Abstract
Objective
We wanted to assess the trends of CT examinations that were conducted in an adult emergency department (ED).
Materials and Methods
We searched the medical database to identify adult patients (≥ 18 years) who had visited the ED and the number of CT examinations of the patients during the period from January 2001 to December 2010. We also analyzed the types of CT scans performed in terms of body parts, they were as follows; head CTs, facial bone CTs, neckl CTs, chest CTs, abdominal CTs, and miscellaneous CTs. Further, miscellaneous CTs were subdivided as CT angiography and others.
Results
A total of 113656 CT scans were examined for 409439 adult ED patients during a 10-year period, and the number of CT scans increased by 255% (from 4743 CTs in 2001 to 16856 CTs in 2010), while the adult ED patient volume increased by 34% during the same period. Although the head CTs proportionally occupied the most, the facial bone CTs had the largest rate of increase (3118%), followed by cervical CTs (1173%), chest CTs (455%), miscellaneous CTs (388%; 862% and 84% for CT angiography and others, respectively), abdominal CTs (315%) and head CTs (95%) per 1000 patients during the decade.
Conclusion
CT use in adult ED has increased at a rate that far exceeds the growth of ED patient volume, with facial bone CTs and cervical CTs having the largest increasing rate, followed by chest CTs, miscellaneous CTs, abdominal CTs and head CTs.
Keywords: Computed tomography, Utilization, Adult, Emergency department
INTRODUCTION
Several studies from Western countries showed a steady increase in the use of computed tomography (CT) examinations in the emergency department (ED) with the need for rapid and accurate diagnosis, as well as the trend toward less invasive diagnostic testing (1-5). However, CT becomes a source of concern to the medical community from the perspective of increased cost and radiation dose to the patient population. For these reasons, detailed analysis of CT utilization pattern, in the clinical practice, may be valuable. This is the first report regarding the trends of CT examinations for adult patients in a Korean ED.
MATERIALS AND METHODS
The institutional review board of our hospital approved this retrospective study and the requirement for informed patient consent was waived.
Study Population
We searched the Gachon University Gil Hospital Emergency Center Database (GUGHEC database) to identify all the adult patients (≥ 18 years) who visited the ED between January 2001 and December 2010. Using the radiology database, we identified the CT scans performed on adult ED patients during the same period. CT scan data was also stratified by age of patients into two groups: ≤ 40 years of age and > 40 years of age.
CT Scans
In our hospital, a multi-detector CT (Somatom Sensation 16 scanner, Siemens Medical Solutions, Forchbeim, Germany) has been exclusively used for ED patients, since March 2005. Before March 2005, a single-spiral CT (Somatom Plus Four Expert, Siemens Medical Solutions, Forchbeim, Germany) was used for the ED patients. The CT scans were categorized by body regions into six groups (head, facial bone, cervical, chest, abdomen and miscellaneous). Facial bone CTs included facial bone, orbit, mandible and paranasal sinus. Chest CTs included pulmonary CT angiographies, pre-contrast and post-contrast chest CTs. The abdominal CTs included only the abdomen CTs, as well as the abdomen and pelvic CTs. Miscellaneous CTs contained various uncommon CT scans (CTs of the thoracic or lumbar spine and extremities) and CT angiographies except pulmonary CT angiography.
Methods of Assessment
We assessed the total number of patients and the number of CT examinations for the adult patients who visited ED, and we calculated the rate of CT examinations per every 1000 patients. The increased rates of CT scans, as classified by the body part from the initial year (2001 year), were also calculated as follows.
The increased rate of CT scans from the year 2001 = (number of CTs per 1000 patients in the year - number of CTs per 1000 patients in 2001 year) / number of CTs per 1000 patients in 2001 year
Using the GUGHEC and radiology database, we also determined the number of patients who had received multiple CT examinations on the day of admission and the reasons for the examinations.
Statistical Analysis
Standard descriptive statistical methods were performed with Microsoft Excel 2007 (Microsoft, Redmond, WA, USA).
RESULTS
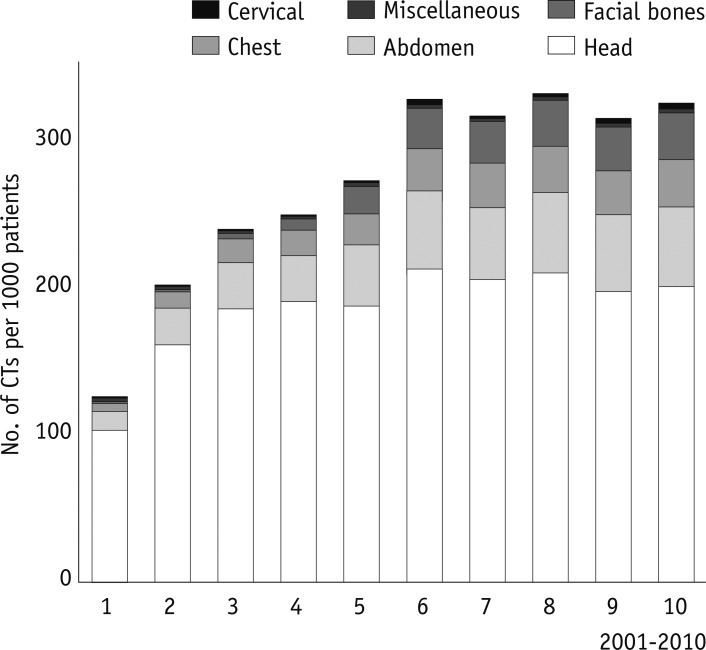
A total of 409439 adult patients (214213 men and 195226 women, mean age: 47 years) visited our ED during a 10 year period. A total of 113656 CT examinations were performed on 95271 patients (51754 men and 43517 women, mean age: 50 years), for an increase of 255% (from 4743 CTs in 2001 to 16856 CTs in 2010), while the adult ED patients' volume increased by 34% (38209 in 2001 to 51030 in 2010), during the study period. Overall, the number of CT examinations far exceeded the increasing rate of patients: the CT scans per every 1000 patients increased from 124 CTs in 2001 to 330 CTs in 2010 (Fig. 1).
Fig. 1.
Total number of CT scans performed for adult patients who visited emergency department for previous decade. CT scans per every 1000 patients increased from 124 CTs in 2001 to 330 CTs in 2010.
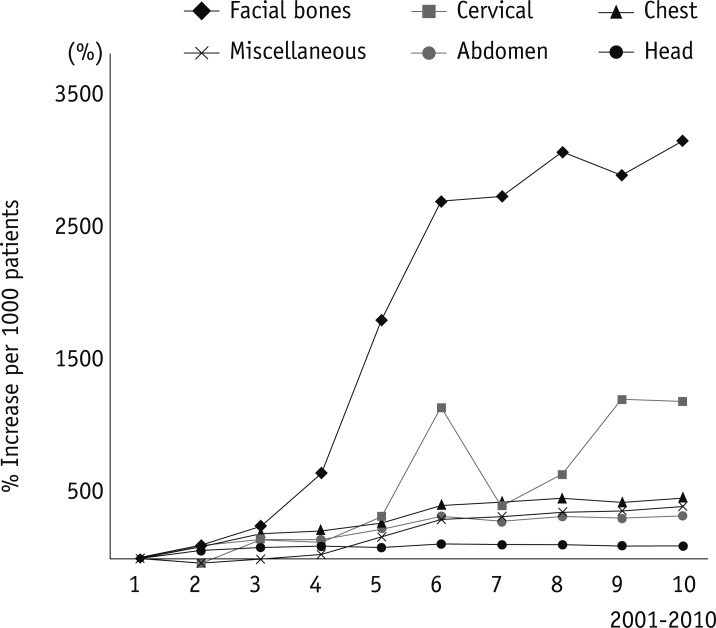
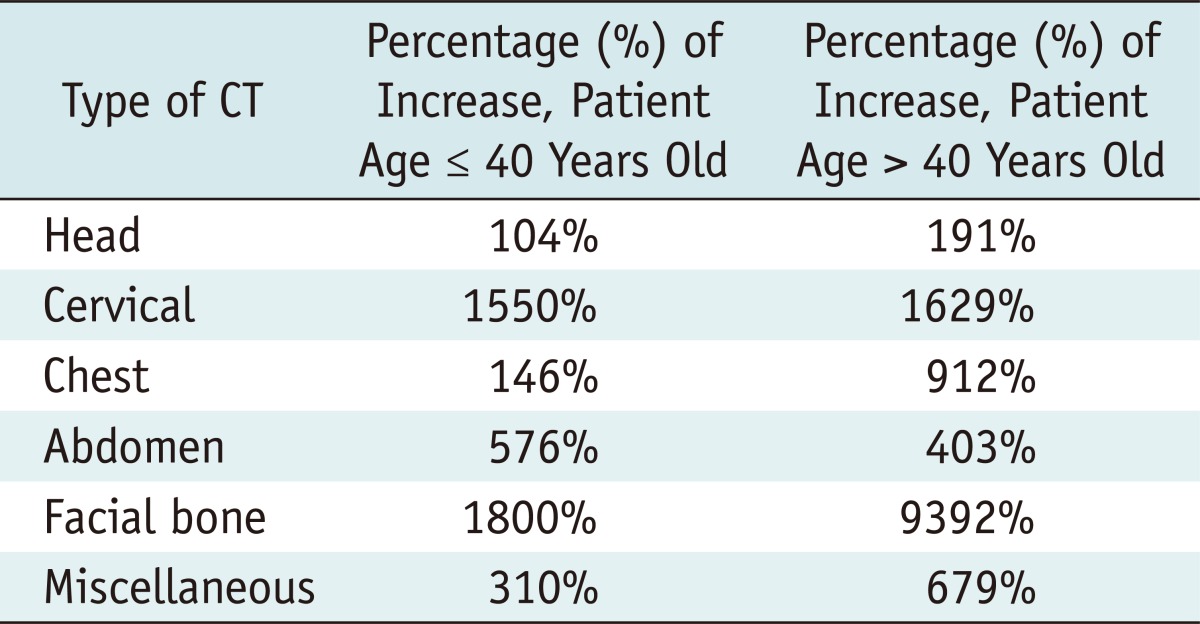
In terms of the CT types by anatomic regions, head CTs (67.5%) and abdominal CTs (14.8%) occupied the majority of the total scans, followed by chest CTs (8.1%), facial bone CTs (6.6%), miscellaneous CTs (1.5% and 0.9% for CT angiographies and et cetera, respectively) and cervical CTs (0.6%) (Fig. 1). Although the head CTs occupied proportionally the most, facial bone CTs revealed the largest rate of increase (3118%), followed by cervical CTs (1173%) and chest CTs (455%), miscellaneous CTs (388%), abdominal CTs (315%) and head CTs (95%), per 1000 patients for a decade (Fig. 2). Among the miscellaneous CT, CT angiographies showed increased rate of 862% per 1000 patients for a decade. The increase of CT examination occurred in both patients, younger and older than 40 years old (Table 1). The rate of increase for abdomen CTs was greater in younger patients, while the others were greater in patients older than 40 years old.
Fig. 2.
Increase rate of CT examinations by anatomic region for previous decade. Compared with 2001 years, facial bone CTs shows largest rate of increase (3118%), followed by cervical CTs (1173%), chest CTs (455%), and miscellaneous CTs (388%; 862% and 84% for CT angiographies and et cetera, respectively), abdominal CTs (315%), and head CTs (95%) per 1000 patients.
Table 1.
Percent Increast in CT Utilization in Emergency Department during 2000-2010 by Patient Age
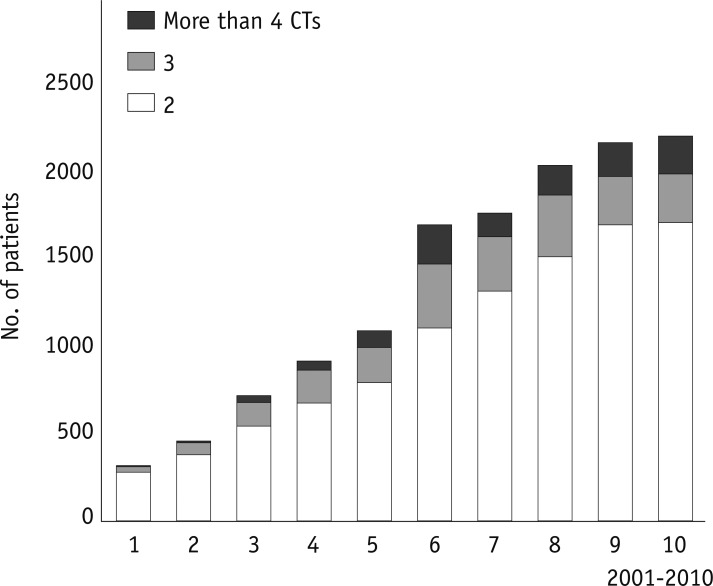
Of a total of 95271 adult patients, who had CT examinations in the ED, 14.0% (n = 13300) had multiple CT examinations on the admission day (Fig. 3). The most common reason for multiple CT examinations was the evaluation for traumatic injuries (81%), fever focus (10%), insufficient clinical assessment (6%) caused by impaired cognitive function for old age or abnormal mentality, and et cetera (3%).
Fig. 3.
Number of patients who had multiple CT examinations.
DISCUSSION
Similar with a few reports from Western countries, our study also shows that CT use has grown than the growth of patient volume for the past decade, although, the rate of increase varies with the particular body region imaged. Furthermore, the increase has occurred in both younger and older adults.
In terms of the CT scans, as classified by body parts, the facial bone CTs showed the largest rate of increase (3118%), followed by cervical CTs (1173%), chest CTs (455%), miscellaneous CTs (388%), abdominal CTs (315%) and head CTs (95%). Compared with the previous studies that revealed chest CTs and cervical CTs as showing a greatest increase (600% and 500% increase, respectively by Lee et al. and 226% and 463%, respectively by Broder et al.) (2, 5), the dramatic increase of facial bone CTs in our study seems to be an interesting aspect worth noting. The increase rate of each CT scans may reflect the disease prevalence of the patients, and the reasoning of physicians who order the test. However, the increased use of facial bone CTs, as well as cervical CTs, may not be surprising because recent studies have questioned the use of plain radiographs in the evaluation of traumatic injuries, as a standard of care for their inferior diagnostic accuracy (6-8). CT imaging in these patients helps in the assessment of multiple bone fractures, and allows the surgeon to make proper planning before a surgical procedure.
The factors that promote the utility of CT include the increasing availability of CT scanners and the technological improvements in the efficiency of a scanner and image resolution with the introduction of multi-detector CT (MDCT), the cost and time benefits from the improved diagnosis (9-11). Since March 2005, when the MDCT was first introduced in our ED, the number of CT examination showed a rapid increase, compared with the previous years (Fig. 1). The number of patients who had multiple CT examinations on the same day and the number of CT angiographic examinations were also markedly increased since the time. With MDCT scanners, the acquisition of multi-planar reconstruction and sub-millimeter resolution images of the entire body is possible in a matter of seconds, and as a noninvasive diagnostic modality, MDCT has become a vital component in the ED (12).
Computed tomography examinations provide a significant source of radiation exposure. The radiation from a single CT scan ranges from 2 to 31 mSv, depending on the patient's age and the irradiated body organ (13). Although the radiation induced cancer risk has been revealed to be relatively low by CT examinations (relative risk = 0.035, mortality = 0.1-0.12% in individual patients in high-risk of death from a cancer), patients could potentially be at higher risk for recurrent and cumulative CT examinations (14, 15). While our study did not directly address the issue of medical appropriateness and radiation hazard, the increasing use of CT in the ED raises the question of whether the increasing utility of CT scans is moving toward an appropriate rate or if it has moved beyond it.
Although our data show a substantial increase for the past 10 years, they also showed the tapered increase of CT use since 2007, that is similar with those of Levin et al. (16) who found that the rates of all types of imaging in the outpatient setting began to decline in 2006. Levin et al. (16, 17) have described the increased number of radiology benefit management companies, the dissemination of appropriateness criteria by major medical societies and the effects of decreased reimbursement imposed in compliance with the Deficit Reduction Act of 2005, as the reason of the decreasing growth of performing imaging.
This study had several limitations. First, as a retrospective study, data could have been missing from the GUGHEC and radiology database. Second, our study was a single institution's results. However, as a south sea regional representative emergency medical center and one of the largest EDs in Korea, in terms of the number of visited patients, our data might reflect the national trend of ED, in Korea. Third, we did not specifically evaluate the clinical usefulness or radiation hazards from CT examinations for the patients. However, the primary objective of this study was to analyze the trends of CT usage in an adult ED of Korea.
Despite the limitations, our study is the first report on the trends of CT use in an adult Korean ED. We revealed the increased rate of CT scans has outpaced the increase of the ED patient volume for the previous decade, with facial bone CTs and cervical CTs being increased the most, followed by chest CTs, miscellaneous CTs (CT angiographies and et cetera), abdominal CTs and head CTs. The increased rates of CT examinations raise the question concerning the appropriateness of these examinations due to both the advantages (a rapid and accurate diagnosis) and disadvantages (increased radiation exposure and medical cost).
References
- 1.Brody AS, Seidel FG, Kuhn JP. CT evaluation of blunt abdominal trauma in children: comparison of ultrafast and conventional CT. AJR Am J Roentgenol. 1989;153:803–806. doi: 10.2214/ajr.153.4.803. [DOI] [PubMed] [Google Scholar]
- 2.Broder J, Warshauer DM. Increasing utilization of computed tomography in the adult emergency department, 2000-2005. Emerg Radiol. 2006;13:25–30. doi: 10.1007/s10140-006-0493-9. [DOI] [PubMed] [Google Scholar]
- 3.Boone JM, Brunberg JA. Computed tomography use in a tertiary care university hospital. J Am Coll Radiol. 2008;5:132–138. doi: 10.1016/j.jacr.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaewlai R, Avery LL, Asrani AV, Novelline RA. Multidetector CT of blunt thoracic trauma. Radiographics. 2008;28:1555–1570. doi: 10.1148/rg.286085510. [DOI] [PubMed] [Google Scholar]
- 5.Lee J, Kirschner J, Pawa S, Wiener DE, Newman DH, Shah K. Computed tomography use in the adult emergency department of an academic urban hospital from 2001 to 2007. Ann Emerg Med. 2010;56:591–596. doi: 10.1016/j.annemergmed.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 6.Tanrikulu R, Erol B. Comparison of computed tomography with conventional radiography for midfacial fractures. Dentomaxillofac Radiol. 2001;30:141–146. doi: 10.1038/sj/dmfr/4600593. [DOI] [PubMed] [Google Scholar]
- 7.Reuben AD, Watt-Smith SR, Dobson D, Golding SJ. A comparative study of evaluation of radiographs, CT and 3D reformatted CT in facial trauma: what is the role of 3D? Br J Radiol. 2005;78:198–201. doi: 10.1259/bjr/26977910. [DOI] [PubMed] [Google Scholar]
- 8.Bailitz J, Starr F, Beecroft M, Bankoff J, Roberts R, Bokhari F, et al. CT should replace three-view radiographs as the initial screening test in patients at high, moderate, and low risk for blunt cervical spine injury: a prospective comparison. J Trauma. 2009;66:1605–1609. doi: 10.1097/TA.0b013e3181a5b0cc. [DOI] [PubMed] [Google Scholar]
- 9.Flohr TG, Schaller S, Stierstorfer K, Bruder H, Ohnesorge BM, Schoepf UJ. Multi-detector row CT systems and image-reconstruction techniques. Radiology. 2005;235:756–773. doi: 10.1148/radiol.2353040037. [DOI] [PubMed] [Google Scholar]
- 10.Baker LC, Atlas SW, Afendulis CC. Expanded use of imaging technology and the challenge of measuring value. Health Aff (Millwood) 2008;27:1467–1478. doi: 10.1377/hlthaff.27.6.1467. [DOI] [PubMed] [Google Scholar]
- 11.Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP. National trends in CT use in the emergency department: 1995-2007. Radiology. 2011;258:164–173. doi: 10.1148/radiol.10100640. [DOI] [PubMed] [Google Scholar]
- 12.Kock MC, Adriaensen ME, Pattynama PM, van Sambeek MR, van Urk H, Stijnen T, et al. DSA versus multi-detector row CT angiography in peripheral arterial disease: randomized controlled trial. Radiology. 2005;237:727–737. doi: 10.1148/radiol.2372040616. [DOI] [PubMed] [Google Scholar]
- 13.Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–2086. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology. 2004;232:735–738. doi: 10.1148/radiol.2323031095. [DOI] [PubMed] [Google Scholar]
- 15.Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251:175–184. doi: 10.1148/radiol.2511081296. [DOI] [PubMed] [Google Scholar]
- 16.Levin DC, Rao VM, Parker L. Physician orders contribute to high-tech imaging slowdown. Health Aff (Millwood) 2010;29:189–195. doi: 10.1377/hlthaff.2009.0528. [DOI] [PubMed] [Google Scholar]
- 17.Levin DC, Bree RL, Rao VM, Johnson J. A prior authorization program of a radiology benefits management company and how it has affected utilization of advanced diagnostic imaging. J Am Coll Radiol. 2010;7:33–38. doi: 10.1016/j.jacr.2009.09.012. [DOI] [PubMed] [Google Scholar]