0.99 (0.98–1.00) | 0.025 | 0.99 (0.99–1.00) | 0.174 | ||
| Education (ref=College Graduate) | Less Than High School | 1.86 (1.32–2.62) | <0.001 | 1.47 (1.00–2.17) | 0.048 | ||
| High School Graduate | 1.68 (1.34–2.10) | <0.001 | 1.62 (1.27–2.07) | 0.001 | |||
| Some College | 1.38 (1.10–1.73) | 0.005 | 1.33 (1.05–1.70) | 0.018 | |||
| Income (ref=≥$75,000) | <$10,000 | 1.96 (1.20–3.21) | 0.007 | 1.35 (0.74–2.46) | 0.330 | ||
| $10–$15,000 | 2.08 (1.34–3.24) | 0.001 | 1.49 (0.91–2.45) | 0.113 | |||
| $15–$20,000 | 1.64 (1.11–2.43) | 0.013 | 1.23 (0.80–1.89) | 0.348 | |||
| $20–$25,000 | 1.79 (1.28–2.49) | <0.001 | 1.33 (0.91–1.94) | 0.142 | |||
| $25–$35,000 | 1.22 (0.90–1.67) | 0.205 | 1.02 (0.74–1.39) | 0.922 | |||
| $35–$50,000 | 1.28 (0.97–1.67) | 0.080 | 1.13 (0.85–1.50) | 0.400 | |||
| $50–$75,000 | 1.02 (0.78–1.34) | 0.866 | 1.00 (0.75–1.33) | 0.991 | |||
| Employment (ref= Employed) | Self Employed | 1.08 (0.78–1.50) | 0.649 | 0.98 (0.71–1.36) | 0.905 | ||
| Out of Work >1yr | 1.74 (1.01–2.97) | 0.044 | 1.22 (0.63–2.35) | 0.558 | |||
| Out of Work <1yr | 2.25 (1.31–3.85) | 0.003 | 1.85 (0.99–3.46) | 0.052 | |||
| Home Maker | 1.23 (0.92–1.65) | 0.170 | 1.24 (0.90–1.72) | 0.193 | |||
| Student | 0.86 (0.50–1.47) | 0.575 | 0.97 (0.56–1.69) | 0.919 | |||
| Retired | 1.26 (0.96–1.66) | 0.094 | 1.32 (0.99–1.77) | 0.060 | |||
| Unable to Work | 3.79 (2.69–5.32) | <0.001 | 2.25 (1.50–3.38) | 0.001 | |||
| Marital Status (ref=married) | Divorced | 1.13 (0.89–1.44) | 0.309 | 1.01 (0.77–1.31) | 0.954 | ||
| Widowed | 0.98 (0.72–1.34) | 0.900 | 0.97 (0.69–1.37) | 0.875 | |||
| Separated | 2.33 (1.23–4.43) | 0.009 | 1.58 (0.84–3.00) | 0.158 | |||
| Never Married | 1.24 (0.93–1.67) | 0.146 | 1.28 (0.94–1.75) | 0.115 | |||
| Unmarried | 1.13 (0.68–1.90) | 0.633 | 1.01 (0.57–1.78) | 0.981 | |||
| State (ref=Michigan) | Wisconsin | 0.87 (0.74–1.02) | 0.081 | 0.96 (0.81–1.15) | 0.682 | ||
| Depression | Depression | 1.32 (1.27–1.37) | <0.001 | ||||
| Interaction Effects | P Value | P Value | P Value | ||||
| Race/EthnicityX Racism | 0.671 | 0.728 | 0.790 | ||||
| Sex X Racism | 0.023 | 0.031 | 0.102 | ||||
| State X Racism | 0.509 | 0.735 | |||||
| Employment X Racism | 0.126 | 0.406 | |||||
| State X Race/EthnicityX Racism | 0.465 | 0.566 | |||||
| Employment X Race/EthnicityX Racism | 0.704 | 0.499 | |||||
Model 1 includes Racism, Race and Sex; Model 2 includes Model 1 variables + Age, Education, Income and Employment; Model 3 includes Model 2 variables + Depressed Mood (Days in the past 30 felt down or depressed). Employment Interactions exclude Unemployed < 1yr and Student due to inadequate cell sizes
Table 3.
Odds Ratios (and 95% Confidence Intervals) for Daytime Fatigue Using Logistic Regression Across Models*
| Independent Variables | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | OR (95%CI) | P | ||
| Race (ref=White) | Black/African-American | 0.93 (0.67–1.27) | 0.632 | 0.66 (0.46–0.94) | 0.021 | 0.74 (0.50–1.09) | 0.130 |
| Racism (ref=Same) | Worse | 2.07 (1.46–2.95) | <0.001 | 1.59 (1.12–2.26) | 0.009 | 1.19 (0.81–1.73) | 0.376 |
| Sex(ref=Male) | Female | 1.60 (1.37–1.86) | <0.001 | 1.48 (1.25–1.75) | <0.001 | 1.45 (1.21–1.73) | 0.001 |
| Age | (Continuous) | 0.99 (0.98–0.99) | <0.001 | 0.99 (0.98–1.00) | 0.008 | ||
| Education (ref=College Graduate) | Less Than High School | 1.42 (1.01–2.00) | 0.045 | 0.99 (0.65–1.50) | 0.967 | ||
| High School Graduate | 1.39 (1.13–1.73) | 0.002 | 1.30 (1.03–1.63) | 0.026 | |||
| Some College | 1.33 (1.08–1.64) | 0.007 | 1.27 (1.02–1.59) | 0.033 | |||
| Income (ref=≥$75,000) | <$10,000 | 1.67 (1.01–2.75) | 0.045 | 0.90 (0.47–1.69) | 0.735 | ||
| $10–$15,000 | 3.33 (2.15–5.15) | <0.001 | 2.62 (1.50–4.57) | 0.001 | |||
| $15–$20,000 | 2.87 (1.97–4.17) | <0.001 | 2.38 (1.61–3.54) | <0.001 | |||
| $20–$25,000 | 2.39 (1.73–3.31) | <0.001 | 1.82 (1.27–2.60) | 0.001 | |||
| $25–$35,000 | 1.67 (1.23–2.27) | 0.001 | 1.45 (1.05–2.00) | 0.022 | |||
| $35–$50,000 | 1.61 (1.25–2.09) | <0.001 | 1.45 (1.11–1.90) | 0.006 | |||
| $50–$75,000 | 1.26 (0.98–1.63) | 0.066 | 1.28 (0.99–1.66) | 0.064 | |||
| Employment (ref= Employed) | Self Employed | 0.91 (0.66–1.25) | 0.548 | 0.77 (0.56–1.07) | 0.115 | ||
| Unemployed>1yr | 1.88(1.17–3.02) | 0.009 | 1.36 (0.69–2.68) | 0.368 | |||
| Unemployed<1yr | 1.10 (0.65–1.86) | 0.724 | 0.67 (0.37–1.22) | 0.188 | |||
| Home Maker | 1.17 (0.89–1.53) | 0.263 | 1.18 (0.88–1.58) | 0.272 | |||
| Student | 0.85 (0.51–1.41) | 0.519 | 0.99 (0.59–1.67) | 0.972 | |||
| Retired | 1.10 (0.85–1.41) | 0.467 | 1.16 (0.88–1.52) | 0.299 | |||
| Unable to Work | 3.83 (2.72–5.40) | <0.001 | 2.27 (1.52–3.40) | 0.001 | |||
| Marital Status (ref=Married) | Divorced | 1.20 (0.95–1.52) | 0.124 | 1.07 (0.83–1.38) | 0.606 | ||
| Widowed | 0.90 (0.67–1.20) | 0.476 | 0.86 (0.62–1.21) | 0.395 | |||
| Separated | 2.19 (1.25–3.82) | 0.006 | 1.47 (0.90–2.40) | 0.128 | |||
| Never Married | 0.86 (0.64–1.16) | 0.315 | 0.80 (0.59–1.10) | 0.173 | |||
| Unmarried | 0.98 (0.59–1.62) | 0.936 | 0.79 (0.47–1.33) | 0.370 | |||
| State (ref=Michigan) | Wisconsin | 0.82 (0.71–0.96) | 0.014 | 0.92 (0.78–1.09) | 0.329 | ||
| Depression | (Continuous) | 1.44 (1.37–1.51) | <.001 | ||||
| Interaction Effects | P Value | P Value | P Value | ||||
| Race X Racism | 0.580 | 0.743 | 0.827 | ||||
| Sex X Racism | 0.902 | 0.538 | 0.059 | ||||
| State X Racism | 0.284 | 0.400 | |||||
| Employment X Racism | 0.293 | 0.643 | |||||
| State X Race X Racism | 0.622 | 0.744 | |||||
| Employment X Race X Racism | 0.615 | 0.353 | |||||
Model 1 includes Racism, Race and Sex; Model 2 includes Model 1 variables + Age, Education, Income and Employment; Model 3 includes Model 2 variables + Depressed Mood (Days in the past 30 felt down or depressed). Employment Interactions exclude Unemployed < 1yr and Student due to inadequate cell sizes
In the stratified analysis, ORs were similar for both groups. For the effects of perceived racism on Sleep Disturbance, in the fully-adjusted model, the OR for the Non-Hispanic White group was 1.66 and the OR for the Black/African-American group was 1.52. For the effects of perceived racism on Sleep Disturbance, in the fully-adjusted model, the OR for the Non-Hispanic White group was 1.18 for the Non-Hispanic White group and 1.40 for the Black/African-American group. However, only the values in the Non-Hispanic White group demonstrate statistical significance (p<.05).
Impact of Perceived Racism on Sleep Disturbance
Odds Ratios and 95% Confidence Intervals for Sleep Disturbance are reported in Table 2 for perceived racism, as well as for all covariates across all 3 Models. In Model 1, adjusting only for sex and race, the OR for Sleep Disturbance associated with perceived racism was 2.61 (95% CI 1.79–3.80; p<.0001), indicating that those who reported that they were treated worse were over two and a half times as likely to have sleep disturbance than those who were treated the same or better. After socio-demographic and socioeconomic variables (age, education, income and employment) were entered into Model 2, the relationship between perceived racism and sleep disturbance was attenuated but remained statistically significant at OR = 1.97 (95% CI 1.35–2.89; p<0.001). In Model 3, which includes depressed mood, this relationship was further attenuated but remained significant at OR = 1.61 (95% CI 1.03–2.51; p<.05). The OR for Sleep Disturbance across models is also seen in Figure 1. When Non-Hispanic White and Black/African-American groups were examined separately, a significant (p<.05) OR was found for Racism in the Non-Hispanic White group for Model 1 (OR=2.79), Model 2 (OR=2.08), and Model 3 (OR=1.66). For the Black/African-American group, a significant OR was found in Model 1 (OR=2.32), but not in Model 2 (OR=1.88) or Model 3 (OR=1.52).
Figure 1. Perceived Racial Discrimination as an Independent Predictor of Sleep Disturbance and Daytime Fatigue across 3 Models.
Odds Ratios for Sleep Disturbance and Daytime Fatigue for those who experience perceived racism, across Model 1 (Demographics), Model 2 (Demographics and Socioeconomics) and Model 3 (Demographics, Socioeconomics and Depressed Mood) (* = p<0.05).
Impact of Perceived Racism on Daytime Fatigue
Odds Ratios and 95% Confidence Intervals for Daytime Fatigue are reported in Table 3 for perceived racism, as well as for all covariates across all 3 Models. In Model 1, adjusting only for sex and race, the OR for Daytime Fatigue associated with perceived racism was 2.07 (95% CI 1.45–2.94; p<.0001), indicating that those who reported that they were treated worse because of their race were over twice as likely to report daytime fatigue than those who were treated the same or better. Adjusting for socio-demographic and socioeconomic variables in Model 2 (age, education, income and employment), attenuated this relationship but the OR remained significant (OR = 1.57; 95% CI 1.11–2.23; p<.05). In Model 3, which includes depressed mood, this relationship was further attenuated and was no longer significant (OR = 1.18; 95% CI 0.81–1.72; p>.05). The OR for Daytime Fatigue across models is also observed in Figure 1. When Non-Hispanic White and Black/African-American groups were examined separately, a significant (p<.05) OR for Racism was found for the Non-Hispanic White group in Model 1 (OR=2.25) and Model 2 (OR=1.65) but not Model 3 (OR=1.18). ORs for the Black/African-American group were not significant in Model 1 (OR=1.78), Model 2 (OR=1.62) or Model 3 (OR=1.40).
Interactions with Sex and Employment Status
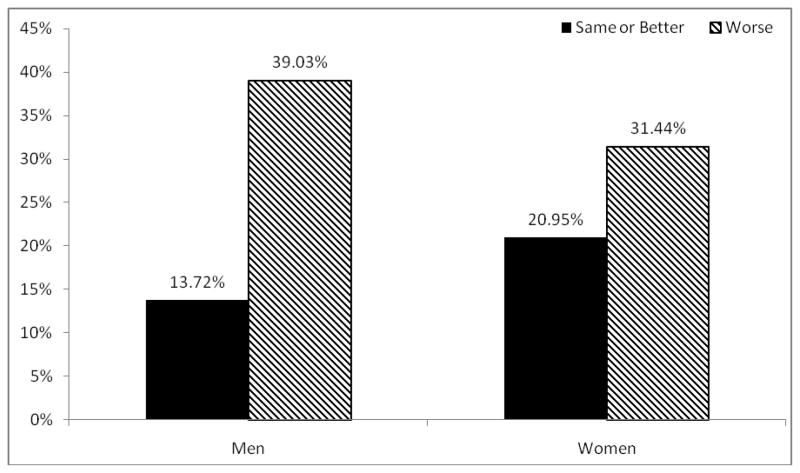
We found a significant main effect for sex, such that, overall, women reported more Sleep Disturbance and Daytime Fatigue than men (Tables 2 and 3). However, a significant sex*racism interaction was present for Sleep Disturbance in both Models 1 and 2, demonstrating that the effect of racism on sleep disturbance differed by sex (depicted in Figure 2). Specifically, the association between perceived racism and Sleep Disturbance was stronger for men than it was for women. In model 3, which included depressed mood, this interaction was no longer significant.
Figure 2. Sex Differences in Sleep Disturbance Associated with Perceived Racism.
Weighted prevalence of Sleep Disturbance relative to perceived racism, for men and women. A significant Racism*Sex interaction was found in Model 1 (Demographics) and Model 2 (Demographics and Socioeconomics), but not Model 3 (Demographics, Socioeconomics and Depression).
Regarding employment, the Black/African-American group was more likely to be unable to work, which may influence the results of the study. We examined the possibility of a Race/Ethnicity*Employment*Racism interaction. Employment groups were collapsed to employed, unemployed, unable to work and “other” (retired, homemaker or student) due to cell sizes necessary for interaction. This was not significant for Sleep Disturbance or Daytime Fatigue, suggesting that the effects of racism and race on these sleep outcomes is not differential based upon unemployment or inability to work.
Discussion
The present study was one of the first to examine a specific form of perceived institutional racial discrimination (i.e., in healthcare settings) in relation to sleep disturbance and daytime fatigue. Results showed that perceived racism in the healthcare setting was associated with increased risk of having sleep disturbance, and this relationship remained significant (though attenuated), even after adjusting for several risk factors known to covary with perceptions of racism and disturbed sleep. Perceived racism was also associated with increased risk of having significant daytime fatigue; however, this effect was largely accounted for by depressed mood. These results suggest that the fatigue associated with depressed mood accounted for the fatigue associated with perceived racial discrimination. However, the sleep disturbance associated with depressed mood only partially explained the sleep disturbance that was associated with the perceived racial discrimination, suggesting that racism contributes unique variance to sleep disturbance.
When we performed a stratified analysis by race/ethnicity group, we did see that ORs were roughly the same for both groups. However, only the values for the Non-Hispanic White group were significant, which may have been due to power issues; the Non-Hispanic White group was considerably larger than the Black/African-American group.
These findings support previous studies that have found that perceived racial discrimination has a negative impact on sleep (Steffen & Bowden, 2006; Thomas, et al., 2006) and that sleep disturbance is important factor in the relationship between perceived racism and depressed mood (Steffen & Bowden, 2006). Perceived racism is a newer factor identified in the social environment that has significant bearing on Sleep Disturbance. Past studies that have identified the proximal nature of the effect of depression upon insomnia (Hale et al., 2009) may have captured a contribution of perceived racism. This study adds to this literature by evaluating perceived racism relative to sleep-related problems and showing that perceived racism has an impact on sleep at night over and above age, sex, race, and a number of socioeconomic factors, and (in the case of Sleep Disturbance) depressed mood. It should be noted that, unlike previous studies, sleep disturbance was only measured in the present study using a single survey item.
In addition to supporting the findings of previous studies, this analysis makes a number of unique contributions. First, the sample in this study is much larger than any that has previously addressed this question; also, generalizability is maximized with the use of weighted cases. Second, this analysis shows that perceived racial discrimination is related to sleep disturbance in a specific context (healthcare settings). This allows for the generation of specific questions for future studies, including: (1) To what extent is this reflective of psychosocial stress? (2) How does this relate to the disparity in treatment for sleep disorders (Jean-Louis et al., 2008) or other medical conditions (Farmer & Ferraro, 2005; Laveist, Thorpe, Galarraga, Bower, & Gary-Webb, 2009)? and (3) Is this a reflection of negative health consequences of institutionalized racism, which might render certain individuals more vulnerable to other health conditions that may lead to sleep disturbance?
In addition to replicating and extending previous findings regarding perceived racism, this study also is consistent with previous studies investigating socioeconomic factors, including education, financial strain and unemployment. Specifically, data from the Survey of Texas Adults shows associations between worse self-repeated sleep quality and low education, financial strain, and unemployment (Hill, et al., 2009). Prior work on sleep duration shows that being unemployed and low levels of education are associated with increased odds of high-risk sleep duration (Hale, 2005; Hale & Do, 2007; Krueger & Friedman, 2009). Since the present study evaluated only Non-Hispanic White and Black/African-American respondents, it is unclear as to whether the observed relationships also pertain to other groups (e.g., Hispanic/Latino, Asian). Since these results are consistent with the one previous study in Hispanics, it is likely that this group, as well, may demonstrate the same relationship. Since no previous study has investigated Asian-Americans, it is unknown whether these results apply to this group as well, or others that have also not been studied.
When the Non-Hispanic White and Black/African-American groups were assessed separately, some of the relationships were maintained, and many (especially in the Black/African-American group) were not. It should be noted that the magnitude of the ORs was similar (reflecting the lack of interaction). The likely explanation for the increase in p values is a reduction in statistical power due to reductions in sample size. It is possible that in a larger group of Black/African-American respondents, an interaction may be discerned, which would justify interpreting the stratified results. On the other hand, the non-significant race*racism interaction, suggests that although Black/African-Americans are three times more likely to perceive racism, the effect of racism on sleep is similar among Black/African Americans and Non-Hispanic whites.
Limitations
There were a number of limitations to this study. First, the sleep problems and daytime fatigue reported in BRFSS are self-reported, general measures from single items, with unknown reliability. They do not suggest any particular sleep-related pathology, such as sleep apnea or insomnia, and may not be predictive of objective sleep problems. Future studies should employ validated self-report assessments of sleep in the context of racism. In addition, the BRFSS does not include a measure of sleep duration. Second, the sample of this study was primarily comprised of Non-Hispanic White individuals, and data were gathered only in the states of Michigan and Wisconsin, where these measures were administered. Given that the sample was primarily Non-Hispanic White, it is unclear whether these results are generalizable to environments that have a larger Black/African-American presence or other minority populations.
Conclusions
Acknowledgement of the influence of the social environment upon sleep (Grandner & Patel, 2009; Grandner, Patel, Hale, et al., 2010)growsrapidly. As others have indicated, a broad socio-ecological approach is critical to investigating the social determinants of sleep attainment. Looking beyond commonly quoted factors such as socioeconomic status and assessing for the effects of other socio-ecological factors is pertinent. The present study suggests that perceived racial discrimination, an important social factor, is a significant predictor of sleep disturbance and daytime fatigue, after adjusting for demographic and socioeconomic variables, and the relationship to sleep disturbance remains after adjusting for depressed mood. The magnitude of this relationship suggests that individuals who experience perceived discrimination are ~60% more likely to experience sleep difficulties, even after adjusting for social, demographic, and mental health covariates. Future research should further explore the impact of perceived racism in other regions, using both subjective and objective measures of sleep disturbance, and also examine the underlying factors that specifically link perceived racism to increased sleep disturbances.
Acknowledgments
This work was supported by T32HL007713 and a pilot grant from the University of Pennsylvania CTSA (UL1RR024134), as well as K23HL093220 (WMT).
Contributor Information
Michael A. Grandner, Center for Sleep and Circadian Neurobiology, Division of Sleep Medicine, Department of Medicine, University of Pennsylvania.
Lauren Hale, Division of Evaluative Sciences, Department of Preventive Medicine, Stony Brook University.
Nicholas Jackson, Center for Sleep and Circadian Neurobiology, Division of Sleep Medicine, Department of Medicine, University of Pennsylvania.
Nirav P. Patel, Respiratory Specialists and Reading Hospital and Medical Center.
Nalaka S. Gooneratne, Center for Sleep and Circadian Neurobiology and Division of Geriatric Medicine, University of Pennsylvania.
Wendy M. Troxel, Department of Psychiatry and Psychology, University of Pittsburgh.
References
- Aanes MM, Hetland J, Pallesen S, Mittelmark MB. Does loneliness mediate the stress-sleep quality relation? The Hordaland HealthStudy. Int Psychogeriatr. 2011:1–9. doi: 10.1017/S1041610211000111. [DOI] [PubMed]
- Anic GM, Titus-Ernstoff L, Newcomb PA, Trentham-Dietz A, Egan KM. Sleep duration and obesity in a population-based study. Sleep Med. 2010;11(5):447–451. doi: 10.1016/j.sleep.2009.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. Behavioral Risk Factor Surveillance System. Atlanta, Georgia: Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Google Scholar]
- Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Freid VM, Prager K, MacKay AP, Xia H. Chartbook on Trends in the Health of Americans. Health, United States, 2003. Hyattsville, MD: National Center for Health Statistics; 2003. [Google Scholar]
- Gallicchio L, Kalesan B. Sleep Duration and Mortality: A Systematic Review and Meta-analysis. J Sleep Res. 2009;18(2):148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- Geiger-Brown J, Trinkoff A, Rogers VE. The impact of work schedules, home, and work demands on self-reported sleep in registered nurses. J Occup Environ Med. 2011;53(3):303–307. doi: 10.1097/JOM.0b013e31820c3f87. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Patel NP. From sleep duration to mortality: implications of meta-analysis and future directions. J Sleep Res. 2009;18(2):145–147. doi: 10.1111/j.1365-2869.2009.00753.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: Bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14:239–247. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who sleeps better? Socioeconomic differences in reports of sleep disturbance. Sleep. 2009;32:A422–423. Abstract Supplement. [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep disturbance. Sleep Med. 2010;11:470–479. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Hale L, Moore M. Mortality associated with sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14:191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hairston KG, Bryer-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: the IRAS family study. Sleep. 2010;33(3):289–295. doi: 10.1093/sleep/33.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27(2):205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Do DP, Basurto-Davila R, Heron M, Finch BK, Dubowitz T, et al. Does mental health history explain gender disparities in insomnia symptoms among young adults? Sleep Med. 2009;10(10):1118–1123. doi: 10.1016/j.sleep.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15(4):1006–1013. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Jansson-Frojmark M, Linton SJ. The course of insomnia over one year: a longitudinal study in the general population in Sweden. Sleep. 2008;31(6):881–886. doi: 10.1093/sleep/31.6.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Louis G, von Gizycki H, Zizi F, Dharawat A, Lazar JM, Brown CD. Evaluation of sleep apnea in a sample of black patients. J Clin Sleep Med. 2008;4(5):421–425. [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Med. 2011;12(1):28–33. doi: 10.1016/j.sleep.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laveist TA, Thorpe RJ, Jr, Galarraga JE, Bower KM, Gary-Webb TL. Environmental and Socio-Economic Factors as Contributors to Racial Disparities in Diabetes Prevalence. J Gen Intern Med. 2009 doi: 10.1007/s11606-009-1085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine RS, Foster JE, Fullilove RE, Fullilove MT, Briggs NC, Hull PC, et al. Black-white inequalities in mortality and life expectancy, 1933–1999: implications for healthy people 2010. Public Health Rep. 2001;116(5):474–483. doi: 10.1093/phr/116.5.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyytikainen P, Lallukka T, Lahelma E, Rahkonen O. Sleep problems and major weight gain: a follow-up study. Int J Obes (Lond) 2010 doi: 10.1038/ijo.2010.113. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87(3):873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- Nielsen LS, Danielsen KV, Sorensen TI. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev. 2010 doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- Patel NP, Grandner MA, Gehrman P, Xie D, Sha D, Weaver TE, et al. Effects of sociodemographic and socioeconomic factors on sleep complaints depend on an individual’s race/ethnicity. Sleep. 2010;33:A307. Abstract Supplement. [Google Scholar]
- Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. "Sleep disparity" in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10(1):475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piffath TA, Whiteman MK, Flaws JA, Fix AD, Busht TL. Ethnic differences in cancer mortality trends in the US, 1950–1992. Ethn Health. 2001;6(2):105–119. doi: 10.1080/13557850120068432. [DOI] [PubMed] [Google Scholar]
- Runeson R, Lindgren T, Wahlstedt K. Sleep problems and psychosocial work environment among Swedish commercial pilots. Am J Ind Med. 2011 doi: 10.1002/ajim.20943. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, RNA . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006;16(1):16–21. [PubMed] [Google Scholar]
- Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychol. 2006;25(5):635–642. doi: 10.1037/0278-6133.25.5.635. [DOI] [PubMed] [Google Scholar]
- van Cauter E, Leproult R. Sleep and diabesity in older adults. In: Pandi-Perumal SR, Monti JR, Monjan AA, editors. Principles and Practice of Geriatric Sleep Medicine. Cambridge: Cambridge; 2010. pp. 107–120. [Google Scholar]
- Watanabe M, Kikuchi H, Tanaka K, Takahashi M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. SLEEP. 2010;33(2):161–167. doi: 10.1093/sleep/33.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev. 2000;57(Suppl 1):36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findingsfrom community studies. Am J Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]