Abstract
We report a case of thymic carcinoma presenting as unilateral shoulder pain for 13 months. Before an accurate diagnosis was made, the patient received conservative treatment, cervical discectomies, and myofascial trigger point injection, none of which relieved his pain. When thymic carcinoma was eventually diagnosed, he received total resection of the tumor and the shoulder pain subsided completely. Thymic carcinoma is a rare carcinoma, and our review of the literature did not show shoulder pain as its initial presentation except for one case report. The purpose of this report is to document our clinical experience so that other physiatrists can include thymic carcinoma in their differential diagnosis of shoulder pain.
Keywords: referred pain, shoulder pain, thymic carcinoma
Introduction
Shoulder pain is a very common complaint, and several major etiologies include rotator cuff injury, adhesive capsulitis, shoulder instability, and arthritis.1 However, one should not exclude the possibility of referred pain from another anatomic location. The documented potential sources of referred pain to the shoulder include cervical spondylolysis, cervical arthritis, cervical disc disease, myocardial ischemia, diaphragmatic irritation, reflex sympathetic dystrophy, thoracic outlet syndrome, and gallbladder disease.2 It is very important to accurately identify the underlying etiology in order to effectively treat shoulder pain.
Thymic carcinoma is a rare carcinoma arising from the thymic epithelium presenting with highly malignant features such as adjacent tissue invasion and metastases.3 It represents less than 1% of thymic tumors, but often presents with advanced disease upon diagnosis, with a reported 5-year survival of 30%–50%.3,4 Typical initial presentations of thymic carcinoma include cough, chest pain, phrenic nerve palsy, or superior vena cava syndrome; these features can also be identified as incidental findings.3
We report a case with chronic right shoulder pain as the initial major symptom of thymic carcinoma. Incidentally, shoulder pain has long been a recognized feature of referred pain from phrenic nerve pathology and diaphragmatic irritation.5 Although the association between shoulder pain and the existence of a neoplasm has been previously described,6,7 we were unable to identify this occurrence in English-language based literature search.
Case description
A 48-year-old male with no systemic disease or trauma history visited his family physician’s clinic at a teaching hospital for recurrent right shoulder pain, which had been bothering him for approximately 6 months. The pain was dull in nature and was typically aggravated after shoulder movement. The pain intensity measured on an 11-point pain intensity numerical rating scale (NRS)8 was 5–6. Physical examination of the right shoulder revealed that the pain was located at the upper portion of right trapezius muscle, with local tenderness over this area. The range of motion, manual muscle testing, and sensation of right shoulder region were all within normal limits. The supraspinatus tendinitis test, Apley scratch test, Speed’s test, Hawkins-Mennedy test, and Lippman’s test were all negative. Myofascial trigger points (MTrPs) were identified in the right supraspinatus muscle, right infraspinatus muscle, right upper trapezius muscle and right lower trapezius muscle.
Under the impression that soft tissue injury was the cause of his pain, he received conservative treatment. However, the patient responded poorly to medication and physical therapy. Five months later, he visited a neurosurgeon, who arranged a magnetic resonance image (MRI) of the cervical spine, which revealed multiple mild herniated intervertebral discs, including C3/4, C4/5, and C6/7, with posterior compression to the spinal cord. Thus, the patient received anterior disectomies at C4/5 and C5/6 and interbody fusion of C4/5, C5/6 with polyetheretherketone cages. Unfortunately, the pain did not improve after the surgery, so he visited a physiatry clinic, where MTrPs were identified in the right upper trapezius muscle, right lower trapezius muscle, right rhomboid major and minor muscles, and right infraspinatus muscle. MTrPs were identified based on the following criteria: (1) exquisite painful spot in a taut band, (2) pain recognition at the spot, (3) typical referred pain pattern.9,10 Therefore, trigger points injection was performed, which relieved his shoulder pain for several days. However, the pain eventually recurred approximately 1–2 weeks after injection. Moreover, there was an increased frequency of intermittent right chest pain.
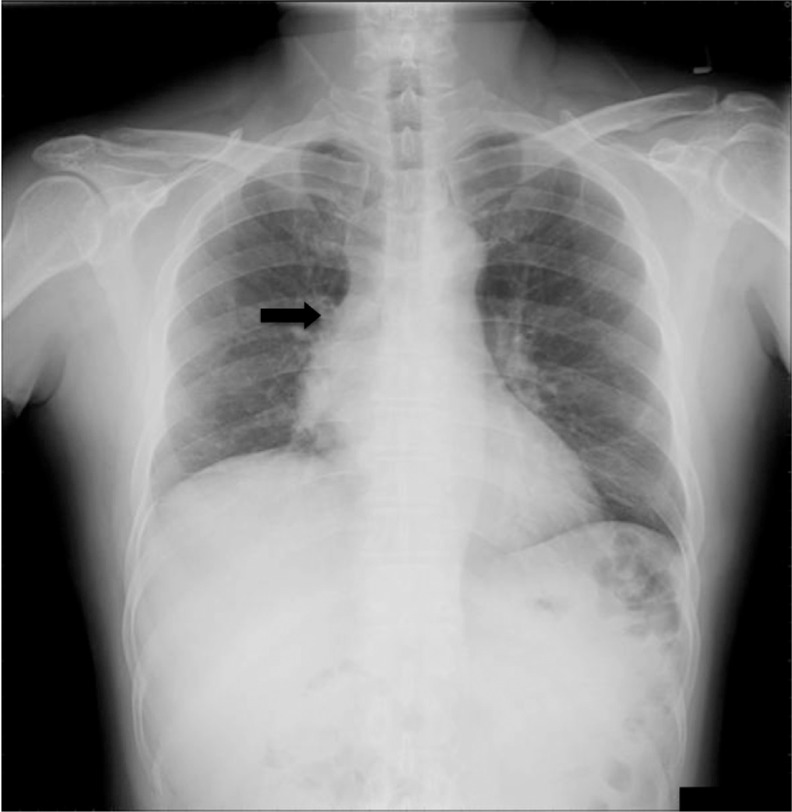
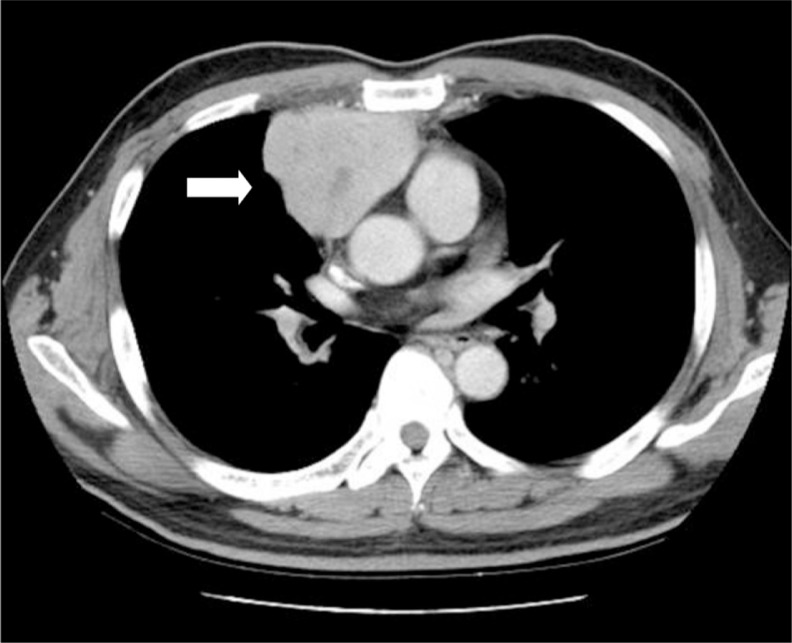
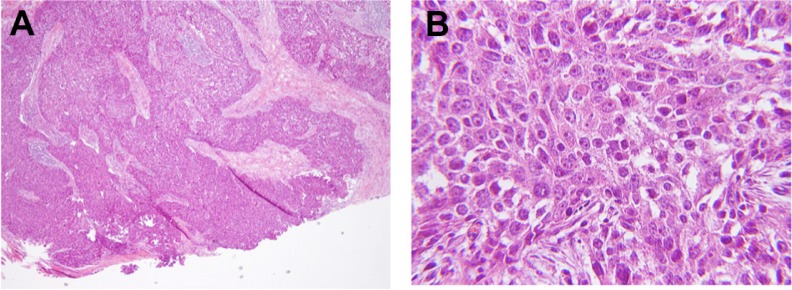
Due to new-onset and progressively worsening dull chest pain, additional diagnostic studies were performed. A chest X-ray revealed enlargement of the right hilum when compared with previous films (Figure 1). Computed tomography (CT) disclosed an anterior mediastinal tumor (Figure 2), and thymic carcinoma was suspected. After a CT-guided biopsy, squamous cell carcinoma of thymic origin was confirmed. Within a few days, the patient received total resection of mediastinal tumor and operative findings revealed a large, white, solid, and hard tumor containing a fibrotic change approximately 10 cm ×9 cm ×5 cm in size with invasion to pericardial membrane, right phrenic nerve, and right side parietal pleura. The pathologic sections from total resection of the thymus showed thymic carcinoma with epitheloid tumor cells, nuclear pleomorphism, apparent nucleoli, and mitotic feature in a solid nest or sheet arrangement (Figure 3). Immunohistochemical analysis showed positive cytokeratin, positive c-Kit (CD117), and negative leukocyte common antigen (LCA) in the tumor cells, which is consistent with thymic carcinoma.
Figure 1.
Chest X-ray indicating enlargement of the right hilar area and suspicious mass in the right heart border.
Figure 2.
Chest CT showing an anterior mediastinal tumor, approximately 69 ×55 ×68 mm in size.
Abbreviation: CT, computed tomography.
Figure 3.
Pathology slides from total thymus resection showed thymic carcinoma composed of epitheloid tumor cells with nuclear pleomorphism, apparent nucleoli, and mitotic features (H&E, 400×) in solid nest or sheet arrangement (H&E, 100×).
Abbreviation: H&E, hematoxylin and eosin.
After the surgery, the patient achieved significant relief of the right shoulder pain (to NRS 2–3) and chest pain. He underwent scheduled chemotherapy and radiation therapy thereafter. During follow-up examination three months later, the previously identified MTrPs were shown to have transformed from active to latent MTrPs. The patient no longer experienced spontaneous pain (NRS = 0) or noticed a recognizable painful spot.
Discussion
In this case report of thymic carcinoma, the initial and persistent manifestation was right shoulder pain. Right shoulder pain can result from referred pain, possibly as a result of pericardial or phrenic nerve involvement from the tumor. Anatomically, it has been documented that the phrenic nerve provides sensory innervations to the diaphragm, most structures of the mediastinum (ie, the mediastinal pleura and the pericardium), and even some abdominal structures (ie, superior peritoneum, liver, or gallbladder).11 Because the phrenic nerve originates from the fourth cervical nerve, which also provides cutaneous innervation for the anterior aspect of the shoulder girdle,11–13 it may explain the referred pain to the shoulder. In a review of current literature, referred pain to the shoulder from the mediastinal area has been described and documented in anatomic textbooks14 and several other clinical diagnoses.5,12,15–18 Some examples include (1) post-thoracotomy ipsilateral shoulder pain due to irritation of the pericardium or mediastinal and diaphragmatic pleural surfaces;15–17 (2) post laparoscopic shoulder pain after various laparoscopic surgical procedures due to overstretching of the diaphragmatic muscle fibers induced by the pressure of the pneumoperitoneum;12,18 or (3) shoulder pain as a symptom of lung cancer with intrathoracic injury of the phrenic nerve and its relief by mediastinal irradiation.5 In this case report, the clinical mechanism of shoulder pain was very similar to the third situation described above. However, we were unable to identify literature written in English regarding thymic carcinoma with shoulder pain as the initial clinical manifestation, except for one case.19 In that case, the author reported a case of thymic carcinoma with left shoulder pain lasting for two years without other major symptoms before diagnosis. Unfortunately, however, the topic of the article focused on medicolegal issues, and there was no further discussion regarding the correlation between shoulder pain and thymic carcinoma. This extremely limited documentation may be due to the rarity of thymic carcinoma, its aggressiveness and its poor prognosis.20
The most common initial presentations of thymic carcinoma include chest pain, shortness of breath, cough, superior vena cava syndrome, or phrenic nerve palsy due to direct compression or invasion of the tumor mass. In some patients, thymic carcinomas were incidentally found during routine chest radiographs.3,4 Other nonspecific symptoms include malaise, weight loss, fatigue, fever, and anorexia.21,22 Rarely, paraneoplastic syndrome and myasthenia gravis were reported in well-differentiated thymic carcinomas.4 In most instances, invasion of adjacent mediastinal structures or metastatic spread had already occurred at the time of diagnosis of thymic carcinoma.4,20
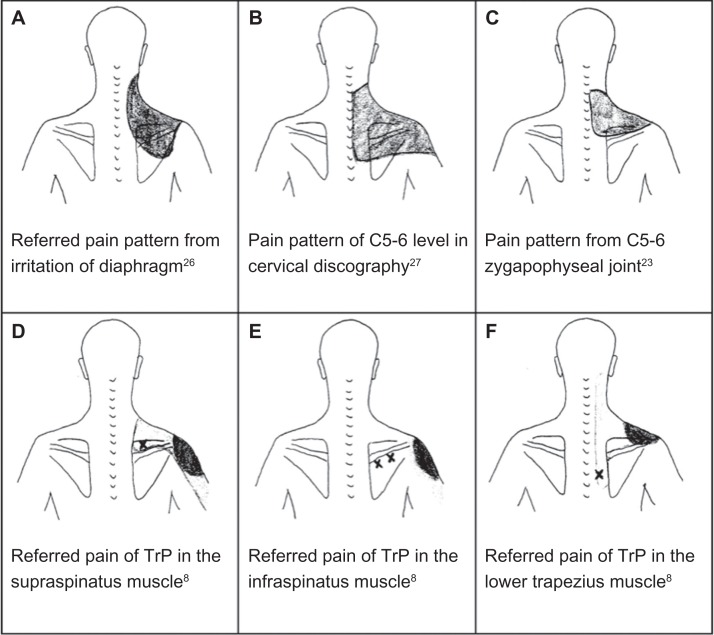
Notably, our patient also experienced superimposed myofascial pain (pain due to MTrP) and cervical discogenic pain. A review of previous literature revealed that the most frequent site of referred pain via phrenic nerve is around the lateral third of the trapezius border, extending to the acromion.23 This area overlapped with the referred pain pattern of several trigger points of trapezius muscle proposed by Simons et al,9 and the pain referral map of C4/5, C5/6, C6/7 intervertebral discs proposed by Slipman et al,24 and the pain referral from C5/6, C6/7 facet joints proposed by Dwyer et al25 (Figure 4). After suffering from right shoulder pain for five months, the patient received discectomies for C4/5, C5/6 with interbody fusion because the origin of pain from herniated intervertebral discs C4/5 and C5/6 were revealed by MRI. Unfortunately, the tumor mass did not appear on the MRI at that time since the non-contrast MRI conducted before surgery was focused on the C-spine, in which the lowest spinal level was shown only to T3. However, chest CT with contrast conducted eight months later revealed that the highest level of the anterior mediastinal mass began approximately at the T5 level. Additionally, the mass was likely smaller before disc surgery. The patient received trigger point injections, which relieved the pain according to the patient. In the perspective of myofascial pain syndrome, Hong has proposed the hypothesis that a persistent or recurrent trigger point is typically caused by an underlying lesion other than the muscle itself.26,27 Therefore, it is possible that the phrenic nerve lesion caused by thymic carcinoma can also elicit pain due to MTrP. In such a case, identifying and treating the etiological lesion to eliminate chronic pain remains very useful and crucial. The purpose of this report is to document our experience of shoulder pain as a symptom of referred pain from thymic carcinoma due to phrenic nerve invasion, which may be very similar to myofascial pain syndrome, pain from a cervical disc, or referred pain from the zygapophyseal joint.
Figure 4.
Several possible etiologies in the diagnosis of chronic shoulder pain.
Conclusion
Chronic shoulder pain may be an initial major manifestation of thymic carcinoma likely due to phrenic nerve or pericardium involvement, and this type of pain may be similar to myofascial pain syndrome, neurogenic pain from a cervical disc, and referred pain from the zygapophyseal joint. With the correct diagnosis, the treating physician can solve the patient’s pain problem rather than providing symptomatic treatment. We hope that our clinical experience may assist other physicians who diagnose and treat shoulder pain.
Footnotes
Disclosure
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
References
- 1.Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: part I. Evaluation and diagnosis. Am Fam Physician. 2008;77(4):453–460. [PubMed] [Google Scholar]
- 2.Stevenson JH, Trojian T. Evaluation of shoulder pain. J Fam Pract. 2002;51(7):605–611. [PubMed] [Google Scholar]
- 3.Eng TY, Fuller CD, Jagirdar J, Bains Y, Thomas CR., Jr Thymic carcinoma: state of the art review. Int J Radiat Oncol Biol Phys. 2004;59(3):654–664. doi: 10.1016/j.ijrobp.2003.11.021. [DOI] [PubMed] [Google Scholar]
- 4.Srirajaskanthan R, Toubanakis C, Dusmet M, Caplin ME. A review of thymic tumours. Lung Cancer. 2008;60(1):4–13. doi: 10.1016/j.lungcan.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 5.Khaw PY, Ball DL. Relief of non-metastatic shoulder pain with mediastinal radiotherapy in patients with lung cancer. Lung Cancer. 2000;28(1):51–54. doi: 10.1016/s0169-5002(99)00112-9. [DOI] [PubMed] [Google Scholar]
- 6.Huygen F, Patijn J, Rohof O, et al. 9. Painful shoulder complaints. Pain Pract. 2010;10(4):318–326. doi: 10.1111/j.1533-2500.2010.00389.x. [DOI] [PubMed] [Google Scholar]
- 7.House J, Mooradian A. Evaluation and management of shoulder pain in primary care clinics. South Med J. 2010;103(11):1129–1137. doi: 10.1097/SMJ.0b013e3181f5e85f. [DOI] [PubMed] [Google Scholar]
- 8.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 9.Simons DG, Travell JG, Simons LS. Travell and Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Baltimore: Williams & Wilkins; 1999. [Google Scholar]
- 10.Hong CZ. Muscle Pain Syndromes. In: Braddom RL, editor. Physical Medicine and Rehabilitation. 4th ed. Philadelphia: Elsevier Saunders; 2011. pp. 971–1001. [Google Scholar]
- 11.Schuenke M, Schulte E, Schumacher U, et al. Neck and Internal Organs. Stuttgart: Thieme; 2006. (THIEME Atlas of Anatomy). [Google Scholar]
- 12.Shin HY, Kim SH, Lee YJ, Kim DK. The effect of mechanical ventilation tidal volume during pneumoperitoneum on shoulder pain after a laparoscopic appendectomy. Surg Endosc. 2010;24(8):2002–2007. doi: 10.1007/s00464-010-0895-3. [DOI] [PubMed] [Google Scholar]
- 13.Petchkrua W, Harris SA. Shoulder pain as an unusual presentation of pneumonia in a stroke patient: a case report. Arch Phys Med Rehabil. 2000;81(6):827–829. doi: 10.1016/s0003-9993(00)90119-9. [DOI] [PubMed] [Google Scholar]
- 14.Williams PL, Warwick R, Dyson M, et al. Gray’s Anatomy. Edinburgh: Churchill Livingston; 1989. [Google Scholar]
- 15.Tan N, Agnew NM, Scawn ND, Pennefather SH, Chester M, Russell GN. Suprascapular nerve block for ipsilateral shoulder pain after thoracotomy with thoracic epidural analgesia: a double-blind comparison of 0.5% bupivacaine and 0.9% saline. Anesth Analg. 2002;94(1):199–202. doi: 10.1097/00000539-200201000-00038. table of contents. [DOI] [PubMed] [Google Scholar]
- 16.Scawn ND, Pennefather SH, Soorae A, Wang JY, Russell GN. Ipsilateral shoulder pain after thoracotomy with epidural analgesia: the influence of phrenic nerve infiltration with lidocaine. Anesth Analg. 2001;93(2):260–264. doi: 10.1097/00000539-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Barenys C, Busquets J, de Castro PE, et al. Randomized double-blind comparison of phrenic nerve infiltration and suprascapular nerve block for ipsilateral shoulder pain after thoracic surgery. Eur J Cardiothorac Surg. 2011;40(1):106–112. doi: 10.1016/j.ejcts.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 18.Suginami R, Taniguchi F, Suginami H. Prevention of post laparo-scopic shoulder pain by forced evacuation of residual CO2. JSLS. 2009;13(1):56–59. [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor P, Collier J, Bower J, Freedman C, Ellis P. Delay in diagnosing thymic carcinoma leading to cerebral infarct and death. Clinical Risk. 2010;16:74–75. [Google Scholar]
- 20.Magois E, Guigay J, Blancard PS, et al. Multimodal treatment of thymic carcinoma: Report of nine cases. Lung Cancer. 2008;59(1):126–132. doi: 10.1016/j.lungcan.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 21.Moran CA, Suster S. Thymic carcinoma: current concepts and histologic features. Hematol Oncol Clin North Am. 2008;22(3):393–407. doi: 10.1016/j.hoc.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Chung DA. Thymic carcinoma – analysis of nineteen clinicopathological studies. Thorac Cardiovasc Surg. 2000;48(2):114–119. doi: 10.1055/s-2000-9868. [DOI] [PubMed] [Google Scholar]
- 23.Morton DP, Callister R. Factors influencing exercise-related transient abdominal pain. Med Sci Sports Exerc. 2002;34(5):745–749. doi: 10.1097/00005768-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Slipman CW, Plastaras C, Patel R, et al. Provocative cervical discography symptom mapping. Spine J. 2005;5(4):381–388. doi: 10.1016/j.spinee.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers. Spine (Phila Pa 1976) 1990;15(6):453–457. doi: 10.1097/00007632-199006000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Hong CZ. Considerations and recommendations regarding myofascial trigger point injection. J Musculoskeletal Pain. 1994;2(1):29–59. [Google Scholar]
- 27.Hsu HC, Hong CZ. Floating kidney with chronic myofascial pain syndrome in the abdominal muscles as the major clinical manifestation: A case report. J Musculoskeletal Pain. 2008;16(3):199–204. [Google Scholar]
- 28.Moore KL, Dalley AF. Clinically oriented anatomy. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 29.Grubb SA, Kelly CK. Cervical discography: clinical implications from 12 years of experience. Spine (Phila Pa 1976) 2000;25(11):1382–1389. doi: 10.1097/00007632-200006010-00010. [DOI] [PubMed] [Google Scholar]