Abstract
Over two-thirds of the 11.4 million cancer survivors in the United States can expect long-term survival, with many others living with cancer as a chronic disease controlled by ongoing therapy. However, behavioral co-morbidities often arise during treatment and persist long-term to complicate survival and reduce quality of life. In this review, the inter-relationships between cancer, depression, and sleep disturbance are described, with a focus on the role of sleep disturbance as a risk factor for depression. Increasing evidence also links alterations in inflammatory biology dynamics to these long-term effects of cancer diagnosis and treatment, and the hypothesis that sleep disturbance drives inflammation, which together contribute to depression, is discussed. Better understanding of the associations between inflammation and behavioral co-morbidities has the potential to refine prediction of risk and development of strategies for the prevention and treatment of sleep disturbance and depression in cancer survivors.
Introduction
With over 11.4 million cancer survivors, nearly 5% of the US population has been diagnosed with cancer in 2006 (Office of Cancer Survivorship, 2009). Over the next decade, the number of cancer survivors will grow dramatically due to the aging of the population and the resultant increased cancer incidence. Moreover, due to earlier detection and successful treatment for the disease, over two-thirds of individuals diagnosed with cancer today can expect long-term survival, with many others living with cancer as a chronic disease controlled by ongoing therapy.
Despite considerable advancements in diagnosis and treatment, symptoms or problems often arise during treatment and persist long-term to complicate improved survival and reduce quality of life. Indeed long-term behavioral co-morbidities such as depression and sleep disturbance are prominent and are thought to relate to the onset of cancer-related somatic symptoms such as fatigue and pain, and possibly cancer recurrence or second malignancies. In this review, the inter-relationships between cancer, depression, and sleep disturbance are described, with a focus on the role of sleep disturbance as a risk factor for depression. In addition, increasing evidence links alterations in inflammatory biology dynamics to these long-term and late effects of cancer treatment, and the hypothesis that sleep disturbance drives inflammation, which together contribute to depression, is discussed. Given the growing number of cancer survivors, effective management of the late effects of cancer and its treatment is needed. To this end, better understanding of the associations between inflammation and post-treatment symptoms has the potential to inform risk identification and the development of strategies for prevention and treatment of such behavioral co-morbidities as sleep disturbance and depression.
Depression
Prevalence
Major depression in patients with cancer occurs at a high rate, with a median point prevalence (15% to 29%) that is approximately three to five times greater than the general population (Miller et al., 2008; Raison et al., 2003; Rooney et al., 2011). However, prevalence estimates vary from 1.5% to 50%, depending on the cancer type, as well as the definition of depression and method of assessment (Fann et al., 2008; Massie, 2004). Indeed, the majority of studies find that 20% to 30% of women with breast cancer, for example, experience elevated depressive symptoms (Fann et al., 2008). Yet, the prevalence of major depressive disorder may be considerably lower; major depressive disorder is a clinical syndrome that lasts for at least 2 weeks and causes significant impairment in normal functioning. Among women newly diagnosed with breast cancer, about 9% also experienced major depression as determined by a structured clinical interview (Coyne et al., 1995). In contrast, among women with recurrent breast cancer, the prevalence of depression appears to be considerably higher (Gotay et al., 2007) with rates substantially exceeding that of the general population (Massie, 2004). Mitchell et al recently examined the meta-analytical pooled prevalence of depression defined by the Diagnostic and Statistical Manual of Mental Disorders using 24 studies with 4007 individuals across seven countries in palliative-care settings, and found rates of 16·5% (95% CI 13·1–20·3) for DSM-defined major depression, and 9·6% (3·6–18·1) for DSM-defined minor depression, although all types of depression occurred in 20·7% (12·9–29·8) of patients (Mitchell et al., 2011). However, despite the high prevalence of depression in association with cancer, there are few consistent correlates of this risk, as neither age, sex, nor clinical setting are associated with depression. Furthermore, there are inadequate data to examine the effects of cancer type and illness duration on depression occurrence (Mitchell et al., 2011).
Depression Disease Burden
As the population ages and the number of cancer survivors grows dramatically, depression is will increase by 2030 to a position of the greatest contributor to illness burden (Mathers et al., 2006). Moreover, because adults and especially older adults with depression often do not receive diagnosis and treatment (Alexopoulos, 2005), and only about 30–35% achieve remission using current treatment approaches (Evans et al., 2005), over two-thirds of the depression disease burden persists (Andrews et al., 2004; Chisholm et al., 2004) leading to staggering health care costs (Vos et al., 2004).
Depressed patients are also less likely to adhere to recommendations for treatment including cancer therapies. Meta-analytic findings demonstrate that depression triples the risk for nonadherence to medications (Fann et al., 2008). In turn, the use of emergency and medical inpatient services is disproportionately increased in persons diagnosed with cancer. For example, among Medicare beneficiaries diagnosed with cancer, use of emergency departments and medical inpatient services is twice as likely if they have significant depressive symptoms than if they do not (Himelhoch et al., 2004). These findings are consistent with other diseases in which co-morbid depression increases health care use, functional disability, and work absence (Stein et al., 2006). Lower medical adherence which is associated with poorer understanding of treatment recommendations, which in turn heightens anxiety about treatment adverse effects in depressed cancer patients (Ell et al., 2005).
Depression also increases risk for morbidity and mortality in several chronic diseases, including AIDS (Ickovics et al., 2001) and cardiovascular disease (Barefoot et al., 2000). In addition, some evidence suggests that depressed cancer patients have increased morbidity and, possibly, mortality (Gallo et al., 2007; Spiegel et al., 2003), although findings among cancer survivors are less consistent (Goodwin et al., 2004; Steel et al., 2007). Nevertheless, when the association between depressive symptoms and mortality rates were compared between participants with and without cancer among 10,025 participants in the National Health and Nutrition Examination Survey (Onitilo et al., 2006), results demonstrated that participants with both cancer and depressive symptoms had a 19% increased risk of death compared to participants with cancer only after adjusting for confounders. Likewise, Mykletun (Mykletun et al., 2007) found a 33% increased risk of death from cancer associated with disorder-level depressive symptoms in a prospective study of 61,349 adults in Norway followed for 4.4 years after depression assessment. Moreover, when the depression is unremitting and chronic, adverse health outcomes are more prominent as compared to the effects of an acute depressive episode (e.g., (Evans et al., 2005; Stommel et al., 2002). Finally, Pril et al recently reported that the presence of major depression was associated with worse survival in patients with non-small cell lung carcinoma, although treatment of such depression did not yield survival benefit (Pirl et al., 2012).
Risk Factors: Role of Cancer in Catalyzing the Occurrence of Depression
In the midst of receiving a diagnosis of cancer and managing the subsequent psychological and physiological challenges, rates of depressive symptoms markedly rise with increases typically highest in the first 6 months after cancer diagnosis, followed by declines over time with adjustment to the initial shock of diagnosis and acute effects of cancer treatment (Schag et al., 1993). For example, cancer treatments alone are associated with increased risks of depressive symptoms; prior to medical treatment about 10% of patients diagnosed with various cancers show depressed mood or anhedonia, two hallmark symptoms of depression, whereas during treatment over 20% endorse one of these symptoms (Fann et al., 2009). Importantly, one large-scale prospective study suggests that cancer diagnosis and treatment provokes depression leading to a four-fold increase in depression occurrence during the first two years after diagnosis as compared those who remain medically healthy. (Polsky et al., 2005) examined depressive symptoms prior to and after disease diagnosis in 5 biennial waves of the Health and Retirement Study involving more than 8,000 adults aged 51 to 61 without depressive symptoms at study onset. Within 2 years following diagnosis, individuals with cancer had the highest risk of significant depressive symptoms relative to no incident disease (Hazard Ratio = 3.55) and other diagnosed diseases (e.g., heart disease, arthritis). Moreover, the experience of cancer can prompt an episode of depression in addition to triggering depressive symptoms. Kangas et al. (Kangas et al., 2005) found that 29% of head/neck/lung cancer patients met interview-assessed criteria for major depressive disorder within 1 month of diagnosis, of whom only 29% met criteria for prior lifetime major depressive disorder. At 6 months, 22% met criteria for major depressive disorder, and 27% of those were new diagnoses. In comparison, note that the major depressive disorder point prevalence in women in the US general population is estimated at 5–9% and lifetime prevalence at 21% (Kessler et al., 2005); men have lower rates. Thus, the prevalence of depression in cancer survivors might be nearly four-fold greater than that in the general population. Studies also document elevated suicidal ideation/behavior in individuals with cancer, including breast cancer (for review see; Miller et al., 2008).
Sleep disturbance
Prevalence
Even before treatment, patients with cancer report significant sleep impairment, and among cancer survivors, sleep problems persist well beyond primary treatment. In an unselected sample of women with non-metastatic breast cancer, Savard et al. (Savard et al., 2001b) found that 19% met diagnostic criteria for insomnia, and that 58% of the women reported that the cancer or its treatment (e.g., adjuvant tamoxifen) either caused or aggravated their sleep problems. Indeed, cancer survivors have a 2- to 3 fold increase in the prevalence of insomnia symptoms compared to healthy adults, with nearly 51% reporting difficulties sleeping during the cancer survivorship period (Savard et al., 2001a). However, patients with different types of cancer reported different rates of sleep problems. In a survey of more than 1,000 patients with different types of cancer, 31% reported insomnia, with lung cancer patients having highest prevalence of sleep problems in general, and breast cancer patients having the highest prevalence of insomnia coupled with fatigue (Davidson et al., 2002). However, in a sample of 823 patients with diverse cancers receiving chemotherapy longitudinally, Palesh et al. found that breast cancer patients had the highest number of overall insomnia complaints, although lung cancer patients showed the highest prevalence of insomnia diagnosis or syndrome (Palesh et al. 2010). Importantly, the severity of insomnia persisted over the course of chemotherapy treatment with similar rates of insomnia complaints at cycle 1 and cycle 2. Polysomnographic data confirm reduced sleep efficiency, prolonged latency to fall asleep, and increased awake time during the night among cancer survivors (Savard et al., 2001b), and lung cancer show marked reductions in sleep efficiency as compared to insomniacs or breast cancer survivors (Silberfarb et al., 1993). However in one study, total sleep time as indexed by actigraphy increased during a course of chemotherapy in breast cancer patients (Liu et al., 2012b).
Sleep Disturbance and Disease Burden
Sleep disturbance comes at a considerable price. For example, sleep disturbance is a predictor of cancer-related fatigue. As pointed out by Fiorentino and Ancoli-Israel in a recent review of insomnia and its treatment in women with breast cancer (Fiorentino et al., 2006), sleep disturbance often co-occurs with fatigue in breast cancer patients and survivors. Disturbed sleep can be a predictor of fatigue; in turn, less physical activity as a result of fatigue may exacerbate sleep disturbance. However, among women undergoing chemotherapy for breast cancer, fatigue was related to daytime sleepiness and subjective reports of poor sleep quality, but not total sleep time as objectively assessed by actigraphy (Liu et al., 2012b). Hence, is unclear whether these two symptoms of fatigue and sleep disturbance merely co-occur in the same patient or have a causal association. Nevertheless, other data as further discussed below indicate that sleep disturbance is a potent predictor of depression relapse in persons with a history of prior depression (Cho et al., 2008), although there are no prospective data to address this question in cancer survivors.
Epidemiological data also implicate insomnia as a predictor of all-cause disease mortality over and above age, gender, and medical burden (Althuis et al., 1998; Ayas et al., 2003; Dew et al., 2003; Mallon et al., 2002; Newman et al., 2000). Indeed, EEG measures of prolonged sleep latency, sleep efficiency, and percentage of REM sleep predict all-cause mortality taking into the account of other known factors (e.g., age, gender, medical burden) (odds ratio 2.1, 95% CI: 1.25–3.66; odds ratio 1.93, 95% CI: 1.14–3.25; odds ratio, 1.7, 95% CI: 1.01–2.91) (Dew et al., 2003).
Risk Factors: Role of Cancer
In cancer survivors, sleep impairments are primarily characterized by problems falling asleep (Andrykowski et al., 1998), with difficulties of sleep maintenance (Engstrom et al., 1999) and duration also reported (Savard et al., 2001a). Given the varying kinds of sleep disturbance found in cancer survivors, it is thought that a number of different clinical factors can precipitate and/or perpetuate insomnia in cancer survivors. Old age, for example, increases the vulnerability for insomnia in cancer survivors (Savard et al., 2001a). Furthermore, it is generally assumed that insomnia is secondary to psychological distress and anxiety of cancer diagnosis and treatment, although Cimprich (Cimprich, 1999) found that sleep problems are frequent even in those patients who report low levels of anxiety. Pain is less likely to be a factor in sleep problems among cancer survivors who show no indication of residual or recurrent disease (Fortner et al., 2002).
Among cancer survivors, other cancer specific factors should also be considered. For example, Berger and Farr (Berger et al., 1999) reported that women undergoing chemotherapy showed a progressive increase in the number of awakenings with the duration of the treatment cycle. However, Liu et al. found no change in subjective sleep quality with an increase in total sleep time, during chemotherapy for women with breast cancer (Liu et al., 2012b) similar to the findings of Palesh et al across diverse cancer types(Palesh et al. 2010). Other studies also report that the prevalence of sleep problems was not related to time since diagnosis nor to treatment type (Savard et al., 2001a) and that sleep disturbance was similar across groups who receive different treatment (e.g., surgery, chemotherapy, radiation) (Davidson et al., 2002), although nocturnal menopausal symptoms increases reports of insomnia. Nevertheless, high rates of sleep complaints occur after initiation of adjuvant therapy (e.g., tamoxifen) for breast cancer, which can hasten premature menopause. Together, these data suggest that insomnia develops a chronic course in a substantial proportion of cancer survivors, especially in older adults (Savard et al., 2001a), contributing to fatigue, impairments in quality of life, and possibly depression. Despite such evidence, it also important to note that findings are mixed and adjuvant endocrine therapies (e.g., tamoxifen) have not been consistently related to either the onset or maintenance of insomnia symptoms (Berger et al., 2000; Stein et al., 2000). Circadian rhythm disturbances might also contribute to sleep disturbance, but consideration of the associations between cancer and biological rhythms is beyond the scope of this review. In sum, multiple cancer-specific factors increase vulnerability for sleep complaints and likely contribute to the perpetuation of these sleep problems and the onset of sleep disturbance in breast cancer survivors (Savard et al., 2001a). However, additional research is needed to uncover cancer-specific physiological, psychological, and behavioral factors that contribute to the development of insomnia during chemotherapy, similar to the conclusion offered by Palesh et al (Palesh et al.) in the largest study to date that longitudinally examined insomnia symptoms and clinical characteristics in a diverse sample of cancer patients undergoing chemotherapy.
Sleep Disturbance and Depression Risk
Insomnia is the most frequent sleep disturbance in depressed patients, and such sleep impairment is viewed as a symptomatic dimension of current depression. Sleep disturbance often lingers and its persistence can represent a residual phase of a major mood disorder. Alternatively, emergence of disturbed sleep may serve as a precursor or prodrome of depression that occurs later in life. Indeed, insomnia is increasingly viewed as an independent risk factor for depression. Although there are no prospective data in cancer survivors, some limited prospective data are available in non-cancer adults and older adults. For example, as part of the Epidemiologic Catchment Area study, Ford and Kamerow (Ford et al., 1989) found that persistent insomnia was associated with the incidence of new major depression. As such, these findings were among the first to identify the need for research to determine if early recognition and treatment of sleep disturbance, a modifiable risk factor (Cole et al., 2003), might forestall or prevent incident depression. Even less is known about the prospective association between sleep disturbance and depression recurrence, as opposed to incident new major depression. Whereas sleep disturbance has been shown to predict depression relapse and recurrence in late life (Buysse et al., 1996; Dew et al., 2001; Dombrovski et al., 2007; Flint et al., 2000), these data are limited to populations who were conveniently recruited from specialty clinics. Hence, the generalizability of such observations to community dwelling adults and/or cancer survivors is not known.
Furthermore, despite evidence that sleep disturbance and other factors (e.g., life stress, social support) are associated with persistence of depression in community dwelling adults (Beekman et al., 2001; Beekman et al., 1995; Denihan et al., 2000), their prospective contribution to depression recurrence has not been extensively evaluated nor examined in large groups of cancer survivors. For example, in a meta-analysis of 20 prospective studies (Cole et al., 2003), only four studies used multivariate approaches to identify sleep disturbance as a predictor of depression onset among elderly community subjects and none of these studies addressed cancer-related variable, and many of these studies included small samples. However, in community-dwelling older adults, Cho et al. recently found in a two-year longitudinal study that sleep disturbance is a predictor of incident depression among non-depressed elderly community subjects, and that the risk posed by sleep disturbance is greater – maybe specific – for depression recurrence than for depression incidence (Cho et al., 2008). For example, in this sample depression occurrence was strongly predicted by prior depression history (odds ratio 38.65, 95% CI 4.72–316.43, P=0.001), with a cumulative incidence of depressive disorders of 16.9% (11.0–24.3%) at 2 years. Moreover, sleep disturbance at baseline was significantly associated with depression recurrence (odds ratio 4.84, 95% CI 1.40–16.73, P=0.01), taking into account other predictors of depression recurrence including antidepressant medication use (3.25, 1.23–8.53, P=0.02), and other depressive symptoms (1.15, 1.02–1.30, P=0.03). Given that over one-third of individuals with prior depression history were using antidepressant medications, and such use was not protective in ameliorating the risk of sleep disturbance on depression occurrence, interventions that specifically target sleep disturbance might have a unique role in reducing subsequent depressive morbidity. Importantly, cancer diagnosis and treatment introduce many extraneous variables that might alter the association between sleep disturbance and depression risk; research that target cancer survivors is needed to determine whether risk models that perform well in older adults generalize to cancer survivors.
Inflammation, Sleep Disturbance and Depressive Symptoms in Cancer
Overview
Among the biological mechanisms contributing to onset and maintenance of sleep disturbance and/or depression, inflammation has emerged as one important pathway, which may be especially relevant in cancer survivors. In association with increased prevalence of sleep disturbance and depression, prominent increases in proinflammatory cytokine activity occur in cancer survivors. Indeed, epidemiological studies have shown that chronic inflammation predisposes individuals to various types of cancer including breast cancer, and underlying inflammatory responses are linked to 15–20% of all deaths from cancer worldwide (Mantovani et al., 2008). In addition, chronic inflammation is reported to be associated with recurrence of breast cancer (Cole, 2009). Moreover, cancer treatments are potential inducers of inflammation. For example, chemotherapy is associated with acute increases in inflammatory markers (Mills et al., 2008; Mills et al., 2004; Wang et al., 2010), which may persist long into survivorship, with some data suggesting that such increases may be associated with fatigue and sleep disturbance during chemotherapy treatment (Liu et al., 2012a; Liu et al., 2012c). Among the panoply of molecules involved in cancer-related inflammation, key endogenous factors can be identified including transcription factors such as nuclear factor-κB (NF-κB), and major inflammatory cytokines (such as IL-1β, IL-6, and TNF-α)(Karin, 2006). As described below, wake–sleep cycles have emerged as homeostatic regulators of inflammatory biology, in which sleep loss induces activation of NF-κB to coordinate the production of inflammatory mediators and systemic inflammation. In turn, proinflammatory cytokines are thought to contribute, in part, to the onset of depressive symptoms. In addition, inflammatory processes are being investigated as explanatory mechanisms for the demonstrated links between depression and morbidity and all-cause and disease-specific mortality, including cancer.
Studies in laboratory animals and humans provide compelling evidence that administration of innate immune cytokines induces a syndrome of “sickness behavior” that has many overlapping features with the behavioral symptoms commonly experienced by cancer patients, including sleep disturbance and depression (Dantzer et al., 2008; Irwin et al., 2011a). Such behavioral effects of inflammatory cytokines are secondary to the capacity of peripheral cytokine signals to access the brain, activate inflammatory responses within the brain, and interact with neurobiolgical pathways involved in behavioral states such as sleep disturbance and depression (Dantzer et al., 2008; Irwin et al., 2011a; Miller et al., 2008). Within the brain, pro-inflammatory cytokines decrease the activity of key behavior-modulating neurotransmitter systems including norepinephrine, dopamine and serotonin (Miller et al., 2009) all of which play a major role in the regulation of multiple behaviors and are the primary targets for currently available psychopharmacologic treatments of depression (Dantzer et al., 2008; Irwin et al., 2011a; Miller et al., 2008).
Sleep Disturbance and Inflammation
Sleep has key consequences for proinflammatory cytokine expression. Experimental sleep restriction, with a loss of total sleep time, leads to daytime increases in production and circulating levels IL-6 levels (Meier-Ewert et al., 2004); (Redwine et al., 2003; Shearer et al., 2001; Vgontzas et al., 1999). In addition, loss of sleep for only part of the night induces an upregulation of leukocyte expression of pro-inflammatory cyotkine genes and increased NF-kB activity (Irwin et al., 2006b; Irwin et al., 2008). These effects are especially pronounced in women (Irwin et al., 2010; Irwin et al., 2008), possibly due to sex differences in sympathetic nervous system upregulation of IL-6 production (O’Connor et al., 2007), which together might contribute to sex differences in the incidence of inflammation-related behavioral and autoimmune diseases. Observational studies have also identified elevated levels of C-reactive protein (CRP) and other inflammation-related biomarkers in night-shift workers who have a disruption of sleep-wake activity, as well as insomniacs who report poor sleep quality and disruption of sleep continuity (e.g., difficulties with sleep onset or sleep maintenance with an overall decreases in total sleep time) (Motivala et al., 2007). Little is know about the effects of hypersomnia on inflammatory markers, although there is evidence that long sleepers (i.e., total sleep time more than 8 hours per day) have an increased risk of mortality similar to short sleeper (i.e., total sleep time less than 6 hours per day) (Kripke et al., 2002). However, despite evidence of increased inflammation in cancer survivors and compelling observational and experimental data indicating a relationship between sleep disturbance and innate immune cytokines such as IL-6, the relationship between sleep and inflammatory markers in cancer survivors has not been rigorously examined.
Systemic inflammation may also have reciprocal effects and play a role in the homeostatic regulation of sleep (Imeri et al., 2009). Animal genetic studies and LPS administration studies in humans (Imeri et al., 2009; Mullington et al., 2000) have linked changes in non-rapid eye movement (NREM) sleep to elevated levels of circulating type I IFN and pro-inflammatory cytokines. In animals, cytokines such as TNF increase NREM- and decrease REM sleep (Imeri et al., 2009), although Hogan et al. found that IL-6 administration produces a fragmentation of sleep in rats (Hogan et al., 2003). In humans, pharmacological administration of a single dose of IL-6 or treatment with IFNα in humans induce decreases in NREM, slow-wave sleep and increases in REM sleep (Imeri et al., 2009; Raison et al.). In contrast, a single dose of endotoxin, which induces physiologic, as opposed to pharmacological, elevations of proinflammatory cytokines, has been found to enhance sleep depth (Mullington et al., 2000). However, these pharmacologic and experimental approaches yield elevations of proinflammatory cytokines that are several fold greater than found in the resting, baseline condition, and a further question concerns the association between varying levels of proinflammatory cytokines at rest and sleep measures. In healthy individuals, levels of IL-6 and TNFα obtained prior to sleep onset, and without experimental or pharmacologic induction, temporally correlate with increased sleep latency and REM sleep independent of other clinical factors (Irwin et al., 2004). Moreover, TNF antagonism that blocks endogenous levels of TNFα has also been found to normalize REM sleep levels (for example, in abstinent alcohol-dependent patients, who have elevated amounts of REM sleep) (Irwin et al., 2009).
In summary, regulation of sleep architecture by the innate immune system may play a substantial role in structuring overall inflammatory homeostasis (Imeri et al., 2009; Motivala et al., 2007), given the substantial fraction of time we spend asleep, the general immunological activation that occurs during sleep (Motivala et al., 2007) and epidemiological links between abnormally high REM sleep and mortality (Dew et al., 2003). Future research is needed to determine whether increases of proinflammatory cytokines are a key biological mechanism through which disordered sleep accelerates morbid outcomes, including depression risk, in cancer survivors.
Depression and Inflammation
Proinflammatory cytokines are thought to contribute, in part, to the onset of depressive symptoms, and possibly to the onset and incidence of major depressive disorder in susceptible populations such as cancer survivors. A recent meta-analysis (Howren et al., 2009) revealed significant effect sizes for the relation of depression and C-reactive protein (CRP) (51 studies), interleukin (IL)-6 (62 studies), IL-1 (14 studies), and IL-1 receptor antagonist (IL-1ra) (9 studies), with effect sizes ranging from d =0.15 to 0.35. Effect sizes remained significant when body mass index was controlled, and the effects were larger when medication use (e.g., antidepressants, statins) was controlled. Clinically depressed patient samples demonstrated the strongest relations, although relations also were reliable in community samples. Among the seven study samples with cancer, depression was related significantly to IL-6 (Musselman et al., 2001b; Seruga et al., 2008; Soygur et al., 2007). Tumor necrosis factor (TNF-α) also has been linked to depression (Seruga et al., 2008); relevant research on other inflammatory markers was not available in cancer samples. Howren et al (Howren et al., 2009) noted the plausibility of causation in either direction, although as described above, basic animal research has implicated proinflammatory activity in inducing a motivational state that parallels depressive symptoms (Dantzer et al., 2008). Indeed, some large scale prospective studies have found that elevated levels of systemic inflammation (e.g., C-reactive protein, CRP) are prospectively associated with depression (Gimeno et al., 2009; Matthews et al., 2007), although others have suggested that depression leads to elevated levels of inflammatory markers (Duivis et al., 2011). Nevertheless, administration of the cytokine interferon-α to cancer patients and other clinical samples induces increases of depressive symptoms that are responsive to treatment with antidepressants (Miller et al., 2008). Together, these naturalistic and experimental observations suggest that activation of inflammatory pathways may be causally linked to the onset of depressive symptoms, at least in certain vulnerable patient populations such as those with cancer.
Inflammatory cytokines can alter the metabolism of key monoamines that are involved in the pathogenesis of mood disorders (Dantzer et al., 1999). For example, cytokine-induced behavioral changes are associated with alterations in the metabolism of relevant neurotransmitters such as serotonin, norepinephrine, and dopamine, all of which play a major role in the regulation of depressive symptoms. (Miller et al., 2008; Miller et al., 2009). Proinflammatory cytokines through stimulation of multiple inflammatory signaling pathways (e.g., nuclear factor κB, NF-κB) activate neurotransmitter metabolism, which in turns leads to decreased availability of tryptophan, the amino acid precursor for serotonin. Furthermore, the reuptake of monoamines is influenced by cytokines and their signaling pathways, which further reduces the availability of these neurotransmitters contributing behavioral symptoms such as depression.
Additionally, recent evidence suggests that polymorphisms in several cytokine genes are potential markers for genetic susceptibility for depressive symptoms and treatment response (Miller et al., 2009). Together, these results suggest that blockade of inflammatory cytokines might diminish risk and improve treatment response of depression, although there are no studies in cancer survivors with evidence of increases in markers of inflammation. These data also raise the possibility that circulating inflammatory biomarkers and inflammation-related genetic polymorphisms might be used to help guide targeted therapy for specific major depressive disorder subtypes that are thought to have an inflammatory component such as depression in older adults or in those with inflammation-associated disease including cancer. It is important to note further that links between inflammation and depressive symptoms have also led to the hypothesis that the increased prevalence of major depressive in modern industrialized society may stem form decreased exposure to tolerogenic microorganisms, which contributes to dysregulated inflammatory signaling (a psychiatric version of the “hygiene hypothesis”)(Raison et al., 2010).
Given the “main effects” of inflammation-related gene polymorphisms on depression (i.e., mediated via genetic effects on inflammatory cytokine levels), it is also conceivable that inflammatory signaling may interact with brain neurotransmitter systems to affect the risk or severity of depression. Under such a model, polymorphisms in neurotransmitter-related genes (e.g., the serotonin transporter promoter polymorphism 5HTTLPR, coding polymorphisms in BDNF and COMT genes;(Uher et al., 2008) might affect CNS vulnerability/resilience to the depression-promoting effects of inflammatory cytokines. With this hypothesis, inflammation could be viewed as a moderator of brain-related genetic risk factors for depression, serving as a physiologic “stress” to actualize a genetic “diathesis” as previously observed in studies of interaction between psychosocial stress and the 5HTTLPR polymorphism (Caspi et al., 2003). Consistent with this notion, antidepressant medications (e.g., serotonin- and norepinephrine reuptake inhibitors) interact with brain neurotransmitter gene polymorphisms (serotonin transporter gene) to affect monoamine metabolism, which in turn have been shown to influence the development of cytokine-induced depressive symptoms in humans (Bull et al., 2009). Alternatively, variants neurotransmitter genes such as the serotonin transporter gene might influence inflammatory profile and risk for depression. Indeed, it is thought that variants in the serotonin transporter gene (i.e., 5-HTTLPR polymorphisms) influence susceptibility to depression in which those carrying two short alleles of the 5-HTTLPR gene have increased risk of depression. Recent evidence demonstrated that SS individuals exhibit a pro-inflammatory bias under resting conditions and/or during laboratory stress(Fredericks et al., 2010). Moreover, among individual who have the serotonin transporter gene variant, SLC6A4 gene, increases in both depressive symptoms and IL-6 plasma levels have been identified (Su et al., 2009).
Functional neuroimaging studies in humans have begun to map the specific neural circuits associated with cytokine-induced depressive symptoms, and have identified altered connectivity among the subgenual anterior cingulate cortex, amygdala and medial prefrontal cortex (Eisenberger et al., 2009; Harrison et al., 2009) and reduced ventral striatum response to reward cues (Eisenberger et al. 2010a). It is known, for example, that clinical depression is associated with alterations in brain circuits that are involved in emotion processing (e.g., anterior cingulate cortex). In addition to playing an important role in detecting physical and social threat, and subsequently recruiting attention and coping resources to minimize danger (Lieberman et al., 2009), increased activity of the anterior cingulate cortex has been demonstrated in individuals at risk for mood and anxiety disorders, including those with high-trait anxiety, neuroticism, and obsessive-compulsive disorder (Eisenberger et al., 2004). Using an experimental challenge, inflammatory activation increased in regional blood flow in the dorsal part of the anterior cingulate cortex (dACC) as revealed by functional magnetic resonance imaging during a social rejection task (Eisenberger et al., 2010b; Eisenberger et al., 2009). In association with such cytokine-inducted activation of the dACC, depressive symptoms were elevated, and the severity of depressive symptoms correlated with dACC in women, but not in men (Eisenberger et al., 2009). Finally, we have found that experimentally-induced systemic inflammation alters neural activity that is associated with anhedonia, a key diagnostic symptom of depression (Eisenberger et al., 2010a). Along with increases in self-reported and observer-rated depressed mood, activity in the ventral striatum was reduced in response to monetary reward cues. Hence, inflammation alters reward-related neural responding in humans and these reward-related neural responses mediate the effects of inflammation on depressed mood (Eisenberger et al., 2010a).
In summary, we and others have found that activation of proinflammatory cytokines leads to marked increases in depressed mood (Eisenberger et al., 2010b; Eisenberger et al. 2009). In contrast, pharmacologic blockade of inflammation activity improves sleep (Irwin et al., 2009) and reduces depressive symptom severity (Tyring et al., 2006). Further research is needed to examine the bi-directional relationships between inflammation and depression occurrence, and the potential role of sleep disturbance in driving activation of inflammatory biology. Such work has the potential to guide development of personalized strategies for depression treatment, and possibly depression prevention in cancer survivors who are at high risk for depression occurrence and/or recurrence.
Development of Biological Treatments Targeting Inflammatory Biology
Biological pathways such as inflammation are hypothesized to contribute to depression occurrence, which together are driven in part by biobehavioral risk factors such as sleep disturbance. Hence, it is important to utilize such pathophysiological models of depression to inform the development of interventions that have the potential to treat and/or prevent depression (Munoz et al., 2010; Reynolds, 2009). Insight into the role of these biological mechanisms has the potential to improve the efficiency of risk identification and depression prevention and possibly treatment, which may be especially true for cancer survivors who show greater abnormalities in inflammatory dynamics. As an example, the use of molecular signaling methodologies can be utilized to assist in identifying the upstream mechanisms that are differentially expressed in cancer survivors, triggered by sleep disturbance, and causal in the differential increased risk of depression in cancer survivors versus. adults.
Under this hypothesis, it is logical to consider treatments that target the upstream components in the cytokine-to-CNS-behavior link. For example, candidate pharmacologic treatments would include cytokine antagonists, anti-inflammatory agents, and other drugs that disrupt cytokine signaling pathways (eg, NF-κB) (Miller et al., 2008; Miller et al., 2009). Indeed, several recent trials have demonstrated that TNF-α-blockade with etanercept is safe in patients with advanced cancer (Madhusudan et al., 2004; Madhusudan et al., 2005), and one study found that chemotherapy fatigue was reduced with this medication (Monk et al., 2006). Moreover, given the role of NFκB pathways in cancer etiology and progression (Karin, 2006), this work would provide a foundation for collaborative efforts between behavioral scientists and oncologists on the full spectrum of activity of relevant antagonists of inflammatory pathways on health and quality of life outcomes in cancer patients. Alternatively, at the level of the CNS, inflammation induced alterations in neurotransmitter systems might be targeted by agents for specific monoamine systems. For example, use of a serotonin reuptake inhibitor, paroxetine, prior to cancer treatment has been found to reduce depression in cancer patients undergoing chemotherapy with IFNα (Musselman et al., 2001a). In addition, the use of paroxetine has been found to effectively reduce depressive symptom severity, but not fatigue, during chemotherapy in breast cancer patients (Roscoe et al., 2005). Coupling such clinical trials with monitoring specific inflammatory biomarkers has the potential to optimize treatment response characterization. Moreover, knowledge about variants in inflammatory response genes might identify those patient populations who are most likely to benefit from such inflammation-targeted and/or neuropsychopharmacologic treatments.
Development of Behavioral Treatments Targeting Inflammatory Biology
Given the role of psychological stress on inflammatory dynamics, interventions that specifically target stress responses such as cognitive-behavioral psychotherapies may be especially relevant in the link between sleep disturbance, inflammation, and depression risk. Furthermore, given cancer treatment is associated with the onset of sleep disturbance and increases in depressive symptoms, the use of such interventions prior and during cancer treatment may hold considerable promise, although to our knowledge there is an absence of such research to date.
Such behavioral therapies include components such as relaxation training, enhancement of coping and/or emotion regulation skills, and establishment of appropriate sleep-wake habits and beliefs about sleep. For example, a recent cognitive-behavioral therapy program focusing on coping, sleep, physical activity, and social support was found to lead to significant improvements in fatigue in 54% of cancer survivors compared with 4% of patients assigned to a control condition, although inflammation was not evaluated (Gielissen et al., 2006). However, among those with an underlying inflammatory disorder (i.e., rheumatoid arthritis), we determined that an intervention that specifically targets emotion regulation is more effective in improving depression outcomes than an omnibus cognitive behavioral treatment, and that this benefit is particularly robust among those who have a prior history of depression (Zautra et al., 2008). The intervention for emotion regulation was based on practices of mindfulness, whereas the cognitive behavioral treatment involved a program of specific verbal/written protocols guiding participants through exercises designed to restructure dysfunctional thoughts and ruminations that contribute to negative perceptions of self and the environment. Benefits on the cellular expression of proinflammatory cytokines were found after 16 weeks in persons who had an improvement of depression (Zautra et al., 2008).
Several other behavioral interventions have been found to modulate inflammatory signaling in the innate immune system including aerobic exercise (Nicklas et al., 2008), compassion meditation (Pace et al., 2009) and Tai Chi (Irwin et al., 2011b; Lavretsky et al.) in association in improvements in sleep disturbance, for example. Moderate intensity physical activities such as walking for 20–30 minutes per day, which provides aerobic training without activating anaerobic respiration led to benefits on inflammatory markers after 12 months (Nicklas et al., 2008), but only among those who had elevated levels at baseline. Similarly, a meditation that involved thought focusing directed toward compassion of others has been to reduce sympathetic arousal mechanisms, and alter inflammatory responses to stress with benefits on inflammatory markers after 6 weeks (Pace et al., 2009). Finally, Tai Chi Chih, a Westernized form of the Chinese martial art Tai Chi, involving a slow moving meditation involving 20 minutes of aerobic exercise with relaxed breathing and attentional focus and body awareness led to benefits on inflammatory markers after 25 weeks (Irwin et al., 2011b) with impacts reported on biomarkers of inflammation including pro-inflammatory cytokine levels (e.g., CRP) and ex vivo cellular production of TNF and IL-6 in response to LPS stimulation. Moreover, the latter intervention has been found to improve sleep quality (Irwin et al., 2011b), and augment the treatment efficacy of antidepressant medications concomitant with reductions in inflammation (Lavretsky et al., 2011). Importantly, the regulation of leukocytes by these behavioral treatments may contribute to their neurobiological and behavioral impact if, for example, neurally-mediated reductions in peripheral inflammation feed back to reciprocally reduce depressive symptoms.
Summary: Toward Depression Prevention in Cancer Survivors
Multiple clinical, behavioral (e.g., sleep disturbance), and biological factors (e.g., inflammation) have been found to contribute to depression risk in non-cancer adults. However, cancer-related variables may alter the depression risk profile initially found in non-cancer persons; prospective research in cancer survivors is needed to address this critical gap.
Insight into the selective profile of risk indicators in cancer survivors has the potential to advance the design of a depression prevention trial. For example, consideration of profiles of two or more risk factors (Schoevers et al., 2006) is a necessary strategy to optimize health gains, minimize effort and concomitant costs, and lead to a substantial drop in number needed to treat (NNT) in a prevention trial. Unfortunately, the majority of prior depression prevention studies have selected broad target groups (e.g., primary care patients; those with medical disorders) rather than using disease specific and/or multivariate approaches in selection of a high risk population (Munoz et al., 2010). No depression prevention study has been conducted in cancer survivors despite the high prevalence of depression in this population.
Defining the unique and specific role of sleep disturbance in depression risk represents an important paradigm shift in depression treatment and/or prevention trials. Most prior research, conducted in non-cancer populations, have typically employed broad-based psychoeducational treatments within the cognitive behavioral “family”, in order for participants to learn practical skills intended to help them cope with and overcome depressive feelings, possibly in the context of interpersonal events (e.g. conflicts, transitions)(Munoz et al., 2010). Given that cancer specific factors uniquely contribute to sleep disturbance in cancer survivors, development of a specific intervention that targets this modifiable risk factor is an efficient strategy. Moreover, using an efficacious treatment such as cognitive behavioral therapy for insomnia, which is found to be as effective as pharmacologic treatments, shows considerable promise in improving sleep disturbance (Irwin et al., 2006a; Nicassio et al., 1997).
Finally, understanding the role of inflammatory biology dynamics in sleep disturbance and depression has the potential to refine prediction of risk and treatment response. Alternatively, the efficacy of behavioral interventions might be bolstered by the use of medications or other interventions (e.g., exercise) that attenuate inflammation. As such, an increasing focus on inflammation represents a major advance for current clinical practices, by providing a plausible biologic mechanism to explain variability in risk and response to treatment in cancer populations with depression.
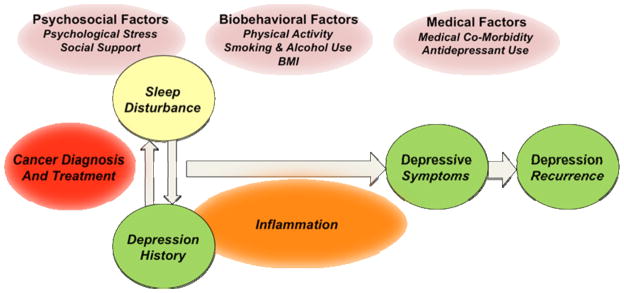
Figure 1.
Model depicting the impact of depression history and sleep disturbance on occurrence of depressive symptoms and depressive episode(s), taking into account the relationships with inflammation and psychosocial-, biobehavioral-, and medical factors in cancer survivors.
Highlights.
Sleep disturbance and inflammation are critical biobehavioral targets for the identification of risk and prevention of depression in cancer survivors.
Acknowledgments
Supported by R01-AG034588; R01-AG026364; R01-CA119159; R01-HL079955; R01 HL095799; P30-AG028748; UL RR 033176 to MI, and the Cousins Center for Psychoneuroimmunology (MRI); R01-CA 109650 and the Breast Cancer Research Foundation (PAG), and R01CA136743-01A2 (RH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- Althuis MD, Fredman L, Langenberg PW, Magaziner J. The relationship between insomnia and mortality among community-dwelling older women. J Am Geriatr Soc. 1998;46:1270–1273. doi: 10.1111/j.1532-5415.1998.tb04544.x. [DOI] [PubMed] [Google Scholar]
- Andrews G, Issakidis C, Sanderson K, Corry J, Lapsley H. Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry. 2004;184:526–533. doi: 10.1192/bjp.184.6.526. [DOI] [PubMed] [Google Scholar]
- Andrykowski MA, Curran SL, Lightner R. Off-treatment fatigue in breast cancer survivors: a controlled comparison. J Behav Med. 1998;21:1–18. doi: 10.1023/a:1018700303959. [DOI] [PubMed] [Google Scholar]
- Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, Hu FB. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Brummett BH, Helms MJ, Mark DB, Siegler IC, Williams RB. Depressive symptoms and survival of patients with coronary artery disease. Psychosom Med. 2000;62:790–795. doi: 10.1097/00006842-200011000-00008. [DOI] [PubMed] [Google Scholar]
- Beekman AT, Deeg DJ, Geerlings SW, Schoevers RA, Smit JH, van Tilburg W. Emergence and persistence of late life depression: a 3-year follow-up of the Longitudinal Aging Study Amsterdam. J Affect Disord. 2001;65:131–138. doi: 10.1016/s0165-0327(00)00243-3. [DOI] [PubMed] [Google Scholar]
- Beekman AT, Deeg DJ, Smit JH, van Tilburg W. Predicting the course of depression in the older population: results from a community-based study in The Netherlands. J Affect Disord. 1995;34:41–49. doi: 10.1016/0165-0327(94)00103-g. [DOI] [PubMed] [Google Scholar]
- Berger AM, Farr L. The influence of daytime inactivity and nighttime restlessness on cancer-related fatigue. Oncol Nurs Forum. 1999;26:1663–1671. [PubMed] [Google Scholar]
- Berger AM, Higginbotham P. Correlates of fatigue during and following adjuvant breast cancer chemotherapy: a pilot study. Oncol Nurs Forum. 2000;27:1443–1448. [PubMed] [Google Scholar]
- Bull SJ, Huezo-Diaz P, Binder EB, Cubells JF, Ranjith G, Maddock C, Miyazaki C, Alexander N, Hotopf M, Cleare AJ, Norris S, Cassidy E, Aitchison KJ, Miller AH, Pariante CM. Functional polymorphisms in the interleukin-6 and serotonin transporter genes, and depression and fatigue induced by interferon-alpha and ribavirin treatment. Mol Psychiatry. 2009;14:1095–1104. doi: 10.1038/mp.2008.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, 3rd, Hoch CC, Houck PR, Kupfer DJ, Mazumdar S, Frank E. Longitudinal effects of nortriptyline on EEG sleep and the likelihood of recurrence in elderly depressed patients. Neuropsychopharm. 1996;14:243–252. doi: 10.1016/0893-133X(95)00114-S. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Chisholm D, Sanderson K, Ayuso-Mateos JL, Saxena S. Reducing the global burden of depression: population-level analysis of intervention cost-effectiveness in 14 world regions. Br J Psychiatry. 2004;184:393–403. doi: 10.1192/bjp.184.5.393. [DOI] [PubMed] [Google Scholar]
- Cho HJ, Lavretsky H, Olmstead R, Levin MJ, Oxman MN, Irwin MR. Sleep disturbance and depression recurrence in community-dwelling older adults: a prospective study. Am J Psychiatry. 2008;165:1543–1550. doi: 10.1176/appi.ajp.2008.07121882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimprich B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs. 1999;22:185–194. doi: 10.1097/00002820-199906000-00001. quiz 195. [DOI] [PubMed] [Google Scholar]
- Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160:1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- Cole SW. Chronic inflammation and breast cancer recurrence. J Clin Oncol. 2009;27:3418–3419. doi: 10.1200/JCO.2009.21.9782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC, Schwenk TL, Fechner-Bates S. Nondetection of depression by primary care physicians reconsidered. Gen Hosp Psychiatry. 1995;17:3–12. doi: 10.1016/0163-8343(94)00056-j. [DOI] [PubMed] [Google Scholar]
- Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantzer R, Wollman EE, Yirmiya R, editors. Cytokines, Stress and Depression. Kluwer Academic Publishers; New York: 1999. [DOI] [PubMed] [Google Scholar]
- Davidson JR, MacLean AW, Brundage MD, Schulze K. Sleep disturbance in cancer patients. Soc Sci Med. 2002;54:1309–1321. doi: 10.1016/s0277-9536(01)00043-0. [DOI] [PubMed] [Google Scholar]
- Denihan A, Kirby M, Bruce I, Cunningham C, Coakley D, Lawlor BA. Three-year prognosis of depression in the community-dwelling elderly. Br J Psychiatry. 2000;176:453–457. doi: 10.1192/bjp.176.5.453. [DOI] [PubMed] [Google Scholar]
- Dew MA, Hoch CC, Buysse DJ, Monk TH, Begely AE, Houck PR, Hall M, Kupper DJ, Reynold CF. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65:63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- Dew MA, Reynolds CF, 3rd, Mulsant B, Frank E, Houck PR, Mazumdar S, Begley A, Kupfer DJ. Initial recovery patterns may predict which maintenance therapies for depression will keep older adults well. J Affect Disord. 2001;65:155–166. doi: 10.1016/s0165-0327(00)00280-9. [DOI] [PubMed] [Google Scholar]
- Dombrovski AY, Mulsant BH, Houck PR, Mazumdar S, Lenze EJ, Andreescu C, Cyranowski JM, Reynolds CF., 3rd Residual symptoms and recurrence during maintenance treatment of late-life depression. J Affect Disord. 2007;103:77–82. doi: 10.1016/j.jad.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duivis HE, de Jonge P, Penninx BW, Na BY, Cohen BE, Whooley MA. Depressive symptoms, health behaviors, and subsequent inflammation in patients with coronary heart disease: prospective findings from the heart and soul study. Am J Psychiatry. 2011;168:913–920. doi: 10.1176/appi.ajp.2011.10081163. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Berkman ET, Inagaki TK, Rameson LT, Mashal NM, Irwin MR. Inflammation-induced anhedonia: endotoxin reduces ventral striatum responses to reward. Biol Psychiatry. 2010a;68:748–754. doi: 10.1016/j.biopsych.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR. Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Behav Immun. 2010b;24:558–563. doi: 10.1016/j.bbi.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Inagaki TK, Rameson LT, Mashal NM, Irwin MR. An fMRI study of cytokine-induced depressed mood and social pain: the role of sex differences. Neuroimage. 2009;47:881–890. doi: 10.1016/j.neuroimage.2009.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD. Why rejection hurts: a common neural alarm system for physical and social pain. Trends Cogn Sci. 2004;8:294–300. doi: 10.1016/j.tics.2004.05.010. [DOI] [PubMed] [Google Scholar]
- Ell K, Sanchez K, Vourlekis B, Lee PJ, Dwight-Johnson M, Lagomasino I, Muderspach L, Russell C. Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecologic cancer. J Clin Oncol. 2005;23:3052–3060. doi: 10.1200/JCO.2005.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom CA, Strohl RA, Rose L, Lewandowski L, Stefanek ME. Sleep alterations in cancer patients. Cancer Nurs. 1999;22:143–148. doi: 10.1097/00002820-199904000-00006. [DOI] [PubMed] [Google Scholar]
- Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishnan KR, Nemeroff CB, Bremner JD, Carney RM, Coyne JC, Delong MR, Frasure-Smith N, Glassman AH, Gold PW, Grant I, Gwyther L, Ironson G, Johnson RL, Kanner AM, Katon WJ, Kaufmann PG, Keefe FJ, Ketter T, Laughren TP, Leserman J, Lyketsos CG, McDonald WM, McEwen BS, Miller AH, Musselman D, O’Connor C, Petitto JM, Pollock BG, Robinson RG, Roose SP, Rowland J, Sheline Y, Sheps DS, Simon G, Spiegel D, Stunkard A, Sunderland T, Tibbits P, Jr, Valvo WJ. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Fann JR, Fan MY, Unutzer J. Improving primary care for older adults with cancer and depression. J Gen Intern Med. 2009;24(Suppl 2):S417–424. doi: 10.1007/s11606-009-0999-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow J. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30:112–126. doi: 10.1016/j.genhosppsych.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Fiorentino L, Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Med Rev. 2006;10:419–429. doi: 10.1016/j.smrv.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flint AJ, Rifat SL. Maintenance treatment for recurrent depression in late life. A four-year outcome study. Am J Geriat Psychiatry : official journal of the American Association for Geriatric Psychiatry. 2000;8:112–116. [PubMed] [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Fortner BV, Stepanski EJ, Wang SC, Kasprowicz S, Durrence HH. Sleep and quality of life in breast cancer patients. J Pain Symptom Manage. 2002;24:471–480. doi: 10.1016/s0885-3924(02)00500-6. [DOI] [PubMed] [Google Scholar]
- Fredericks CA, Drabant EM, Edge MD, Tillie JM, Hallmayer J, Ramel W, Kuo JR, Mackey S, Gross JJ, Dhabhar FS. Healthy young women with serotonin transporter SS polymorphism show a pro-inflammatory bias under resting and stress conditions. Brain Behav Immun. 2010;24:350–357. doi: 10.1016/j.bbi.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo JJ, Bogner HR, Morales KH, Post EP, Lin JY, Bruce ML. The effect of a primary care practice-based depression intervention on mortality in older adults: a randomized trial. Ann Intern Med. 2007;146:689–698. doi: 10.7326/0003-4819-146-10-200705150-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielissen MF, Verhagen S, Witjes F, Bleijenberg G. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24:4882–4887. doi: 10.1200/JCO.2006.06.8270. [DOI] [PubMed] [Google Scholar]
- Gimeno D, Kivimaki M, Brunner EJ, Elovainio M, De Vogli R, Steptoe A, Kumari M, Lowe GD, Rumley A, Marmot MG, Ferrie JE. Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychol Med. 2009;39:413–423. doi: 10.1017/S0033291708003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin JS, Zhang DD, Ostir GV. Effect of depression on diagnosis, treatment, and survival of older women with breast cancer. J Am Geriat Soc. 2004;52:106–111. doi: 10.1111/j.1532-5415.2004.52018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotay CC, Ransom S, Pagano IS. Quality of life in survivors of multiple primary cancers compared with cancer survivor controls. Cancer. 2007;110:2101–2109. doi: 10.1002/cncr.23005. [DOI] [PubMed] [Google Scholar]
- Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Critchley HD. Inflammation causes mood changes through alterations in subgenual cingulate activity and mesolimbic connectivity. Biol Psychiatry. 2009;66:407–414. doi: 10.1016/j.biopsych.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004;42:512–521. doi: 10.1097/01.mlr.0000127998.89246.ef. [DOI] [PubMed] [Google Scholar]
- Hogan D, Morrow JD, Smith EM, Opp MR. Interleukin-6 alters sleep of rats. J Neuroimmunol. 2003;137:59–66. doi: 10.1016/s0165-5728(03)00038-9. [DOI] [PubMed] [Google Scholar]
- Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, Moore J. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285:1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- Imeri L, Opp MR. How (and why) the immune system makes us sleep. Nat Rev Neurosci. 2009;10:199–210. doi: 10.1038/nrn2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin M, Rinetti G, Redwine L, Motivala S, Dang J, Ehlers C. Nocturnal proinflammatory cytokine-associated sleep disturbances in abstinent African American alcoholics. Brain Behav Immun. 2004;18:349–360. doi: 10.1016/j.bbi.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Irwin MR, Carrillo C, Olmstead R. Sleep loss activates cellular markers of inflammation: sex differences. Brain Behav Immun. 2010;24:54–57. doi: 10.1016/j.bbi.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Cole JC, Nicassio PM. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychol. 2006a;25:3–14. doi: 10.1037/0278-6133.25.1.3. [DOI] [PubMed] [Google Scholar]
- Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nature Rev Immunol. 2011a;11:625–632. doi: 10.1038/nri3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Olmstead R. Mitigating cellular inflammation in older adults. Am J Geriatr Psychiatry. 2011b doi: 10.1097/JGP.0b013e3182330fd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Olmstead R, Valladares EM, Breen EC, Ehlers CL. Tumor necrosis factor antagonism normalizes rapid eye movement sleep in alcohol dependence. Biol Psychiatry. 2009;66:191–195. doi: 10.1016/j.biopsych.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin MR, Wang M, Campomayor CO, Collado-Hidalgo A, Cole S. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med. 2006b;166:1756–1762. doi: 10.1001/archinte.166.16.1756. [DOI] [PubMed] [Google Scholar]
- Irwin MR, Wang M, Ribeiro D, Cho HJ, Olmstead R, Breen EC, Martinez-Maza O, Cole S. Sleep loss activates cellular inflammatory signaling. Biol Psychiatry. 2008;64:538–540. doi: 10.1016/j.biopsych.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kangas M, Henry JL, Bryant RA. The course of psychological disorders in the 1st year after cancer diagnosis. J Consult Clin Psychol. 2005;73:763–768. doi: 10.1037/0022-006X.73.4.763. [DOI] [PubMed] [Google Scholar]
- Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441:431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Alstein LL, Olmstead RE, Ercoli LM, Riparetti-Brown M, St Cyr N, Irwin MR. Complementary use of Tai Chi Chih augments escitalopram treatment of geriatric depression: a randomized controlled trial. Am J Geriatr Psychiatry : official journal of the American Association for Geriatric Psychiatry. 2011 doi: 10.1097/JGP.0b013e31820ee9ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman MD, Eisenberger NI. Neuroscience. Pains and pleasures of social life Science. 2009;323:890–891. doi: 10.1126/science.1170008. [DOI] [PubMed] [Google Scholar]
- Liu L, Mills PJ, Rissling M, Fiorentino L, Natarajan L, Dimsdale JE, Sadler GR, Parker BA, Ancoli-Israel S. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun. 2012a doi: 10.1016/j.bbi.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Rissling M, Natarajan L, Fiorentino L, Mills P, Dimsdale J, Sadler G, Parker B, Ancoli-Israel S. The longitudinal relationship between fatigue and sleep in breast cancer patients undergoing chemotherapy. Sleep. 2012b;35:237–245. doi: 10.5665/sleep.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhusudan S, Foster M, Muthuramalingam SR, Braybrooke JP, Wilner S, Kaur K, Han C, Hoare S, Balkwill F, Talbot DC, Ganesan TS, Harris AL. A phase II study of etanercept (Enbrel), a tumor necrosis factor alpha inhibitor in patients with metastatic breast cancer. Clin Cancer Res. 2004;10:6528–6534. doi: 10.1158/1078-0432.CCR-04-0730. [DOI] [PubMed] [Google Scholar]
- Madhusudan S, Muthuramalingam SR, Braybrooke JP, Wilner S, Kaur K, Han C, Hoare S, Balkwill F, Ganesan TS. Study of etanercept, a tumor necrosis factor-alpha inhibitor, in recurrent ovarian cancer. J Clin Oncol. 2005;23:5950–5959. doi: 10.1200/JCO.2005.04.127. [DOI] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–216. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Schott LL, Bromberger J, Cyranowski J, Everson-Rose SA, Sowers MF. Associations between depressive symptoms and inflammatory/hemostatic markers in women during the menopausal transition. Psychosom Med. 2007;69:124–130. doi: 10.1097/01.psy.0000256574.30389.1b. [DOI] [PubMed] [Google Scholar]
- Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, Mullington JM. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- Miller AH, Ancoli-Israel S, Bower JE, Capuron L, Irwin MR. Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol. 2008;26:971–982. doi: 10.1200/JCO.2007.10.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills PJ, Ancoli-Israel S, Parker B, Natarajan L, Hong S, Jain S, Sadler GR, von Kanel R. Predictors of inflammation in response to anthracycline-based chemotherapy for breast cancer. Brain Behav Immun. 2008;22:98–104. doi: 10.1016/j.bbi.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills PJ, Parker B, Jones V, Adler KA, Perez CJ, Johnson S, Cohen-Zion M, Marler M, Sadler GR, Dimsdale JE, Ancoli-Israel S. The effects of standard anthracycline-based chemotherapy on soluble ICAM-1 and vascular endothelial growth factor levels in breast cancer. Clin Cancer Res. 2004;10:4998–5003. doi: 10.1158/1078-0432.CCR-0734-04. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- Monk JP, Phillips G, Waite R, Kuhn J, Schaaf LJ, Otterson GA, Guttridge D, Rhoades C, Shah M, Criswell T, Caligiuri MA, Villalona-Calero MA. Assessment of tumor necrosis factor alpha blockade as an intervention to improve tolerability of dose-intensive chemotherapy in cancer patients. J Clin Oncol. 2006;24:1852–1859. doi: 10.1200/JCO.2005.04.2838. [DOI] [PubMed] [Google Scholar]
- Motivala S, Irwin MR. Sleep and immunity: cytokine pathways linking sleep and health outcomes. Curr Dir Psychol Sci. 2007;16:21–25. [Google Scholar]
- Mullington J, Korth C, Hermann DM, Orth A, Galanos C, Holsboer F, Pollmächer T. Dose-dependent effects of endotoxin on human sleep. Am J Physiol Regul Integr Comp Physiol. 2000;278:R947–955. doi: 10.1152/ajpregu.2000.278.4.R947. [DOI] [PubMed] [Google Scholar]
- Munoz RF, Cuijpers P, Smit F, Barrera AZ, Leykin Y. Prevention of major depression. Annu Rev Clin Psychol. 2010;6:181–212. doi: 10.1146/annurev-clinpsy-033109-132040. [DOI] [PubMed] [Google Scholar]
- Musselman DL, Lawson DH, Gumnick JF, Manatunga AK, Penna S, Goodkin RS, Greiner K, Nemeroff CB, Miller AH. Paroxetine for the prevention of depression induced by high-dose interferon-alfa. NEJM. 2001a;344:961–966. doi: 10.1056/NEJM200103293441303. [DOI] [PubMed] [Google Scholar]
- Musselman DL, Miller AH, Porter MR, Manatunga AK, Gao F, Penna S, Pearce BD, Landry J, Glover S, McDaniel JS, Nemeroff CB. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry. 2001b;158:1252–1257. doi: 10.1176/appi.ajp.158.8.1252. [DOI] [PubMed] [Google Scholar]
- Mykletun A, Bjerkeset O, Dewey M, Prince M, Overland S, Stewart R. Anxiety, depression, and cause-specific mortality: the HUNT study. Psychosom Med. 2007;69:323–331. doi: 10.1097/PSY.0b013e31803cb862. [DOI] [PubMed] [Google Scholar]
- Newman AB, Spiekerman CF, Enright P, Lefkowitz D, Manolio T, Reynolds CF, Robbins J. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. J Am Geriatr Soc. 2000;48:115–123. doi: 10.1111/j.1532-5415.2000.tb03901.x. [DOI] [PubMed] [Google Scholar]
- Nicassio PM, Schuman C, Kim J, Cordova A, Weisman MH. Psychosocial factors associated with complementary treatment use in fibromyalgia. J Rheum. 1997;24:2008–2013. [PubMed] [Google Scholar]
- Nicklas BJ, Hsu FC, Brinkley TJ, Church T, Goodpaster BH, Kritchevsky SB, Pahor M. Exercise training and plasma C-reactive protein and interleukin-6 in elderly people. J Am Geriatr Soc. 2008;56:2045–2052. doi: 10.1111/j.1532-5415.2008.01994.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor MF, Motivala SJ, Valladares EM, Olmstead R, Irwin MR. Sex differences in monocyte expression of IL-6: role of autonomic mechanisms. Am J Physiol Reg Integ Comp Physiol. 2007;293:R145–151. doi: 10.1152/ajpregu.00752.2006. [DOI] [PubMed] [Google Scholar]
- Office of Cancer Survivorship. 2009. [Google Scholar]
- Onitilo AA, Nietert PJ, Egede LE. Effect of depression on all-cause mortality in adults with cancer and differential effects by cancer site. Gen Hosp Psych. 2006;28:396–402. doi: 10.1016/j.genhosppsych.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Pace TW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, Issa MJ, Raison CL. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrin. 2009;34:87–98. doi: 10.1016/j.psyneuen.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palesh OG, Roscoe JA, Mustian KM, Roth T, Savard J, Ancoli-Israel S, Heckler C, Purnell JQ, Janelsins MC, Morrow GR. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer. J Clin Oncol. 28:292–298. doi: 10.1200/JCO.2009.22.5011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirl WF, Greer JA, Traeger L, Jackson V, Lennes IT, Gallagher ER, Perez-Cruz P, Heist RS, Temel JS. Depression and survival in metastatic non-small-cell lung cancer. J Clin Oncol. 2012 doi: 10.1200/JCO.2011.38.3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky D, Doshi JA, Marcus S, Oslin D, Rothbard A, Thomas N, Thompson CL. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med. 2005;165:1260–1266. doi: 10.1001/archinte.165.11.1260. [DOI] [PubMed] [Google Scholar]
- Raison CL, Lowry CA, Rook GA. Inflammation, sanitation, and consternation: loss of contact with coevolved, tolerogenic microorganisms and the pathophysiology and treatment of major depression. Arch Gen Psychiatry. 2010;67:1211–1224. doi: 10.1001/archgenpsychiatry.2010.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raison CL, Miller AH. Depression in cancer: new developments regarding diagnosis and treatment. Biol Psychiatry. 2003;54:283–294. doi: 10.1016/s0006-3223(03)00413-x. [DOI] [PubMed] [Google Scholar]
- Raison CL, Rye DB, Woolwine BJ, Vogt GJ, Bautista BM, Spivey JR, Miller AH. Chronic interferon-alpha administration disrupts sleep continuity and depth in patients with hepatitis C: association with fatigue, motor slowing, and increased evening cortisol. Biol Psychiatry. 68:942–949. doi: 10.1016/j.biopsych.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redwine L, Dang J, Hall M, Irwin M. Disordered sleep, nocturnal cytokines, and immunity in alcoholics. Psychosom Med. 2003;65:75–85. doi: 10.1097/01.psy.0000038943.33335.d2. [DOI] [PubMed] [Google Scholar]
- Reynolds CF., 3rd Prevention of depressive disorders: a brave new world. Depress Anxiety. 2009;26:1062–1065. doi: 10.1002/da.20644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooney AG, McNamara S, Mackinnon M, Fraser M, Rampling R, Carson A, Grant R. Frequency, clinical associations, and longitudinal course of major depressive disorder in adults with cerebral glioma. J Clin Oncol. 2011;29:4307–4312. doi: 10.1200/JCO.2011.34.8466. [DOI] [PubMed] [Google Scholar]
- Roscoe JA, Morrow GR, Hickok JT, Mustian KM, Griggs JJ, Matteson SE, Bushunow P, Qazi R, Smith B. Effect of paroxetine hydrochloride (Paxil) on fatigue and depression in breast cancer patients receiving chemotherapy. Breast Cancer Res Treat. 2005;89:243–249. doi: 10.1007/s10549-004-2175-1. [DOI] [PubMed] [Google Scholar]
- Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001a;19:895–908. doi: 10.1200/JCO.2001.19.3.895. [DOI] [PubMed] [Google Scholar]
- Savard J, Simard S, Blanchet J, Ivers H, Morin CM. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001b;24:583–590. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- Schag CA, Ganz PA, Polinsky ML, Fred C, Hirji K, Petersen L. Characteristics of women at risk for psychosocial distress in the year after breast cancer. J Clin Oncol. 1993;11:783–793. doi: 10.1200/JCO.1993.11.4.783. [DOI] [PubMed] [Google Scholar]
- Schoevers RA, Smit F, Deeg DJ, Cuijpers P, Dekker J, van Tilburg W, Beekman AT. Prevention of late-life depression in primary care: do we know where to begin? Am J Psychiatry. 2006;163:1611–1621. doi: 10.1176/ajp.2006.163.9.1611. [DOI] [PubMed] [Google Scholar]
- Seruga B, Zhang H, Bernstein LJ, Tannock IF. Cytokines and their relationship to the symptoms and outcome of cancer. Nature Rev Cancer. 2008;8:887–899. doi: 10.1038/nrc2507. [DOI] [PubMed] [Google Scholar]
- Shearer WT, Reuben JM, Mullington JM, Price NJ, Lee BN, Smith EO, Szuba MP, Van Dongen HP, Dinges DF. Soluble TNF-alpha receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J Allergy Clin Immunol. 2001;107:165–170. doi: 10.1067/mai.2001.112270. [DOI] [PubMed] [Google Scholar]
- Silberfarb PM, Hauri PJ, Oxman TE, Schnurr P. Assessment of sleep in patients with lung cancer and breast cancer. J Clin Oncol. 1993;11:997–1004. doi: 10.1200/JCO.1993.11.5.997. [DOI] [PubMed] [Google Scholar]
- Soygur H, Palaoglu O, Akarsu ES, Cankurtaran ES, Ozalp E, Turhan L, Ayhan IH. Interleukin-6 levels and HPA axis activation in breast cancer patients with major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1242–1247. doi: 10.1016/j.pnpbp.2007.05.001. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Giese-Davis J. Depression and cancer: mechanisms and disease progression. Biol Psychiatry. 2003;54:269–282. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- Steel JL, Geller DA, Gamblin TC, Olek MC, Carr BI. Depression, immunity, and survival in patients with hepatobiliary carcinoma. J Clin Oncol. 2007;25:2397–2405. doi: 10.1200/JCO.2006.06.4592. [DOI] [PubMed] [Google Scholar]
- Stein BD, Meili R, Klein D. Datapoints: general medical costs of recipients of behavioral health care. Psychiatr Serv. 2006;57:620. doi: 10.1176/ps.2006.57.5.620. [DOI] [PubMed] [Google Scholar]
- Stein KD, Jacobsen PB, Hann DM, Greenberg H, Lyman G. Impact of hot flashes on quality of life among postmenopausal women being treated for breast cancer. J Pain Symptom Manage. 2000;19:436–445. doi: 10.1016/s0885-3924(00)00142-1. [DOI] [PubMed] [Google Scholar]
- Stommel M, Given BA, Given CW. Depression and functional status as predictors of death among cancer patients. Cancer. 2002;94:2719–2727. doi: 10.1002/cncr.10533. [DOI] [PubMed] [Google Scholar]
- Su S, Zhao J, Bremner JD, Miller AH, Tang W, Bouzyk M, Snieder H, Novik O, Afzal N, Goldberg J, Vaccarino V. Serotonin transporter gene, depressive symptoms, and interleukin-6. Circ Cardiovasc Genet. 2009;2:614–620. doi: 10.1161/CIRCGENETICS.109.870386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyring S, Gottlieb A, Papp K, Gordon K, Leonardi C, Wang A, Lalla D, Woolley M, Jahreis A, Zitnik R, Cella D, Krishnan R. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet. 2006;367:29–35. doi: 10.1016/S0140-6736(05)67763-X. [DOI] [PubMed] [Google Scholar]
- Uher R, McGuffin P. The moderation by the serotonin transporter gene of environmental adversity in the aetiology of mental illness: review and methodological analysis. Mol Psychiatry. 2008;13:131–146. doi: 10.1038/sj.mp.4002067. [DOI] [PubMed] [Google Scholar]
- Vgontzas AN, Papanicolaou DA, Bixler EO, Lotsikas A, Zachman K, Kales A, Prolo P, Wong ML, Licinio J, Gold PW, Hermida RC, Mastorakos G, Chrousos GP. Circadian interleukin-6 secretion and quantity and depth of sleep. J Clin Endocrin Metab. 1999;84:2603–2607. doi: 10.1210/jcem.84.8.5894. [DOI] [PubMed] [Google Scholar]
- Vos T, Haby MM, Barendregt JJ, Kruijshaar M, Corry J, Andrews G. The burden of major depression avoidable by longer-term treatment strategies. Arch Gen Psychiatry. 2004;61:1097–1103. doi: 10.1001/archpsyc.61.11.1097. [DOI] [PubMed] [Google Scholar]
- Wang XS, Shi Q, Williams LA, Mao L, Cleeland CS, Komaki RR, Mobley GM, Liao Z. Inflammatory cytokines are associated with the development of symptom burden in patients with NSCLC undergoing concurrent chemoradiation therapy. Brain Behav Immun. 2010;24:968–974. doi: 10.1016/j.bbi.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Nicassio P, Tennen H, Finan P, Kratz A, Parrish B, Irwin MR. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J Consult Clin Psychol. 2008;76:408–421. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]