Abstract
Regulatory T-cells (Tregs) constitute a small subset of cells that are actively involved in maintaining self-tolerance, in immune homeostasis and in antitumor immunity. They are thought to play a significant role in the progression of cancer and are generally increased in patient with chronic lymphocytic leukemia (CLL). Their number correlates with more aggressive disease status and is predictive of the time to treatment, as well. Moreover, it is now clear that dysregulation in Tregs cell frequency and/or function may result in a plethora of autoimmune diseases, including multiple sclerosis, type 1 diabetes mellitus, myasthenia gravis, systemic lupus erythematosus, autoimmune lymphoproliferative disorders, rheumatoid arthritis, and psoriasis. Efforts are made aiming to develop approaches to deplete Tregs or inhibit their function in cancer and autoimmune disorders, as well.
A Brief History
The human immune system is a well-coordinated network of cells, organs and glands acting in harmony to protect the host from a broad range of pathogenic microorganisms and, at the same time, to avoid responsiveness to self-antigens (immunological self-tolerance) and to control the quality and the magnitude of immune responses to non-self-antigens thus avoiding damage to the host (immune homeostasis). Several mechanisms are thought to be involved in this complex control system (Table 1). In this scenario, a distinct small subset of specialized T-lymphocytes, the so-called regulatory T-cells (Tregs), seem to play a pivotal role in maintaining homeostasis and self-tolerance.1,2 In fact, Tregs act suppressing the function of self-reactive T-cells to protect the host from autoimmune disease. At the same time they seem to be able to prevent antitumor immune responses.3
Table 1.
The main mechanisms of immunological tolerance
| Central tolerance | Clonal deletion |
| Clonal anergy | |
| Receptor editing | |
| Peripheral tolerance | Immune deviation |
| Suppression | |
| Immune privilege | |
| Network-mediated regulation | |
| Coreceptor modulation |
Gershon and Kondo of Yale University firstly proposed the existence of T-cells with suppressive activity more than 40 years ago.4 However, its better identification lacked for several years and this field of research shrank until to 1995, when Shimon Sakaguchi and coworkers identified a population of CD4+ T-cells expressing surface interleukin-2 (IL)-2 receptor α-chain (recognized by CD25) and termed them ‘regulatory’ T-cells.5 However, CD25 is not exclusively restricted to Tregs because of its expression on the surface of T effector lymphocytes after activation.6 Baecher-Allan and co-workers, by means of flow cytometry and in vitro study of sorted cells, identified a very small subset of T cells with high expression of CD25 that exhibited a strong regulatory function in humans.7–9 CD4+CD25+high cells inhibited proliferation and cytokine secretion by activated CD4+CD25+ responder T-cells in a contact-dependent manner.
In addition, it has been experimentally demonstrated that depleting Tregs produces inflammatory bowel disease, resulting from excessive immune response to intestinal commensal bacteria.10 Finally, reducing or removing Tregs leads to effective tumor immunity leading in turn to tumor eradication.11,12
More recently, the intracellular transcription factor forkhead/winged helix box P3 (FoxP3), also called scurfin, has been identified as the most accepted marker for Tregs.13–15 It functions regulating a set of genes involved in the suppression, proliferation and metabolic activities of Tregs. Moreover, CD127, that identified the heterodimeric IL-7 receptor, combined with CD4, CD25 and FoxP3, has been shown to better identify Tregs avoiding the contamination of this small cell population (accounting for 1–4% of circulating CD4+ lymphocytes in humans) with activated T-cells.16,17
Tregs and Autoimmunity
It is now clear that dysregulation in Tregs cells may result in a plethora of autoimmune diseases, including multiple sclerosis, type 1 diabetes mellitus, myasthenia gravis, systemic lupus erythematosus, autoimmune lymphoproliferative disorders, rheumatoid arthritis, and psoriasis.18
As a matter of the fact, complex genetic disorders typically associated with the MHC chromosomal region as well as the dysregulation of Treg cells frequency and/or function appear to be involved in autoimmune diseases.19 In particular, FoxP3, IL-2 and relative receptor play a key role in the maintenance of Tregs associated pathological immune responses.20
Deficiency in FoxP3 due to genetic mutations results in a lethal X-linked recessive lymphoproliferative disease in mice and human subjects characterized by immunodysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome.21 This autoimmune disorder is characterized by a severe intestinal pathology, with massive T-cell infiltration, type 1 diabetes mellitus, eczema, anemia, liver infiltration, thrombocytopenia, hypothyroidism, and the presence of various autoantibodies. FoxP3 deficiency was also found in the multiple sclerosis although Treg cells frequency was comparable with healthy individuals.22,23 Similar results emerged in type 1 autoimmune diabetes, psoriasis, myasthenia gravis and autoimmune polyglandular syndromes (APS).24–26 The degree of deficiency of functional anomaly of FoxP3+ natural Tregs is able to alter the manifestation of autoimmunity. Alterations of Tregs were also reported in rheumathoid arthtritis and in idiopathic juvenile arthritis. Results obtained may suggest a possible role of Tregs in the downregulation of the joint inflammation.27
Defining Tregs
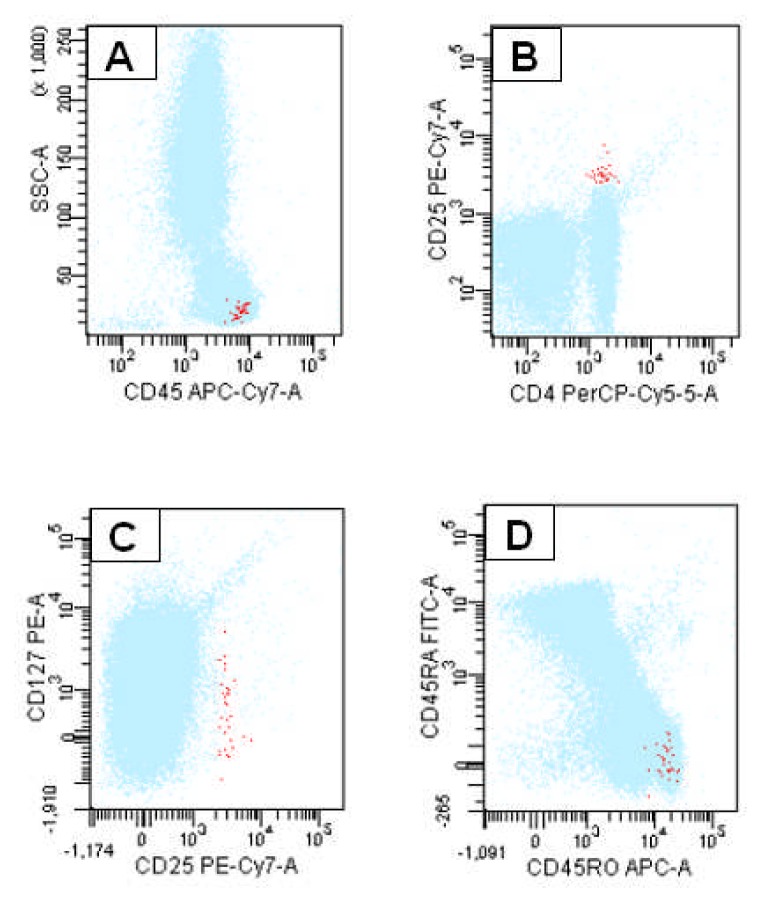
Taken all above into account, Tregs may be defined as a small population of T-cells with a relevant role in the immune homeostasis. For this reason, they are actively involved in the immunosurveillance against autoimmune disorders and cancer, as well. Tregs may be defined as CD4+ T-cells expressing CD25 at high levels, cytoplasmic FoxP3, and very low to undetectable CD127 on their surface (Figure 1). However, several other markers have been associated to Tregs, but none of them may be considered as a unique marker (Table 2).
Figure 1.
Flow cytometric detection of Tregs. Tregs are CD4+ lymphocytes displaying a CD45 expression of T-cell subpopulations (A). CD25 antigen is expressed at high density whereas CD127 at low to undetectable levels (B and C).Selected CD25+/CD127+ lymphocytes are positive for CD45RO (D).
Table 2.
Immunophenotype of Tregs
| Antigen | Expression |
|---|---|
| CD4 | Positive |
| CD8 | Negative |
| CD25 | High |
| CD127 | Low to undetectable |
| FoxP3 | Positive |
| GITR | High |
| IL-10 | Positive |
| TGF-β | Positive |
| CD152 (CTLA-4) | High |
| CD154 (CD40L) | Negative |
| CD45RA | Negative |
| CD45RO | Positive |
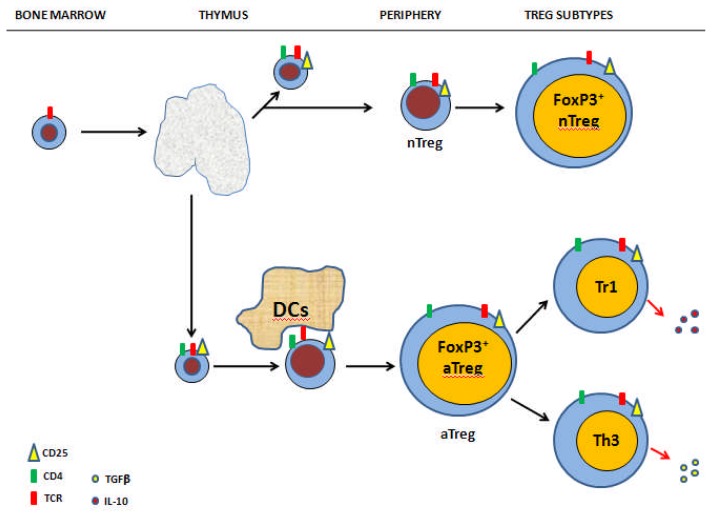
Two main subsets of Tregs have been described according to their origin. Innate (or naturally occurring) Tregs originate in the thymus as a consequence of the interaction with high-affinity antigens expressed in thymic stroma and constitutively expressing FoxP3.28 They are involved in immune homeostatis, thus suppressing the response against self antigens. Such cells persist throughout life despite thymic involution after puberty. Adaptative Tregs emerges also from the thymus but acquire its suppressive activity in periphery regulating the response against self and non-self-antigens.29 Figure 2 summarizes the generation and subpopulations of Tregs.
Figure 2.
Regulatory T-cells: development and subsets. Three major subjects of Tregs have been recognized so far. A) Tregs (innate and adaptative): they express CD25, FoxP3, CTLA-4, αβ-TCR, and secrete the immunosuppressive lymphokines IL-10 and TGF-β. B) Tr1 cells: they do not express FoxP3 nor large amount of CD25, secrete IL-10 and TGF-β. Tr1 cells are abundant in the intestine where they elicit their main function that is making tolerance to the many agents that are part of its diet. C) Th3 cells: they are also prevalent in the intestine and like to Tr1 cells act suppressing immune responses to ingested antigens (oral tolerance) by means of TGF-β secretion.
Tregs have been shown to suppress the proliferation of antigen-stimulated naïve T-cells and several mechanisms have been suggested by means of which they elicit their suppressive activity.30,31 Either natural and adaptative Tregs are antigen-specific and are seen to need T-cell receptor (TCR) triggering to become suppressive31,32 despite this latter point is still controversial.33, In vitro studies suggested that activated Tregs suppress activated CD4+ or CD8+ effector T-cells by means of cell-to-cell contact. In this mechanism a crucial role is played by the ligation of CD80/CD86 complex on effector cells by cytotoxic T-lymphocytes antigen-4 (CTLA-4) on Tregs surface resulting in the transmission of inhibitory signals of T-cell function.34,35 In a similar fashion, Tregs seem to modulate dendritic cells (DCs) function resulting in the expression and activation of indoleamine 2,3-dioxygenase degradation.36 DCs may be blocked in maturation and/or activation by release of IL-10 and TGF-β that resulting in antigen-presenting capacity impairment due to down-regulation of major histocompatibility complex (MHC) class II and in interfering in costimulatory molecules expression.37,38 Other in vitro studies suggest Tregs inhibition by means of the release of suppressive cytokines, such as IL-10 and TGF-β.39–41 Activated Tregs are capable to express granzyme A or perforin and kill activated CD4+ or CD8+ T-cells, through the perforin-dependent way.42,43
Tregs and Chronic Lymphocytic Leukemia
Chronic lymphocytic leukemia (CLL), the most common form of leukemia in Western countries, is characterized by the accumulation of monoclonal B-lymphocytes in bone marrow, lymphoid organs and peripheral blood.44 Moreover, there is increasing evidence of T cell dysfunction in CLL and this may probably contribute to the etiology and the progression of the disease.45,46 Several authors reported that Tregs are increased in CLL patients.47–51 Using multicolor flow cytometry, we showed that CLL patients had a higher absolute number of circulating Tregs compared to age and sex-matched controls.51 In addition, Tregs cell number was significantly correlated to more advanced Rai clinical stages, peripheral blood B-lymphocytosis, more elevated LDH levels, and absolute number of CD38+ neoplastic B-cells.
The evidence that Tregs are reduced after therapy with fludarabine, agrees with the hypothesis that these cells play a critical role in protecting CLL cells from getting killed by the immune system.47 The same happens when patients with CLL were treated with thalidomide.52 This drug and its analogues, such as lenalidomide, acts as immunomodulatory agents targeting the microenvironment and both are shown to be effective in the treatment of CLL patients, probably by means of TNF modulation.53–55
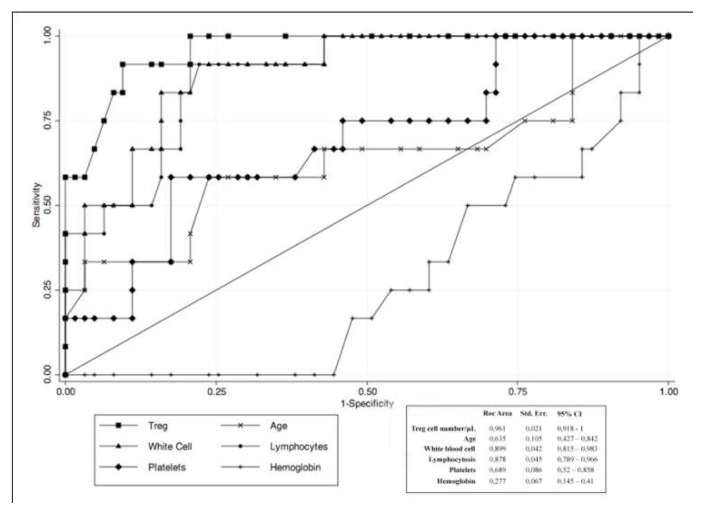
The prognostic role of Tregs have been poorly investigated. Only two paper reported that a shorter time to first treatment may be predicted by the circulating number of Tregs.56,57 As showed in Figure 3, we found a best predictive cut-off of absolute circulating Tregs able to identify patients with early stage CLL at higher risk of requiring therapy.57
Figure 3.
ROC curve graphically showing the trade-offs between sensitivity and specificity for different cutoffs used to discriminate between positive and negative cases (i.e., treatment demand vs no treatment demand patients). The best predictive cutoff of circulating Treg cell number seems to be in the range from ≥40 to ≥42/μL. The result of cutoff ≥41/μL shows the best predictive power among the others.
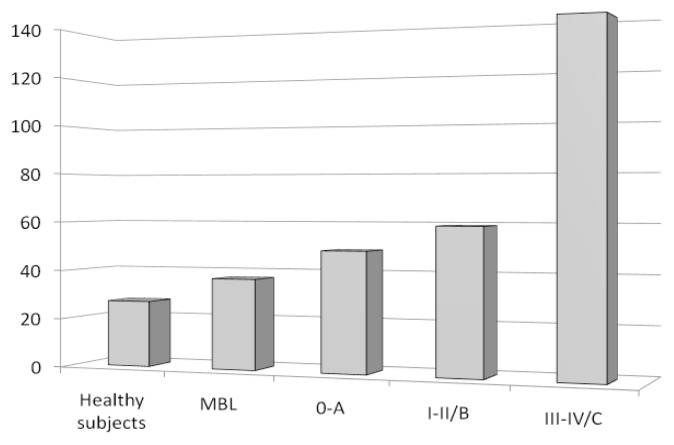
Finally, we have studied Tregs in ‘clinical’ monoclonal B-cell lymphocytosis (MBL), a condition in which less than 5000/μL circulating monoclonal B-cells, in absence of other features of lymphoproliferative disorders, is found.58 We showed that MBL patients had a lower absolute number of Tregs, compared to CLL patients, but higher than controls (Figure 4).59 Taken together, these data show that the tumor mass (from MBL low to intermediate to high-risk CLL) and the circulating Tregs increase simultaneously, thus suggesting that the expected result is a more robust inhibition of tumor inhibiting cells and, ultimately, a greater expansion of neoplastic B cells.
Figure 4.
Circulating Tregs number in healthy subjects, MBL and CLL patients grouped according to Rai/Binet clinical stages. Data are expressed as mean absolute circulating Tregs number (/μL) ± standard deviations.
Conclusions
Tregs play a critical role in immune tolerance (maintaining peripheral tolerance to self-antigens) and in immune homeostasis (regulating the immune response to non self-antigens). Moreover, it is now clear that Tregs have a role in suppressing tumor-specific immunity and for that reason are actively involved in the etiology and in progression of cancer, such as CLL, the most frequent form of leukemia in Western countries. Tregs disregulation is thought to be also involved in the pathogenesis of autoimmune disorders. In light of this, Tregs appear as having a great potential in treating autoimmunity and cancer. There is now considerable evidence in preclinical models to suggest that adoptive Tregs therapy will be highly efficacious. For that reason, clinical strategies are developing to target such cells aiming to modulate their suppressive function.60–65
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Jiang H, Chess L. Regulation of immune responses by T cells. N Engl J Med. 2006;354:1166–1176. doi: 10.1056/NEJMra055446. [DOI] [PubMed] [Google Scholar]
- 2.Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133:775–787. doi: 10.1016/j.cell.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Beyer M, Schultze JL. Regulatory T cells in cancer. Blood. 2006;108:804–811. doi: 10.1182/blood-2006-02-002774. [DOI] [PubMed] [Google Scholar]
- 4.Gershon R, Kondo K. Cell interactions in the induction of tolerance: the role of thymic lymphocytes. Immunology. 1970;18:723–737. [PMC free article] [PubMed] [Google Scholar]
- 5.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic tolerance maintained by activated T cells expressing IL-2 receptor α-chain (CD25): breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 6.Robb RJ, Munck A, Smith KA. T cell growth factor receptors. Quantitation, specificity, and biological relevance. J Exp Med. 1981;154:1455–1474. doi: 10.1084/jem.154.5.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baecher-Allan C, Brown JA, Freeman GJ, Hafler DA. CD4+CD25high regulatory cells in human peripheral blood. J Immunol. 2001;167:1245–1253. doi: 10.4049/jimmunol.167.3.1245. [DOI] [PubMed] [Google Scholar]
- 8.Baecher-Allan C, Viglietta V, Hafler DA. Human CD4+CD25+ regulatory T cells. Semin Immunol. 2004;16:89–97. doi: 10.1016/j.smim.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Baecher-Allan C, Hafler DA. Human regulatory T cells and their role in autoimmune disease. Immunol Rev. 2006;212:203–216. doi: 10.1111/j.0105-2896.2006.00417.x. [DOI] [PubMed] [Google Scholar]
- 10.Singh B, Read S, Asseman C, Malstrom V, Mottet C, Stephens LA, Stepankova R, Tlaskalova H, Powrie F. Control of intestinal inflammation by regulatory T cells. Immunol Rev. 2001;182:190–200. doi: 10.1034/j.1600-065X.2001.1820115.x. [DOI] [PubMed] [Google Scholar]
- 11.Wang HY, Wang RF. Regulatory T cells and cancer. Curr Opin Immunol. 2007;19:217–223. doi: 10.1016/j.coi.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Belkaid Y, Rouse BT. Natural regulatory T cells in infectious disease. Nat Immunol. 2005;6:353–360. doi: 10.1038/ni1181. [DOI] [PubMed] [Google Scholar]
- 13.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor FoxP3. Science. 2003;299:1057–1061. doi: 10.1126/science.1079490. [DOI] [PubMed] [Google Scholar]
- 14.Fontenot JD, Gavin MA, Rudensky AY. FOXP3 programs the development and function of CD4+CD25+ regulatory T-cells. Nat Immunol. 2003;4:330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 15.Rudensky AY, Fontenot JD. A well adapted regulatory contrivance: regulatory T cell development and the forkhead family transcription factor FoxP3. Nature Immunol. 2005;6:331–337. doi: 10.1038/ni1179. [DOI] [PubMed] [Google Scholar]
- 16.Seddiki N, Santner-Nanan B, Martinson J, Zaunders J, Sasson S, Landay A, Solomon M, Selby W, Alexander SI, Nanan R, Kelleher A, Fazekas de St Groth B. Expression of interleukin (IL)-2 and IL-7 receptors discriminate between human regulatory and activated T cells. J Exp Med. 2006;203:1693–1700. doi: 10.1084/jem.20060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu W, Putnam AL, Xu-Yu Z, Szot GL, Lee MR, Zhu S, Gottlieb PA, Kapranov P, Gingeras TR, Fazekas de St Groth B, Clayberger C, Soper DM, Ziegler SF, Bluestone JA. CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ Treg cells. J Exp Med. 2006;203:1700–1711. doi: 10.1084/jem.20060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dejaco C, Duftner C, Grubeck-Loebenstein B, Schirmer M. Imbalance of regulatory cells in human autoimmune diseases. Immunology. 2005;117:289–300. doi: 10.1111/j.1365-2567.2005.02317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hafler DA, de Jager PL. Applying a new generation of genetic maps to understand human inflammatory disease. Nat Rev Immunol. 2005;5:83–91. doi: 10.1038/nri1532. [DOI] [PubMed] [Google Scholar]
- 20.Sakaguchi S, Ono M, Setoguchi R, Yagi H, Hori S, Fehervari Z, Shimizu J, Takahashi T, Nomura T. Foxp3+ CD25+ CD4+ natural regulatory T cells in dominant self-tolerance and autoimmune disease. Immunol Rev. 2006;212:8–27. doi: 10.1111/j.0105-2896.2006.00427.x. [DOI] [PubMed] [Google Scholar]
- 21.Godfrey VL, Wilkinson JE, Russell LB. X-linked lymphoreticular disease in the scurfy (sf) mutant mouse. Am J Pathol. 1991;138:1379–1387. [PMC free article] [PubMed] [Google Scholar]
- 22.Viglietta V, Baecher-Allan C, Weiner HL, Hfler DA. Loss of cunctional suppression by CD4+CD25+ regulatory T cells in patients with multiple sclerosis. J Exp Med. 2004;199:971–979. doi: 10.1084/jem.20031579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huan J, Culbertson N, Spencer L, Bartholomew R, Burrows GG, Chou YK, Bourdette D, Ziegler SF, Offner H, Vandenbark AA. Decreased FOXP3 in multiple sclerosis patients. J Neurosci Res. 2005;81:45–52. doi: 10.1002/jnr.20522. [DOI] [PubMed] [Google Scholar]
- 24.Kriegel MA, Lohamann T, Gabler C, Blank N, Kalden JR, Lorenz HM. Defective suppressor function of human CD4+CD25+ regulatory T cells in autoimmune polygranular T cells in autoimmunepolygrandular syndrome type II. J Exp Med. 2004;199:1285–1891. doi: 10.1084/jem.20032158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balandina A, Lecart S, Dartevelle P, Saoudi A, Berrih-Aknin S. Functional defect of regulator CD4(+)CD25+ T cells in the thymus of patients with autoimmune myasthenia gravis. Blood. 2005;105:735–41. doi: 10.1182/blood-2003-11-3900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ono M, Shimizu J, Miyachi Y, Sakaguchi S. Control of autoimmune myocarditis and multi-organ inflammation by GITRhigh FoxP3- expressing CD25+ and CD25− regulatory T cells. J Immunol. 2006;176:4748–4756. doi: 10.4049/jimmunol.176.8.4748. [DOI] [PubMed] [Google Scholar]
- 27.Horak I, Lohler J, Ma A, Smith KA. Interleukin-2 deficient mice: a new model to study autoimmunity and self-tolerance. Immunol Rev. 1995;148:35–44. doi: 10.1111/j.1600-065X.1995.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 28.Aschenbrenner K, D’Cruz LH, Vollmann EH, Hintenberger M, Emmerich J, Swee LK, Rolink A, Klein L. Selection of FoxP3 regulatory T cells specific for self antigen expressed and presented by Aire+ medullary thymic epithelial cells. Nature Immunol. 2007;8:351–358. doi: 10.1038/ni1444. [DOI] [PubMed] [Google Scholar]
- 29.Piccirillo CA, Thornton AM. Cornerstone of peripheral tolerance: naturally occurring CD4+CD24+ regulatory T cells. Trends Immunol. 2004;25:374–380. doi: 10.1016/j.it.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Corthay A. How do regulatory T cells work? Scand J Immunol. 2009;70:326–336. doi: 10.1111/j.1365-3083.2009.02308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sakaguchi S, Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T. Regulatory T cells: how do they suppress immune responses? Int Immunol. 2009;21:1105–1111. doi: 10.1093/intimm/dxp095. [DOI] [PubMed] [Google Scholar]
- 32.Thornton AM, Shevac EM. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takahashi T, Kuniyasu Y, Toda M, Sakaguchi N, Itoh M, Iwata M, Shimizu J, Jakaguchi J. Immunologic self-tolerance maintained by CD25+CD4+ naturally anergic and suppressive T cells: induction of autoimmune disease by breaking their anergic/suppressive state. Int Immunol. 1998;10:1969–1980. doi: 10.1093/intimm/10.12.1969. [DOI] [PubMed] [Google Scholar]
- 34.Walunas TL, Bluestone JA. CTLA-4 regulates tolerance induction and T cell differentiation in vivo. J Immunol. 1998;160:3855–3860. [PubMed] [Google Scholar]
- 35.Shimuzu J, Yamazaki S, Takahashi T, Ishida Y, Sakaguchi S. Stimulation of CD25+CD4+ regulatory T cells through GITR breaks immunological self-tolerance. Nat Immunol. 2002;3:135–142. doi: 10.1038/ni759. [DOI] [PubMed] [Google Scholar]
- 36.Deaglio S, Dwyer KM, Gao W, Friedman D, Usheva A, Erat A, Chen JF, Enjyoji K, Linden K, Oukka M, Kuchroo VK, Strom TB, Robson SC. Adenosine generations catalyzed by CD39 and CD73 expressed on regulatory T cells mediates immune suppression. J Exp Med. 2007;204:1257–1265. doi: 10.1084/jem.20062512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geissmann F, Revy P, Regnault A, Lepelletier Y, Dy M, Brousse N, Amigorena S, Hermine O, Durandy A. TGF-beta 1 prevents the noncognate maturation of human dendritic Langherans cells. J Immunol. 1999;162:4567–4575. [PubMed] [Google Scholar]
- 38.Strobl H, Knapp W. TGF-β1 regulation of dendritic cells. Microbes Infection. 1999;1:1283–1290. doi: 10.1016/S1286-4579(99)00256-7. [DOI] [PubMed] [Google Scholar]
- 39.Shevac EM. CD4+CD25+ suppressor T cells: more questions than answers. Nat Rev Immunol. 2002;2:389–400. doi: 10.1038/nri821. [DOI] [PubMed] [Google Scholar]
- 40.Taylor A, Vehagen J, Blaser K, Akdis M, Akdis CA. Mechanisms of immune suppression by interleukin-10 and transforming growth factor-β: the role of T regulatory cells. Immunol. 2006;117:443–442. doi: 10.1111/j.1365-2567.2006.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levings MK, Bacchetta R, Schulz U, Roncarolo MG. The role of IL-10 and TGF-β in the differentiation and effector function of T regulatory cells. Int Arch Allergy Immunol. 2002;129:263–276. doi: 10.1159/000067596. [DOI] [PubMed] [Google Scholar]
- 42.Grossman WJ, Verbsky JW, Barchet W, Colonna M, Atkinson JP, Ley TJ. Human T regulatory cells can use the perforin pathway to cause autologous target cell death. Immunity. 2004;21:589–601. doi: 10.1016/j.immuni.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 43.Grossman WJ, Verbsky JW, Tollefsen BL, Kemper C, Atkinson JP, Levy TJ. Differential expression of granzymes A and B in human cytotoxic lymphocyte subsets and T regulatory cells. Blood. 2004;104:2840–2848. doi: 10.1182/blood-2004-03-0859. [DOI] [PubMed] [Google Scholar]
- 44.Chiorazzi N, Rai KR, Ferrarini M. Chronic lymphocytic leukemia. N Engl J Med. 2005;352:804–815. doi: 10.1056/NEJMra041720. [DOI] [PubMed] [Google Scholar]
- 45.Scrivener S, Goddard RV, Kaminski ER, Prentice AG. Abnormal T-cell function in B-cell chronic lymphocytic leukaemia. Leuk Lymphoma. 2003;44:383–389. doi: 10.1080/1042819021000029993. [DOI] [PubMed] [Google Scholar]
- 46.Christopoulos P, Pfeifer D, Bartholome K, Follo M, Timmer J, Fisch P, Veelken H. Definition and characterization of the systemic T-cell dysregulation in untreated indolent B-cell lymphoma and very early CLL. Blood. 2011;117:3836–3846. doi: 10.1182/blood-2010-07-299321. [DOI] [PubMed] [Google Scholar]
- 47.Beyer M, Kochanek M, Darabi K, Popov A, Jensen M, Endl E, Knolle PA, Thomas RK, von Bergwelt-Baildon M, Debey S, Hallek M, Schultze JL. Reduced frequencies and suppressive function of CD4+CD25hi regulatory T cells in patients with chronic lymphocytic leukemia after therapy with fludarabine. Blood. 2005;106:2018–2025. doi: 10.1182/blood-2005-02-0642. [DOI] [PubMed] [Google Scholar]
- 48.Giannopoulos K, Schmitt M, Kowal M, Wlasiuk P, Bojarska-Junak A, Chen J, Rolinski J, Dmoszynska A. Characterization of regulatory T cells in patients with B-cell chronic lymphocytic leukemia. Oncol Rep. 2008;20:677–682. [PubMed] [Google Scholar]
- 49.Deutsch V, Pierry C, Polliack A. Expansion of regulatory T cells in B chronic lymphocytic leukemia: enhanced ‘brakes’ on host immunity. Leuk Lymphoma. 2009;50:687–688. doi: 10.1080/10428190902954389. [DOI] [PubMed] [Google Scholar]
- 50.Jak M, Mous R, Remmerswaal EBM, Spijker R, Jaspers A, Yague A, Eldering E, van Lier RAW, Van Oers MHJ. Enhanced formation and survival of CD4+CD25highFoxP3+ T-cells in chronic lymphocytic leukemia. Leuk Lymphoma. 2009;50:788–801. doi: 10.1080/10428190902803677. [DOI] [PubMed] [Google Scholar]
- 51.D’Arena G, Laurenti L, Minervini MM, Deaglio S, Bonello L, De Martino L, De Padua L, Savino L, Tarnani M, De Feo V, Cascavilla N. Regulatory T-cell number is increate in chronic lymphocytic leukemia patients and correlate with progressive disease. Leuk Res. 2011;35:363–368. doi: 10.1016/j.leukres.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 52.Giannopoulos K, Schmitt M, Wlasiuk P, Chen J, Bojarska-Junak A, Kowal M, Rolinski J, Dmoszynska A. The high frequency of T regulatory cells in patients with B-cell chronic lymphocytic leukemia is diminished through treatment with thalidomide. Leukemia. 2008;22:222–224. doi: 10.1038/sj.leu.2404869. [DOI] [PubMed] [Google Scholar]
- 53.Valencia X, Stephens G, Goldbach-Mansky R, Wilson M, Shevach EM, Lipsky PE. TNF downmodulates the function of human CD4+CD25hi T-regulatory cells. Blood. 2006;108:253–261. doi: 10.1182/blood-2005-11-4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramsay AG, Gribben JG. Immune dysfunction in chronic lymphocytic leukemia T cells and Lenalidomide as an immunodulatory drug. Haematologica. 2009;94:1198–1202. doi: 10.3324/haematol.2009.009274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee B-N, Gao H, Cohen EN, Badoux X, Wierda WG, Estrov Z, Faderl SH, Keating MJ, Ferrajoli A, Reuben JM. Treatment with Lenalidomide modulates T-cell immunophenotype and cytokine production in patients with chronic lymphocytic leukemia. Cancer. 2011;117:3999–4008. doi: 10.1002/cncr.25983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weiss L, Melchardt T, Egle A, Grabmer C, Greil R, Tinhofer I. Regulatory T cells predict the time to initial treatment in early stage chronic lymphocytic leukemia. Cancer. 2011;117:2163–2169. doi: 10.1002/cncr.25752. [DOI] [PubMed] [Google Scholar]
- 57.D’Arena G, D’Auria F, Simeon V, Laurenti L, Deaglio S, Mansueto G, Del Principe MI, Statuto T, Pietrantuono G, Guariglia R, Innocenti I, Martorelli MC, Villani O, De Feo V, Del Poeta G, Musto P. A shorter time to the first treatment may be predicted by the absolute number of regulatory T-cells in patients with Rai stage 0 chronic lymphocytic leukemia. Am J Hematol. 2012;87:628–631. doi: 10.1002/ajh.23170. [DOI] [PubMed] [Google Scholar]
- 58.Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, Hillmen P, Keating MJ, Montserrat E, Rai KR, Kipps JK. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute– Working Group 1996 Guidelines. Blood. 2008;111:5446–5456. doi: 10.1182/blood-2007-06-093906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.D’Arena G, Rossi G, Minervini MM, Savino L, D’Auria F, Laurenti L, Del Principe MI, Deaglio S, Biagi A, De Martino L, De Feo V, Cascavilla N, Musto P, Del Poeta G. Circulating regulatory T cells in “clinical” monoclonal B-cell lymphocytosis. Int J Immunopathol Pharmacol. 2011;24:915–923. doi: 10.1177/039463201102400410. [DOI] [PubMed] [Google Scholar]
- 60.Chatila TA. Role of regulatory T cells in human disease. J Allergy Clin Immunol. 2005;116:949–959. doi: 10.1016/j.jaci.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 61.Colombo MP, Piconese S. Regulatory T-cell inhibition versus depletion: the right choice in cancer immunotherapy. Nature Rev. 2007;7:880–887. doi: 10.1038/nrc2250. [DOI] [PubMed] [Google Scholar]
- 62.Brusko TM, Putnam AL, Bluestone JA. Human regulatory T cells: role in autoimmune disease and therapeutic opportunities. Immunol Rev. 2008;223:371388. doi: 10.1111/j.1600-065X.2008.00637.x. [DOI] [PubMed] [Google Scholar]
- 63.Nizar S, Copier J, Meyer B, Bodman-Smith M, Galustian C, Kumar D, Dalgleish A. T-regulatory cell modulation: the future of cancer immunotherapy? Br J Caner. 2009;100:1697–1703. doi: 10.1038/sj.bjc.6605040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.D’Arena G, Deaglio S, Laurenti L, De Martino L, De Feo V, Fusco BM, Carella AM, Cascavilla N, Musto P. Targeting regulatory t cells for anticancer therapy. Mini-Rev Med Chem. 2011;11:480–485. doi: 10.2174/138955711795843365. [DOI] [PubMed] [Google Scholar]
- 65.Wright GP, Ehrenstein MR, Stauss HJ. Regulatory T-cell adoptive immunotherapy: potential for treatment of autoimmunity. Expert Rev Clin Immunol. 2011;7:213–225. doi: 10.1586/eci.10.96. [DOI] [PubMed] [Google Scholar]