Abstract
Wearable hip protectors (padded garments) represent a promising strategy to decrease impact force and hip fracture risk during falls, and a wide range of products are currently marketed. However, little is known about how design features of hip protectors influence biomechanical effectiveness. We used a mechanical test system (simulating sideways falls) to measure the attenuation in femoral neck force provided by 26 commercially available hip protectors at three impact velocities (2, 3, and 4 m/s). We also used a materials testing machine to characterize the force–deflection properties of each device. Regression analyses were performed to determine which geometric (e.g., height, width, thickness, volume) and force–deflection properties were associated with force attenuation. At an impact velocity of 3 m/s, the force attenuation provided by the various hip protectors ranged between 2.5% and 40%. Hip protectors with lower stiffness (measured at 500 N) provided greater force attenuation at all velocities. Protectors that absorbed more energy demonstrated greater force attenuation at the higher impact velocities (3 and 4 m/s conditions), while protectors that did not directly contact (but instead bridged) the skin overlying the greater trochanter attenuated more force at velocities of 2 and 3 m/s. At these lower velocities, the force attenuation provided by protectors that contacted the skin overlying the greater trochanter increased with increasing pad width, thickness, and energy dissipation. By providing a comparison of the protective value of a large range of existing hip protectors, these results can help to guide consumers and researchers in selecting hip protectors, and in interpreting the results of previous clinical trials. Furthermore, by determining geometric and material parameters that influence biomechanical performance, our results should assist manufacturers in designing devices that offer improved performance and clinical effectiveness.
Keywords: Hip protectors, Hip fractures, Proximal femur, Osteoporosis, Impact, Materials testing
1. Introduction
Hip fractures (i.e., fractures of the proximal femur) are a major public health problem for older adults. The lifetime risk for hip fracture in the USA is 17% for Caucasian women and 6% for Caucasian men (Cummings and Melton, 2002). While bone density is a major determinant of fracture risk, the majority of hip fractures occur in persons who do not suffer from osteoporosis (Dargent-Molina et al., 1996; Taylor et al., 2004). Instead, fall mechanics and the resulting loads applied to the proximal femur during impact are the factors most closely associated with the risk of suffering a hip fracture (Cummings and Nevitt, 1994). Sideways falls increase hip fracture risk by 5-fold when compared to forwards or backwards falls (Hayes et al., 1993); the risk increases by 32-fold when direct impact to the greater trochanter occurs (Nevitt and Cummings, 1993). Accordingly, protective devices that reduce the force applied to the proximal femur during fall-related impacts have the potential to reduce hip fracture risk.
Wearable hip protectors (padded garments) are a promising strategy for decreasing hip fracture risk by reducing the loads applied to the proximal femur during fall-related impacts. Until recently there were no established guidelines for assessing the biomechanical and clinical effectiveness of these devices (Cameron et al., 2010; Robinovitch et al., 2009). Consequently, there are currently more than two dozen commercially marketed hip protectors in North America that utilize a surprisingly diverse array of design philosophies, materials, and geometry. The first generation of hip protectors used ‘hard shell’ domes, which bridged over the greater trochanter, to shunt energy away from the proximal femur during impact (Kannus et al., 2000; Lauritzen et al., 1993). More recently, soft shell hip protectors have become more common. These products reduce the force applied to the proximal femur by absorbing energy in the pad material, and reducing the local stiffness over the greater trochanter through a “springs-in-series” mechanism (Laing and Robinovitch, 2008a, 2008b).
Researchers have shown that the biomechanical effectiveness (i.e. force attenuation capacity) of hip protectors is influenced by external factors including impact velocity, soft tissue properties, and pelvic surface geometry (Kannus et al., 1999; Laing and Robinovitch, 2008b; Mills, 1996; van Schoor et al., 2006). Presumably, pad geometry (thickness, surface area) and material properties (stiffness, damping) also affect force attenuation. In controlled experiments, Robinovitch et al. (1995) found that increasing the thickness of ‘horse-shoe’ shaped pads (of identical surface area) from 18 to 38 mm increased force attenuation by 66%. However, the force–deflection and geometric properties of commercially marketed hip protectors vary widely, and it is not known whether specific biomechanical variables govern (or explain) between-product variations in force attenuation. Such information should guide users in the selection of products, and manufacturers in the design of a new generation of hip protectors with increased biomechanical effectiveness.
The goals of this study were therefore to test the hypotheses that the force attenuation provided by a range of hip protectors when positioned correctly over the greater trochanter would significantly associate with their geometry (e.g. width, thickness) and force–deflection properties (e.g. stiffness, energy absorption). Towards these ends, we used a mechanical test system to measure the force attenuation provided by 26 commercially available hip protectors. For each hip protector, we also used a materials testing system to measure the force–deflection properties, and digital calipers to measure pad geometry. Regression analyses were used to test whether force attenuation depended on material and geometric properties.
2. Methods
2.1. Hip protector brands and characteristics
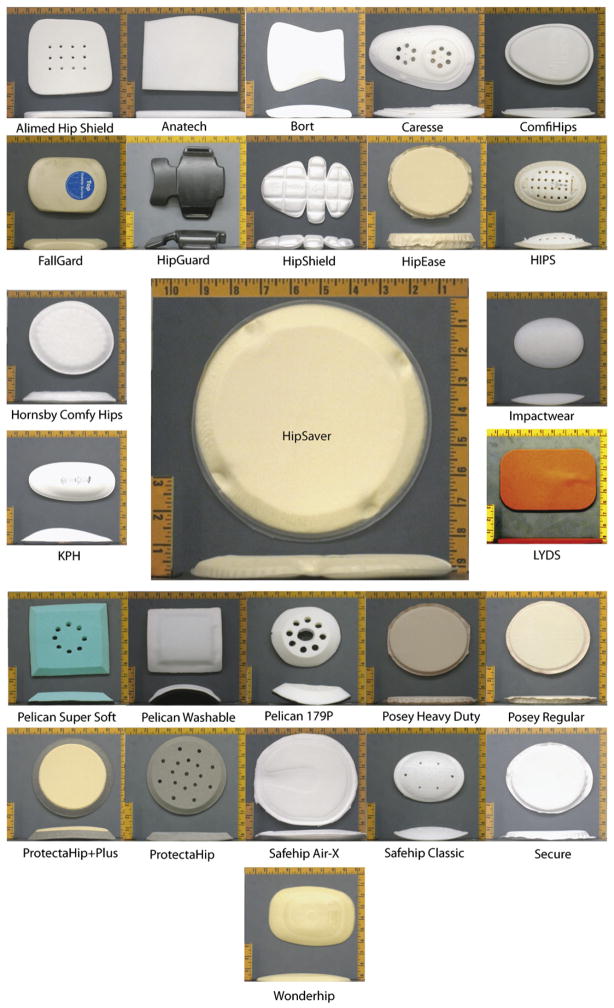
We used a combination of literature review and Internet searching (using search terms such as “hip protector”, “hip pad”, “seniors”, and “hip fracture”) to identify 26 commercially available hip protectors from distributors in nine different countries for testing (Table 1; Fig. 1). We used a binary variable (materialtype) to categorize the products according to their dominant material type (hard versus soft shell). Specifically, ‘soft shell’ protectors consisted primarily of foam and fabric (21 models), while ‘hard shell’ protectors contained a relatively stiff material that bridged over the greater trochanter (5 models). We also categorized the protectors based on their dominant geometry type (geometrytype), which describes the nature of the interface between the hip protector surface and the skin overlying the lateral pelvis. In particular, we categorized 21 models as ‘touching’, and 5 models as ‘not touching’ the skin directly overlying the greater trochanter. Basic information on the material types used in the each protector is available as Appendix A in supplementary website material.
Table 1.
Manufacturer, general design approach, and geometric variables measured from 26 hip protectors.
| Hip protector name | Company | Materialtype | Geometrytypea | Height (mm) | Width (mm) | Thickpad (mm) | Thickwearing (mm) | Volume (mm3) |
|---|---|---|---|---|---|---|---|---|
| Alimed® Hip Shield | AliMed® | Soft | Y | 170 | 190 | 14 | 14 | 452,200 |
| Anatech | Anatech | Soft | Y | 160 | 210 | 13.5 | 14 | 453,600 |
| Bort | Bort Medical | Soft | Y | 170 | 150 | 15 | 19 | 382,500 |
| Caresse | Remploy Healthcare | Hard | Y | 230 | 140 | 22 | 22 | 708,400 |
| ComfiHips™ | ComfiHips LLC | Soft | Y | 195 | 145 | 17.5 | 17 | 494,813 |
| FallGard | FallGard | Soft | Y | 175 | 120 | 17.5 | 19 | 367,500 |
| Hip Guard | HipGuard™ Ltd. | Hard | N | 155 | 165 | 20.4 | 19 | 521,730 |
| Hip Shield | Promedics | Soft | Y | 200 | 150 | 16 | 17 | 480,000 |
| HipEase | Patterson Medical/Sammons Preston | Soft | Y | 170 | 150 | 32 | 31 | 816,000 |
| HIPS | Qvortrup Medical A/S | Hard | N | 160 | 110 | 5 | 25 | 88,000 |
| Hipsaver® | Hipsaver® | Soft | Y | 220 | 200 | 18 | 19 | 792,000 |
| Hornsby Comfy Hip | Hornsby Comfy Hips Pty Ltd | Soft | Y | 195 | 165 | 18 | 21 | 579,150 |
| Impactwear® -Flexible | Impactwear | Soft | Y | 155 | 120 | 16 | 19 | 297,600 |
| KPH® | Medlogics | Hard | N | 190 | 95 | 15 | 31 | 270,750 |
| LYDS | Comfortable | Soft | Y | 205 | 135 | 6.5 | 7 | 179,888 |
| Pelican Super Soft | Pelican Manufacturing PTY LTD | Soft | Y | 170 | 160 | 21 | 22 | 571,200 |
| Pelican Washable | Pelican Manufacturing PTY LTD | Soft | Y | 160 | 150 | 17 | 18 | 408,000 |
| Pelican 179P | Pelican Manufacturing PTY LTD | Soft | Y | 155 | 140 | 23 | 24 | 499,100 |
| Posey Heavy Duty | J.T. Posey company | Soft | Y | 170 | 140 | 14.5 | 14 | 345,100 |
| Posey Regular | J.T. Posey company | Soft | Y | 165 | 140 | 13 | 13 | 300,300 |
| ProtectaHip+Plus® | Plum Enterprises INC | Soft | Y | 180 | 180 | 18 | 20 | 583,200 |
| ProtectaHip® | Plum Enterprises INC | Soft | Y | 180 | 180 | 14.5 | 16 | 469,800 |
| Safehip® Air-X™ | TYTEX A/S | Soft | N | 210 | 185 | 16 | 16 | 621,600 |
| Safehip® Classic | TYTEX A/S | Hard | N | 160 | 115 | 8.6 | 24 | 158,240 |
| Secure | Personal Safety Corporation | Soft | Y | 165 | 145 | 16 | 16 | 382,800 |
| WonderHip™ | Vital Base AS | Soft | Y | 193 | 137 | 15 | 16 | 396,615 |
Geometrytype indicates whether the protector touches (Y) or does not touch (N) the skin directly overlying the greater trochanter.
Fig. 1.
Photographs showing top and side views of the 26 hip protectors tested. Scale of individual photograph frames is 26.7 cm horizontal ×24.1 cm vertical (10.5 in. × 9.5 in.).
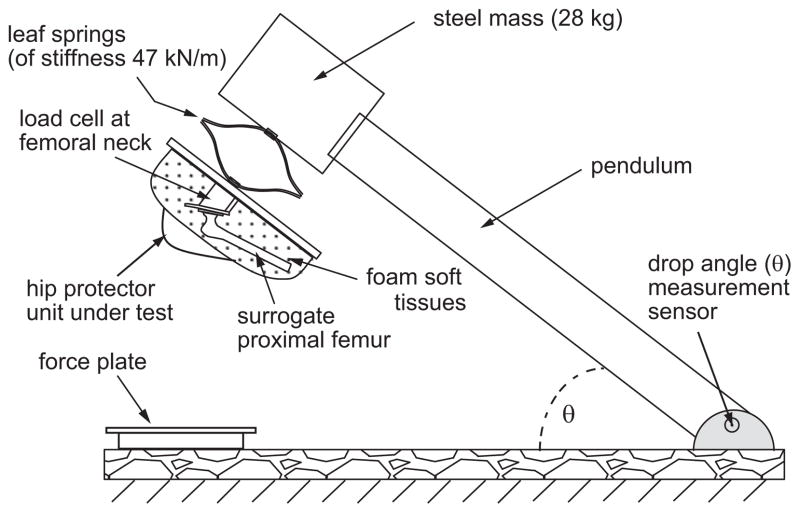
2.2. Impact force attenuation tests
We used the Simon Fraser University hip impact simulator (Fig. 2) to measure the biomechanical effectiveness of each hip protector. The system and test method have been described in detail previously (Laing and Robinovitch, 2008b, 2009), and are generally compatible with guidelines from an international team of biomechanics and clinical experts (Robinovitch et al., 2009). The system consists of an impact pendulum and surrogate pelvis released from an inclined position by an electromagnet to strike the ground in a horizontal position. The surrogate pelvis is comprised of foam-rubber soft tissues and an instrumented proximal femur (Sawbones, Vashon, WA, USA). Surface geometry and local variation in soft tissue stiffness match average measurements from older women to within one standard deviation (Laing and Robinovitch, 2008b). The surrogate pelvis is connected to the pendulum via leaf springs that simulate the compliance of the pelvis producing a total effective stiffness of 42.2 kN/m (Laing and Robinovitch, 2010; Robinovitch et al., 1997). The effective mass of the system (28.0 kg) is within one standard deviation of the mean measured from women during lateral falls on the hip (Robinovitch et al., 1997). Impact velocity is varied by adjusting the angle of the pendulum before release, and is measured by a rotary variable inductance transducer (Shaevitz RVIT 15-1201). The force applied to the femoral neck is measured by a load cell (Kistler Model 9712A5000, Amherst, NY, USA), and the total impact force is measured with a force plate (model 2535-08, Bertec Corp., Columbus, OH, USA). During test sessions, hip protectors were positioned according to manufacturer instructions with the aid of a laser that indicated the location of the greater trochanter within the surrogate pelvis.
Fig. 2.
Simon Fraser University hip impact simulator. The impact pendulum is connected in series with a surrogate pelvis. A load cell located in the femoral neck measures the force applied to the proximal femur during simulated sideways falls.
Based on findings that the impact velocity during unexpected sideways falls averages 3.0 m/s (SD 1.0 m/s) (Feldman and Robinovitch, 2007), we simulated mild (2 m/s), moderate (3 m/s), and severe (4 m/s) falls. For each impact velocity, we collected three unpadded trials, followed by two sequential trials with each hip protector. The hip protectors were tested in a random order. This number of repeated impacts is smaller than the five recommended in recent guidelines (Robinovitch et al., 2009), but the compromise was considered reasonable given the large number of hip protectors tested, and the observation that the difference in peak force between repeated trials was only 0.7%, on average. A 3 min refractory period was inserted after each trial. All hip protectors were preconditioned for at least 24 h in the test facility using a thermostat to maintain temperature at approximately 21 °C. Sensors were sampled for 2 s at 1000 Hz. Force data were filtered with a dual-pass fourth-order Butterworth low pass filter with a 35 Hz cut-off frequency (Labview 6.1, National Instruments, Austin, TX, USA). For each trial, we identified the peak femoral neck force (Fneck). For each hip protector, the attenuation in femoral neck force (Fneck_atten) was calculated as the average percentage decrease in Fneck in the padded trials compared to the unpadded conditions.
2.3. Geometric variables
We used digital callipers to measure the maximum dimensions of each protector in the inferior–superior (height) and anterior–posterior (width) directions. We also measured the outer- to inner-surface thickness of the portion of the pad that overlied the greater trochanter (thickpad), and the product of height, width, and thickpad (volume). Finally, we used a customized clamp (Fig. 3) to measure the increase in pelvic width in the frontal plane when wearing the protector (thickwearing, in mm resolution). In some cases, thickwearing was smaller than thickpad, due to the tight fit of the garment compressing the soft tissues of the surrogate pelvis. For protectors that bridged over the greater trochanter, a general approximation of the thickness of air gap between the medial aspect of the protector and the skin surface over the greater trochanter is given by subtracting thickpad from thickwearing (except for Hip Guard, for which the compression of the tissues over the greater trochanter was greater than the pad thickness in that area).
Fig. 3.
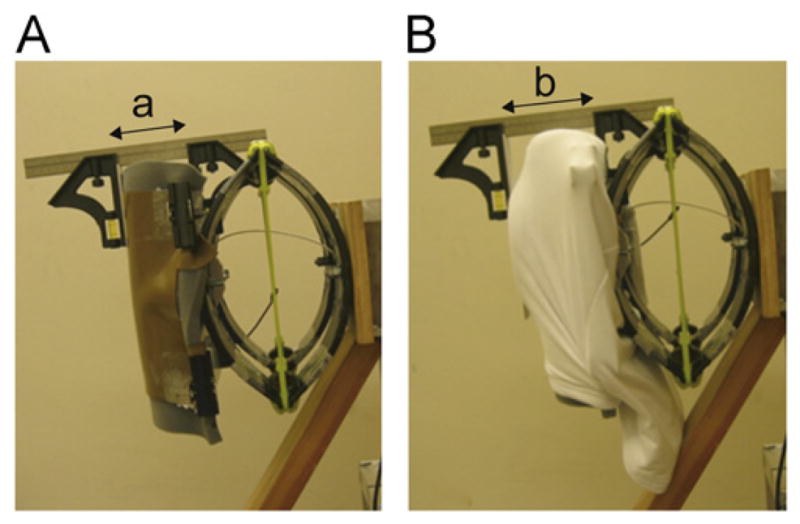
Illustration of the protocol for measuring the increase in pelvic width in the frontal plane when wearing the protector (thickwearing). This variable was calculated as the distance from the medial aspect of the surrogate pelvis to the lateral surface of the hip protector (measure ‘b’ in subplot B) minus the distance between the medial and lateral aspects of the unpadded surrogate pelvis (measure ‘a’ in subplot A).
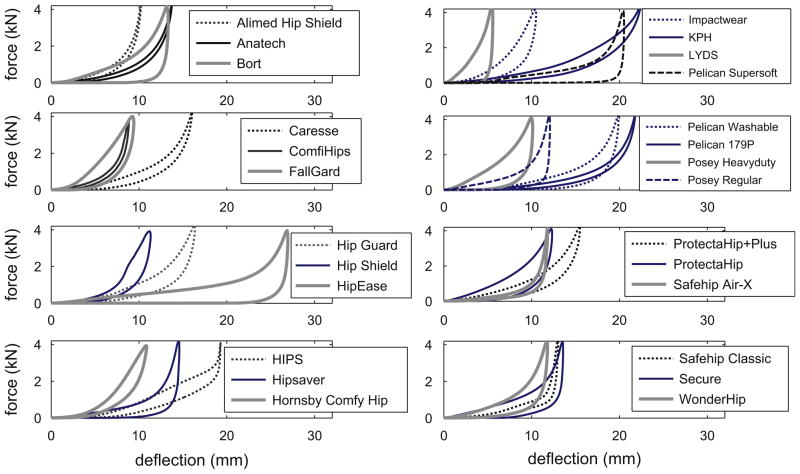
2.4. Force–deflection variables
We measured the force–deflection properties of each hip protector (Fig. 4) through dynamic indentation tests with a servohydraulic testing system (Fas-tTrack™ 8874, Instron Corporation, Canton, MA, USA). We used a rigid hip-shaped indenter that matched the pelvic surface geometry of a female model of body mass 49.1 kg and height 1.55 m (Laing et al., 2006). Trials were conducted using ramp loading and unloading rates of 35 mm/s to a peak force of 4 kN, the approximate peak load applied to the hip during a sideways fall from standing (Laing and Robinovitch, 2009; Laing et al., 2006). The data acquisition rate was 1000 Hz.
Fig. 4.
Force–deflection profile for each of the 26 hip protectors tested.
A custom software routine (Matlab v2006a, The Mathworks, Natick, MA, USA) was used to calculate the force–deflection outcomes of interest. Stiffness was measured as the tangent of the force–deflection curve during the compression phase at 500 N (k500), 2000 N (k2000), and 3000 N (k3000). Energy absorbed (Eabs) was calculated as the area under the force–deflection curve during the compression phase. Absolute energy dissipated (Edis) was calculated by subtracting from Eabs the area under the curve during the decompression phase. Relative energy dissipation (Edis%) was defined as (Edis/Eabs) × 100%
2.5. Statistics
We conducted separate linear regression analyses for the data at 2, 3, and 4 m/ s to determine whether the biomechanical effectiveness (Fneck_atten) of the hip protectors was associated with general material and geometry type (materialtype, geometrytype), geometric parameters (height, width, thickpad, volume, thickwearing) or force–deflection properties (k500, k2000, k3000, Eabs, Edis, Edis%). We initially conducted univariate analyses to identify the parameters (those with p<0.10) to include in the multivariate regression models. We then used backwards stepwise regression (removal from model: p>0.1) to determine the final predictive models. When we observed geometrytype as a significant predictor we performed subset analyses (using the same univariate/multivariate approach described above) to identify significant predictors of Fneck_atten for devices that did versus did not touch the skin overlying the greater trochanter. All analyses were performed with statistical analysis software (SPSS Version 17.0, Chicago, IL, USA).
3. Results
For each hip protector, geometric parameters are presented in Table 1, while the force–deflection properties and biomechanical effectiveness values are provided in Table 2. Fneck during the baseline unpadded conditions averaged 1392, 2100, and 2698 N for the 2, 3, and 4 m/s impact velocity conditions, respectively. Fneck during the padded condition ranged from 726 to 1478 at 2 m/s, 1271 to 2040 N at 3 m/s, and 1889 to 2630 N at 4 m/s. Corresponding values of Fneck_atten ranged from 38.4% to −6.4% (mean (SD)=20.2 (13.1)%) at 2 m/s, from 40% to 2.5% (mean (SD)=20.2 (9.1)%) at 3 m/s, and from 30.1% to 2.4% (mean (SD)=15.2% (6.6)%) at 4 m/s.
Table 2.
Force–deflection and biomechanical effectiveness variables measured from the 26 hip protectors.
| Hip protector name | k500 (kN/m) | k2000 (kN/m) | k3000 (kN/m) | Eabs (J) | Edis (J) | Edis% (%) |
Fneck_atten (%)
|
||
|---|---|---|---|---|---|---|---|---|---|
| 2 m/s | 3 m/s | 4 m/s | |||||||
| Alimed® Hip Shield | 183 | 963 | 1991 | 8.7 | 2.32 | 26.7 | 23.7 | 20 | 14.8 |
| Anatech | 144 | 677 | 1402 | 11.64 | 2.64 | 22.7 | 22.3 | 22.6 | 18.3 |
| Bort | 158 | 509 | 945 | 14.71 | 13.46 | 91.5 | 0.3 | 10.2 | 8.5 |
| Caresse | 151 | 472 | 965 | 15.43 | 5.91 | 38.3 | 30.9 | 22.1 | 15.4 |
| ComfiHips™ | 192 | 1432 | 2264 | 6.72 | 1.86 | 27.7 | 10.1 | 7.5 | 11.1 |
| FallGard | 349 | 587 | 740 | 13.1 | 9.03 | 68.9 | 2.9 | 12.4 | 10.7 |
| Hip Guard | 133 | 449 | 774 | 17.6 | 8.95 | 50.8 | 20.6 | 22.2 | 18.1 |
| Hip Shield | 197 | 902 | 795 | 11.27 | 6.35 | 56.4 | 16.1 | 12.4 | 7.3 |
| HipEase | 46 | 433 | 954 | 22.91 | 20.8 | 90.8 | 38.4 | 40 | 30.1 |
| HIPS | 155 | 207 | 795 | 20.03 | 8.62 | 43.1 | 48.3 | 37.1 | 26.6 |
| Hipsaver® | 95 | 877 | 1728 | 11.4 | 9.12 | 80 | 23.6 | 23.5 | 17.6 |
| Hornsby Comfy Hip | 270 | 684 | 776 | 12.24 | 5.39 | 44 | 8.2 | 15.1 | 8.9 |
| Impactwear® – Flexible | 252 | 668 | 962 | 12.23 | 7.07 | 57.8 | −6.4 | 2.5 | 2.4 |
| KPH® | 92 | 276 | 438 | 26.1 | 9.75 | 37.4 | 41.5 | 36.6 | 23 |
| LYDS | 443 | 889 | 1569 | 7.77 | 7.18 | 92.4 | 10.6 | 10.1 | 8.2 |
| Pelican Super Soft | 68 | 742 | 1616 | 14.08 | 13.05 | 92.7 | 33 | 30.2 | 25.3 |
| Pelican Washable | 110 | 497 | 1047 | 15.76 | 10.43 | 66.2 | 20 | 18.9 | 16 |
| Pelican 179P | 92 | 545 | 1196 | 14.97 | 4.52 | 30.2 | 22.5 | 20.2 | 15.6 |
| Posey Heavy Duty | 266 | 477 | 821 | 13.87 | 11.42 | 82.3 | 3.8 | 15.4 | 15 |
| Posey Regular | 116 | 895 | 1806 | 10.4 | 8.69 | 83.6 | 26.2 | 23 | 15.6 |
| ProtectaHip+Plus® | 130 | 429 | 769 | 17.45 | 8.79 | 50.4 | 23.3 | 24.5 | 19.7 |
| ProtectaHip® | 185 | 421 | 752 | 16.14 | 11.22 | 69.5 | 20.7 | 22.5 | 17.5 |
| Safehip® Air-X™ | 156 | 1781 | 3278 | 6.52 | 2.84 | 43.5 | 34 | 26.6 | 18.7 |
| Safehip® Classic | 157 | 1981 | 3421 | 8.12 | 3.49 | 43 | 19.4 | 17.5 | 8.2 |
| Secure | 125 | 536 | 1308 | 14.26 | 11.31 | 79.3 | 24.6 | 21.3 | 15.4 |
| WonderHip™ | 158 | 647 | 1270 | 12.17 | 8.47 | 69.6 | 8 | 12.2 | 7.1 |
Results from univariate regression analyses are summarized in Tables 3 and 4. When all hip protectors were combined (Table 3) the variables that associated significantly with Fneck_atten differed with impact velocity (materialtype, geometrytype, k500, Eabs, and thickwearing at 2 m/s; geometrytype, k500, Eabs, Edis, and thickwearing at 3 m/s; k500, Eabs, Edis, and thickwearing at 4 m/s). As geometrytype was a significant predictor of Fneck_atten in the 2 and 3 m/s conditions, we performed subset analyses at these impact velocities. There were no significant univariate predictors of Fneck_atten for the pads that bridged over the greater trochanter (likely related to the small sample size of 5), so multivariate regression analyses were not performed for this subset of hip protectors. In contrast, for pads that touched the skin overlying greater trochanter (Table 4) there were six common univariate predictors of Fneck_atten in the 2 and 3 m/s datasets (k500, Eabs, width, thickpad, thickwearing, and volume), in addition to Edis for the 3 m/s condition.
Table 3.
Univariate regression summary for the dependent variable Fneck_atten across all hip protectors. Unstandardized regression coefficients, p values, and unadjusted r values are provided.
| Regression coefficient
|
p value
|
Unadjusted r
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2 m/s | 3 m/s | 4 m/s | 2 m/s | 3 m/s | 4 m/s | 2 m/s | 3 m/s | 4 m/s | |
| Materialtype | −14.70 | −8.492 | −3.789 | 0.021* | 0.059 | 0.257 | 0.450 | 0.375 | 0.231 |
| Geometrytype | −15.47 | −9.609 | −4.625 | 0.015* | 0.031* | 0.164 | 0.473 | 0.424 | 0.281 |
| k500 | −0.093 | −0.066 | −0.046 | 0.001* | 0.001* | 0.001* | 0.617 | 0.634 | 0.609 |
| k2000 | −0.003 | −0.006 | −0.005 | 0.620 | 0.180 | 0.095 | 0.102 | 0.271 | 0.334 |
| k3000 | 0.002 | −0.001 | −0.001 | 0.664 | 0.703 | 0.538 | 0.089 | 0.078 | 0.127 |
| Eabs | 1.291 | 1.244 | 0.866 | 0.018* | <0.001* | 0.001* | 0.461 | 0.641 | 0.614 |
| Edis | 0.445 | 0.847 | 0.700 | 0.489 | 0.049* | 0.023* | 0.142 | 0.390 | 0.444 |
| Edis% | −10.88 | −1.027 | 0.889 | 0.358 | 0.901 | 0.882 | 0.188 | 0.026 | 0.031 |
| Height | 0.040 | −0.024 | −0.036 | 0.753 | 0.783 | 0.573 | 0.065 | 0.057 | 0.116 |
| Width | 0.017 | 0.019 | 0.039 | 0.860 | 0.780 | 0.420 | 0.036 | 0.058 | 0.165 |
| Thickpad | 0.258 | 0.405 | 0.408 | 0.616 | 0.250 | 0.105 | 0.103 | 0.234 | 0.326 |
| Thickwearing | 1.243 | 1.036 | 0.633 | 0.011* | 0.001* | 0.010* | 0.492 | 0.592 | 0.498 |
| Volume | <0.001 | <0.001 | <0.001 | 0.414 | 0.255 | 0.118 | 0.167 | 0.231 | 0.314 |
Indicates significant univariate predictors that were used as inputs in the multivariate models that combined all hip protectors.
Table 4.
Univariate regression summary for the dependent variable Fneck_atten for only the subset of hip protectors with a geometrytype that touched the skin overlying the greater trochanter. Unstandardized regression coefficients, p values, and unadjusted r values are provided.
| Regression coefficient
|
p value
|
Unadjusted r
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 2 m/s | 3 m/s | 4 m/s | 2 m/s | 3 m/s | 4 m/s | 2 m/s | 3 m/s | 4 m/s | |
| k500 | −0.082 | −0.059 | NA | 0.001* | 0.001* | NA | 0.676 | 0.670 | NA |
| k2000 | −0.005 | −0.012 | NA | 0.636 | 0.115 | NA | 0.110 | 0.354 | NA |
| k3000 | 0.006 | <0.001 | NA | 0.313 | 0.973 | NA | 0.231 | 0.008 | NA |
| Eabs | 1.307 | 1.493 | NA | 0.073* | 0.002* | NA | 0.399 | 0.635 | NA |
| Edis | 0.628 | 0.972 | NA | 0.303 | 0.018* | NA | 0.236 | 0.509 | NA |
| Edis% | −0.443 | 6.320 | NA | 0.969 | 0.435 | NA | 0.009 | 0.180 | NA |
| Height | 0.044 | −0.033 | NA | 0.733 | 0.718 | NA | 0.079 | 0.084 | NA |
| Width | 0.199 | 0.148 | NA | 0.058* | 0.049* | NA | 0.420 | 0.434 | NA |
| Thickpad | 1.186 | 1.038 | NA | 0.022* | 0.004* | NA | 0.498 | 0.607 | NA |
| Thickwearing | 0.892 | 0.887 | NA | 0.106* | 0.020* | NA | 0.362 | 0.502 | NA |
| Volume | <0.001 | <0.001 | NA | 0.003* | 0.001* | NA | 0.610 | 0.653 | NA |
Indicates significant univariate predictors that were used as inputs in the multivariate models that included hip protectors that touched the skin overlying the greater trochanter (thickwearing at 2 m/s included as it was of borderline significance). Analyses for this subset of hip protectors were not conducted for Fneck_atten at 4 m/s as univariate analyses including all hip protectors (Table 3) found no significant effect of geometrytype at this impact velocity.
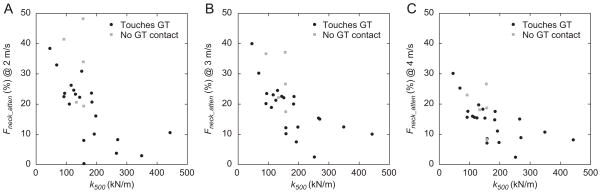
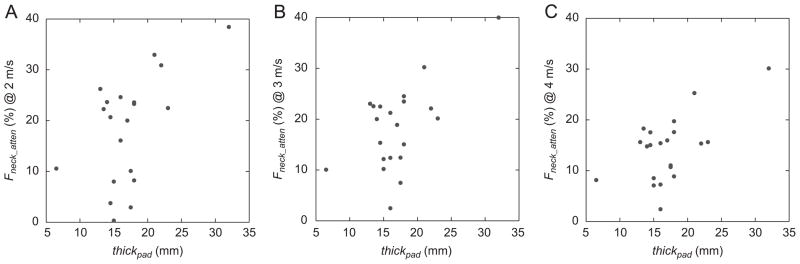
The final predictive models from the multivariate regression analyses are presented in Tables 5 and 6. When all hip protectors were combined (Table 5), lower k500 values (i.e. lower stiffness at 500 N) were associated with greater force attenuation at all impact velocities (Fig. 5). Specifically, a 100 kN/m decrease in k500 was associated with an absolute increase in Fneck_atten of 8.3% at 2 m/s, 4.3% at 3 m/s, and 3.2% at 4 m/s. In addition, hip protectors that absorbed more energy (Eabs) were associated with greater attenuation in femoral neck force (Fneck_atten) in the 3 and 4 m/s conditions. Pads that did not contact the skin overlying the greater trochanter attenuated (on average) 1.9-fold more force at 2 m/s, and 1.5-fold more force at 3 m/s compared to pads that directly covered the greater trochanter.
Table 5.
Multivariate regression summary for the final model predictors of Fneck_atten across all hip protectors. Unstandardized regression coefficients and p values for dependent variables and the overall adjusted r2 for each model are provided.
| Regression coefficient | p value | Adjusted r2 for model | |
|---|---|---|---|
| 2 m/s | |||
| Geometrytype | −12.28 | 0.018 | 0.476 |
| k500 | −0.083 | 0.001 | |
| 3 m/s | |||
| Geometrytype | −6.01 | 0.058 | 0.582 |
| k500 | −0.043 | 0.010 | |
| Eabs | 0.788 | 0.011 | |
| 4 m/s | |||
| k500 | −0.032 | 0.015 | 0.480 |
| Eabs | 0.607 | 0.013 | |
Table 6.
Multivariate regression summary for the final model predictors of Fneck_atten for the subset of hip protectors with a geometrytype that touched the skin overlying the greater trochanter. Unstandardized regression coefficients and p values for dependent variables and the overall adjusted r2 for each model are provided. No information is provided for the subset of hip protectors that did not touch the skin overlying the greater trochanter (N=5) as there were no significant predictors of Fneck_atten for this group.
| Regression coefficient | p value | Adjusted r2 for model | |
|---|---|---|---|
| 2 m/s | |||
| Width | 0.209 | 0.006 | 0.615 |
| Thickpad | 5.63 | 0.001 | |
| Thickwearing | −4.69 | 0.003 | |
| 3 m/s | |||
| Edis | 0.787 | 0.003 | 0.789 |
| Width | 0.179 | <0.001 | |
| Thickpad | 3.09 | <0.001 | |
| Thickwearing | −2.48 | 0.004 | |
Fig. 5.
Scatterplots of Fneck_atten versus k500 broken down by geometrytype (i.e. protectors that do or do not touch the skin overlying the greater trochanter) at the: (A) 2 m/s, (B) 3 m/s, and (C) 4 m/s impact velocity conditions.
The results of the multivariate regression analyses for the subset of protectors that touch the skin overlying the greater trochanter are presented in Table 6. Significant predictors of Fneck_atten included increased width, thickpad, and thickwearing for the 2 m/s data, and Edis, width, thickpad, and thickwearing for the 3 m/s condition.
4. Discussion
In the current study, we used regression analyses to determine whether the force attenuation (biomechanical effectiveness) provided by 26 commercially available hip protectors could be predicted by factors including general design characteristics, geometric parameters or force–deflection properties. We observed a wide range among these devices in biomechanical performance: at an impact velocity of 3 m/s, force attenuation ranged from 2.5% to 40%. We found that hip protectors with lower initial stiffness attenuated greater force at all impact velocities. Protectors that absorbed more energy demonstrated greater force attenuation at the higher impact velocities (3 and 4 m/s conditions), while protectors that did not directly cover (but instead bridged) the skin overlying the greater trochanter attenuated up to 1.9-fold more force in the mild and moderate fall conditions (2 and 3 m/s impact velocities). Subset analyses at these lower velocities demonstrated that force attenuation for protectors that rested against the skin overlying the greater trochanter increased with increasing pad width, thickness, and energy dissipation.
Our results suggest that, among the range of hip protectors we tested, biomechanical effectiveness depends more on the general geometry type than the general material type. For example, force attenuation did not associate with materialtype, with the top four performing protectors consisting of two soft shell designs (HipEase and Pelican Super Soft) and two hard shell products (KPH and HIPS). On the other hand, hip protectors that bridged over the proximal femur were associated with greater force attenuation at low-to-moderate impact velocities, likely due to their enhanced ability to shunt energy away from the proximal femur and into the iliac crest (superiorly) and surrounding soft tissues (anteriorly and posteriorly). These results agree with Kannus et al. (1999) and van Schoor et al. (2006) who also observed superior performance of energy-shunting hip protectors for low and/or moderate energy levels. However, we found that these designs provided no benefit over those that directly covered the proximal femur for higher severity falls (geometrytype dropped out of the final model for the 4 m/s condition), perhaps due to a ‘bottoming-out’ of the protective bridge over/around the proximal femur. These findings agree with Derler et al. (2005) who reported that, while no general advantage was evident for energy-shunting vs. energy-absorbing designs, the three energy-shunting hip protectors they tested were associated with slightly higher femoral neck loads at high impact energies. Additional studies are warranted to assess whether increasing the thickness of these protectors enhances their biomechanical effectiveness at higher impact velocities.
Having said that, we did find that several force–deflection properties (which depend in turn on both material and geometrical properties) associated with the force attenuation provided by hip protectors. For example, protectors with lower stiffness (measured at 500 N of applied load) were associated with increased force attenuation. Low initial stiffness likely influences the pad’s ability to deflect and absorb energy before stiffening or “bottoming out” at higher forces; energy absorption was in turn observed to associate positively with force attenuation. Interestingly, three of the four protectors with the highest Eabs values employed hard shell designs (Table 2). This indicates that hard shell protectors – traditionally considered to confer benefits through energy shunting – provide benefits also through deformation and energy absorption in their stiff dome or shell-like elements during impact from a fall.
We found that pad geometry was an especially important predictor of force attenuation for hip protectors that are in direct contact with the skin overlying the greater trochanter. For this group of 21 hip protectors, regression coefficients indicate that a 1 mm increase in pad thickness (Table 6; Fig. 6) was associated with an absolute Fneck_atten increase of 5.6% for 2 m/s impacts, and of 3.1% for 3 m/s impacts (after adjusting for width, thickwearing, and Edis). Increasing the thickness of protective devices has previously been shown to increase force attenuation during sideways falls on the hip (Laing et al., 2006; Nabhani and Bamford, 2004; Parkkari et al., 1994; Robinovitch et al., 1995), likely due to decreased stiffness and increased energy absorption. The observed effect of anterior–posterior pad width on force attenuation is also logical, as a wider pad allows energy to be shunted further from the proximal femur. Despite these distinct biomechanical benefits, hip protector manufacturers are hesitant in developing products with high thickness and width, which users might perceive as ‘bulky’. Clearly, studies are required in various populations (high risk individuals, care providers, and families) to assess how hip protector geometry affects user acceptance and adherence, and determine whether these design trends are justified.
Fig. 6.
Scatterplots of Fneck_atten versus thickpad at the: (A) 2 m/s, (B) 3 m/s, and (C) 4 m/s impact velocity conditions for the subset of hip protectors that directly touch the skin overlying the greater trochanter.
Our results are important for several reasons. First, they should help to guide consumers in selecting between available devices, based on the biomechanical performance. Second, they should assist researchers in selecting devices for future clinical trials, and interpreting the results of previous trials. Finally, by highlighting the geometric and material parameters that influence biomechanical performance, they should assist manufacturers in designing devices that offer improved performance and clinical effectiveness.
There are notable limitations to the current study. First, our sample of 26 hip protectors reflects the range of devices we were able to secure in 2009. Only five of these were classified as ‘hard shell’, or as protectors that bridged over the greater trochanter, reflecting the popularity of ‘soft shell’ products in the marketplace. Second, we only assessed the biomechanical effectiveness of hip protectors positioned over the hip according to manufacturer instructions. Studies should further explore the effect of pad ‘shifting’ on the biomechanical effectiveness of hip protectors (Choi et al., 2010; Schmitt et al., 2004), and whether the predictive factors of force attenuation observed in the current study remain consistent for protectors that are not optimally positioned. Third, we only assessed the ability of hip protectors to attenuate force during sideways falls causing impact to the lateral aspect of the hip. Although falls may produce a range of impact configurations, we focused on sideways impacts as they are linked most closely to hip fracture (Hayes et al., 1993; Nevitt and Cummings, 1993), and most hip protectors are designed primarily to reduce impact force during lateral impacts. Fourth, as the clinical effectiveness of hip protectors depends on user compliance (Forsen et al., 2004; O’Halloran, 2006; van Schoor et al., 2002), additional research is required to determine how the factors we found to influence biomechanical effectiveness affect user acceptance and adherence. Fifth, the resolution of thickwearing and volume were relatively coarse. Future research could employ 3D scanning systems to better characterize geometric parameters of hip protectors. Sixth, the peak femoral neck force (Fneck) measured during the unpadded condition (a mean of 2698 N for the 4 m/s impact velocity condition) is lower than the 3.5–4.5 kN range included in recent test system recommendations (Robinovitch et al., 2009). However, the theoretical bases for these standards were derived from mathematical predictions of total impact force (incorporating effective pelvis mass, stiffness, and impact velocity), and the peak total impact force measured by the force plate (mean=3880 N) in the current study was within this recommended range. Finally, this paper does not report on the potential influence of pad displacement (i.e. shifting from the manufacturers’ suggested positioning) on the biomechanical effectiveness of each hip protector.
In summary, this study illustrates that there is wide variation in the force attenuation provided by currently marketed hip protectors when positioned correctly over the greater trochanter, and shows that a range of material and geometrical variables affect biomechanical effectiveness. When compared to hip protectors that directly cover the greater trochanter, hip protectors that bridged over the greater trochanter provided 1.5 to 1.9-fold greater force attenuation. Force-attenuation also increased with decreasing stiffness at 500 N, and higher energy absorption. For protectors that directly covered the skin overlying the greater trochanter, force attenuation also increased with increases in pad width and thickness. By comparing the protective value of a large range of existing hip protectors, these results help to guide consumers and researchers in selecting hip protectors, and in interpreting the results of previous clinical trials. Furthermore, by determining geometric and material parameters that influenced biomechanical performance, our results should assist manufacturers in designing devices that offer improved performance and clinical effectiveness.
Supplementary Material
Acknowledgments
This research was funded in part by operating grants from the Natural Sciences and Engineering Research Council of Canada (RGPIN 239735) and the Canadian Institutes of Health Research (TIR-103945). SNR also received support from the Canada Research Chairs program.
Appendix A. Supplementary materials
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jbiomech.2011.08.016.
Footnotes
Conflict of interest
Independent of this project, SNR has received funding from Tytex A/S (the producer of the Safehip line of hip protectors) in support of hip protector research. SNR is also a co-inventor on a patent licensed to Tytex A/S, and forming the basis of the Safehip Soft product tested in this study. In 2006, ACL received funding from Tytex A/S to support travel to a conference. These relationships had no bearing on any aspect of the study design, data analysis or interpretation of results. No person other than the authors had input into the study design and subsequent reporting of data.
References
- Cameron ID, Robinovitch SN, Birge SJ, Kannus P, Khan K, Lauritzen JB, Howland J, Evans S, Minns J, Laing A, Cripton PA, Derler S, Plant DDK. Hip protectors: recommendations for conducting clinical trials—an international consensus statement (part II) Osteoporosis International. 2010;21:1–10. doi: 10.1007/s00198-009-1055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi WJ, Hoffer JA, Robinovitch SN. The effect of positioning on the biomechanical performance of soft shell hip protectors. Journal of Biomechanics. 2010;43:818–825. doi: 10.1016/j.jbiomech.2009.11.023. [DOI] [PubMed] [Google Scholar]
- Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- Cummings SR, Nevitt MC. Non-skeletal determinants of fractures: the potential importance of the mechanics of falls. Study of Osteoporotic Fractures Research Group. Osteoporosis International. 1994;4 (Suppl 1):67–70. doi: 10.1007/BF01623439. [DOI] [PubMed] [Google Scholar]
- Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Breart G. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348:145–149. doi: 10.1016/s0140-6736(96)01440-7. [DOI] [PubMed] [Google Scholar]
- Derler S, Spierings AB, Schmitt KU. Anatomical hip model for the mechanical testing of hip protectors. Medical Engineering & Physics. 2005;27:475–485. doi: 10.1016/j.medengphy.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Feldman F, Robinovitch SN. Reducing hip fracture risk during sideways falls: evidence in young adults of the protective effects of impact to the hands and stepping. Journal of Biomechanics. 2007;40:2612–2618. doi: 10.1016/j.jbiomech.2007.01.019. [DOI] [PubMed] [Google Scholar]
- Forsen L, Sandvig S, Schuller A, Sogaard AJ. Compliance with external hip protectors in nursing homes in Norway. Injury Prevention. 2004;10:344–349. doi: 10.1136/ip.2004.005124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcified Tissue International. 1993;52:192–198. doi: 10.1007/BF00298717. [DOI] [PubMed] [Google Scholar]
- Kannus P, Parkkari J, Niemi S, Pasanen M, Palvanen M, Jarvinen M, Vuori I. Prevention of hip fracture in elderly people with use of a hip protector. New England Journal of Medicine. 2000;343:1506–1513. doi: 10.1056/NEJM200011233432101. [DOI] [PubMed] [Google Scholar]
- Kannus P, Parkkari J, Poutala J. Comparison of force attenuation properties of four different hip protectors under simulated falling conditions in the elderly: an in vitro biomechanical study. Bone. 1999;25:229–235. doi: 10.1016/s8756-3282(99)00154-4. [DOI] [PubMed] [Google Scholar]
- Laing AC, Robinovitch SN. Effect of soft shell hip protectors on pressure distribution to the hip during sideways falls. Osteoporosis International. 2008a;19:1067–1075. doi: 10.1007/s00198-008-0571-9. [DOI] [PubMed] [Google Scholar]
- Laing AC, Robinovitch SN. The force attenuation provided by hip protectors depends on impact velocity, pelvic size, and soft tissue stiffness. Journal of Biomechanical Engineering. 2008b;130:061005–061009. doi: 10.1115/1.2979867. [DOI] [PubMed] [Google Scholar]
- Laing AC, Robinovitch SN. Low stiffness floors can attenuate fall-related femoral impact forces by up to 50% without substantially impairing balance in older women. Accident Analysis & Prevention. 2009;41:642–650. doi: 10.1016/j.aap.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Laing AC, Robinovitch SN. Characterizing the effective stiffness of the pelvis during sideways falls on the hip. Journal of Biomechanics. 2010;43:1898–1904. doi: 10.1016/j.jbiomech.2010.03.025. [DOI] [PubMed] [Google Scholar]
- Laing AC, Tootoonchi I, Hulme PA, Robinovitch SN. Effect of compliant flooring on impact force during falls on the hip. Journal of Orthopaedic Research. 2006;24:1405–1411. doi: 10.1002/jor.20172. [DOI] [PubMed] [Google Scholar]
- Lauritzen JB, Petersen MM, Lund B. Effect of external hip protectors on hip fractures. Lancet. 1993;341:11–13. doi: 10.1016/0140-6736(93)92480-h. [DOI] [PubMed] [Google Scholar]
- Mills NJ. The biomechanics of hip protectors. Proceedings of the Institution of Mechanical Engineers. Part H, Journal of Engineering in Medicine. 1996;210:259–266. doi: 10.1243/PIME_PROC_1996_210_422_02. [DOI] [PubMed] [Google Scholar]
- Nabhani F, Bamford J. Impact properties of floor coverings and their role during simulated hip fractures. Journal of Materials Processing Technology. 2004;153–154:139–144. [Google Scholar]
- Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The Study of Osteoporotic Fractures Research Group. Journal of the American Geriatrics Society. 1993;41:1226–1234. doi: 10.1111/j.1532-5415.1993.tb07307.x. [DOI] [PubMed] [Google Scholar]
- O’Halloran PD. Effectiveness of hip protectors: it’s more the effectiveness of compliance strategies. BMJ. 2006;332:729. doi: 10.1136/bmj.332.7543.729-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkkari J, Kannus P, Poutala J, Vuori I. Force attenuation properties of various trochanteric padding materials under typical falling conditions of the elderly. Journal of Bone and Mineral Research. 1994;9:1391–1396. doi: 10.1002/jbmr.5650090910. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Evans SL, Minns J, Laing AC, Kannus P, Cripton PA, Derler S, Birge SJ, Plant D, Cameron ID, Kiel SP, Howland J, Khan K, Lauritzen JB. Hip protectors: recommendations for biomechanical testing—an international consensus statement (part I) Osteoporosis International. 2009;20:1977–1988. doi: 10.1007/s00198-009-1045-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinovitch SN, Hayes WC, McMahon TA. Energy-shunting hip padding system attenuates femoral impact force in a simulated fall. Journal of Biomechanical Engineering. 1995;117:409–413. doi: 10.1115/1.2794200. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Hayes WC, McMahon TA. Distribution of contact force during impact to the hip. Annals of Biomedical Engineering. 1997;25:499–508. doi: 10.1007/BF02684190. [DOI] [PubMed] [Google Scholar]
- Schmitt KU, Spierings AB, Derler S. A finite element approach and experiments to assess the effectiveness of hip protectors. Technology and Health Care. 2004;12:43–49. [PubMed] [Google Scholar]
- Taylor BC, Schreiner PJ, Stone KL, Fink HA, Cummings SR, Nevitt MC, Bowman PJ, Ensrud KE. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. Journal of the American Geriatrics Society. 2004;52:1479–1486. doi: 10.1111/j.1532-5415.2004.52410.x. [DOI] [PubMed] [Google Scholar]
- van Schoor NM, Deville WL, Bouter LM, Lips P. Acceptance and compliance with external hip protectors: a systematic review of the literature. Osteoporosis International. 2002;13:917–924. doi: 10.1007/s001980200128. [DOI] [PubMed] [Google Scholar]
- van Schoor NM, van der Veen AJ, Schaap LA, Smit TH, Lips P. Biomechanical comparison of hard and soft hip protectors, and the influence of soft tissue. Bone. 2006;39:401–407. doi: 10.1016/j.bone.2006.01.156. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.