Abstract
Context:
Reconstruction of the anterior cruciate ligament (ACL) is a common surgical procedure; however, there is no consensus to what the best graft option is to replace the injured ACL. The main options available consist of allografts and autografts, which include patellar tendon, hamstring tendon, and quadriceps tendon autografts.
Evidence Acquisition:
The PubMed database was searched in August 2010 for English-language articles pertaining to ACL grafts.
Results:
Postoperative outcome variables were analyzed to determine similarities and differences among the different graft options. These variables include stability, strength, function, return to sports, patient satisfaction, complications, and cost.
Conclusions:
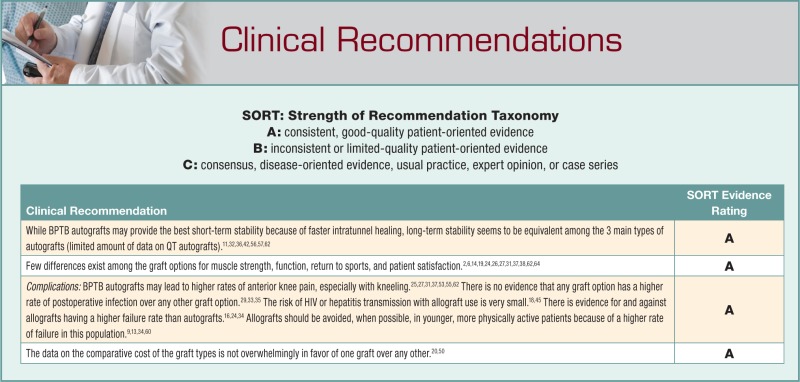
Both allografts and the 3 main options for autografts can provide excellent results in ACL reconstruction and lead to a high percentage of satisfied patients. However, differences exist among the graft choices. Both the similarities and the differences are important to discuss with a patient who will be undergoing ACL reconstruction so that he or she has the best information available when making a choice of graft.
Keywords: anterior cruciate ligament, autograft, allograft, reconstruction
Rupture of the anterior cruciate ligament (ACL) is a common injury, especially among athletes. Each year, 1 out of every 3000 Americans suffers an ACL injury.8,19 Accordingly, between 100 000 and 300 000 ACL reconstructions are performed every year in the United States.8,15,19 An important decision must be made prior to surgery regarding the type of graft that will be used to reconstruct the ACL. The 2 main groups used for grafts in ACL reconstruction are allografts and autografts. The theoretical advantages of an allograft are elimination of donor site morbidity, decreased pain, shorter operating and rehabilitation times, and better cosmesis.17
Three autograft options are commonly used. The bone–patellar tendon–bone (BPTB) allows for bone-to-bone healing within the tibial and femoral tunnels and has theoretical advantages of faster healing. Semitendinosus and gracilis tendons (quadrupled hamstring tendon [HT]) minimize donor site morbidity compared with the BPTB autograft and thus theoretically cause less anterior knee pain. A third option is the quadriceps tendon (QT), which can include a bone block from the patella (BQT).
With the ease of access to information, patients are more educated than ever about their health care issues. However, the abundance of information that exists on ACL graft options can be very confusing. In fact, the primary factor influencing a patient’s choice for an ACL graft is physician recommendation.19 Physicians should analyze the pros and cons regarding graft options. This can be a difficult task since studies often vary with respect to surgical technique, graft fixation method, tunnel positioning, rehabilitation protocol, allograft preparation and sterilization, outcome measures, and bias.
Stability
The primary goal of an ACL reconstruction is to restore stability to the knee. Therefore, measurements of knee stability are one of the most important determinants of success following an ACL reconstruction.
Autograft Versus Allograft
There is a paucity of prospective randomized studies comparing the 2 grafts, largely because patients often have a preference to which graft they receive, making randomization a problem. An exception is a prospective randomized study by Sun et al comparing 86 knees with a BPTB autograft to 86 knees with a BPTB allograft, with an average follow-up of 5.6 years (range, 4-8 years).63 With regard to stability, no difference was found for the Lachman test, pivot-shift test, mean laxity with arthrometer testing, or percentage of knees with greater than 3 mm of laxity on arthrometer testing.
Most studies comparing stability between autografts and allografts are level II-IV evidence. Great variation exists in the results of these studies, which can be at least partially attributed to the preparation of the allografts. Allografts sterilized with osmotic treatment, oxidation, acetone solvent drying, and gamma irradiation had a 45% rupture rate at 6 years’ follow-up.28
Three meta-analyses have been performed to compare the stability of autografts with allografts.16,24,39 Two meta-analyses found no statistically significant differences in knee stability measures (Lachman, pivot-shift, and arthrometer tests).16,39 The third found a small but statistically significant difference in mean anterior knee laxity on arthrometer testing, with the mean allograft laxity being 1.4 ± 0.2 and mean autograft laxity being 1.8 ± 0.1 (P < 0.02). However, no statistical difference existed between the autograft and allograft groups with regard to percentage of knees with less than 3 mm of laxity.24
It is not possible at this point to make any definitive conclusions regarding the resultant stability of these grafts compared with autografts. However, the best available evidence points toward relatively equivalent stability provided by allografts and autografts.
Autograft BPTB Versus HT Versus QT/BQT
A meta-analysis of 6 randomized controlled trials comparing HT and BPTB autografts, with a minimum of 2 years of follow-up, showed no statistical difference for the Lachman test.11 However, the BPTB was found to have a significantly decreased risk of a positive pivot-shift test compared with the HT graft (odds ratio, 0.46; 95% confidence interval, 0.24-0.86).11 A systematic review of 7 randomized controlled trials by Spindler found increased laxity with HT autografts in 3 of the 7 studies and no difference in 4 studies.62 In 2 of the 3 studies that showed increased laxity, a 2-strand HT graft was used instead of the more commonly used 4-strand HT grafts.30
Long-term level I and II evidence studies comparing HT and BPTB autografts have consistently shown no statistically significant difference in knee laxity.32,36,42,56,57 Four studies, with between 5 and 10 years of follow-up and at least 50 patients, found no statistically significant differences in mean side-to-side laxity on arthrometer testing between the 2 graft types.32,36,42,57 However, in one of the studies, when the 2 graft types were pooled and compared with a control group consisting of knees with a native ACL, a statistically significant increase in laxity of 2 mm was found for the reconstructed knees (P < 0.001).36 This difference in laxity did not appear to affect function in this study population.36
Short-term studies comparing stability between BPTB and HT autografts have provided more equivocal results. Some short-term studies have not found a statistically significant difference in knee laxity between the 2 groups.3,7,22,40,64 However, a number have found statistically significant differences in stability, favoring the BPTB autograft.5,10,12,21,23,51 It should be noted, however, that some of the older studies used the biomechanically inferior 2-stranded HT graft instead of the 4-stranded HT graft.5,10,51 Aside from the studies that used a 2-stranded HT graft, it is unclear why some short-term studies have found stability differences between the 2 grafts while other short-term studies and the long-term studies have not.
The QT autografts are the least studied of the 3 main autograft options. There are no prospective studies comparing QT/BQT and BPTB autografts and no prospective or retrospective studies comparing QT/BQT and HT autografts. Three retrospective studies with 2 years of follow-up have compared BQT autografts to BPTB autografts.27,31,37 There were no significant differences in the stability measures (KT-1000 arthrometer, Lachman, pivot-shift) between the 2 graft types in all 3 studies. A retrospective study by Geib et al compared 41 QT autograft reconstructions with 157 BQT autograft reconstructions and then pooled the QT autografts together to compare them with 30 BPTB autograft reconstructions.25 There were no significant differences between the QT and BQT autograft groups with regard to arthrometer and pivot-shift testing. The pooled QT graft group was found to have a significantly lower percentage of knees with greater than 3 mm of side-to-side laxity on arthrometer testing when compared with the BPTB group; however, no significant differences were found between the 2 groups on Lachman and pivot-shift testing.25
Single Bundle Versus Double Bundle
Theoretically, a double-bundle (DB) ACL reconstruction will more accurately reproduce the native structure of the ACL than the more commonly used single-bundle (SB) reconstruction. A more anatomical structure will theoretically provide a more anatomical functional result. SB reconstructions reliably restore anteroposterior tibial stability but may not be as effective at restoring rotational stability.41,67 This has led to the increased popularity of the DB reconstruction over the past decade.
A DB ACL reconstruction yielded better anteroposterior and rotary stability than a SB reconstruction in a cadaveric study.66 Markolf et al found that SB reconstructions sufficiently restored normal knee kinematics during a simulated pivot-shift test (the test most often used to check for rotary instability). DB reconstructions overcorrected for rotary instability and resulted in knees with less tibial rotation than knees with intact, native ACL.44
Clinical studies comparing DB and SB reconstructions have provided equivocal results. Some studies have failed to show any difference in stability measures between the 2 types of reconstructions.1,52,61 Others have reported stability differences but lacked differences in subjective scoring measures.4,49,59
Meredick et al meta-analyzed 4 randomized controlled studies comparing DB and SB reconstructions.46 On arthrometer testing, the DB group was found to have 0.52 mm less anterior tibial translation than the SB group (P < 0.05). To examine rotational stability, pivot-shift testing was also meta-analyzed, and no difference was found between the DB and SB groups. Several key points were raised by the findings of this meta-analysis. The first is the need for more standardized reporting of subjective outcome measures, thus allowing for better analyses of clinical outcome. The second is the need for better measures of rotational stability, as the pivot-shift test is, according to the authors, “subjective and difficult to quantitate.”46 To more objectively assess rotational instability, Yagi et al compared DB with 2 forms of SB reconstructions (anteromedial and posterolateral) using a 3-dimensional electromagnetic sensor system that could measure the acceleration of tibial motion during pivot-shift testing.65 While no intergroup difference was recognized by classic pivot-shift testing, the electromagnetic sensors recorded increased acceleration of tibial motion during pivot-shift testing for the SB group compared with the DB group. This was taken as evidence that the DB reconstructions provided better dynamic rotational stability than the SB reconstructions.65
There are currently limited data supporting the use of a DB reconstruction over a SB reconstruction. Studies showing improved stability have failed to consistently show a correlating improvement in quality of life or subjective outcome measures. Given the relatively recent rise in popularity of the DB reconstruction, no long-term studies exist to compare it with SB reconstruction.
Muscle Strength
Many studies have evaluated muscle strength and power following ACL reconstruction with either BPTB or HT autografts. Short-term follow-up studies have consistently found no difference in quadriceps strength but have shown mixed results with regard to hamstring.2,6,62,64 Holm et al followed patients for 10 years and found no differences between the BPTB and HT groups for quadriceps or hamstring isokinetic strength measurements.32 Spindler et al found no difference in quadriceps isokinetic strength measurements between BPTB and HT autografts in a systematic review of 7 randomized controlled trials. Three of the 7 studies showed statistically significant deficits in hamstring muscle strength in the HT group.62
Data is scarce regarding the return of strength following the use of a QT autograft in ACL reconstruction. A retrospective study by Han et al comparing 72 BQT autografts to 72 BPTB autografts found no significant difference in quadriceps muscle strength at 2 years postoperatively.31
Function
In a systematic review by Spindler et al, 13 functional assessments (Lysholm score, International Knee Documentation Committee [IKDC] score, and Cincinnati knee score) in 8 randomized controlled trials showed no significant differences in 12 of the 13 comparisons of BPTB and HT grafts. In the 1 study showing BPTB superiority, a 2-strand HT graft was used.62
Allografts have also been evaluated with these functional outcome measures. A systematic review of level I and II studies comparing autografts and allografts found no difference in IKDC score.24 Three retrospective studies with 2 years of follow-up compared BQT to BPTB autografts using knee function scales.27,31,37 No significant differences were found for the Lysholm score. Two of the 3 studies found no significant differences in IKDC score, while 1 study found BPTB autografts to have significantly better IKDC scores than BQT autografts.
Return To Sports
Gobbi et al prospectively followed 100 patients after ACL reconstruction (50 BPTB and 50 HT) for 2 years to determine their ability to return to sports.26 Sixty-five percent returned to their preinjury sport at the same level; 24% had shifted to a lower activity level; and 11% were unable to return to their previous sport activities. There was no difference between the BPTB and HT groups with respect to ability to return to sports. Brophy examined the ability to return to the National Football League after an ACL reconstruction prior to the start of one’s career.14 ACL reconstruction did not have a statistically significant reduction in career length or number of games played.
The use of a synthetic graft to replace a torn ACL has gained some popularity among athletes in recent years because of the potential for immediate graft stability, shorter rehabilitation, and a faster return to sports. A systematic review on the Ligament Advanced Reinforcement System by Machotka et al recommended caution when considering this synthetic graft because more research is needed.43
Patient Satisfaction
Cohen et al used a questionnaire-based analysis at an average of 41 months following ACL reconstruction. Of the 240 questionnaires that were returned, 92.9% of the patients were satisfied with their graft selection; both autografts and allografts resulted in satisfaction rates greater than 90%.19 Kocher’s review of 201 patients after ACL reconstruction (minimum 2 years after surgery) demonstrated that graft type did not influence patient satisfaction.38
Complications
Pain
Anterior knee pain, pain with activity, and pain when kneeling are all complications that can follow ACL reconstruction. Knee pain past the immediate postoperative period results in significantly decreased patient satisfaction.38 There is some evidence to suggest that BPTB autografts produce more pain than HT autografts, especially pain with kneeling.53,55,62 A 10-year follow-up study by Pinczewski et al compared the pain outcomes in patients that received either a BPTB or HT autograft.53 Both pain with kneeling and pain with strenuous activity were found to be significantly more common in the BPTB patients (P < 0.05). Harvest site symptoms such as tenderness, irritation, and numbness were significantly more common in the BPTB patients (P < 0.01).
Spindler et al found that only 1 of the 9 studies that evaluated anterior knee pain demonstrated a statistically significant difference in a systematic review with BPTB grafts resulting in greater pain.62 Kneeling pain was significantly more common in BPTB autografts than HT autografts.62 Poolman concluded that “the currently available best evidence, derived from a methodologically sound meta-analysis, suggests that HT autografts are superior for preventing anterior knee pain.”55
Four retrospective studies compared knee pain in QT and BPTB autograft groups.25,27,31,37 Three studies found a statistically significant increase in the incidence of anterior knee pain in the BPTB group.25,27,31 Pain with kneeling was significantly higher in the BPTB group compared to the BQT group.31,37
Poehling compared 118 allografts to 41 BPTB autografts54 and found that pain was significantly less during the first year in the allograft group. These differences did not persist during follow-up years 2 through 5. In a systematic review of allografts and autografts,16 3 studies found no difference between the 2 graft types.
Infection
Infection can result in graft failure, hyaline cartilage loss, and arthrofibrosis.48 Studies have not found a higher rate of postoperative infection with allografts than with autografts.29,33,35 A concern with allografts is the risk of disease transmission, such as HIV or hepatitis. There are no definitive data available regarding this risk because of a lack of reporting guidelines.18 With modern screening and testing protocols, the estimated risk of HIV or hepatitis transmission is less than 1 in 1.6 million.18,45
Graft Rupture/Failure
Rupture of the graft or contralateral native ACL is a psychologically devastating complication for a patient, especially a young athlete hoping to return to athletic competition. A prospective study of 180 ACL reconstruction patients for 10 years found that graft rupture occurred in 7 of 90 BPTB autograft patients (7.8%) and 12 of 90 HT autograft patients (13%).53 The difference between the 2 groups was not statistically significant. Graft rupture was associated with greater than 2 mm of side-to-side laxity at 2 years of follow-up (P < 0.0001). Contralateral ACL rupture occurred in 20 BPTB patients and 9 HT patients. This difference was statistically significant (P = 0.02).
Graft rupture and contralateral ACL rupture was studied in 612 autograft ACL reconstructions.58 At 5 years, graft rupture occurred in 6.4% (39 patients), and contralateral ACL rupture occurred in 5.7% (35 patients). When combined, the yearly ACL injury rate in the study patients was 2.4%, which is higher than the 1.5% to 1.7% ACL injury rate in normal, healthy athletic populations.47,58 The type of autograft did not affect the rate of graft or contralateral ACL rupture. The risk for graft rupture was greatest during the first year following surgery. A risk factor for contralateral ACL rupture was a return to sports that involved sidestepping, pivoting, and jumping.58
Two systematic reviews of studies comparing autografts and allografts found no statistically significant differences in graft failure (including graft rupture, subsequent revision surgery, or excess laxity on clinical or arthrometer testing) rate between the 2 groups.16,24 A prospective cohort study by Kaeding et al looked at a number of variables to determine predictors of graft rupture in the first 2 years following reconstruction.34 Use of an allograft and younger age were found to significantly increase the risk of graft rupture.34 A few other recent studies have found increased rates of graft failure in patients that received an allograft and had a high postoperative activity level.9,13,60 These findings have led some to conclude that allografts are not the best option for younger, more physically active patients.
Cost
In an ambulatory surgery setting, the autograft group had a significantly lower bill than the allograft group.50 The decreased operating room time in the allograft group did not offset the price of the allograft (approximately $1000).
Brophy et al reviewed the economic implications of a widespread conversion from SB to DB reconstructions and concluded that the potential additional costs would be between $36 million and $792 million per year in the United States.15
Conclusions
A number of variables play a role in determining the utility of the graft options: stability, muscle strength, function, return to sports, patient satisfaction, complications, and cost. Both allografts and the 3 main options for autografts can provide excellent results in ACL reconstruction and lead to a high percentage of satisfied patients. However, differences do exist among grafts. Both the similarities and the differences are important to discuss with a patient who will be undergoing ACL reconstruction so that she or he has the best information available when making a choice of graft.
References
- 1. Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y. Reconstruction of the anterior cruciate ligament: single-versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br. 2004;86(4):515-520 [PubMed] [Google Scholar]
- 2. Ageberg E, Roos HP, Silbernagel KG, Thomee R, Roos EM. Knee extension and flexion muscle power after anterior cruciate ligament reconstruction with patellar tendon graft or hamstring tendons graft: a cross-sectional comparison 3 years post surgery. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):162-169 [DOI] [PubMed] [Google Scholar]
- 3. Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone–patellar tendon–bone compared with double semitendinosus and gracilis tendon grafts: a prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86(10):2143-2155 [PubMed] [Google Scholar]
- 4. Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N. Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med. 2010;38(1):25-34 [DOI] [PubMed] [Google Scholar]
- 5. Anderson AF, Snyder RB, Lipscomb AB. Anterior cruciate ligament reconstruction: a prospective randomized study of three surgical methods. Am J Sports Med. 2001;29(3):272-279 [DOI] [PubMed] [Google Scholar]
- 6. Anderson JL, Lamb SE, Barker KL, Davies S, Dodd CA, Beard DJ. Changes in muscle torque following anterior cruciate ligament reconstruction: a comparison between hamstrings and patella tendon graft procedures on 45 patients. Acta Orthop Scand. 2002;73(5):546-552 [DOI] [PubMed] [Google Scholar]
- 7. Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction: a randomized study with two-year follow-up. Am J Sports Med. 2001;29(6):722-728 [DOI] [PubMed] [Google Scholar]
- 8. Baer GS, Harner CD. Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26(4):661-681 [DOI] [PubMed] [Google Scholar]
- 9. Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593-1601 [DOI] [PubMed] [Google Scholar]
- 10. Beynnon BD, Johnson RJ, Fleming BC, et al. Anterior cruciate ligament replacement: comparison of bone–patellar tendon–bone grafts with two-strand hamstring grafts: a prospective, randomized study. J Bone Joint Surg Am. 2002;84(9):1503-1513 [DOI] [PubMed] [Google Scholar]
- 11. Biau DJ, Katsahian S, Kartus J, et al. Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. Am J Sports Med. 2009;37(12):2470-2478 [DOI] [PubMed] [Google Scholar]
- 12. Bizzini M, Gorelick M, Munzinger U, Drobny T. Joint laxity and isokinetic thigh muscle strength characteristics after anterior cruciate ligament reconstruction: bone patellar tendon bone versus quadrupled hamstring autografts. Clin J Sport Med. 2006;16(1):4-9 [DOI] [PubMed] [Google Scholar]
- 13. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37(12):2362-2367 [DOI] [PubMed] [Google Scholar]
- 14. Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF. Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes: a case control study. Am J Sports Med. 2009;37(11):2102-2107 [DOI] [PubMed] [Google Scholar]
- 15. Brophy RH, Wright RW, Matava MJ. Cost analysis of converting from single-bundle to double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(4):683-687 [DOI] [PubMed] [Google Scholar]
- 16. Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009;91(9):2242-2250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Clark JC, Rueff DE, Indelicato PA, Moser M. Primary ACL reconstruction using allograft tissue. Clin Sports Med. 2009;28(2):223-244 [DOI] [PubMed] [Google Scholar]
- 18. Cohen SB, Sekiya JK. Allograft safety in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26(4):597-605 [DOI] [PubMed] [Google Scholar]
- 19. Cohen SB, Yucha DT, Ciccotti MC, Goldstein DT, Ciccotti MA, Ciccotti MG. Factors affecting patient selection of graft type in anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(9):1006-1010 [DOI] [PubMed] [Google Scholar]
- 20. Cole DW, Ginn TA, Chen GJ, et al. Cost comparison of anterior cruciate ligament reconstruction: autograft versus allograft. Arthroscopy. 2005;21(7):786-790 [DOI] [PubMed] [Google Scholar]
- 21. Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament: a comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(4):444-454 [DOI] [PubMed] [Google Scholar]
- 22. Ejerhed L, Kartus J, Sernert N, Kohler K, Karlsson J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med. 2003;31(1):19-25 [DOI] [PubMed] [Google Scholar]
- 23. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564-573 [DOI] [PubMed] [Google Scholar]
- 24. Foster TE, Wolfe BL, Ryan S, Silvestri L, Kaye EK. Does the graft source really matter in the outcome of patients undergoing anterior cruciate ligament reconstruction? An evaluation of autograft versus allograft reconstruction results: a systematic review. Am J Sports Med. 2010;38(1):189-199 [DOI] [PubMed] [Google Scholar]
- 25. Geib TM, Shelton WR, Phelps RA, Clark L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy. 2009;25(12):1408-1414 [DOI] [PubMed] [Google Scholar]
- 26. Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021-1028 [DOI] [PubMed] [Google Scholar]
- 27. Gorschewsky O, Klakow A, Putz A, Mahn H, Neumann W. Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15(11):1284-1292 [DOI] [PubMed] [Google Scholar]
- 28. Gorschewsky O, Klakow A, Riechert K, Pitzl M, Becker R. Clinical comparison of the Tutoplast allograft and autologous patellar tendon (bone-patellar tendon-bone) for the reconstruction of the anterior cruciate ligament: 2- and 6-year results. Am J Sports Med. 2005;33(8):1202-1209 [DOI] [PubMed] [Google Scholar]
- 29. Greenberg DD, Robertson M, Vallurupalli S, White RA, Allen WC. Allograft compared with autograft infection rates in primary anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2010;92(14):2402-2408 [DOI] [PubMed] [Google Scholar]
- 30. Hamner DL, Brown CH, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81(4):549-557 [DOI] [PubMed] [Google Scholar]
- 31. Han HS, Seong SC, Lee S, Lee MC. Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res. 2008;466(1):198-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38(3):448-454 [DOI] [PubMed] [Google Scholar]
- 33. Judd D, Bottoni C, Kim D, Burke M, Hooker S. Infections following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2006;22(4):375-384 [DOI] [PubMed] [Google Scholar]
- 34. Kaeding C, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Katz LM, Battaglia TC, Patino P, Reichmann W, Hunter DJ, Richmond JC. A retrospective comparison of the incidence of bacterial infection following anterior cruciate ligament reconstruction with autograft versus allograft. Arthroscopy. 2008;24(12):1330-1335 [DOI] [PubMed] [Google Scholar]
- 36. Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. Am J Sports Med. 2007;35(5):729-739 [DOI] [PubMed] [Google Scholar]
- 37. Kim SJ, Kumar P, Oh KS. Anterior cruciate ligament reconstruction: autogenous quadriceps tendon-bone compared with bone-patellar tendon-bone grafts at 2-year follow-up. Arthroscopy. 2009;25(2):137-144 [DOI] [PubMed] [Google Scholar]
- 38. Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84(9):1560-1572 [DOI] [PubMed] [Google Scholar]
- 39. Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(3):292-298 [DOI] [PubMed] [Google Scholar]
- 40. Laxdal G, Kartus J, Hansson L, Heidvall M, Ejerhed L, Karlsson J. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(1):34-42 [DOI] [PubMed] [Google Scholar]
- 41. Lewis PB, Parameswaran AD, Rue JP, Bach BR. Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med. 2008;36(10):2028-2036 [DOI] [PubMed] [Google Scholar]
- 42. Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35(5):740-748 [DOI] [PubMed] [Google Scholar]
- 43. Machotka Z, Scarborough I, Duncan W, Kumar S, Perraton L. Anterior cruciate ligament repair with LARS (ligament advanced reinforcement system): a systematic review. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Markolf KL, Park S, Jackson SR, McAllister DR. Simulated pivot-shift testing with single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2008;90(8):1681-1689 [DOI] [PubMed] [Google Scholar]
- 45. McGuire DA, Hendricks SD. Allograft tissue in ACL reconstruction. Sports Med Arthrosc. 2009;17(4):224-233 [DOI] [PubMed] [Google Scholar]
- 46. Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36(7):1414-1421 [DOI] [PubMed] [Google Scholar]
- 47. Mountcastle SB, Posner M, Kragh JF, Taylor DC. Gender differences in anterior cruciate ligament injury vary with activity: epidemiology of anterior cruciate ligament injuries in a young, athletic population. Am J Sports Med. 2007;35(10):1635-1642 [DOI] [PubMed] [Google Scholar]
- 48. Mouzopoulos G, Fotopoulos VC, Tzurbakis M. Septic knee arthritis following ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1033-1042 [DOI] [PubMed] [Google Scholar]
- 49. Muneta T, Koga H, Mochizuki T, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy. 2007;23(6):618-628 [DOI] [PubMed] [Google Scholar]
- 50. Nagda SH, Altobelli GG, Bowdry KA, Brewster CE, Lombardo SJ. Cost analysis of outpatient anterior cruciate ligament reconstruction: autograft versus allograft. Clin Orthop Relat Res. 2010;468(5):1418-1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. O’Neill DB. Arthroscopically assisted reconstruction of the anterior cruciate ligament: a prospective randomized analysis of three techniques. J Bone Joint Surg Am. 1996;78(6):803-813 [PubMed] [Google Scholar]
- 52. Park SJ, Jung YB, Jung HJ, et al. Outcome of arthroscopic single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a preliminary 2-year prospective study. Arthroscopy. 2010;26(5):630-636 [DOI] [PubMed] [Google Scholar]
- 53. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564-574 [DOI] [PubMed] [Google Scholar]
- 54. Poehling GG, Curl WW, Lee CA, et al. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: allograft versus autograft. Arthroscopy. 2005;21(7):774-785 [DOI] [PubMed] [Google Scholar]
- 55. Poolman RW, Abouali JA, Conter HJ, Bhandari M. Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J Bone Joint Surg Am. 2007;89(7):1542-1552 [DOI] [PubMed] [Google Scholar]
- 56. Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33(9):1337-1345 [DOI] [PubMed] [Google Scholar]
- 57. Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34(12):1933-1940 [DOI] [PubMed] [Google Scholar]
- 58. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948-957 [DOI] [PubMed] [Google Scholar]
- 59. Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(2):137-145 [DOI] [PubMed] [Google Scholar]
- 60. Singhal MC, Gardiner JR, Johnson DL. Failure of primary anterior cruciate ligament surgery using anterior tibialis allograft. Arthroscopy. 2007;23(5):469-475 [DOI] [PubMed] [Google Scholar]
- 61. Song EK, Oh LS, Gill TJ, Li G, Gadikota HR, Seon JK. Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med. 2009;37(9):1705-1711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986-1995 [DOI] [PubMed] [Google Scholar]
- 63. Sun K, Tian SQ, Zhang JH, Xia CS, Zhang CL, Yu TB. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft. Arthroscopy. 2009;25(7):750-759 [DOI] [PubMed] [Google Scholar]
- 64. Taylor DC, DeBerardino TM, Nelson BJ, et al. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: a randomized controlled trial using similar femoral and tibial fixation methods. Am J Sports Med. 2009;37(10):1946-1957 [DOI] [PubMed] [Google Scholar]
- 65. Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100-107 [DOI] [PubMed] [Google Scholar]
- 66. Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(5):660-666 [DOI] [PubMed] [Google Scholar]
- 67. Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35(2):223-227 [DOI] [PubMed] [Google Scholar]