Abstract
Background/Objective
To assess the traditional postpartum practices, mother and child nutritional status and associated factors.
Subjects/Methods
A cross-sectional study in 41 randomly selected villages on the outskirts of Vientiane capital city, Lao PDR (Laos). 300 pairs of infants (<6 months of age) and their mothers were enrolled. Information was collected about pregnancy, delivery and traditional practices through a standardized questionnaire. Dietary intake and food frequency were estimated using the 24 h recall method, calibrated bowls and FAO food composition tables. Mothers’ and infants’ anthropometry was assessed and multivariate analysis performed.
Results
Contrasting with a high antenatal care attendance (91%) and delivery under health professional supervision (72%), a high prevalence of traditional practices was found, including exposure to hot beds of embers (97%), use of traditional herb tea as the only beverage (95%) and restricted diets (90%). Twenty-five mothers (8.3%) were underweight. Mothers had insufficient intake of calories (55.6%), lipids (67.4%), iron (92.0%), vitamins A (99.3%) and C (45%), thiamin (96.6%) and calcium (96.6%). Chewed glutinous rice was given to infants as an early (mean 34.6, 95% CI:29.3–39.8 days) complementary food by 53.7% of mothers, and was associated with stunting in 10% children (OR = 1.35, 95% CI:1.04–1.75).
Conclusion
The high prevalence of traditional postpartum restricted diets and practices, and inadequate maternal nutritional intake in urban Laos, suggest that antenatal care may be an important opportunity to improve postpartum diets.
Keywords: food taboo, Lao PDR, mother, beliefs, children, infant
Introduction
The Lao PDR (Laos) is a landlocked country in Southeast Asia, with a multi-ethnic, low-density (24 per km2) population of 5.6 million. It has one of the lowest per capita incomes (US$390) in Asia and is ranked 135th globally according to the Human Development Index (United Nations Development Program, 2006). The Lao National Health Survey documented a high prevalence of stunting (41%) and wasting (15%) among children (0–5years) (Ministry of Health, 2001).
Steamed glutinous rice (‘sticky’ rice) is the staple food in Laos and is complemented mainly by small portions of vegetables and fish. Glutinous rice differs from other rice varieties in that it has a high content of amylose (Gerhold, 1967). Traditional Lao rice processing and cooking may destroy water-soluble vitamins. Sticky rice is washed 3–4 times and then soaked in an excess of water for several hours. The excess water is poured off and the rice steamed until the kernels adhere to each other. The estimated daily dietary energy supply per capita was 2315 kcal in 2003 with rice providing 68 and 64% of the energy and protein supply, respectively (Kaufmann et al., 2003).
In Asia, postpartum maternal food restrictions (‘food avoidances’) are common practices, which may have important health consequences in reducing the nutritional content of breast milk. In Laos, 5% of the children are never breastfed, 28% have exclusive breastfeeding at 3 months and 75% are weaned before 24 months (Ministry of Health, 2001). Inadequate breastfeeding and weaning practices contribute to high rates of malnutrition and infant and child mortality (Kaufmann et al., 2003). Glutinous rice is a frequent first food supplement and is given pre-chewed by mothers to 20–48% of infants in the first week of life (Kaufmann et al., 2003). These traditional nutritional habits are embedded in wider postpartum practices, such as the ‘hot bed’, in which mothers lie on a bed with hot charcoal laid beneath for 3–4 weeks after delivery.
Traditional practices may have important health implications for both mother and infant. Early complementary food may reduce or terminate their breast-milk intake (Drewett et al., 1993; WHO, 1998), may be a source of microbial contamination and interfere in the absorption of essential micronutrients such as iron and zinc (Giugliani and Victora, 2000). Beriberi, or clinical thiamin (vitamin B1) deficiency, has been associated with low diet diversity and consumption of glutinous rice (Soukaloun et al., 2003). The development of bladder stones in early childhood is associated with a dietary carbohydrate-protein imbalance, observed in Lao children who have early glutinous rice supplementation (Sayasone et al., 2004).
As there are no data available on the dietary intake of lactating Lao mothers we carried out a cross-sectional study to assess postpartum traditional practices, to describe the qualitative and quantitative aspects of mothers’ diet, and to identify factors associated with impaired mother and child nutritional status.
Population, materials and methods
Study setting
Vientiane, the country’s capital, has 698 000 inhabitants. Despite recent increasing urbanization, Vientiane preserves rural characteristics such as rice fields and fishponds within the city.
Sampling procedure
From a list of all villages on the outskirts of the capital, defined as 15–25 km from the city centre, a random sample of 41 villages (see sample size below) was drawn using a random number table. All mothers with a child aged less than 180 days and who gave informed oral consent were recruited in March–April 2005.
Mothers’ questionnaire
A structured questionnaire of 45 items, concerning household economic status, morbidity and dietary intake, was used to interview the mothers by a Lao investigator (SC) in the Lao language. Once a 24 h diet recall was performed to report maternal daily food consumption and their children’s daily food frequency (Marr, 1971). Quantities of food items consumed were measured on site using local bowls and cooking tools calibrated with a scale (±5 g). Vegetable weight was estimated using pre-calculated weights based on the size and number of leaves or pieces during a pilot study in three villages. Dietary intakes were estimated for protein, lipids, energy (calories) and vitamins using FAO food composition tables for Asia (FAO, 1972) and compared with daily dietary allowances for lactating women (Latham, 1997). Intakes were considered insufficient as follows: energy<2710 cal J−1, protein<69 g, lipid <45 g, iron<26 mg, calcium<1000 mg, thiamin<1.1 mg, retinol<850 mg, vitamin C<30 mg (Latham, 1997). Excessive intake was defined for energy >3500 kcal J−1 and protein >120 g J−1.
Anthropometry
Mother’s height was measured using wooden measuring boards with 0.1 cm precision (United Nations, 1986). Child’s length was measured in the supine position. Participants were weighed lightly clothed using an infant scale (precision ±10 g) or an electronic SECA scale for adults (precision ±100 g).
Sample size estimation, definitions and analysis
We calculated a necessary sample size of 300 mother–infant pairs on the basis of 78% of mothers observing food avoidance (α = 0.05, β = 0.9) (Ministry of Health, 2001).
Mothers reporting restricted postpartum diet were classified as the ‘restricted diet’ group (RD), and those reporting no restriction as the ‘nonrestricted diet’ group (NRD).
Epinut (Epi Info 6.04d) was used to calculate height for age (stunting), weight for age (underweight) and weight for height (wasting) z-scores for each child. A child was considered malnourished if the z-score was ≤2 s.d. Body mass index (BMI) was calculated for mothers, who were considered underweight or malnourished if BMI was ≤18.5 or ≤17 kg m −2, respectively, and overweight if BMI >27.5 kg m−2 (WHO expert consultation, 2004).
Analysis was carried out by STATA, versions 8 (Stata Corporation, College Station, TX, USA). χ2 and Fisher’s exact tests were used for categorical variables, Student’s t-test and analysis of variance (F-test) for normally distributed continuous data. We carried out a multivariate analysis of the socioeconomic factors associated with the antenatal care (ANC), the place of delivery (home or hospital), observance of postpartum practices and malnutrition among mothers. We considered P<0.05 as statistically significant.
Ethical approval was obtained from the Medical Council of the Lao Ministry of Health.
Results
Demographic and socioeconomic characteristics of the women
No women declined consent to the study and 300 mothers were interviewed 3.0 (95% CI: 2.7–3.2) months after delivery with 32 (10.6%) mothers interviewed during the first fortnight (Table 1). Husbands were mainly farmers or labourers (76%). Drinking water was either purified bottled water (35%) or from wells (64%). Families had very low income (≤40 US$ per month; 43%) and low income (≤100US$ per month; 45%).
Table 1.
Characteristics of all mothers interviewed and those observing and not observing dietary restrictions
| Dietary restriction (n = 274) | No dietary restriction (n = 26) | P | Total (n = 300) | |
|---|---|---|---|---|
| General | ||||
| Age (years)a | 25.1 (24.4–25.8) | 27.3 (25.1–29.5) | 0.04 | 25.3 (24.7–25.9) |
| Weight (kg)a | 51.4 (50.6–52.2) | 51.3 (47.6–54.9) | ns | 51.4 (50.6–52.2) |
| Parity (number of children)a | 1.8 (1.7–1.9)a | 2.0 (1.7–2.3) | ns | 1.8 (1.7–1.9) |
| Distance to Vientiane centre (km)a | 23.0 (22.1–23.9) | 21.3 (18.9–23.6) | ns | 22.8 (22.0–23.6) |
| No latrine useb | 44 (15.9) | 8 (30.7) | 0.05 | 52 (17.3) |
| Completed primary schoolb | 87 (31.7) | 9 (34.6) | ns | 96 (32.0) |
| No formal professionb | 122 (44.5) | 11 (44.3) | ns | 133 (44.3) |
| Own their housec | 266 (97.0) | 25 (96.1) | ns | 291 (97.0) |
| Nutritional status | ||||
| BMI (kg mr−2) (mean)a | 22.2 (22.1–22.2) | 21.5 (21.3–21.7) | ns | 22.1 (21.8–22.4) |
| BMI≤18.5 kg mT−2 (underweight)b | 21 (7.6)d | 4 (15.3) | ns | 25 (8.3) |
| BMI≤17 kg mT−2 (malnutrition)b | 6 (2.1)e | 2 (7.6) | ns | 8 (2.6) |
| BMI≥27.5kgmT−2 (obesity)b,f | 17 (6.2)g | 0 | ns | 17 (6.2) |
| Antenatal and delivery practices | ||||
| ANCb | 250 (91.2) | 24 (92.3) | ns | 274 (91.3) |
| Number of ANC visitsa | 2.7 (2.6–2.7) | 2.6 (2.4–2.8) | ns | 2.7 (2.6–2.8)a |
| No tetanus immunizationb | 19 (6.9) | 2 (7.6) | ns | 21 (7) |
| Delivery at hospitalb | 190 (69.3)h | 26 (100.0)i | <0.001 | 216 (72.0) |
| Caesareanb | 10 (3.6)b | 5 (19.3) | <0.005 | 15 (5.0) |
| Postpartum practices | ||||
| Hot bed exposureb | 270 (98.5) | 22 (84.6) | 0.002 | 292 (97.3) |
| Duration of hot beda exposure (days) | 14.1 (14.0–14.1) | 13.3 (12.9–13.6) | < 0.001 | 14.0 (13.4–14.6) |
Abbreviations: ANC, antenatal care; BMI, body mass index; ns, not significant.
Mean (95% confidence interval (CI)).
Number (%).
Houses made of bamboo (21%), wood (27%) or concrete (53%).
Mean: (95% CI) 17.2 (17.1–17.3).
Mean (95% CI): 16.4 (16.3–16.5).
For Asian women according to WHO, 2004.
Mean (95% CI): 29.2 (29.0–29.4).
152 at the Central hospital, 37 at the District hospital, 1 at the Health centre.
24 at the Central hospital, 2 at the District hospital.
Mother’s nutrition status
Five factors were associated with maternal underweight (BMI <18.5 kg m −2), which was found in 25 (8.3%) mothers (Tables 1 and 2). Multiparity and having her own house were protective factors, while no access to health care, no or basic employment and long time interval after delivery were related with malnutrition (Table 2).
Table 2.
Factors associated with mother nutritional status, antenatal care (ANC), hospital delivery and traditional practices
| OR | 95% CI | P | |
|---|---|---|---|
| No malnutrition (BMI≥18.5 kg m−2) | |||
| Multiparity | 5.0 | 1.7–14.4 | <0.05 |
| Owning her house | 9.9 | 1.8–52.4 | <0.05 |
| No ANC | 0.1 | 0.03–0.5 | <0.001 |
| Time after delivery > 3months | 0.3 | 0.1–0.9 | <0.05 |
| Being jobless or having only farming/ | 0.3 | 0.1–0.9 | <0.05 |
| gardening activities | |||
| No ANC | |||
| > Primary school | 0.1 | 0.05–0.39 | < 0.001 |
| Multiparity (> 1 child) | 5.1 | 1.6–15.7 | 0.004 |
| Delivery at hospitala | |||
| Husband not a farmer | 4.1 | 1.6–10.2 | 0.002 |
| Owns her own house | 2.3 | 1.2–4.3 | 0.010 |
| More than 2 antenatal visits | 4.5 | 1.4–13.8 | 0.008 |
| No antenatal visit | 0.2 | 0.08–0.5 | 0.001 |
| More than 1 child | 0.5 | 0.2–0.9 | 0.020 |
| Exposure to ‘hot bed’ | |||
| Delivery at the hospital | >280 | <0.000 | |
| More than 14 days ‘hot bed’ | |||
| Education beyond primary school | 2.2 | 1.2–4.0 | 0.007 |
| Owns her own house | 2.1 | 1.0–4.3 | 0.03 |
| > 40US$ monthly income | 1.9 | 1.1–3.4 | 0.01 |
| Multiparity (> 1 child) | 0.1 | 0.07–0.2 | <0.000 |
| Ceasarean sectionb | 0.5 | 0.2–0.8 | 0.01 |
| Restricted diet | |||
| Multiparity (> 1 child) | 0.2 | 0.1–0.6 | 0.006 |
| Delivery at the hospital | 0.2 | 0.06–0.7 | 0.01 |
| Exposure to ‘hot bed’ | 14.8 | 3.0–71.5 | 0.001 |
Abbreviations: ANC, antenatal care; BMI, body mass index; CI, confidence interval; OR, odd ratio.
Average hospital stay: 3 days.
Mean (95% CI) exposure: 9.4 (4.5–14.2) days versus 14.1 (13.4–14.7) days (P<0.03) in mother who had and had not Cesarean section, respectively.
Antenatal care and pregnancy
Ninety-one percent of mothers made at least one ANC visit (Table 1). Twenty-eight percent of women delivered without medical supervision, with the help of a family member (44, 14.6%) or a traditional birth attendant (40, 13.3%). Women delivering in hospital, where some health education and immunization are provided, were more common in the NRD group (P<0.001). Women more commonly had their first childbirth in hospital than their subsequent deliveries (53.7 vs 46.3%, P = 0.001). Almost all women (97%) lay on ‘hot beds’ of embers for a mean of 14.0 (95% CI: 13.3–14.6) days.
Education, parity and socioeconomic factors were related to higher ANC and hospital delivery (Table 2).
Postpartum practices
After delivery 274 (93%) women reported a restricted diet (‘phit kam’).
Dietary avoidances were described by 271 women (Table 3), and were strict especially in the first postpartum fortnight. Vegetables and fruits were rarely eaten.
Table 3.
Mothers diet during different postpartum periods
| Day 1–Day 14 (n = 271) | n (%) |
|---|---|
| Rice with dry meat or fish only | 97 (35.7) |
| Glutinous rice with salt only | 42 (15.5) |
| Glutinous rice with salt during 3 days, | 132 (48.7) |
| then rice with dry meat or fish | 72 (26.5) |
| + fruits (oranges) | 19 (7.0) |
| + cooked vegetables | 26 (9.5) |
| + meat or fish soup + fruit | 15 (5.5) |
| + vegetables | 0 |
| Day 15–Day 30 (n = 234) rice with dry meat or fish | 87 (37.1) |
| +cooked vegetables | 34 (14.5) |
| + meat or fish soup and fruit | 24 (10.2) |
| + meat or fish soup, vegetables and fruit | 89 (38.0) |
| Day 30–Day 90 (n = 116) | |
| Standard Lao adult meal | 41 (35.3) |
| without spices and fermented meal | 36 (31.0) |
| without animal with 'white' skina | 39 (33.6) |
| Only home productb,c | 91 (78.4) |
beef, pork, chicken.
Produced by the family with no food bought from the market and always cooked (preferably grilled).
After 90 days 38.8% women still restricted their food to home product.
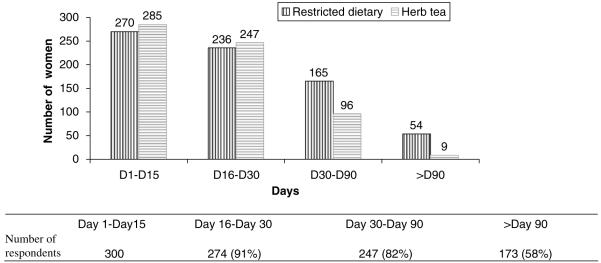
During the first months, mothers did not eat popular Lao foods, such as raw or fermented vegetables, fruits, meat ‘lap-mou’ (pork meat chopped with vegetable), ‘sommou’ (fermented pork meat with vegetable) or ‘pad-dek’ (fermented fish sauce), ‘white’ skinned mammals, liquid meals and sauces, sugar and spices. Most women (81.7%) returned to an unrestricted diet by the third month postpartum (Figure 1).
Figure 1.
Mothers’ restricted diet and traditional herb tea use after delivery (n = 300).
By the third month, 33% of mothers only ate home-produced food. Three mothers did not eat vegetables from their garden, as they were afraid of the consequences of pesticides.
285 (95%) women drank only traditional unsweetened herb tea in the first 15 days postpartum (Figure 1). Herb tea was considered to be beneficial for lactation (201, 70%), healing of tissue injuries caused by delivery (191, 67%) and for prevention of cardiac failure (84, 29%).
Daily nutritional intake of mothers
Assessment of the daily nutritional intakes of mothers showed that all but two ate rice, mostly glutinous (87.3%). (Tables 4-6). Diet in the previous day consisted of rice associated with meat (85.3%), fish (60.0%) or both (47.6%), with fruits (n = 151, 50.3%) or vegetables (n = 163, 54.3%) or roots (n = 66, 22.2%).
Table 4.
Breastfeeding mother (n = 300) meal composition (24 h recall)
| Type of food | Restricted diet (n = 274 (%)) | No Restricted Diet (n = 26 (%)) | P | Total (n = 300 (%)) | Intakea(g) |
|---|---|---|---|---|---|
| Glutinous riceb | 236 (86.1) | 26 (100) | 0.05 | 262 (87.3) | 525 |
| Non-glutinous rice | 50 (18.2) | 3 (11.5) | ns | 53 (17.6) | 664 |
| Meat | 232 (84.6) | 24 (92.3) | ns | 256 (85.3) | 15.3 |
| Fish | 159 (58.0) | 21 (80.2) | 0.03 | 180 (60.0) | 6.6 |
| Egg | 20 (7.3) | 2 (7.6) | ns | 22 (7.3) | 93.6 |
| Vegetable | 148 (54.0) | 15 (55.9) | ns | 163 (54.3) | 141 |
| Roots/leaves | 61 (22.2) | 5 (19.2) | ns | 66 (22.0) | 86 |
| Fruit | 134 (48.9) | 17 (65.3) | ns | 151 (50.3) | 227 |
| Sweet drinksc,d | 48 (17.5) | 7 (26.9) | ns | 55 (18.3) | 299 |
| Soups | 63 (22.9) | 5 (19.2) | ns | 68 (22.6) | 146 |
| Pastry | 11 (4.0) | 4 (15.3) | 0.03 | 15 (5.0) | 44 |
Abbreviation: ns, not significant.
All but five mothers were breastfeeding their child at the time of the survey.
Mean intake among the people who ate the food.
Number and (%).
Sugar cane, soya milk, chocolate, Pepsi or coffee with sugar.
Only four mothers (1.3%) drank milk.
Table 6.
Estimated daily nutritional intake of 274 "reastfeeding mothers in the restricted diet group during and after 15 days postpartum
| Daily nutritional intake | Days 1–Days 15 (n = 31) | After Day 15 (n = 243) | P |
|---|---|---|---|
| Energy (kcal per day)a | 2850 (2430–3269) | 2699 (2593–2804) | ns |
| Protein intakea (g per day) | 61 (49–72) | 108 (103–112) | < 0.0001 |
| Lipid (g per day)a | 17 (10–23) | 31 (24–31) | ns |
| Thiamina (mg) | 0.4 (0.1–0.7) | 0.9 (0.8–0.9) | < 0.0001 |
| Vitamin C (mg)a | 26 (9–42) | 56 (48–63) | = 0.004 |
| Retinol (mg)a | 20 (3–36) | 103 (82–123) | = 0.006 |
| Iron (mg)a | 9 (7–10) | 15 (14–15) | < 0.001 |
| Calcium (mg)a | 311 (188–433) | 456 (411–500) | 0.03 |
Abbreviation: ns, not significant.
Daily recommended intake for "reastfeeding women: energy, 2710 kcal; protein, 69 g J−1; lipid, 45 g; thiamin, 1.1 mg; vitamin C, 30 mg; retinol, 850 μg; iron, 26 mg; calcium, 1000mg (Latham, 1997).
Mean (95% confidence interval).
Half of the mothers reported eating fruits or vegetables, with 94 (31.3%) eating both, while 80 (26.6%) eating neither. Mean daily consumption of meat (15.3 g) and fish (6.6 g) was moderate. Sweet drinks were taken infrequently and accounted for <2% of carbohydrates.
The estimated nutritional values of the preceding day’s food did not differ between the NRD/RD groups (Table 5). Carbohydrates constituted the greatest portion of the diet (median 85.7% (69–96)). Half of the mothers were estimated to have consumed sufficient carbohydrates and proteins but only one third consumed sufficient lipids and micronutrients.
Table 5.
Daily nutritional intake of mothers according to dietary practices after postpartum
| Daily nutritional intake | Restricted diet (n = 274 (%)) | No restricted diet (n = 26 (%)) | P | Total (n = 300(%)) |
|---|---|---|---|---|
| Mean energy per day (kcal per day) a | 2716 (874) | 2526 (948) | ns | 2700 (880) |
| Insufficient <2710b | 151 (55.1) | 16 (61.5) | ns | 167 (55.6) |
| Sufficientb2710−3499 | 72 (26.2) | 6 (23.0) | ns | 78 (26.0) |
| Excessiveb > 3500 | 51 (18.6) | 4 (15.3) | ns | 55 (18.3) |
| Carbohydrate a,c (kcal per day) | 2314 (904) | 2151 (904) | ns | 2300 (845) |
| Protein intake a(g per day) | 102 (40) | 99 (35) | ns | 102 (39) |
| Insufficientb < 69 | 49 (17.8) | 3 (11.5) | ns | 52 (17.3) |
| Sufficientb 69−119 | 148 (54.1) | 19 (73.0) | ns | 167 (55.6) |
| Excessive b> 119 | 77 (28.1) | 4 (15.3) | ns | 81 (27.0) |
| Lipid (g per day) a,d | 30 (47) | 28 (20) | ns | 30 (45) |
| Insufficientb < 45 | 148 (65.8) | 19 (82.6) | ns | 167 (67.4) |
| Thiamina (mg) | 0.8 (0.5) | 0.8 (0.4) | ns | 0.8(0.5) |
| Insufficientb <1.1 | 264 (93.3) | 26 (100) | ns | 290 (96.6) |
| Vitamin C (mg)a | 53(55) | 67(66) | ns | 54 (57) |
| Insufficientb < 30 | 125 (45.6) | 10 (38.4) | ns | 135 (45.0) |
| Retinol (mg) a | 93 (159) | 66 (91) | ns | 91 (154) |
| Insufficientb <850 | 272 (99.2) | 26 (100) | ns | 298 (99.3) |
| Iron (mg) a | 14(6) | 12(5) | ns | 14.2 (6) |
| Insufficientb < 26 | 251 (91.6) | 25 (96.1) | ns | 276 (92) |
| Calcium (mg) a | 439 (363) | 405 (288) | ns | 436 (257) |
| Insufficientb <1000 | 262 (95.6) | 25 (96.1) | ns | 287 (96.6) |
Abbreviation: ns, not significant.
Daily recommended intake for ±reastfeeding women in developing countries considered as ‘safe levels of intake’: energy: 2710 kcal, protein: 69 g, lipid: 45 g, thiamin: 1.1 mg, vitamin C: 30 mg, retinol: 850 μg, iron: 26 mg, calcium: 1000 mg (Latham, 1997)Glutinous rice was the main source for energy (76.8%) and protein.
Mean±s.d.
Number of people and (%).
Part of CHO in total energy 84 and 83%, respectively; recommended part of CHO in total energy: 55% (FAO, 1998).
Part of lipid in energy intake 9.9% in both groups; recommended fat in energy intake <30% (FAO, 1998).
Daily nutritional intake of RD mothers during and after the first fortnight
In the RD group mothers had significantly lower protein and micronutrient intake during, in comparison to after, the first fortnight (Table 6). Protein and micronutrient intakes were below the FAO requirements.
Children nutritional status and feeding practices
Thirty infants (10%) had severe stunting and 9 (3%) had acute malnutrition (Table 7). The stunted children were older than the nonstunted ones (128.7 (95% CI: 112.8–144.6) days vs 87.8 (95% CI: 81.0–94.5) days; P<0.001). Stunting was associated with early rice supplementation (OR = 1.35, 95% CI: 1.04–1.75) and not with the mother’s diet. Before being breastfed, 81 (27%) children received either water or formula milk. Colostrum was given by 276 (92.5%) mothers but mean time to first breastfeeding was given at 14.6 (11.2–18.0) h.
Table 7.
Characteristics of breastfed infants (<180 days) for all mothers interviewed and those observing and not observing dietary restrictions
| Dietary restrictions (n = 274) | No dietary restrictions (n = 26) | P | Total (n = 300) | |
|---|---|---|---|---|
| General | ||||
| Age (months) | 3.0 (2.8–3.2) | 2.9 (2.3–3.4) | ns | 3.3 (3.1–3.5) |
| Female (%) | 146 (53.8) | 15 (51.7) | ns | 161 (53.6) |
| Nutritional status | ||||
| Stunting (HAZ <−2s.d.) | 27 (9.9) | 3 (10.3) | ns | 30 (10) |
| Underweight (WAZ<−2s.d.)a | 9(3.3) | 0 | ns | 9 (3.0) |
| Wasting (WHZ <−2s.d.) | 27 (9.9) | 3 (10.3) | ns | 30 (10) |
| Nutritional practices | ||||
| Colostrum given to infant | 248 (92.1) | 25 (96.1) | ns | 273 (92.5) |
| Time of first breastfeeding (h) | 14.1 (10.9–17.3) | 20.5 (0–42.9) | ns | 14.6 (11.2–18.0) |
| Early food supplementation | 148 (54.0) | 13 (50.0) | ns | 161 (53.7) |
| Time to early food supplement (days) | 35.2 (29.7–40.7) | 29.0 (11.8–46.2) | ns | 34.6 (29.4–39.8) |
| Diet the day before | ||||
| Breastfedb | 269 (98.1) | 26 (100) | ns | 295 (98.4) |
| Rice | 80 (56.2) | 7 (63.5) | ns | 87 (66.8) |
| Rice and fruits | 44 (30.9) | 4 (36.2) | ns | 46 (31.1) |
| Rice soup with vegetable | 13 (9.1) | 0 | ns | 13 (8.5) |
| Fruits | 5 (3.5) | 0 | ns | 5 (3.2) |
Abbreviation: ns, not significant.
Mean (95% confidence intervals) and number (%) for continuous and discrete characteristics, respectively.
P = 0.09.
All but 5 (1.6%) children were still breastfed and 29 (9.6%) were on mixed feeding.
A total of 161 (53.7%) infants received an early food supplement in the form of chewed glutinous rice (77, 25.6%), formula milk (66, 22%) or rice soup with carrots (16, 5.3%). The day before maternal interview, 133 (43.3%) infants received rice (chewed, mixed, as flour) and 64 (21.3) received fruits or vegetables alone or with rice.
Discussion
This study estimates the occurrence and nutritional values of restrictive diets included in a set of postpartum traditional practices among urban Lao women. Restricted diet and postpartum practices are common and similar to those reported nationwide (Ministry of Health, 2001) and to reports from neighbouring north-eastern Thailand (Saowakontha et al., 1995). The first breast meal is still delayed for 14.6 h. The generalized use of colostrum (92.5%) is a notable change from Lao traditional postpartum practices in which colostrum, considered impure because of its colour, is discarded and the first breast meal may be delayed for 2–3 days (FAO and IUCN, 2003). On the outskirts of the capital, recent urbanization and transitional changes in economic status have only moderately affected the persistent high frequency of traditional delivery and postpartum practices. Therefore, efforts are required to inform pregnant women on benefits and risks of traditional practices.
Perception on postpartum practices
Most women observed ‘hot bed’ practices. Noncompliance is regarded as having negative consequences on both maternal and child health (Pottier, 1978). Maternal or infantile death, poor lactation and diseases, such as diarrhoea, are listed among the consequences. Mothers explained that ‘hot bed’ helps to dry up and heal the vagina and uterus, and to relax muscles and decrease pain. Surprisingly, women with higher education stayed longer on ‘hot beds’ than illiterate women. They reported that the ‘hot bed’ was an opportunity to rest, to stay away from daily chores and to strengthen social relations. In addition, reduced physical activity associated with bed rest may compensate for the low daily calorie intake (FAO/WHO, 1998).
Most mothers restricted their diet. Women explained their compliance with traditional food practices in a similar way to the ‘hot bed’ in that not complying would negatively influence the health of the newborn. Grilled food (without fruits and vegetables) is believed to prevent cardiac failure (n = 123, 41%) and to heal internal organ injuries (n = 101, 37%). Eating ‘white’ skinned animals would lead to weakness. These traditions are deeply rooted (Pottier, 1978), and vary according to ethnic group and location (Kaufmann et al., 2001).
Foods avoidances and potential nutritional deficiencies
Food avoidance during pregnancy and after delivery is common in other traditional cultures, and may substantially affect daily intakes of energy, protein and basic nutrients, notably micronutrients (Trigo et al., 1989; Santos-Torres and Vasquez-Garibay, 2003). They may precipitate maternal micronutrient deficiencies (Kachondham and Dhanamitta, 1992). The 31 mothers (10.6%) in the RD group who were interviewed during the first fortnight after delivery consumed an excess of calories with insufficient protein, fat and micronutrients. Three months postpartum, most women had an adequate macronutrient intake, except for lipids. However, the mothers had an inadequate intake of micronutrients, due to the general restriction of vegetables, fruits and meat. Thiamin deficient intake was common both during and after the restricted diet period. Hence, it is likely that thiamin, vitamin A and vitamin C are deficient in breast milk (Latham, 1997), but this needs to be formally assessed. Thiamin deficient intake is of public health concern in Laos, because infantile beriberi is prevalent, at least in Vientiane (Soukaloun et al., 2003).
Mother and child nutritional status
Multivariate analysis revealed that lack of medical care, unemployment and time since delivery were positively associated with poor maternal nutritional status. Due to the rapid postpartum weight loss, we suspect that maternal nutritional status continues to decline after parturition. The high consumption of glutinous rice protects mothers from caloric deficiency. However, our study suggests that 18% women consumed an excess of carbohydrates after delivery, which, associated with chronic carbohydrate imbalance and absence of diet diversification, is known to be associated with future obesity and diabetes, a special concern in developing countries (King et al., 2005). Overall, 10% of children were stunted or wasted which is similar to the national estimate of 10.4% for infants <6 months (Ministry of Health, 2001). The lack of accurate birth weight and gestational age for children born at home limit our interpretation (low birth weight in Laos is estimated to be 14%, UNICEF, 2006).
We observed an association between stunting and early complementary food given to infants but not with maternal food restriction. Exclusively breastfed Lao children tend to be taller than those receiving early glutinous rice supplementation (Graz, 1999). Severe stunting is a major nutritional concern in Laos, especially in remote rural settings where up to 74.1% of school children may be affected (Miyoshi et al., 2005; Phengxay et al., 2007). Early feeding of infants aged <30 days with chewed glutinous rice may also cause protein deficiency, because calories from rice tend to replace calories from breast milk (Valyasevi et al., 1967).
Nutritional education and antenatal care
We observed a high ANC attendance (91.3%), but a lower rate of hospital delivery (72.0%) and related absence of care seeking to education, parity and socioeconomic level. The perception that a healthy pregnancy does not need to be followed up by a health worker is widely held in Laos (FAO and IUCN, 2003). Restricted diet was related to primiparity and the place of delivery. Exposure to the hot bed was lower when the mother delivered at hospital. Delivery at the hospital was positively related with ANC. These associations suggest a role for ANC and post-delivery counselling in reducing inappropriate nutritional practices.
Antenatal attendance could be an ideal opportunity to address nutritional issues. However, the quality of education currently provided during this period is of concern since current practices are similar, apart for colostrums use, to traditional practices. North-east Thai nurses’ beliefs regarding postpartum traditions were quite different from contemporary evidence-based recommendations, with many nurses supporting restrictive diets, hot beds, discarding of colostrum and giving boiled water to neonates (Kaewsarn et al., 2003). Hence, prior to introducing educational programmes in antenatal care services, staff must be trained appropriately. Interventions to alter traditional postpartum dietary behaviour have been carried out in Laos, mainly among ethnic minorities (Khamhong et al., 2000; Kaufmann et al., 2001; Perks et al., 2006). A sustained 15-year community and education based programme, favouring exclusive breastfeeding up to 6 months, and appropriate introduction of nutritious complementary foods proved successful in Sayaboury Province (Perks et al., 2006). Nationwide extension of such programmes may be beneficial. Shorter term programmes have proved unsuccessful in reducing mother and child malnutrition (Khamhong et al., 2000).
Limitations of this study include its descriptive aspect, the late timing of the interviews in relation to delivery, and the inherent inaccuracies of 24 h dietary recall. Overestimation of the macronutritional value and underestimation of micronutritional loss by food processing may have occurred. Furthermore, we did not consider some factors which may hamper the bioavailability of nutrients, such as herbal tea, use of green leaves and fermented fish paste which contain thiaminases, which may aggravate thiamine deficiency (Vimokesant et al., 1975).
The study provides new insights into the continued high frequency of restricted postpartum diets in Laos and their consequences, risking thiamin, vitamin C and vitamin A deficiency in infants. More research is needed to understand the origins of food avoidance behaviours, their health impacts and possible solutions.
Conclusion
Traditional postpartum food restrictions are commonly observed in urban Laos. The diet of lactating women is of low diversity and excessively based on glutinous rice, resulting in intakes below the standard recommendations for lipids, proteins and micronutrients. Infants are at risk of vitamins A, C and thiamin deficiencies. Early infant food supplementation with glutinous rice is widely practiced and associated with infant stunting. More qualitative studies are needed to understand the sociocultural basis of avoidances and the reason for their persistence in Lao society. Attendance at antenatal care is high and could be an opportunity to improve nutrition in Lao women and children.
Acknowledgements
We are grateful for the assistance and collaboration of the health authorities of Vientiane Municipality and for the participation and interest of the mothers with their children. The assistance of V Phuangsavady, P Brossman, Mayfong Mayxay, JP René, L Srour and the staff of Institut de la Francophonie pour la Médecine Tropicale is gratefully acknowledged. Financial support was granted by Agence Universitaire de la Francophonie. Paul N Newton is supported by the Wellcome Trust (UK).
References
- Drewett R, Amatayakul K, Wongsawasdii L, Mangklabruks A, Ruckpaopunt S, Ruangyuttikarn C, et al. Nursing frequency and the energy intake from breast milk and supplementary food in a rural Thai population: a longitudinal study. Eur J Clin Nutr. 1993;47:880–891. [PubMed] [Google Scholar]
- FAO Food Composition Table for Use in East Asia. FAO Food Policy and Nutrition Division and US Department of health education and welfare: Rome. 1972 Part II Section A 1–334. available at: http://www.FAO.org/docrep/003/X6878E/X6878E00.htm#TOC.
- FAO/WHO Carbohydrates in human nutrition. (FAO Food and Nutrition Paper–66). Report of a Joint FAO/WHO Expert Consultation. 1998 available at: http://www.fao.org/docrep/W8079E/W8079E00.htm. [PubMed]
- FAO and IUCN The Role and Nutritional Value of Aquatic Resources in the Livelihoods of Rural People A Participatory Assessment in Attapeu Province, Lao PDR. 2003 available at: www.FAO.org/docrep/004/ad454e/ad454e00.htm.
- Gerhold C. Food habits of the valley people of Laos. J Am Diet Assoc. 1967;50:493–497. [PubMed] [Google Scholar]
- Giugliani ERJ, Victora CS. Complementary feeding. J Pediatr. 2000;76(Suppl 3):253–262. doi: 10.2223/jped.162. [DOI] [PubMed] [Google Scholar]
- Graz B. Impact on health of early supplementation with rice in infants in Laos. Med Trop. 1999;59:102–103. [PubMed] [Google Scholar]
- Kachondham Y, Dhanamitta S. A new horizon: addressing food and nutrition problems in the Lao People’s Democratic Republic. Food Nutr Bull. 1992;14:79–87. [Google Scholar]
- Kaewsarn P, Moyle W, Creedy D. Thai nurses’ beliefs about breastfeeding and postpartum practices. J Clin Nurs. 2003;12:467–475. doi: 10.1046/j.1365-2702.2003.00719.x. [DOI] [PubMed] [Google Scholar]
- Kaufmann S, Marchesich R, Dop MC. FAO Nutrition Country Laos. FAO Nutrition Country Profiles: Rome. 2003:1–38. available at: http://www.fao.org/ad/agn/nutrition/lao-e.stm.
- Kaufmann S, Phanlavong A, Kohl G. Nutrition and Poverty in Northern Laos: Achievements after 4 Years of Intensive Interventions. Institute of Nutritional Sciences, University of Giessen; Germany: 2001. (Lao-German Integrated Food Security Program). available at: http://www.uni-giessen.de/fbr09/int-nutr/Forschung-Arbeitskreis/POSTER-Silvia-Kaufmann.pdf. [Google Scholar]
- Khamhong K, Bodhisane N, Pathammavong C, Ouenvilay S, Senthavisouk B, Pongpaew P, et al. Nutritional status of pre-school children and women in selected villages in the Suvannakhet Province, Lao PDR-an intervention trial. Southeast Asian J Trop Med Public Health. 2000;31(Suppl 2):63–74. [PubMed] [Google Scholar]
- King H, Keuky L, Seng S, Khun T, Roglic G, Pinget M. Diabetes and associated disorders in Cambodia: two epidemiological surveys. Lancet. 2005;366:1633–1639. doi: 10.1016/S0140-6736(05)67662-3. [DOI] [PubMed] [Google Scholar]
- Latham MC. Human Nutrition in the Developing World. 1997 (FAO Food Nutrition Series No. 29) ISBN 92-5-103818-X: available at http://www.FAO.org/docrep/W0073E/W0073E00.htm.
- Marr JV. Individual dietary surveys: purposes and methods. World Rev Nutr Diet. 1971;13:105–164. doi: 10.1159/000391884. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Lao PDR. Health Status of the People in Lao PDR. National Institute of Public Health, Ministry of Health; Vientiane: 2001. pp. 1–144. [Google Scholar]
- Miyoshi M, Phommasack B, Nakamura S, Kuroiwa C. Nutritional status of children in rural Lao PDR: who are the most vulnerable? Eur J Clin Nutr. 2005;59:887–890. doi: 10.1038/sj.ejcn.1602160. [DOI] [PubMed] [Google Scholar]
- Perks C, Toole MJ, Phouthonsy K. District health programmes and health-sector reform: case study in the Lao People’s Democratic Republic. Bull World Health Organ. 2006;84:132–138. doi: 10.2471/blt.05.025403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phengxay M, Ali M, Yagyu F, Phengxay S, Kuroiwa C, Ushijima H. Risk factors for protein—energy malnutrition in children under 5 years: study from Luangprabang province, Laos. Ped Int. 2007;49:260–265. doi: 10.1111/j.1442-200X.2007.02354.x. [DOI] [PubMed] [Google Scholar]
- Pottier R. Santé et Société au Laos (1973–78) Paris Comité de Coopération avec le Laos (Ed); 1978. pp. 1–504. ISBN: 2914898568. [Google Scholar]
- Santos-Torres MI, Vasquez-Garibay E. Food taboos among nursing mothers of Mexico. J Health Popul Nutr. 2003;21:142–149. [PubMed] [Google Scholar]
- Saowakontha S, Chantraphosri V, Kampor P, Ketkowit K, Panomratanarak B, Thaworndunstid P, et al. Breast feeding behavior and supplementary food pattern of villagers in Udon Thani Province, northeast Thailand. Southeast Asian J Trop Med Public Health. 1995;26:73–77. [PubMed] [Google Scholar]
- Sayasone S, Odermatt P, Khammanivong K, Phomluangsyl S, Vinhl CV, Thin HM, et al. Bladder stones in childhood: a descriptive study in a rural setting in Saravan Province, Lao PDR. Southeast Asian J Trop Med Public Health. 2004;35(Suppl 2):S50–S52. [PubMed] [Google Scholar]
- Soukaloun D, Kounnavong S, Pengdy B, Boupha B, Durondej S, Olness K, et al. Dietary and socio-economic factors associated with beriberi in breastfed Lao infants. Ann Trop Paediatr. 2003;23:181–186. doi: 10.1179/027249303322296493. [DOI] [PubMed] [Google Scholar]
- Trigo M, Roncada MJ, Stewien GT, Pereira IM. Food taboos in the northern region of Brazil. Rev Saude Publica. 1989;23:455–464. doi: 10.1590/s0034-89101989000600003. [DOI] [PubMed] [Google Scholar]
- UNICEF Situation des Enfants dans le Monde 2006 New York. 2006 Available at: http://www.unicef.org/french/sowc.06/statistics/tables. php.
- United Nations . How to Weigh and Measure Children: Assessing the Nutritional Status of Young Children in Household Surveys. United Nations; New York: 1986. ISBN-13: 978-92-806-3917-9. Department of Technical Co-operation for Development and Statistical Annexe 1. [Google Scholar]
- United Nations Development Program . Human Development Report 2004: Cultural Liberty in Today’s Diverse World. UNDP; New York: 2006. available at: http://hdr.undp.org/en/reports/global/hdr2004/ [Google Scholar]
- Valyasevi ASB, Halstead S, Pantuwatana C, Tankayul C. Studies of bladder stone disease in Thailand. IV. Dietary habits, nutritional intake, and infant feeding practices among residents of a hypo- and hyper-endemic areas. Am J Clin Nutr. 1967;20:1340–1351. doi: 10.1093/ajcn/20.12.1340. [DOI] [PubMed] [Google Scholar]
- Vimokesant SL, Hilker DM, Nakornchai S, Rungruangsak K, Dhanamitta S. Effects of betel nut and fermented fish on the thiamin status of northeastern Thais. Am J Clin Nutr. 1975;28:1458–1463. doi: 10.1093/ajcn/28.12.1458. [DOI] [PubMed] [Google Scholar]
- WHO Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge. 1998 available from http://www.who.int/child-adolescenthealth/publications/NUTRITION/WHO_NUT_98.1.htm.
- WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]