Abstract
Background
Worldwide, the literature on sexual behaviour has documented associations between gender-based relationship inequality and sexual communication ability and the actual use of condoms or other contraceptives among young women. This study aimed to examine these associations among undergraduate female students in the Mekong Delta of Vietnam.
Methods
A cross-sectional survey of 1181 female third-year students from two universities in the Mekong Delta was conducted. Latent variable modelling and logistic regression were employed to examine the hypothesised associations.
Results
Among the 72.4% of students who had ever had boyfriends, 44.8% indicated that their boyfriends had asked for sex, 13% had had penile–vaginal sex and 10.3% had had oral sex. For those who had had penile–vaginal sex, 33% did not use any contraceptive method, including condoms, during their first sexual intercourse. The greater a student’s perception that women were subordinate to men, the lower her self-efficacy for sexual communication and the lower her actual frequency of discussing safer sex matters and asking her partner to use a condom. Sexual communication self-efficacy was associated with actual contraceptive use (P = 0.039) but only marginally with condom use (P = 0.092) at first sexual intercourse.
Conclusion
Sexual health promotion strategies should address the influence of gender relations on young women’s sexual communication self-efficacy and the subsequent impact on actual contraceptive and condom use.
Additional keywords: condom use, contraceptive use, gender relations, women, youth
Introduction
Currently, about one-third of Vietnam’s population are young people between the ages of 15 and 25 years.1 In this rapidly changing society, young people’s perspectives on gender relations and premarital sex have taken a more liberal turn, much more dramatically in cities than in rural areas.1,2 According to the 2005 Survey Assessment of Vietnamese Youth (SAVY) – the largest and most comprehensive youth health survey in Vietnam – about one-fifth of young, unmarried women considered premarital sex acceptable.2 The overall rate of premarital sex among young women was 4%. Some unpublished surveys have reported that as many as 40% of female college students have premarital sex.1 Once they have had sex, most young people continue having it.2 Although contraception knowledge has increased, with a vast majority of surveyed individuals (97%) knowing at least one contraceptive method, only around two-thirds of unmarried sexually active young people used contraceptives, including condoms, at their first or last sex.2 Contraceptive use by female undergraduate students at first sexual intercourse may be as low as 30%.1,3 Having unprotected sex may place young women at increased risks for many health problems, including early or unintended pregnancy, abortion, and sexually transmissible infections (STIs), including HIV.
One risk factor for not using contraceptives or condoms, highlighted in studies and reports from developing countries, is the woman’s lack of confidence and power to negotiate their use.4–7 This lack is believed to be rooted in unequal or inequitable gender relations. In Vietnam, there are few studies that have tested this hypothesis explicitly and quantitatively, and those that have done so focus primarily on married women and women living in northern or central Vietnam.8,9 Scientific studies on gender inequality and sexual relations in southern Vietnam and in other institutions, such as universities, are limited.10 Although female undergraduate students are more educated than their counterparts in the general population, this education does not confer equal power in relationships11 nor enhanced contraceptive or condom use. One review of HIV/AIDS risk among heterosexual undergraduate students in the United States (US) showed that students rarely communicate about condom use with their partners.12 In addition, levels of safer sex self-efficacy varied and were inversely correlated with HIV transmission risk. Similarly, in several US studies, non-communication was associated with not using contraceptives or condoms.13–15
Preliminary analysis of the association between perceived unequal gender relations and female undergraduate students’ inability to discuss sexual matters with their boyfriends revealed that female students from the Mekong Delta who agreed with the traditional gender roles and norms had lower self-efficacy to refuse unwanted sex or to request condom use.16 One limitation of this analysis was that measures of students’ perceptions of gender relations may have been inadequate or may not have reflected the most salient dimensions related to gender equity. Moreover, the analysis was limited to the relationship between two scales: adherence to traditional gender stereotypes and sexual self-efficacy, and was therefore not able to examine actual sexual communication and practices. Using a larger, more rigorous survey, we aimed to quantitatively re-examine the relationships among perceived gender relations, sexual communication self-efficacy, actual sexual communication, and actual contraceptive or condom use among female undergraduate students in the Mekong Delta. We hypothesised that female students who perceived women as having a lower status than men would have lower sexual communication self-efficacy with their boyfriends and, in turn, would be less likely to use contraception or a condom at first sexual intercourse.
Methods
Sample
We conducted a cross-sectional study among third-year female students at Can Tho University and An Giang University, two large universities in the Mekong Delta. Third-year students were targeted because they were not as busy with schoolwork as seniors, and the likelihood of having had a boyfriend or having had premarital sex was higher than among freshmen and sophomores, making statistical tests of our main hypothesis more feasible. In each school, classes served as the primary sampling units. The universities provided lists of all third-year classes by majors. Each class consisted of 30–50 students, including men and women. We randomly selected about one-quarter of the classes in Can Tho University and one-third of the classes in An Giang University in order to meet our desired sample size. We invited all female students in the selected classes to participate. Participation rates were 94% at Can Tho University and 99% at An Giang University.
Procedure
At Can Tho University, we invited the female students in one to three selected classes to meet in a large lecture hall at predetermined times. At An Giang University, we attended the selected classes at the end of the regular class period, asked the male students to leave, and asked all female students to participate in the survey. We first described the purpose of the study, confidentiality, and the benefits and risks of participation. Informed consent was obtained from each student. Students answered an anonymous, self-administered questionnaire, which took ~30 min to complete. No information that could identify participants was collected. Only the researchers and research assistants were present to answer questions while students took the survey. Upon completing the survey, each student placed her survey into a white envelope and then into a large box located in the corner of the room. The study was approved by both universities’ boards of rectors and by the Institutional Review Board from the University of Texas – Health Science Center at Houston (HSC-SPH-08–0548). Data were collected from March to April 2009.
Measures
Perceived subordination
To develop the measure for this construct, we grounded our work in the Theory of Gender and Power,17 which comprises three critical structures of gender relations: sexual division of labour, sexual division of power, and cathexis. Division of labour includes social rules to allocate particular types of work to a particular gender, such as unpaid housework and childcare for women. It also involves gender differentiation in training, employment, types of jobs and promotion. Division of power comprises authority, hierarchies, coercion and control over resources at different levels: national, organisational, familial and interpersonal. This structure additionally takes cultural power into account such as patriarchal order or the cultural classification of women as ‘weak’. Cathexis depicts social sexual relationships between people manifested in social sexualisation, prohibitions and incitements, beliefs, standards and expectations. To obtain the salient dimensions of these structures in the target population, we conducted qualitative research with eight groups of female undergraduates.11 From numerous dimensions of gender relations in these qualitative results, we selected those which generated different levels of agreement and different levels of acceptance (e.g. the view of housework as women’s duty) to serve as possible measurement items.
Exploratory and confirmatory factor analyses using Analysis of Moment Structures (AMOS) ver. 16.0.1 were conducted to assess each item’s validity in measuring the theoretical structures and the subsequent general construct of ‘perceived subordination’.11 Items were operationalised by asking students, ‘How much do you agree with these statements?’ The seven-point Likert-type response format ranged from ‘completely disagree’ to ‘completely agree’. A second-order confirmatory factor analysis model showed a very good fit, in which 21 items in Table 1 loaded onto three corresponding first-order latent variables (inequity in labour, unequal power and cathexis) and these three first-order factors loaded onto a single second-order factor named ‘perceived subordination’. However, to identify a parsimonious subset of critical items, we ran a further single-factor model, in which all 21 items were loaded onto one latent construct of ‘perceived subordination’. We removed items that had low standardised coefficients (<0.30), those that were only potentially applicable to a subgroup or to a specific context (e.g. dating only), and those for which content was covered by another item. As a result, 10 items were retained as a single measure of ‘perceived subordination’ (Tables 1 and 2).
Table 1.
Original items measuring perceived gender relations in the questionnaire administered to female university students
The stem question for these items was ‘How much do you agree with these statements?’ Responses were on a seven-point scale: 1 = completely disagree, 2 = disagree, 3 = slightly disagree, 4 = indifferent, 5 = slightly agree, 6 = agree and 7 = completely agree
| Description |
|---|
| Inequity in labour (sexual division of labour) |
| Housework is the duty of women.† |
| A mother has more responsibility in childcare and bringing children up than a father does. |
| After marriage, a woman should not do too much paid work but she should attach special importance to running her household life. |
| Some majors, such as land management, physical education, and rural development, are ‘men’s fields’. |
| For matters related to social relations, men do them better than women. |
| It is acceptable for a woman to earn little money and to be provided for by her husband. |
| Unequal power (sexual division of power) |
| It is better to let the man be the head (trụ cột) of the family.† |
| It is more appropriate for men than for women to participate in leadership positions in governmental or policy-making structures.† |
| Valuable property in the household (e.g. house, land, motorbike) should be in the man’s name.† |
| The female is the ‘weaker gender’.† |
| Men should have the final say for important things in a family.† |
| A wife should not have a higher education than her husband. |
| Cathexis |
| After marriage, a wife must reside in her husband’s house. |
| It is almost impossible for a non-virgin woman to get married (including a first-time marriage or remarriage).† |
| If a female takes the initiative to leave her boyfriend, she will be vilified (e.g. ‘to leave an old thing for a new one’). |
| Men should have extensive relationships, including with people of the opposite sex, but women should not.† |
| A woman should always ‘sacrifice’ her own education and career so that her husband can advance in his. |
| A wife should always make concessions to her husband in order to maintain a harmonious relationship in the family.† |
| A woman must be meek and obedient.† |
| It is hard to resist such family or social thoughts as son preference and valuing men above women. |
| A female can take the initiative in declaring her love to a male. |
Indicates the 10 items retained in the final measure for analysis.
Table 2.
Mean and standard deviations for items
The stem question for perceived subordination items was ‘How much do you agree with these statements?’ Responses were: 1 = completely disagree, 2 = disagree, 3 = slightly disagree, 4 = indifferent, 5 = slightly agree, 6 = agree and 7 = completely agree. The stem question for self-efficacy items was ‘How confident you are in doing the following things on a scale from 1 to 7?’ with 1 = not confident at all, 2 = not confident, 3 = slightly not confident, 4 = so-so, 5 = slightly confident, 6 = confident and 7 = absolutely confident
| Items | Mean | s.d. | |
|---|---|---|---|
| Perceived subordination | |||
| Q1 | The female is the ‘weaker gender’. | 3.41 | 0.051 |
| Q2 | Housework is the duty of women. | 3.00 | 0.051 |
| Q3 | A wife should always make concessions to her husband in order to maintain a harmonious relationship in the family. | 3.05 | 0.047 |
| Q4 | Valuable property in the household (e.g. house, land, motorbike) should be in the man’s name. | 2.29 | 0.042 |
| Q5 | A woman must be meek and obedient. | 4.07 | 0.053 |
| Q6 | Men should have extensive relationships, including with people of the opposite sex, but women should not. | 1.88 | 0.034 |
| Q7 | It is more appropriate for men than for women to participate in leadership positions in governmental or policy- making structures. | 2.92 | 0.048 |
| Q8 | Men should have the final say on important things in a family. | 3.30 | 0.053 |
| Q9 | It is almost impossible for a non-virgin woman to get married (including a first-time marriage or remarriage). | 3.33 | 0.056 |
| Q10 | It is better to let the man be the head (trụ cột) of the family. | 4.72 | 0.052 |
| Sexual communication self-efficacy | |||
| Q11 | I can easily initiate and conduct a conversation about safer sex with my boyfriend. | 4.55 | 1.90 |
| Q12 | If I don’t want to have sex before marriage, I can tell my boyfriend about my personal limit even if he has not asked for sex yet. | 6.03 | 1.13 |
| Q13 | If my boyfriend wants to have sex but I don’t want to, I can easily refuse without it breaking up our relationship. | 6.12 | 1.18 |
| Q14 | I can ask my boyfriend to use a condom if I want him to do so. | 5.96 | 1.38 |
| Q15 | I can start a conversation about using a contraceptive with my boyfriend before we have sex for the first time. | 5.67 | 1.59 |
This single-factor model had a highly superior fit and was stable across 500 hypothetical bootstrapping samples. The Cronbach’s coefficient α value measuring the internal consistency reliability of scores for this 10-item scale was 0.71. We tolerated reliability values around 0.70 because of the multidimensional nature of the latent construct ‘perceived subordination’.
Sexual communication self-efficacy
Perceived self-efficacy has been defined as the confidence one feels about executing a particular behaviour.18 Many health behaviour changes have occurred subsequent to perceived self-efficacy enhancement.19,20 Utilising the instrument bank established by the Center for HIV Identification, Prevention and Treatment Services (2006)21 of the University of California at Los Angeles, we generated a contextually and culturally adapted measure for sexual communication self-efficacy. This scale included items that measured one’s self-efficacy in refusing sex and in initiating communication about contraceptive or condom use (Table 2). Recognising that operationalising self-efficacy should be situation-specific,22 we eliminated items about unlikely or inapplicable situations. For example, self-efficacy to refuse sex with a new partner or when intoxicated were unlikely to be relevant because most target subjects were unlikely to have had more than two sexual partners,16 and because there was little evidence of the co-occurrence of drinking and having sex in this population. Furthermore, we were more interested in assessing communication and negotiation for multiple domains of sexual practices than in focusing on a single domain, such as condom use, in different situations. The Cronbach’s α coefficient of this scale was 0.68.
Actual sexual communication
Three separate outcome variables for the sexual communication assessed the frequency of discussing safer sex matters, the frequency of discussing contraceptive use and the frequency of asking for condom use. With regard to discussing safer sex matters, we asked currently dating participants, ‘How many times have you discussed safer sex matters with your boyfriend(s) in the past month?’ The term ‘safer sex’ (an toàn tình dục) is commonly used in sexual and reproductive health education programs in the south of Vietnam, and generally implies not having penetrative sex and being protected from getting pregnant and STIs. We used this term because it was familiar to participants. Analysis related to this outcome variable was limited to a subgroup of participants who currently had had their boyfriends for 6 months or longer (n = 465). We selected 6 months, which was the first quartile of time spent in a current relationship, because we assumed that the level of intimacy would be sufficient for partners to discuss sexual matters. The median number of times for talking with a boyfriend about safer sex matters was once and the maximum was 20. Since less than 3% of participants reported a frequency greater than five, we placed these cases into a single group of ‘five times or more,’ making this variable a categorical one with a range of 1–5. For the frequency variables discussing contraceptive use and condom use, we asked sexually experienced students (n = 111) two questions, ‘How often do
you talk to your boyfriend about using contraceptives?’ and ‘How often do you ask your boyfriend to use a condom?’ Response options ranged from 1 = never to 5 = every time we have sex.
Sexual behaviour at first sex
Participants who had had penile–vaginal sex were asked whether they used a contraceptive method the first time and, if so, what method they used and who suggested its use.
The survey instrument was developed in Vietnamese. It was reviewed by nine Vietnamese gender researchers and practitioners, and then was pretested with a group of 25 female students to assess face and content validity. The word ‘sex’ in the questionnaire and also in this report was defined as penile–vaginal sexual intercourse, unless otherwise specified. ‘Oral sex’ was defined as the use of the mouth of one partner to sexually stimulate the penis or vagina of the other.
Data screening, preparation and analysis
We primarily employed latent variable modelling (LVM) to examine the relationships among latent variables measured by multiple items using categorical scales. For binary sexual behavioural outcomes that were inappropriate for analysis via LVM, we used logistic regression to examine their relationships with independent variables. Specifically, the directional associations among perceived subordination, sexual communication self-efficacy, and actual sexual communication were investigated using LVM. The relationships among perceived subordination, sexual communication self-efficacy, and sexual behaviour at first sex were examined using logistic regression.
Latent variable modelling
A potential advantage of LVM is that it provides a convenient and straightforward way to handle observable and unobservable (i.e. latent) variables. The hypothesised directional relatedness among observable items (e.g. the level of agreement that housework was women’s work) and latent variables (e.g. perceived subordination) were directly estimated and visualised via the regression paths among them. Additionally, LVM provided the ability to assess measurement error and imperfect score reliability. The use of LVM based on maximum likelihood procedures using AMOS 16.0.1 requires there to be no missing values, a continuous scale for measures and a multivariate normal distribution. Of 21 observable items, 14 had one to nine missing values. These were imputed using series medians. Treating categorical variables with four or more categories as continuous variables is an accepted practice, particularly when a covariance rather than a correlation matrix is used in a maximum likelihood estimation.23 By utilising seven-point scales for our measures and a covariance matrix for analyses, issues related to the use of noncontinuous scales were minimal.
Based on recommendations from Kline (2005)24 and Hu & Bentler (1999),25 we considered that the presentation of a set of fit statistics, including the model χ2, Tucker–Lewis Index (TLI), comparative fit index (CFI), root mean square error of approximation (RMSEA) and standardised root mean square residual (SRMR) would be appropriate and sufficient to evaluate model fit in our analyses. When the model adequately fits the observed data, a nonsignificant P-value and the accompanying χ2 statistic are expected. Nevertheless, when the sample size is large, a trivial difference between observed and predicted covariances may result in a statistically significant value for a model χ2. In order to address this sensitivity of the χ2-test to sample size, researchers suggest using a value called the normed χ2, which results from dividing the χ2 value by the degrees of freedom.24 A reasonable model fit is indicated by a normed χ2 value of less than 3.0. Values of TLI and CFI greater than 0.90 indicate a reasonably good fit, and those greater than 0.95 indicate a superior fit.24 For RMSEA and SRMR, values <0.06 are evidence of well fitting models.25 When these statistics independently corroborate the goodness of fit, a model’s fit is more reliable.
Logistic regression analysis
We recorded sexual behaviour outcomes at first penile–vaginal sex into binary variables: (1) whether or not participants used a contraceptive method at first sex; (2) whether participants used condoms or other contraceptive methods such as emergency contraception or withdrawal; and (3) whether or not female participants initiated contraceptive or condom use. Regarding the third variable, because this study specifically examined whether female participants took the initiative to request that a boyfriend used a condom or another contraceptive method, the response ‘I suggested it’ was coded as 1 and all other responses (including ‘My boyfriend suggested it,’ ‘Nobody suggested it; I used it by myself’, ‘Nobody suggested it; my boyfriend used it by himself,’ and ‘I don’t want to answer’) were recoded as 0. As these binary outcome variables could not be examined using LVM, we used logistic regression modelling to test the association among these behaviours and perceived subordination and sexual communication self-efficacy. For the perceived subordination and sexual communication self-efficacy variables in this case, we summed the original scores to generate a single continuous variable. This practice was justified because the factor loadings of items onto corresponding latent variables were comparable in measurement models (data not shown).
Results
Of 1208 completed questionnaires, 27 were excluded due to missing data (i.e. more than one of eight pages was unmarked). The final sample size was 1181 respondents (881 from Can Tho University and 300 from An Giang University). Table 3 displays participants’ characteristics. The average age of participants was 21.6 years (range = 19–27, s.d. = 1.0). They represented 37 areas of study, including both the natural and social sciences. Among those who reported ever having a boyfriend (‘ever-partnered’) (72.4%, n = 852), most had had one (62%) or two (26%) boyfriends. Among those who currently had a boyfriend (53.5%, n = 633), the average length of the relationship was 20.2 months (maximum = 108 months, s.d. = 17.6). For those who reported ever having a boyfriend (72.4%, n = 852), 44.8% indicated that the boyfriend had asked for sex. A total of 111 unmarried participants had ever had penile–vaginal sex, accounting for 9.4% of the whole sample (n = 1181) and for 13.0% of ever-partnered participants (n = 852). Only one participant was married at the time of first sexual intercourse and this case was excluded from further analyses. A separate subset of 88 unmarried participants had had oral sex, representing 7.5% of the whole sample and 10.3% of ever-partnered participants (n = 852). About 16% of ever-partnered participants refused to disclose their sexual status or left the question unmarked; this subgroup did not differ from those who answered the question by age, academic year, urban vs. rural residence, religious beliefs, ethnicity or perceived subordination (P-values ranged from 0.12 to 0.86). Of those who had ever had penile–vaginal sex, 33% did not use any contraceptive method at first sex. For those who did, the most commonly used methods included emergency contraceptive pills (43.5%), condoms (32.4%) and withdrawal (20.3%). The percentages of participants who reported having had penile–vaginal sex and who reported contraceptive use at first sex did not differ statistically between those reporting religious beliefs versus those who did not, between those living in urban versus rural areas, and between the two universities (all P-values > 0.22).
Table 3.
Survey participant characteristics (n = 1181)
| Characteristic | n | % |
|---|---|---|
| Academic year | ||
| Third year | 1145 | 97.0 |
| Residence within the Mekong Delta | 1170 | 99.1 |
| Rural | 775 | 66.1 |
| Urban | 308 | 26.3 |
| Religion† | ||
| No religion | 714 | 60.5 |
| Buddhism | 290 | 24.6 |
| Catholicism | 61 | 5.2 |
| Hoa Hao | 87 | 7.4 |
| Cao Dai | 16 | 1.4 |
| Ethnicity | ||
| Kinh | 1124 | 95.2 |
| Chinese | 20 | 1.7 |
| Khmer | 23 | 1.9 |
Hoa Hao is a traditional religion based on Buddhism; Cao Dai is a traditional religion inspired by the three teachings from Buddha, Sage, and Saint.
Perceived subordination, sexual communication self-efficacy, and actual sexual communication
Table 2 displays the means and standard deviations of measured items for perceived subordination and sexual communication self-efficacy. Table 4 shows the descriptive statistics of endogenous variables in the latent variable models and dependent variables in the logistic regression.
Table 4.
Descriptive statistics of dependent and endogenous variables
| Variables | n | % |
|---|---|---|
| Frequency of discussing safer sex matters in the past month (among students who currently had had a boyfriend(s) for ≥6 months) | 465 | |
| Never | 212 | 45.6 |
| Once | 99 | 21.3 |
| Twice | 69 | 14.8 |
| Three times | 38 | 8.2 |
| Four times | 14 | 3.0 |
| Five times or more | 33 | 7.1 |
| Frequency of discussing contraceptive use (among sexually experienced survey respondents) | 111 | |
| Never | 8 | 7.2 |
| Rarely | 6 | 5.4 |
| Sometimes | 27 | 24.3 |
| Often | 30 | 27.0 |
| Every time we have sex | 40 | 36.0 |
| Frequency of asking for condom use (among sexually experienced survey respondents) | 111 | |
| Never | 20 | 18.0 |
| Rarely | 10 | 9.0 |
| Sometimes | 22 | 19.8 |
| Often | 18 | 16.2 |
| Every time we have sex | 41 | 36.9 |
| Contraceptive use at first sex (among sexually experienced survey respondents) | 111 | |
| Yes | 71 | 65.1 |
| Types of contraceptive used at first sex | 71 | |
| Emergency contraception pill | 30 | 43.5 |
| Condom | 23 | 32.4 |
| Rhythm method | 2 | 2.9 |
| Withdrawal | 14 | 20.3 |
| Who suggested contraceptive use at first sex | 71 | |
| I suggested it | 28 | 39.4 |
| My boyfriend suggested it | 28 | 39.4 |
| Nobody suggested it; I used it by myself | 0 | 0.0 |
| Nobody suggested it; my boyfriend used it by himself | 11 | 15.5 |
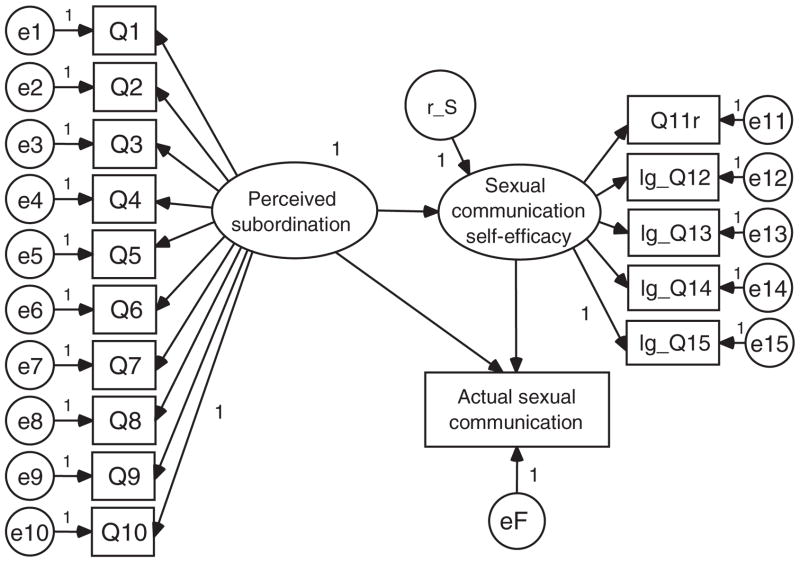
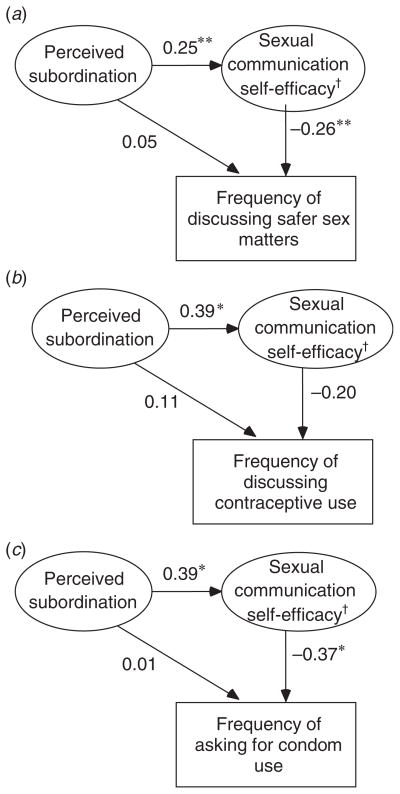
Figure 1 shows the model used to examine the associations among perceived subordination, sexual communication self-efficacy and three outcomes of actual sexual communication: frequency of discussing safer sex matters (assessed among participants who currently had boyfriends for 6 months or longer), frequency of discussing contraceptive use and frequency of asking for condom use (the latter two were assessed in sexually experienced participants). Three parameters of interest in this model included the regression paths between perceived subordination and sexual communication self-efficacy, between sexual communication self-efficacy and actual sexual communication, and between perceived subordination and actual sexual communication. The coefficients of these three paths for each outcome of actual sexual communication are shown in Fig. 2. For the frequency of discussing safer sex matters, an outlying modification index in the initial run of the model indicated a potential correlation between the error terms of item Q11 ‘I can easily initiate and conduct a conversation about safer sex with my boyfriend,’ (abbreviated as e11) and of the outcome variable (abbreviated as eF). Given the very close relatedness in the content of item Q11 and the frequency of discussing safer sex matters, we allowed this correlated error. All three models had a good fit (Table 5). Perceived subordination was consistently associated with sexual communication self-efficacy in all three models. Sexual communication self-efficacy was associated with frequency of discussing safer sex matters and frequency of asking for condom use, but was not associated with frequency of discussing contraceptive use. All other parameters were statistically significant at the <0.05 level except the marginal significance of the factor loading from perceived subordination onto item Q1 (P = 0.07).
Fig. 1.
Model of hypothesised relationships among perceived subordination, sexual communication self-efficacy and actual sexual communication.
Note: All items’ scores of sexual communication self-efficacy were reversed. Q indicates an item with corresponding question number. lg_Q denotes a base-10 logarithm transformation of the reversed score due to the score’s slightly non-normal distribution. r_S stands for residual; e stands for error terms.
Fig. 2.
Path coefficients of hypothesised relationships among perceived subordination, sexual communication self-efficacy and actual sexual communication. (a) Actual sexual communication assessed as the frequency of discussing safe-sex matters. (b) Actual sexual communication assessed as the frequency of discussing contraceptive use. (c) Actual sexual communication assessed as the frequency of asking for condom use.
Note: *, P < 0.05; **, P < 0.001; †, reversed score: the higher the score, the lower the self-efficacy.
Table 5.
Model goodness-of-fit indices
| CMIN | TLI | CFI | RMSEA | SRMR | |||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | d.f. | P | CMIN/df | RMSEA | 90% CI | ||||
| Actual sexual communication outcomes: | |||||||||
| Frequency of discussing safer sex matters | 151.31 | 102 | <0.001 | 1.48 | 0.933 | 0.943 | 0.032 | 0.021–0.043 | 0.046 |
| Frequency of discussing contraceptive use | 105.98 | 103 | 0.400 | 1.03 | 0.983 | 0.985 | 0.016 | 0.000–0.053 | 0.071 |
| Frequency of asking for condom use | 110.34 | 103 | 0.290 | 1.07 | 0.959 | 0.965 | 0.025 | 0.000–0.057 | 0.072 |
CMIN, minimum discrepancy; TLI, Tucker–Lewis Index; CFI, comparative fit index; RMSEA, root mean square error of approximation; 90% CI, 90% confident interval; SRMR, standardised root mean square residual
Perceived subordination, sexual communication self-efficacy and actual sexual behaviour
Table 6 displays the results for logistic regression models with three sexual behavioural outcomes. Among those who ever had sex (n = 111), contraceptive use at first penile–vaginal sex was associated with higher sexual communication self-efficacy but was not associated with perceived subordination. For those who used a contraceptive method (n = 71), whether the contraceptive used was a condom and who suggested its use were not associated with perceived subordination nor with sexual communication self-efficacy.
Table 6.
Logistic regression results
| Independent variables | Dependent variable = contraceptive use (yes = 1) | Dependent variable = condom use (condom = 1, other contraceptive methods = 0) | Dependent variable = who suggested contraceptive use (self-suggested = 1, boyfriend suggested = 0) | |||
|---|---|---|---|---|---|---|
| eβ | P-value | eβ | P-value | eβ | P-value | |
| Perceived subordination | 1.02 | 0.535 | 1.01 | 0.820 | 1.01 | 0.721 |
| Safer sex communication self-efficacy | 1.13 | 0.039 | 1.15 | 0.092 | 0.93 | 0.207 |
| n | 111 | 71 | 71 | |||
| −2 × log-likelihood | 132.21 | 93.27 | 130.22 | |||
Discussion
The study findings indicated that about one-tenth of unmarried, female third-year students at two Mekong River Delta universities had ever had penile-vaginal sex and another one-tenth had experienced oral sex. However, almost 16% of subjects refused to answer questions about their sexual status and behaviours, suggesting that the percentage of sexually experienced students may have been underestimated. In the national SAVY results, 2.6% of unmarried females aged 18–25 years reported ever having had sex and only 14.7–22% viewed premarital sex as acceptable, indicating the existing social taboo on premarital sex.2 The figure in the current study is higher than the SAVY data but is in keeping with the levels of sexual experience previously reported among female Vietnamese undergraduate students in large cities.1 One reason for the lower level of sexual experience reported in the SAVY may have been the greater potential for under-reporting by young women due to cultural beliefs and the stigma attached to premarital sex.2 Our study may have benefited from being self-administered, in addition to other practices that ensured anonymity and confidentiality. Alternatively, these findings may indicate that university students hold more liberal views and hence may be more likely to engage in premarital sex than young women in nonacademic settings.
Participants who perceived women to have a subordinate status had lower sexual communication self-efficacy. Sexual communication self-efficacy was positively related to the frequency of safer sex discussions in the previous month and to the frequency of asking boyfriends to use condoms during actual sexual activity, but not to the frequency of discussing contraceptive use. As manifested in the models, we can interpret that the effect of perceived subordination on actual sexual communication was indirect, through sexual communication self-efficacy. Apart from this indirect pathway, the residuals were apparently negligible and caused an insignificant direct relationship between perceived subordination and actual sexual communication outcomes. Our findings corroborated existing evidence of the associations between gender-based power imbalance and young unmarried females’ ability to communicate or negotiate safer sex practices.26–28
Higher sexual communication self-efficacy was also associated with a higher likelihood of actually using a contraceptive method at first penile–vaginal sex. Sexual communication self-efficacy could have increased the likelihood of actual condom use at first sex compared with using another contraceptive method use; however, in the small sample (n = 71), the statistical power might have been insufficient to detect the association, generating a marginal P-value of 0.092. Studies worldwide have substantiated the relationships among safer sex communication self-efficacy, actual communication and actual condom use among youth.29–36 In the 2005 SAVY results, the most commonly selected contraceptive methods used by unmarried couples at first sex and last sex included condoms, withdrawal and the rhythm method. In our study, the most commonly used contraceptive methods were emergency contraceptive pills, condoms and withdrawal. Given the existing stigma against premarital sex in Vietnam, ‘young unmarried women who engage in premarital sex find it difficult or embarrassing to seek contraception and counselling’ and ‘when contraception was used, men often made the decision and chose the method’1. Among those who used emergency contraceptive pills at first sex in our study, no case reported that she used it by herself without communicating with her partner about the use. Presumably, the contraceptive methods which the unmarried couples commonly selected, even including emergency contraceptive pills, required the agreement or assistance of the male partners. In most cases, contraception during premarital sex is not a solely the female’s decision but a mutual collaboration; hence frequent communication about its use becomes more critical. Therefore, it is imperative to address gender relations and safer sex communication self-efficacy in order to promote active communication and actual use of condoms or other contraceptive methods. Given our argument that contraceptive use is a mutual process, the promotion of equal or equitable gender relations and communication self-efficacy interventions should target both men and women, and should encourage shared responsibility in contraception practices.
Certain limitations in this study should be noted. The most apparent was the uncertainty in relationship directionality among latent variables due to the cross-sectional design. Although the inverse direction (e.g. sexual communication self-efficacy was a cause of perceived subordination) was unlikely, given findings from previous studies, it could be that both perceived subordination and sexual communication self-efficacy were independent outcomes of a certain unknown cause. A second limitation was that the temporal relationships of a few variables in the subgroup analyses might be ambiguous. Perceived subordination, for instance, was measured in the present and thus might differ from perceptions of subordination in the past, such as before first sex. This might be a reason for the nonassociation between perceived subordination and contraceptive use at first sex in the logistic regression model. However, the difference in perceived subordination, if any, was likely to bias results in one direction only, in that it would have diminished over the ensuing period. Finally, although a cluster effect may exist due to the cluster sampling, we judged that this effect was moderate because: (1) each course (subject) had one to eight sections or classes; (2) the classes were randomly selected; and (3) students taking a certain class unselectively came from different majors in the credit system.
Conclusion
A noticeable proportion of female undergraduate students in the Mekong Delta have engaged in premarital sexual activity. Attention to promoting sexual and reproductive health for this population is needed in order to protect against the potentially negative consequences related to unintended pregnancies, abortions and STI and HIV transmission. The use of the most commonly selected contraceptive methods for premarital sex could not be solely decided upon and executed by female students. Instead, they require the male partners’ agreement or cooperation; hence the desire for contraceptive or condom use must be communicated and negotiated. Yet, sexual communication self-efficacy was consistently and inversely associated with perceived subordination. Female students who agreed on the subordinate status of women, which may translate into a power imbalance in interpersonal sexual relationships, had lower self-efficacy in communicating about contraceptive or condom use and ultimately were less likely to use them. Adding activities related to in-school gender equity promotion to sexual health campaigns at the university level or at earlier education levels (e.g. high schools) may more effectively foster female students’ safer sex discussions and practices. For out-of-school female adolescents and young women, whose perceived subordination is potentially more extreme, it may be even more necessary and important to to address gender relation issues at the interpersonal level in future sexual and reproductive health promotion interventions. These promotion programs should involve both males and females.
Acknowledgments
We gratefully acknowledge the Fogarty International Center, National Institutes of Health, USA (AITRP D43 TW007669) for funding this study and TCB’s education. TCB is also a fellow of the Vietnam Education Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Fogarty International Center, the National Institutes of Health or the Vietnam Education Foundation. We especially thank Can Tho University and An Giang University for assistance in data collection.
Footnotes
Conflicts of interest
None declared.
References
- 1.World Health Organization (WHO) Sexual and reproductive health of adolescents and youths in Vietnam: a review of literature and projects 1995–2002. Hanoi: WHO, Western Pacific Region; 2005. [Google Scholar]
- 2.Ministry of Health of Vietnam. Survey Assessment of Vietnamese Youth (SAVY) Hanoi: Ministry of Health of Vietnam, General Statistics Office of Vietnam, United Nations Children’s Fund, World Health Organization; 2005. [Google Scholar]
- 3.Mensch BS, Clark WH. Adolescents and social changes in Vietnam. Hanoi: Population Council, Institute of Sociology; 2000. [Google Scholar]
- 4.Francisco A, Dixon-Mueller R, d’Arcangues C. Research issues in sexual and reproductive health for low- and middle-income countries. Geneva: Global Forum for Health Research, World Health Organization; 2007. [Google Scholar]
- 5.Marston C, King E. Factors that shape young people’s sexual behaviour: a systematic review. Lancet. 2006;368(9547):1581–6. doi: 10.1016/S0140-6736(06)69662-1. [DOI] [PubMed] [Google Scholar]
- 6.Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, et al. Sexual behaviour in context: a global perspective. Lancet. 2006;368(9548):1706–28. doi: 10.1016/S0140-6736(06)69479-8. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) Promoting and safeguarding the sexual and reproductive health of adolescents. Geneva: WHO; 2006. [Google Scholar]
- 8.Consultation of Investment in Health Promotion. Link between gender and sexual and reproductive health in Vietnam. Hanoi: Consultation of Investment in Health Promotion; 2005. [Google Scholar]
- 9.Santillan D, Schuler S, Hoang Tu A, Tran Hung M, Bui Thi Thanh M. Limited equality: contradictory ideas about gender and the implications for reproductive health in rural Vietnam. Journal of Health Management. 2002;4(2):251–67. doi: 10.1177/097206340200400210. [DOI] [Google Scholar]
- 10.Scott S, Chuyen TTK. Gender research in Vietnam: traditional approaches and emerging trajectories. Womens Stud Int Forum. 2007;30(3):243–53. doi: 10.1016/j.wsif.2007.03.006. [DOI] [Google Scholar]
- 11.Bui TC. DrPH thesis. Houston: The University of Texas – Health Science Center at Houston, School of Public Health; 2010. Perceived gender relations and sexual relations among undergraduate female students in the Mekong Delta of Vietnam. [Google Scholar]
- 12.Lewis JE, Malow RM, Ireland SJ. HIV/AIDS risk in heterosexual college students. A review of a decade of literature. J Am Coll Health. 1997;45(4):147–58. doi: 10.1080/07448481.1997.9936875. [DOI] [PubMed] [Google Scholar]
- 13.Crosby RA, DiClemente RJ, Wingood GM, Salazar LF, Harrington K, Davies SL, et al. Identification of strategies for promoting condom use: a prospective analysis of high-risk African American female teens. Prev Sci. 2003;4(4):263–70. doi: 10.1023/A:1026020332309. [DOI] [PubMed] [Google Scholar]
- 14.DiIorio C, Dudley WN, Lehr S, Soet JE. Correlates of safer sex communication among college students. J Adv Nurs. 2000;32(3):658–65. doi: 10.1046/j.1365-2648.2000.01525.x. [DOI] [PubMed] [Google Scholar]
- 15.Noar SM, Carlyle K, Cole C. Why communication is crucial: meta-analysis of the relationship between safer sexual communication and condom use. Journal of Health Communication. 2006;11(4):365–90. doi: 10.1080/10810730600671862. [DOI] [PubMed] [Google Scholar]
- 16.Bui TC, Diamond PM, Markham C, Ross MW, Nguyen-Le T-A, Tran LHT. Gender relations and sexual communication among female students in the Mekong River Delta of Vietnam. Culture, Health & Sexuality: An International Journal for Research. Culture, Health & Sexuality. 2010;12(6):591–601. doi: 10.1080/13691050902968769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Connell R. Gender and power. Stanford: Stanford University Press; 1987. [Google Scholar]
- 18.Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman & Co; 1997. [Google Scholar]
- 19.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. Speaking of health: assessing health communication strategies for diverse populations. Washington D. C: National Academy Press; 2002. [PubMed] [Google Scholar]
- 21.Center for HIV Identification, Prevention and Treatment Services. Instrument bank home. Los Angeles: Center for HIV Identification, Prevention and Treatment Services; 2006. Available online at: http://chipts.ucla.edu/assessment/ib_directory.asp [verified September 2007] [Google Scholar]
- 22.Forsyth AD, Carey MP. Measuring self-efficacy in the context of HIV risk reduction: research challenges and recommendations. Health Psychology. 1998;17(6):559–68. doi: 10.1037/0278-6133.17.6.559. [DOI] [PubMed] [Google Scholar]
- 23.Byrne BM. Structural equation modeling with AMOS: basic concepts, applications, and programming. New Jersey: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- 24.Kline RB. Principles and practice of structural equation modeling. 2. New York: The Guilford Press; 2005. [Google Scholar]
- 25.Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 26.Boer H, Mashamba T. Gender power imbalance and differential psychosocial correlates of intended condom use among male and female adolescents from Venda, South Africa. Br J Health Psychol. 2007;12(1):51–63. doi: 10.1348/135910706X102104. [DOI] [PubMed] [Google Scholar]
- 27.Langen TT. Gender power imbalance on women’s capacity to negotiate self-protection against HIV/AIDS in Botswana and South Africa. Afr Health Sci. 2005;5(3):188–97. doi: 10.5555/afhs.2005.5.3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wingood GM, DiClemente RJ, Harrington KF, Lang DL, Davies SL, Hook EW, et al. Efficacy of an HIV prevention program among female adolescents experiencing gender-based violence. Am J Public Health. 2006;96(6):1085–90. doi: 10.2105/AJPH.2004.053595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Babalola S. Gender differences in the factors influencing consistent condom use among young people in Tanzania. Int J Adolesc Med Health. 2006;18(2):287–98. doi: 10.1515/IJAMH.2006.18.2.287. [DOI] [PubMed] [Google Scholar]
- 30.Brien TM, Thombs DL, Mahoney CA, Wallnau L. Dimensions of self-efficacy among three distinct groups of condom users. J Am Coll Health. 1994;42(4):167–74. doi: 10.1080/07448481.1994.9939665. [DOI] [PubMed] [Google Scholar]
- 31.Halpern-Felsher BL, Kropp RY, Boyer CB, Tschann JM, Ellen JM. Adolescents’ self-efficacy to communicate about sex: its role in condom attitudes, commitment, and use. Adolescence. 2004;39(155):443–56. [PubMed] [Google Scholar]
- 32.Mahoney CA, Thombs DL, Ford OJ. Health belief and self-efficacy models: their utility in explaining college student condom use. AIDS Educ Prev. 1995;7(1):32–49. [PubMed] [Google Scholar]
- 33.Raiford JL, Wingood GM, DiClemente RJ. Correlates of consistent condom use among HIV-positive African American women. Womens Health (Lond Engl) 2007;46(2–3):41–58. doi: 10.1300/J013v46n02_04. [DOI] [PubMed] [Google Scholar]
- 34.Sayles JN, Pettifor A, Wong MD, MacPhail C, Lee SJ, Hendriksen E, et al. Factors associated with self-efficacy for condom use and sexual negotiation among South African youth. J Acquir Immune Defic Syndr. 2006;43(2):226–33. doi: 10.1097/01.qai.0000230527.17459.5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schroder KE, Johnson CJ, Wiebe JS. An event-level analysis of condom use as a function of mood, alcohol use, and safer sex negotiations. Arch Sex Behav. 2009;38(2):283–9. doi: 10.1007/s10508-007-9278-9. [DOI] [PubMed] [Google Scholar]
- 36.Taffa N, Klepp KI, Sundby J, Bjune G. Psychosocial determinants of sexual activity and condom use intention among youth in Addis Ababa, Ethiopia. International Journal of STD & AIDS. 2002;13(10):714–9. doi: 10.1258/095646202760326480. [DOI] [PubMed] [Google Scholar]