Abstract
Context:
Several factors have been associated with the development of osteoarthritis after anterior cruciate ligament (ACL) reconstruction, yet little attention has been given to the association between range of motion (ROM) and osteoarthritis after ACL reconstruction. Several studies have shown a link between ROM loss and a higher incidence of osteoarthritis.
Evidence Acquisition:
A search was performed with PubMed (MEDLINE) for English-language level I-IV studies involving the long-term evaluation of ROM and osteoarthritis after ACL reconstruction. Keywords were osteoarthritis, anterior cruciate ligament, and range of motion.
Results:
Six studies considered whether ROM was a factor in association with osteoarthritis after ACL reconstruction: In 3 of these studies, an association was found between loss of knee motion and the development of osteoarthritis, while the other 3 studies failed to identify a significant association. Two studies identified an association between ROM loss and decreased subjective outcomes after ACL reconstruction.
Conclusions:
Previous studies have shown an association between loss of knee ROM and osteoarthritic changes on radiographs in the long term after ACL reconstruction. Loss of ROM and osteoarthritis are also associated with lower subjective scores. Other factors related to osteoarthritis, such as meniscal and articular cartilage status, cannot be modified, but through implementation of a directed rehabilitation program before and after ACL surgery, the achievement of full symmetric ROM can be promoted. More emphasis needs to be placed on careful and precise examination of knee ROM, as well as rehabilitation to achieve and maintain full symmetric ROM in the long term after ACL reconstruction.
Keywords: range of motion, anterior cruciate ligament reconstruction, osteoarthritis
In the recent literature, there has been an increasing amount of attention given to the development of osteoarthritis (OA) after anterior cruciate ligament (ACL) reconstruction.†
Concomitant injuries affecting the menisci or articular cartilage are commonly accepted as predisposing factors of future OA‡; however, few studies8,18,21,22,28 have included range of motion (ROM) loss in a regression model looking at potential factors associated with OA after ACL reconstruction. Results of these studies are mixed, with some showing an association between ROM loss and the development of OA22,28 and with others8,18,21 showing no significant relationship.
Two studies have found an association between loss of knee ROM and decreased subjective results after ACL reconstruction,11,26 but is it possible that loss of ROM after ACL reconstruction may lead to the development of OA? This factor is important because it may be controlled by implementing better pre- and postoperative rehabilitation programs and ensuring that surgical techniques do not “capture the knee,” cause impingement, or restrict rehabilitation unnecessarily. In comparison with factors such as associated injuries to the menisci or articular cartilage, which are not modifiable factors, obtaining full ROM of the knee is a relatively easy and low-cost method of improving short- and long-term outcomes after ACL reconstruction.2,26
This has been a challenging topic to research because to understand the true incidence of OA after ACL reconstruction, comprehensive objective follow-up of all ACL patients over a long period is required. Studies with the “standard” 2-year follow-up time frame simply do not follow patients for a duration long enough to detect arthritic changes and evaluate the associated symptoms. Furthermore, there are several ways to evaluate and categorize arthritic changes in the knee joint, as well as a wide variation in the surgical and rehabilitation techniques utilized after ACL reconstruction. Many studies do not examine ROM loss as a possible factor associated with the development of OA after ACL reconstruction, and there is little to no consistency in regard to the definition of full ROM and the methods for measuring it. Each of these factors makes it difficult to formulate conclusions in this area.
The purpose of this review is to summarize the current literature regarding the association between loss of knee ROM and the development of OA after ACL reconstruction.
What is “Normal” Knee ROM?
Subtle degrees of ROM loss, as small as 3° of extension compared with the opposite knee, have been linked to lower subjective and objective results after ACL surgery.26 This trend becomes even more pronounced when articular cartilage or meniscal damage is also present in the knee.26 To detect knee motion loss, the ROM of both knees needs to be critically assessed.
It may seem like a simple question, but what is “normal” knee ROM? As an example, one orthopaedic textbook defines it as 0° of extension and 135° of flexion, although the author notes that extension may go up to 15° of hyperextension, especially in women.14
This can be problematic in clinical practice. Based on this definition, a patient could be considered back to normal knee motion after ACL reconstruction when he or she reaches 0° of knee extension and 135° of knee flexion. However, what if the patient’s opposite, normal knee has 10° of hyperextension and 155° of flexion? The patient certainly would not feel like the ACL knee is back to “normal” if the opposite knee has 10 additional degrees of extension and 20 additional degrees of flexion. Consequently, we would argue that normal ROM is unique to each patient; therefore, normal ROM should be based on the available ROM in the opposite, noninjured knee. In some instances, the opposite knee may not be normal and may also have limited ROM, which makes determining the goals for ROM more difficult. However, the point remains that some amount of knee hyperextension is common and the goals for physical therapy should not be merely based on achieving 0° of extension. When both knees have limited ROM, attempts should be made to achieve knee hyperextension. Although the end goal may not be as clearly defined, work to maximize ROM of both knees until the patient reaches a plateau; do not stop simply because 0° of extension is achieved.
How to Accurately Measure Knee Extension and Flexion
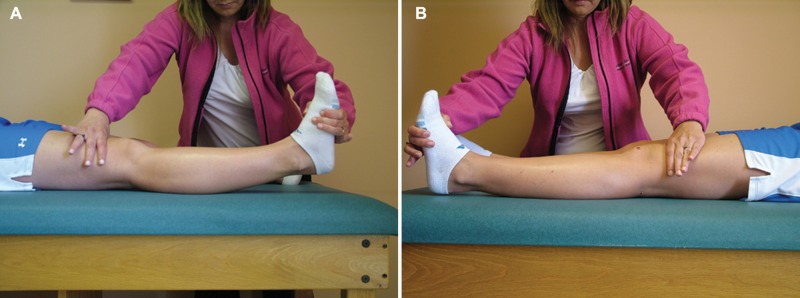
To assess knee extension, we recommend beginning with a passive knee extension assessment first: Place one hand above the knee to stabilize the femur while grasping the forefoot with the other hand; then passively extend the knee by lifting the foot while stabilizing the femur on the table. Do this on the noninvolved knee first. Afterward, compare the amount of movement available and the quality of the end feel to the opposite knee (Figure 1A and 1B). This method of assessing knee extension is used in conjunction with goniometric measurements as a way to detect a tight end feel that may be too subtle to be captured with a goniometric measurement. This technique also allows the patient to kinesthetically feel the difference between the amount of extension in one knee compared with the other.
Figure 1.
Assessment of passive knee extension is performed by stabilizing the femur on the examination table with one hand while using the other hand to grasp the forefoot and lift upward. The amount of extension and/or hyperextension can be assessed kinesthetically and visually to detect side-to-side differences. The amount of knee extension available in the noninvolved, normal knee (A) compared with the loss of extension in the involved knee (B).
To measure knee extension with a goniometer, have the patient lie supine with both heels propped on a bolster high enough to allow the knees to fall into hyperextension. First, perform a visual assessment of the position of the knees. Do they both fall into hyperextension? Are they level, or is one knee higher than the other, indicating a loss of extension ROM compared with the opposite side (Figure 2)? Next, measure the knee extension with a long-arm goniometer, lining the axis up with the joint line, the proximal arm with the middle of the greater trochanter, and the distal arm with the middle of the lateral malleolus.
Figure 2.

Position used for measuring knee extension with a goniometer and for visually detecting any difference in the amount of knee extension. This picture shows a slight loss of extension in the left knee.
Note that hyperextension of the knee is normal. DeCarlo and Sell4 found that some degree of hyperextension is present in 95% of men and 96% of women, with the mean being 5° and 6°, respectively.
We recommend that ROM be recorded using the A-B-C format, with A representing the degree of hyperextension; B, the degree short of 0° of extension; and C, the degree of flexion. With this format, the ROM of a knee with 5° of hyperextension and 155° of flexion would be recorded as 5-0-155. If the knee was lacking 5° of extension and had 155° of flexion, the ROM would be recorded as 0-5-155. This method of recording knee ROM is beneficial because it eliminates the use of negative numbers. A negative number for extension could indicate extension loss or hyperextension. The A-B-C format eliminates this potential source of confusion.
If ROM was consistently evaluated with this level of scrutiny, a slight loss of motion could be detected and treated sooner, which should increase the likelihood of regaining full symmetric ROM. Without measuring and recording ROM in this manner, knee ROM could easily be overlooked as a potential risk factor for the development of OA.
Achieving Full Symmetric ROM After ACL Injury and Surgery
Achieving full symmetric ROM in the early time frame after ACL surgery is paramount to allow patients to regain and maintain good ROM in the long term.2,15 Several key factors should be incorporated into the ACL reconstruction process to ensure that full symmetric ROM is achieved: preoperative rehabilitation, timing of surgery, surgical technique, prevention of a hemarthrosis after surgery, and appropriate and immediate postoperative rehabilitation.
After an ACL tear, an effusion and loss of knee extension and flexion occur. A directed rehabilitation program should be designed to eliminate the effusion and restore full symmetric knee extension and flexion. The effusion is treated with elevation of the knee above the level of the heart and the use of a cold/compression device. The initial goal is to regain symmetric knee extension through the use of the towel stretch (Figure 3), heel prop (Figure 4), and prone hang exercises. Occasionally, knee extension is initially limited because a portion of the torn ACL is stuck in the intercondylar notch, blocking extension. By performing exercises to achieve terminal extension, the ACL stump is forced out of the intercondylar notch, making it easier to achieve full symmetric extension. This also results in increased comfort to the patient and improved gait. A passive knee extension device can be a helpful adjunct to the knee extension exercises to achieve the goal of full symmetric knee extension (Figure 5).
Figure 3.

The towel stretch exercise is performed by using one hand to stabilize the thigh on the table while the other hand pulls upward on the towel to stretch the knee into hyperextension.
Figure 4.

The heel prop exercise is a low-load, long-duration stretch performed with the patient lying supine and the heels propped on a bolster high enough to allow the knees to fall into hyperextension. Light ankle weights may be placed over the leg proximal and distal to the knee to increase the intensity of the stretch.
Figure 5.

The passive knee extension device is used to provide a low-load, long-duration stretch to the knee.
Once knee extension is full and symmetric to the opposite knee, the focus shifts to working on knee flexion. A heel slide exercise can be done to improve knee flexion (Figure 6). The presence of an effusion can limit the amount of knee flexion available, so efforts to reduce the effusion should also continue until the effusion is resolved. Most patients find it more comfortable to hold the knee in a slightly flexed position when an effusion is present, which may lead to the development of a flexion contracture, but note that full knee extension is achievable even when an effusion is present.
Figure 6.

The heel slide exercise is done to increase knee flexion.
Patients are also encouraged to use the ACL-injured knee normally to avoid perpetuating any strength or ROM loss because of disuse. If the patient desires to return to sports or activities that involve cutting, pivoting, or change of direction, an ACL reconstruction is recommended to allow participation without instability. Prior to surgery, the patient needs to meet the following goals: no effusion, full symmetric knee extension, full symmetric knee flexion, and normal gait pattern. The risk of developing postoperative ROM limitations is greatly reduced by delaying surgery until these goals are achieved and the knee has returned to quiescent state.15,29
A desirable ACL reconstruction technique is one that eliminates the problem of knee instability without “capturing the knee” or causing graft impingement and allows for postoperative rehabilitation without restrictions in weightbearing status or ROM.
Prevention of a hemarthrosis postoperatively is important for pain control and regaining ROM.27 To achieve this goal, patients remain in antiembolism stockings, a continuous passive motion machine for elevation of the knee above the heart, and a cold/compression device for the first 5 to 7 days after surgery. During the first postoperative week, patients remain flat on their backs, continuously using the cold/compression device and continuous passive motion machine unless they are performing an exercise session or taking a restroom break.
Beginning on the day of surgery, patients perform 3 exercise sessions a day. The focus is primarily on knee extension, knee flexion, and quadriceps muscle control. Although postoperative swelling limits the amount of knee flexion, patients should be able to easily achieve full knee extension immediately after surgery. Towel stretch (Figure 3) and heel prop (Figure 4) exercises are done to maintain full extension.
It is important to achieve and maintain full extension immediately after surgery, during the time that the graft is remodeling. If any tightness in extension is noticed, the passive knee extension device is used for a prolonged, low-load stretch. If any extension loss occurs, it is also important to discontinue knee flexion exercises and focus on knee extension in isolation until symmetry is regained. Similarly, any true strengthening exercises beyond those that work to maintain neuromuscular control of the quadriceps muscle group should be delayed until full knee flexion and extension symmetry is regained. Our experience has shown that rehabilitation progress is delayed when it attempts to address strength and ROM deficits at the same time.
Prevention and early detection of motion problems is key. By following these rehabilitation principles, we have been able to greatly reduce the incidence of postoperative ROM deficits.
Effect of ROM on Outcomes After ACL Reconstruction Surgery
Previous studies have shown that patients who maintain normal ROM according to International Knee Documentation Committee (IKDC) criteria have better outcomes after ACL surgery.11,26 The IKDC criteria consider normal knee extension to be within 2° of the opposite normal knee and normal flexion within 5° of the opposite normal knee.
Regression analysis from the study by Shelbourne and Gray26 showed that a lack of normal knee extension was the most important factor related to lower subjective scores and that lack of normal knee flexion was also a significant factor. This study showed that even a slight loss of extension (3°-5° compared with the opposite knee) can cause adverse symptoms, especially when damage to the articular cartilage or menisci is present in the knee. The following variables were included in the regression analysis: (1) intact or removed medial meniscus, (2) intact or removed lateral meniscus, (3) normal or damaged articular cartilage, (4) normal or less-than-normal knee extension after surgery, (5) normal or less-than-normal knee flexion after surgery, (6) time from injury to surgery, (7) KT-1000 manual maximum difference, (8) age at the time of surgery, and (9) injury type of acute or chronic. In patients with normal menisci, normal articular cartilage, and normal knee motion, 98% (153 of 156) had normal radiographic findings according to IKDC criteria at a minimum of 10 years after surgery. When compared with patients who had normal knee motion, patients who had less-than-normal knee motion were 2.4 times more likely to have abnormal radiographic findings.
In a more recent study, Shelbourne et al28 further investigated the effect of ROM loss on the incidence of arthritic changes observed on radiographs at a minimum of 5 years after ACL reconstruction in a group of 780 patients. Radiographs were graded according to the criteria described by the IKDC, and for this study the presence of OA was defined as any knee receiving a radiographic grade less than A (normal) in any compartment. The percentage of patients who had normal radiographic results at a mean of 10.5 years after ACL reconstruction was 71% in patients with normal knee extension and flexion, compared with 55% for patients who had any deficit in ROM at final follow-up (P < 0.01). Forty percent (188 of 479) of patients who had normal extension and flexion from early to final follow-up had radiographic evidence of OA, versus 53% (32 of 60) who had less-than-normal extension or flexion throughout follow-up (P = 0.04). Multivariate logistic regression analysis showed that the following factors were related to the presence of OA on radiographs: abnormal knee flexion at early follow-up, abnormal knee extension at final follow-up, abnormal knee flexion at final follow-up, partial medial meniscectomy, and articular cartilage damage. In fact, the factors of abnormal knee extension and abnormal knee flexion were equally as significant when compared with having a partial medial meniscectomy, with nearly 2 times the odds of developing OA. When one or both of the menisci were partially removed, the percentage of patients with normal radiographs was significantly higher if normal ROM was also achieved and maintained. Abnormal knee extension at early follow-up was the other factor included in the multivariate regression analysis, but it showed only a trend toward statistical significance (P = 0.05). Univariate regression analysis was performed on continuous variables, including age at the time of surgery and length of follow-up time. Older age at the time of surgery (P < 0.01) and longer follow-up time (P < 0.01) were statistically significant factors related to OA. The effects of partial meniscectomy on the development of OA may be reduced by achieving and maintaining normal knee ROM after ACL surgery.
Salmon et al22 found an association between ROM loss and abnormal radiographic results after ACL reconstruction with a patellar tendon graft. The regression analysis showed that abnormal radiographic grade at 13 years after ACL surgery was associated with medial meniscectomy, greater laxity on the Lachman test at latest follow-up, and loss of extension at latest follow-up. However, similar studies did not find a direct relationship between ROM loss and abnormal radiographs.8,18,21
Outside the context of ACL reconstruction, several studies have investigated the relationship between ROM loss and abnormal radiographs in patients with OA.5,7,17 In a study of 497 patients diagnosed with early knee OA, Holla et al7 found a significant association between decreased knee flexion and moderate or severe joint space narrowing in the medial compartment, osteophyte formation, subchondral sclerosis, and bony enlargement. Knee extension was not measured or considered as a potential factor in this study. Another study5 looked at the association between ROM loss and Kellgren-Lawrence scores in patients with bilateral OA (diagnosis based on meeting the criteria of the American College of Rheumatology for knee OA). It found that 82.5% of the knees studied could not achieve 0° of extension. It also found a significant negative correlation between knee extension/flexion and the Kellgren-Lawrence scores. Neither of these studies was designed to determine cause and effect, but they interpreted the loss of knee motion to be an indication of the extent of OA.
Salmon et al22 and Roe et al21 both found that the percentage of patients with extension loss significantly increased with time after surgery. This is in contrast to the work of Shelbourne and Gray,26 where the percentage of patients with > 5° of extension loss did not significantly increase over time; the authors reported only 1.7% of patients with > 5° of extension loss at a mean of 14.1 years after surgery. It is possible that a slight amount of extension loss (1°-2°) still considered “normal” by IKDC criteria may progress to a larger extension loss over a longer period. In contrast, patients who regain complete extension symmetry immediately after surgery may be better equipped to maintain that full symmetry over time. This would highlight the importance of regaining full knee extension preoperatively to allow for symmetric extension to be easily regained immediately after surgery and maintained in the long term.
A slight loss of knee extension is a catalyst in the development of other knee problems; specifically, patients can no longer stand with their weight shifted onto that leg and lock their knee out comfortably with the quadriceps muscles relaxed. It then becomes a subconscious habit to stand with the weight shifted onto the opposite, noninvolved knee with the involved knee flexed. Over time, this disuse may perpetuate the loss of knee extension motion and lead to decreased strength in the involved lower extremity. If the knee becomes increasingly stiff and weak, the pain increases, causing the patient to favor the normal leg even more.
Although statistical associations between different factors and the development of OA are available, determining causation is extremely difficult. Current clinical reasoning is dominated by the idea that the presence of OA leads to a loss of ROM.5,7,17 Is it possible that the ROM loss could lead to the development of OA? Many rehabilitation programs for patients with knee OA emphasize strengthening and functional activities over exercises to regain ROM,6,20,31 presumably because the ROM loss is assumed to be a consequence of the OA and, therefore, efforts to regain full ROM are thought to be ineffective.
We argue that the overall rehabilitation concept of first regaining full symmetric knee extension, followed by symmetric knee flexion, then symmetric strength, is helpful in the treatment of a variety of knee conditions, not just ACL injuries. In 2007, Shelbourne et al25 published outcomes of this rehabilitation philosophy in the treatment of 50 patients with deconditioned knees, 41 of whom had tibiofemoral joint space narrowing. Over 3 months of treatment, the mean ROM deficit (compared to the opposite knee) improved from 10° to 3° for knee extension and from 19° to 9° for knee flexion. Correspondingly, the IKDC subjective scores also improved from a mean of 34.5 to 64.1 points after 3 months of treatment, with continued improvement to a mean of 70.5 points at final follow-up 1 year later. Most of these patients had been told that they would need a total knee arthroplasty or arthroscopic procedure to alleviate their pain; however, 1 year after initial evaluation, 84% of patients in this study improved without surgical treatment.
Using this rehabilitation philosophy, Shelbourne et al25 showed that ROM can improve in patients with OA and that their subjective scores can improve correspondingly. Similarly, Shelbourne et al26 demonstrated that loss of ROM is associated with decreased subjective scores in the long term after ACL reconstruction. A recent study28 showed a relationship between loss of ROM and increased odds of developing OA after ACL reconstruction. If having full ROM after ACL reconstruction is associated with a lower risk of osteoarthritic changes on radiographs, then it stands to reason that the goal for all patients with any knee problem should be to regain and maintain full symmetric ROM. More emphasis should be placed on examining the ROM of both knees, including hyperextension, and on implementing treatment approaches that emphasize the goal of regaining and maintaining full symmetric knee motion.
Conclusions
There is an association between loss of knee ROM and OA changes on radiographs in the long term after ACL reconstruction. Loss of ROM and OA are also associated with lower subjective scores. Other factors related to OA, such as meniscal and articular cartilage status, cannot be modified, but through implementation of a directed rehabilitation program before and after ACL surgery, full symmetric ROM can be achieved.
Footnotes
One or more of the authors has declared a potential conflict of interest: K. Donald Shelbourne serves as an unpaid consultant for Kneebourne Therapeutic LLC and has received royalties from DJO, Inc related to the Cryo/Cuff.
References
- 1. Aglietti P, Zaccherotti G, DeBiase P, Taddei I. A comparison between medial meniscus repair, partial meniscectomy, and normal meniscus in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1994;307:165-173 [PubMed] [Google Scholar]
- 2. Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. N Am J Sports Phys Ther. 2009;4(1):2-12 [PMC free article] [PubMed] [Google Scholar]
- 3. Cohen M, Amaro JT, Ejnisman B, et al. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy. 2007;23(6):629-634 [DOI] [PubMed] [Google Scholar]
- 4. DeCarlo MS, Sell KE. Normative data for range of motion and single-leg hop in high school athletes. J Sport Rehabil. 1997;6:246-255 [Google Scholar]
- 5. Ersoz M, Ergun S. Relationship between knee range of motion and Kellgren-Lawrence radiographic scores in knee osteoarthritis. Am J Phys Med Rehabil. 2003;82(2):110-115 [DOI] [PubMed] [Google Scholar]
- 6. Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(4):452-469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holla JFM, Steultjens MPM, van der Leeden M, et al. Determinants of range of joint motion in patients with early symptomatic osteoarthritis of the hip and/or knee: an exploratory study in the CHECK cohort. Osteoarthritis Cartilage. 2011;19:411-419 [DOI] [PubMed] [Google Scholar]
- 8. Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med. 2011;39:89-98 [DOI] [PubMed] [Google Scholar]
- 9. Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188-193 [PubMed] [Google Scholar]
- 10. Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC. Factors involvedin the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med. 2010;38(3):455-463 [DOI] [PubMed] [Google Scholar]
- 11. Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins R. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2002;84:1560-1572 [DOI] [PubMed] [Google Scholar]
- 12. Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft. Am J Sports Med. 2008;36(7):1275-1282 [DOI] [PubMed] [Google Scholar]
- 13. Liden M, Sernert N, Rostgard-Christensen L, Kartus C, Ejerhed L. Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7 year radiographic and clinical follow-up study. Arthroscopy. 2008;24(8):899-908 [DOI] [PubMed] [Google Scholar]
- 14. Knee Magee DJ. In: Orthopedic Physical Assessment. 4th ed. Philadelphia, PA: Saunders; 2002:675-676 [Google Scholar]
- 15. McHugh MP, Tyler TF, Gleim GW, Nicholas SJ. Preoperative indicators of motion loss and weakness following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;27;407-411 [DOI] [PubMed] [Google Scholar]
- 16. Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10-15 years of follow-up. Am J Sports Med. 2010;38(11):2201-2210 [DOI] [PubMed] [Google Scholar]
- 17. Ozdemir F, Tukenmez O, Kokino S, Turan FN. How do marginal osteophytes, joint space narrowing and range of motion affect each other in patients with knee osteoarthritis. Rheumatol Int. 2006;26:516-522 [DOI] [PubMed] [Google Scholar]
- 18. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564-574 [DOI] [PubMed] [Google Scholar]
- 19. Reider B. ACL and OA [editorial]. Am J Sports Med. 2009;37(7):1279-1281 [DOI] [PubMed] [Google Scholar]
- 20. Roddy E, Zhang W, Doherty M. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis. 2005;64(4):544-548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarties. Am J Sports Med. 2005;33:1337-1345 [DOI] [PubMed] [Google Scholar]
- 22. Salmon LJ, Russell VJ, Refshauge K, et al. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34:721-732 [DOI] [PubMed] [Google Scholar]
- 23. Selmi TA, Fithian D, Neyret P. The evolution of osteoarthritis in 103 patients after ACL reconstruction at 17 years follow-up. Knee. 2006;13:353-358 [DOI] [PubMed] [Google Scholar]
- 24. Seon JK, Song EK, Park SJ. Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop. 2006;30(2):94-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shelbourne KD, Biggs A, Gray T. Deconditioned knee: the effectiveness of a rehabilitation program that restores normal knee motion to improve symptoms and function. N Am J Sports Phys Ther. 2007;2:81-89 [PMC free article] [PubMed] [Google Scholar]
- 26. Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471-480 [DOI] [PubMed] [Google Scholar]
- 27. Shelbourne KD, Liotta FJ, Goodloe SL. Preemptive pain management program for anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11:116-119 [PubMed] [Google Scholar]
- 28. Shelbourne KD, Urch SE, Gray T, Freeman H. Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery [published online ahead of print October 11, 2011]. Am J Sports Med. [DOI] [PubMed] [Google Scholar]
- 29. Shelbourne KD, Wilckens JH, Mollabash A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction: the effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19(4):332-336 [DOI] [PubMed] [Google Scholar]
- 30. Wu WH, Hackett T, Richmond JC. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med. 2002;30(6):845-850 [DOI] [PubMed] [Google Scholar]
- 31. Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16:137-162 [DOI] [PubMed] [Google Scholar]