Abstract
Context:
Prolonged symptoms after concussion are called post-concussion syndrome (PCS), which is a controversial disorder with a wide differential diagnosis.
Evidence Acquisition:
MEDLINE and PubMed searches were conducted for the years 1966 to 2011 using the search terms brain concussion/complications OR brain concussion/diagnosis OR brain concussion/therapy AND sports OR athletic injuries. Secondary search terms included post-concussion syndrome, trauma, symptoms, metabolic, sports medicine, cognitive behavioral therapy, treatment and rehabilitation. Additional articles were identified from the bibliographies of recent reviews.
Results:
Of 564 studies that fulfilled preliminary search criteria, 119 focused on the diagnosis, pathophysiology, and treatment/rehabilitation of concussion and PCS and formed the basis of this review. Rest is the primary treatment for the acute symptoms of concussion. Ongoing symptoms are either a prolonged version of the concussion pathophysiology or a manifestation of other processes, such as cervical injury, migraine headaches, depression, chronic pain, vestibular dysfunction, visual dysfunction, or some combination of conditions. The pathophysiology of ongoing symptoms from the original concussion injury may reflect multiple causes: anatomic, neurometabolic, and physiologic.
Conclusions:
Treatment approaches depend on the clinician’s ability to differentiate among the various conditions associated with PCS. Early education, cognitive behavioral therapy, and aerobic exercise therapy have shown efficacy in certain patients but have limitations of study design. An algorithm is presented to aid clinicians in the evaluation and treatment of concussion and PCS and in the return-to-activity decision.
Keywords: concussion, post-concussion syndrome, physiology, rehabilitation, cognitive behavioral therapy
Concussion, a form of mild traumatic brain injury (TBI), is a leading public health problem, with an estimated 1.6 to 3.8 million sport-related concussions each year in the United States.63 The majority of patients with sport-related concussion recover within a 7- to 10-day period, although children and adolescents require more time to recover than do collegiate or professional athletes.8,75 Persistence of symptoms beyond the generally accepted time frame for recovery may represent a prolonged concussion or may herald the development of post-concussion syndrome (PCS).117 The accepted time frame for recovery is not scientifically established and is influenced by factors such as age, sex, and history of prior concussions.43,54,74 Approximately 10% of athletes have persistent signs and symptoms of concussion beyond 2 weeks.117 In non-sport–related concussion, most individuals recover completely within the first 3 months68; however, up to 33%12,95 may exhibit symptoms beyond that.
There is some uncertainty about the definition of PCS, in part because it is diagnosed according to clinical criteria. PCS is defined by the fourth edition of the Diagnostic and Statistics Manual as (1) cognitive deficits in attention or memory and (2) at least 3 or more of the following symptoms: fatigue, sleep disturbance, headache, dizziness, irritability, affective disturbance, apathy, or personality change.13 However, these criteria are conservative. The broader definition of PCS is represented by clinical criteria of the World Health Organization’s International Classification of Diseases, or ICD-10—namely, 3 or more of the following symptoms: headache, dizziness, fatigue, irritability, insomnia, concentration difficulty, or memory difficulty. Use of these criteria is 6 times more sensitive for identifying patients with PCS.13 After 3 weeks, patients (especially athletes) begin to worry about when they will recover, and by 6 weeks, if symptoms persist, PCS can alter their lives.117
There is considerable controversy regarding PCS because of the nonspecificity of symptoms and the fact that most cognitive deficits resolve within 1 to 3 months after mild TBI in the majority of patients.2,16 The differential diagnosis includes depression, somatization, chronic fatigue and pain, cervical injury, vestibular dysfunction, visual dysfunction, or some combination of these conditions.2 Patients often present with considerable insecurity about PCS symptoms: headache, fatigue, sleep disturbance, vertigo, irritability, anxiety, depression, apathy, and difficulty with concentration and exercise.117 The clinical challenge is to determine whether prolonged symptoms reflect a version of the concussion pathophysiology versus a manifestation of a secondary process, such as premorbid clinical depression or migraine headaches.21,62 If symptoms that were experienced early after the injury are exacerbated with exertion, but improved with rest, then the original concussion pathophysiology is likely persisting.62 If ongoing symptoms are exacerbated by even minimal activity and no longer respond to rest, this may represent psychologic symptoms related to prolonged inactivity and frustration with inability to return to usual activities.62 Data suggest that at least some patients with PCS have measurable pathophysiology. For example, concussed athletes with prolonged depressive symptoms showed reduced functional magnetic resonance imaging activation in the dorsolateral prefrontal cortex and striatum and attenuated deactivation in medial frontal and temporal regions accompanied by gray matter loss in these areas.18 Some PCS patients have persistent abnormalities of brain blood flow on single-photon emission computed tomography scan,1 neurochemical imbalances (eg, serum S100B),102 and electrophysiologic indices of impairment.4,27 Postural instability is much more likely when other signs and symptoms are the result of organic-based PCS.40
Theory of Prolonged Symptoms
Animal research suggests that the concussed brain is in a vulnerable state that places it at increased risk of more debilitating injury should more trauma occur before metabolic homeostasis is restored.32,70 This vulnerable state can be inferred in humans from data that concussion risk increases after having had 1 or more concussions43 and from the second impact syndrome (SIS).15 SIS is based on rare and disputed cases in children and adolescents in which a second mild head injury is thought to occur before resolution of a concussion, with resulting malignant brain edema. McCrory76 argues that rather than SIS being a complication of recurrent concussion, it represents “diffuse cerebral swelling,” which is a well-recognized complication of TBI in children. Additionally, a recent review of death caused by blunt trauma found subdural hematoma to be the cause of all 17 cases of SIS. It is unclear whether concussion may have increased the risk of bleeding or whether the initial injuries were occult subdural injuries diagnosed as concussions.107 There is also accumulating evidence of potential long-term sequelae in humans from studies showing that previous concussions may be associated with slower recovery of neurologic function43 and that repeated concussions can result in permanent neurocognitive impairment41,43,53 and perhaps an increased incidence of depression.42 Predictors of PCS are not known with certainty, but some clinical variables appear to increase the risk. These include a history of prior concussions,42,43,90 female sex,90,93 younger age,71,90 history of cognitive dysfunction,106 and affective disorders, such as anxiety and depression.17,72,74 Predictors related to injury severity, such as length of posttraumatic amnesia and cognitive difficulties, are clearly associated with symptoms at 1 month but less so at 6 months after injury.7 Interestingly, no study has identified injury severity as a factor contributing to the development of PCS.
Anatomic/Mechanical
The acceleration-deceleration forces applied to the moving brain cause shearing of neural and vascular elements55 with sudden neuronal depolarization followed by a period of nerve cell transmission failure101,115 that can result in loss of consciousness.84 Animal studies of concussion show neuropathologic changes in the hippocampus and diffuse axonal injury along with disruption of the blood-brain barrier and eventual neuronal loss.5,48,85,118 Diffusion tensor imaging of the corpus callosum within 6 days of concussion in adolescents showed white matter edema that correlated with symptom severity.116 Quantitative electroencephalography and single-photon emission computed tomography showed focal cortical dysfunction in conjunction with persistent blood-brain barrier disruption and reduced global and regional cerebral blood flow in patients with PCS for more than a month post-injury.60
Neurometabolic
The neurometabolic basis for concussion and post-concussive symptoms has been described in animal models.51 Experimental brain injury induces a cascade of neurochemical, ionic, and metabolic changes that change cerebral glucose metabolism and blood flow and alter mitochondrial respiration.50,57,58,78 There is an initial phase of hyperglycolysis, followed by a prolonged phase of metabolic depression that can last 7 to 10 days in adult rats.51 This basic pathologic response has been reported after human brain injury in positron emission tomography studies showing a similar pattern of early hyperglycolysis, followed by glucose metabolic depression (Figure 1).9,10 In magnetic resonance spectroscopy studies of human concussion, athletes who reported being symptom free at 3 to 15 days did not demonstrate complete metabolic recovery until a mean of 30 days post-injury.111 Mitochondrial metabolism took significantly longer (an additional 15 days) to recover in athletes with a second concussion.112
Figure 1.
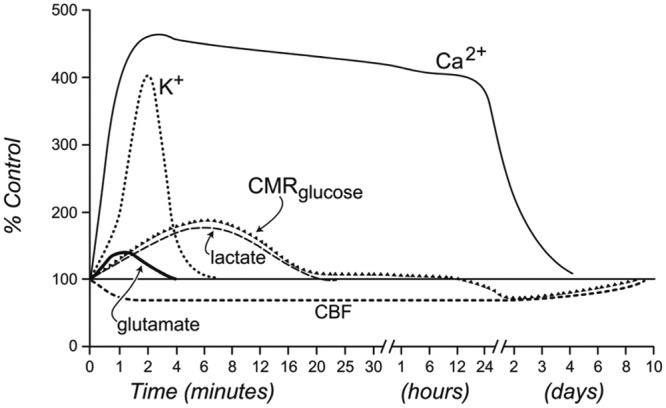
Neurometabolic cascade following concussion.
K+, potassium; CMRglucose, cerebral metabolic rate of glucose utilization; Ca2+, calcium; CBF, cerebral blood flow. With permission (adapted from Hovda et al50).
Physiologic
Concussion-induced mechanical changes coupled with the neurometabolic alterations can affect functional cerebral circulation.5,104,105 Concussion is also associated with metabolic and physiologic changes in organ systems outside the brain.67 Concussed patients have higher heart rates at rest59 and after cognitive45 and physiological stress.30 Autonomic nervous system (ANS) function may be disturbed after concussion.88 Severe TBI,59 cerebral infarction,113 and concussion in athletes29 are associated with greater sympathetic nervous activity and lower parasympathetic activity when compared with controls. Autonomic dysregulation is proportional to TBI severity and improves during TBI recovery.35 Increased sympathetic nervous activity may be due to an altered endocrine99 or neuropeptide36 milieu after TBI. Autoregulation, the maintenance of cerebral blood flow at appropriate levels during changes in systemic blood pressure, and cerebral blood flow are also disturbed after concussion,56,103 which may explain why symptoms often reappear or worsen with physical and/or mental exertion. Impairment of the cerebral vasculature after TBI sensitizes the brain to secondary insults, such as hypotension, intracranial hypertension, and dehydration.33
Cerebral artery regulation is very sensitive to the arterial carbon dioxide tension (PaCO2) and responds with vasoconstriction when PaCO2 is low and vasodilation when it increases.69 The major determinant of the blood PaCO2 is pulmonary ventilation. This physiologic process is diminished in severely brain-injured humans24 and is altered early after experimental concussive injury in animals.34 If concussed patients have an altered ANS balance, pulmonary ventilation may be altered as well, especially during exertion.
It is not known how physiologic dysfunction develops and persists after TBI. The primary ANS control center is located in the brainstem.98 Recent functional magnetic resonance imaging evidence82 suggests that the ANS is more diffusely distributed in the human brain beyond the brainstem to include higher cortical (eg, dorsolateral prefrontal, posterior insular, and middle temporal cortices) and limbic-related regions (eg, amygdala, hippocampus, and thalamus). A head injury resulting from a twisting mechanism or direct trauma to the upper cervical/posterior skull region may damage this center. Thus, brain injury may alter central ANS regulation, disrupting cardiorespiratory control of ventilation and leading to the symptom exacerbation seen with physical exertion after concussion.67
Assessment and Differential Diagnosis
Patient history should include a description of the mechanism and force of the head trauma; the number and severity of symptoms, including retrograde and anterograde amnesia; and a history of any prior concussions, including mechanism, symptom type, and duration.79 The nature, burden, and duration of symptoms appear to be the primary determinant of injury severity in concussion.79 A history of multiple concussions appears to increase the risk for PCS.43,90 The older teenage or adult patient may be experiencing PCS if symptoms persist beyond 3 to 4 weeks, especially in athletes.117 A history of migraine headaches, depression, anxiety, attention-deficit/hyperactivity disorder, or learning disability is also crucial since TBI can exacerbate these conditions.62 Depression is an important differential diagnoses for PCS, in part because of overlapping symptoms. A study of physician-diagnosed depressive disorder found that 9 out of 10 patients met liberal criteria for PCS, whereas 5 out of 10 met more conservative criteria.52
A detailed headache history is helpful because those with migraines may be at increased risk of concussion with severe and prolonged postconcussion symptoms.62,64 Upper cervical spine injury can also mimic the symptoms of concussion and PCS.23,109
The physical examination should include an assessment of concentration (eg, drills such as stating the months of the year in reverse, a series of digits backward tests), memory (recall of 3 words at 5 minutes), and examination of the cranial nerves,79 particularly extraocular motion, since PCS patients can have persistent abnormalities of smooth pursuit saccadic eye movements.46 The Romberg test,20 tandem gait, and vestibular testing should also be performed.87 After the neurologic examination, the cervical spine should be carefully assessed for tenderness, spasm, and range of motion. Precipitation of headaches, dizziness, or vertigo should direct therapy to address a cervical injury.109
The physical examination should include an assessment of concentration (eg, drills such as stating the months of the year in reverse, a series of digits backward tests), memory (recall of 3 words at 5 minutes), and examination of the cranial nerves,79 particularly extraocular motion, since PCS patients can have persistent abnormalities of smooth pursuit saccadic eye movements.46 The Romberg test,20 tandem gait, and vestibular testing should also be performed.87 After the neurologic examination, the cervical spine should be carefully assessed for tenderness, spasm, and range of motion. Precipitation of headaches, dizziness, or vertigo should direct therapy to address a cervical injury.109
Diagnostic Testing
A standardized treadmill test employing a Balke protocol66 to determine physiologic recovery has very good interrater and sufficient retest reliability for identifying patients with symptom exacerbation from concussion.65 Concussion symptoms are typically exacerbated by exercise,77 while exercise may rapidly improve depression.22 If patients can exercise to exhaustion without reproduction or exacerbation of headache or other concussion symptoms, then the symptoms may be due to another problem.65,66 Computerized neuropsychological testing is widely employed in sport even though there are concerns with retest reliability and no data are available to suggest improved outcomes.14,94,100
Rehabilitation of Concussion and Pcs
Current guidelines recommend a period of cognitive and physical rest in the early postinjury period because symptoms can increase with cognitive and physical exertion.73,77 Prolonged rest, especially in athletes, can lead to physical deconditioning,117 metabolic disturbances,44 and secondary symptoms such as fatigue and reactive depression.11 There is no scientific evidence that prolonged rest for more than several weeks in concussed patients is beneficial.
Reassurance, discussions of expected recovery time, and compensatory strategies can improve symptoms of PCS.80,114 An information booklet92 and psychological intervention81 can reduce PCS symptoms at 3 to 6 months after injury.
A recent systematic review of psychological interventions for PCS concluded that there was limited evidence of benefit.2 Cognitive behavioral therapy is a form of psychological intervention that focuses on identifying and changing patterns of maladaptive thinking and behavior that can exacerbate—or, in some cases, even cause—affective symptoms often associated with persistent effects of direct brain injury, including depression and anxiety. Three randomized controlled trials and 7 other studies of cognitive behavioral therapy all found some benefit, although there were limitations in study design.2
In children, most post-concussion symptoms resolve within a month.89 The exceptions are children who have a history of previous head injury, learning difficulties, or family stressors.89 An information booklet on strategies for dealing with posttraumatic symptoms resulted in fewer symptoms and less behavioral changes in children 3 months after injury.91
Interventions to improve cognition have improved performance on selected neuropsychological test scores and cognitive function following neurocognitive rehabilitation in patients with mild or mild-to-moderate TBI.19,47,49 Neurocognitive rehabilitation uses cognitive tasks to improve cognitive processes, or it may involve developing compensatory strategies to address difficulties with aspects of cognition, such as attention, memory, and executive functioning. Empirical support varies for neurocognitive rehabilitation of different cognitive processes. Neurocognitive rehabilitation of attention processes has received the most empirical support after TBI.19,47,86,96 A small randomized controlled trial of an 11-week program of combined neurocognitive rehabilitation and cognitive behavioral therapy in mild-to-moderate TBI improved divided auditory attention, anxiety, and depression in participants who were symptomatic for 5 years.108
There is no scientific evidence that medication speeds recovery from concussion in humans. The most common medications prescribed for PCS are antidepressants.80 Selective serotonin reuptake inhibitors have become the primary treatment for head injury–associated depression25,117 and can improve depression and the cognitive deficits associated with concussion.25,31,117 Tricyclic antidepressants such as low-dose amitriptyline110 are often used clinically to aid sleep and headaches in patients with PCS, but there are no controlled trials of their efficacy in restoring normal function.
The excitatory amino acids glutamate and aspartate may be important mediators of brain injury. NMDA and AMPA antagonists have been proposed for brain injury recovery.83 The deficits in attention and memory seen after TBI mimic those in Alzheimer disease. There is some evidence that cholinergic agents (physostigmine and donepezil—acetylcholinesterase inhibitors that temporarily increase brain acetylcholine levels) and lecithin and CDP-choline (precursors of brain acetylcholine) alleviate some of the cognitive deficits suffered by brain injured patients.39,97
Vestibular dysfunction is commonly associated with TBI.3 Vestibular suppressants may delay recovery and have been replaced by vestibular rehabilitation for posttraumatic vertigo.26 Vestibular rehabilitation may reduce dizziness and improve gait and balance in children and adults.3
The upper cervical spine is particularly vulnerable to trauma because it is the most mobile part of the vertebral column, with a complex proprioceptive system that has connections to the vestibular and visual systems.61 Cervical vertigo or dizziness after whiplash injury can mimic the symptoms of PCS. It may be due to mechanoreceptor dysfunction109 or posttraumatic vertebrobasilar circulatory insufficiency.23
Physiologic disequilibrium may be a significant modulating factor in concussion and PCS.67 Uncontrolled human activity too soon after concussion is detrimental to recovery.43,73 Experimental animal data show that premature voluntary exercise within the first week after concussion impairs recovery while aerobic exercise performed 14 to 21 days after concussion improves cognitive performance.37,38 Neurotrophins (brain-derived neurotrophic factor) promote neuronal recovery.6 Premature voluntary exercise within the first week after concussion interferes with the postconcussion rise of brain-derived neurotrophic factor and is associated with impaired cognitive memory task performance.37,38 Conversely, aerobic exercise performed 14 to 21 days after TBI upregulated brain-derived neurotrophic factor in association with improved cognitive performance.37,38
The most recent consensus statement on concussion in sport advises that when asymptomatic at rest, concussed patients should progress stepwise from light aerobic activity, such as walking or stationary cycling, up to sport- or work-specific activities.79 The guideline recognizes the important physiologic component of testing and recovery after concussion.
Controlled aerobic exercise rehabilitation after establishing symptom-free exercise capacity via treadmill testing has helped athlete and nonathlete PCS patients recover.66 Exercise testing and rehabilitation should be employed only if patients have persistent symptoms for 3 to 6 weeks or more.38,65,66 A similar rehabilitation program has been established for children with PCS after sport-related concussion that combines gradual, closely monitored physical conditioning, general coordination exercises, visualization, education, and motivation activities.28
Figure 2 presents a suggested progression for making the return-to-activity decision in patients who have recovered from the acute effects of concussion and in those whose symptoms persist beyond 3 weeks.65,66
Figure 2.
Return-to-activity algorithm for concussion and postconcussion syndrome. *Time for symptom resolution will vary depending on clinical circumstances. Most athletes recover within 1 to 3 weeks. **Treadmill testing in patients with persistent symptoms should not be performed before 3 weeks after injury. Neuropsychological testing is not indicated, because the patient is still symptomatic. ¶If neuropsychological testing has been used, assume that there is a baseline preinjury test or valid normative data for the particular patient. †Exercise to exhaustion without exacerbation of symptoms. ‡Exercise stopped at a submaximal effort level because of symptom exacerbation. §Repeat testing interval will vary depending on clinical circumstances; it may be several days to several weeks. If athlete is not recovering, consider aerobic exercise rehabilitation. If computerized neuropsychological testing has been used and remains abnormal, continue exercise treatment and consider consultation with a neuropsychologist to evaluate for a specific cognitive deficit. RTA, return to activity; PCS: postconcussion syndrome; NP, neuropsychological.
Conclusions
Rest is the primary treatment for the acute symptoms of concussion.79 Ongoing symptoms reflect either a prolonged version of the concussion or a manifestation of other processes, such as cervical injury, migraine headaches, depression, chronic pain, vestibular dysfunction, visual dysfunction, or a combination of conditions.62 The pathophysiology of ongoing symptoms from the original concussion injury may reflect multiple causes: anatomic, neurometabolic, and physiologic.51,67,116 Treatment approaches depend on the clinician’s ability to differentiate among the various conditions associated with PCS. Early education,80,114 cognitive behavioral therapy,2 and aerobic exercise therapy66 have been shown to be effective in certain patients.
References
- 1. Agrawal D, Gowda NK, Bal CS, Pant M, Mahapatra AK. Is medial temporal injury responsible for pediatric postconcussion syndrome? A prospective controlled study with single-photon emission computerized tomography. J Neurosurg. 2005;102(2)(suppl):167-171 [DOI] [PubMed] [Google Scholar]
- 2. Al Sayegh A, Sandford D, Carson AJ. Psychological approaches to treatment of postconcussion syndrome: a systematic review. J Neurol Neurosurg Psychiatry. 2010;81(10):1128-1134 [DOI] [PubMed] [Google Scholar]
- 3. Alsalaheen BA, Mucha A, Morris LO, et al. Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther. 2010;34(2):87-93 [DOI] [PubMed] [Google Scholar]
- 4. Arciniegas DB, Topkoff JL. Applications of the P50 evoked response to the evaluation of cognitive impairments after traumatic brain injury. Phys Med Rehabil Clin N Am. 2004;15(1):177-203 [DOI] [PubMed] [Google Scholar]
- 5. Baldwin SA, Fugaccia I, Brown DR, Brown LV, Scheff SW. Blood-brain barrier breach following cortical contusion in the rat. J Neurosurg. 1996;85(3):476-481 [DOI] [PubMed] [Google Scholar]
- 6. Barde YA. Trophic factors and neuronal survival. Neuron. 1989;2(6):1525-1534 [DOI] [PubMed] [Google Scholar]
- 7. Bazarian JJ, Atabaki S. Predicting postconcussion syndrome after minor traumatic brain injury. Acad Emerg Med. 2001;8(8):788-795 [DOI] [PubMed] [Google Scholar]
- 8. Belanger HG, Vanderploeg RD. The neuropsychological impact of sports-related concussion: a meta-analysis. J Int Neuropsychol Soc. 2005;11(4):345-357 [DOI] [PubMed] [Google Scholar]
- 9. Bergsneider M, Hovda DA, Lee SM, et al. Dissociation of cerebral glucose metabolism and level of consciousness during the period of metabolic depression following human traumatic brain injury. J Neurotrauma. 2000;17(5):389-401 [DOI] [PubMed] [Google Scholar]
- 10. Bergsneider M, Hovda DA, Shalmon E, et al. Cerebral hyperglycolysis following severe traumatic brain injury in humans: a positron emission tomography study. J Neurosurg. 1997;86(2):241-251 [DOI] [PubMed] [Google Scholar]
- 11. Berlin AA, Kop WJ, Deuster PA. Depressive mood symptoms and fatigue after exercise withdrawal: the potential role of decreased fitness. Psychosom Med. 2006;68(2):224-230 [DOI] [PubMed] [Google Scholar]
- 12. Binder LM, Rohling ML, Larrabee GJ. A review of mild head trauma: part I. Meta-analytic review of neuropsychological studies. J Clin Exp Neuropsychol. 1997;19(3):421-431 [DOI] [PubMed] [Google Scholar]
- 13. Boake C, McCauley SR, Levin HS, et al. Diagnostic criteria for postconcussional syndrome after mild to moderate traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2005;17(3):350-356 [DOI] [PubMed] [Google Scholar]
- 14. Broglio SP, Ferrara MS, Macciocchi SN, Baumgartner TA, Elliott R. Test-retest reliability of computerized concussion assessment programs. J Athl Train. 2007;42(4):509-514 [PMC free article] [PubMed] [Google Scholar]
- 15. Cantu RC. Second-impact syndrome. Clin Sports Med. 1998;17(1):37-44 [DOI] [PubMed] [Google Scholar]
- 16. Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;43(suppl):84-105 [DOI] [PubMed] [Google Scholar]
- 17. Chamelian L, Feinstein A. The effect of major depression on subjective and objective cognitive deficits in mild to moderate traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2006;18(1):33-38 [DOI] [PubMed] [Google Scholar]
- 18. Chen JK, Johnston KM, Petrides M, Ptito A. Neural substrates of symptoms of depression following concussion in male athletes with persisting postconcussion symptoms. Arch Gen Psychiatry. 2008;65(1):81-89 [DOI] [PubMed] [Google Scholar]
- 19. Cicerone KD. Remediation of “working attention” in mild traumatic brain injury. Brain Inj. 2002;16(3):185-195 [DOI] [PubMed] [Google Scholar]
- 20. Del Percio C, Babiloni C, Marzano N, et al. “Neural efficiency” of athletes’ brain for upright standing: a high-resolution EEG study. Brain Res Bull. 2009;79(3-4):193-200 [DOI] [PubMed] [Google Scholar]
- 21. Dimberg EL, Burns TM. Management of common neurologic conditions in sports. Clin Sports Med. 2005;24(3):637-662 [DOI] [PubMed] [Google Scholar]
- 22. Dimeo F, Bauer M, Varahram I, Proest G, Halter U. Benefits from aerobic exercise in patients with major depression: a pilot study. Br J Sports Med. 2001;35(2):114-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Endo K, Ichimaru K, Komagata M, Yamamoto K. Cervical vertigo and dizziness after whiplash injury. Eur Spine J. 2006;15(6):886-890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Enevoldsen EM, Jensen FT. Autoregulation and CO2 responses of cerebral blood flow in patients with acute severe head injury. J Neurosurg. 1978;48(5):689-703 [DOI] [PubMed] [Google Scholar]
- 25. Fann JR, Uomoto JM, Katon WJ. Sertraline in the treatment of major depression following mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2000;12(2):226-232 [DOI] [PubMed] [Google Scholar]
- 26. Friedman JM. Post-traumatic vertigo. Med Health R I. 2004;87(10):296-300 [PubMed] [Google Scholar]
- 27. Gaetz M, Weinberg H. Electrophysiological indices of persistent post-concussion symptoms. Brain Inj. 2000;14(9):815-832 [DOI] [PubMed] [Google Scholar]
- 28. Gagnon I, Galli C, Friedman D, Grilli L, Iverson GL. Active rehabilitation for children who are slow to recover following sport-related concussion. Brain Inj. 2009;23(12):956-964 [DOI] [PubMed] [Google Scholar]
- 29. Gall B, Parkhouse W, Goodman D. Heart rate variability of recently concussed athletes at rest and exercise. Med Sci Sports Exerc. 2004;36(8):1269-1274 [DOI] [PubMed] [Google Scholar]
- 30. Gall B, Parkhouse WS, Goodman D. Exercise following a sport induced concussion. Br J Sports Med. 2004;38(6):773-777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gebke KB. Mild traumatic brain injury. Curr Sports Med Rep. 2002;1(1):23-27 [DOI] [PubMed] [Google Scholar]
- 32. Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228-235 [PMC free article] [PubMed] [Google Scholar]
- 33. Golding EM, Robertson CS, Bryan RM., Jr The consequences of traumatic brain injury on cerebral blood flow and autoregulation: a review. Clin Exp Hypertens. 1999;21(4):299-332 [DOI] [PubMed] [Google Scholar]
- 34. Golding EM, Steenberg ML, Contant CF, Jr, Krishnappa I, Robertson CS, Bryan RM., Jr. Cerebrovascular reactivity to CO(2) and hypotension after mild cortical impact injury. Am J Physiol. 1999;277(4)(pt 2):H1457-H1466 [DOI] [PubMed] [Google Scholar]
- 35. Goldstein B, Toweill D, Lai S, Sonnenthal K, Kimberly B. Uncoupling of the autonomic and cardiovascular systems in acute brain injury. Am J Physiol. 1998;275(4)(pt 2):R1287-R1292 [DOI] [PubMed] [Google Scholar]
- 36. Gray TS. Autonomic neuropeptide connections of the amygdala. In: Tahe Y, Morley JE, Brown MR, eds. Neuropeptides and Stress. Berlin, Germany: Springer-Verlag; 1989:92-105 [Google Scholar]
- 37. Griesbach GS, Gomez-Pinilla F, Hovda DA. The upregulation of plasticity-related proteins following TBI is disrupted with acute voluntary exercise. Brain Res. 2004;1016(2):154-162 [DOI] [PubMed] [Google Scholar]
- 38. Griesbach GS, Hovda DA, Molteni R, Wu A, Gomez-Pinilla F. Voluntary exercise following traumatic brain injury: brain-derived neurotrophic factor upregulation and recovery of function. Neuroscience. 2004;125(1):129-139 [DOI] [PubMed] [Google Scholar]
- 39. Griffin SL, van Reekum R, Masanic C. A review of cholinergic agents in the treatment of neurobehavioral deficits following traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2003;15(1):17-26 [DOI] [PubMed] [Google Scholar]
- 40. Guskiewicz KM. Assessment of postural stability following sport-related concussion. Curr Sports Med Rep. 2003;2(1):24-30 [DOI] [PubMed] [Google Scholar]
- 41. Guskiewicz KM, Marshall SW, Bailes J, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57(4):719-726 [DOI] [PubMed] [Google Scholar]
- 42. Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903-909 [DOI] [PubMed] [Google Scholar]
- 43. Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2549-2555 [DOI] [PubMed] [Google Scholar]
- 44. Hamilton MT, Hamilton DG, Zderic TW. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev. 2004;32(4):161-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hanna-Pladdy B, Berry ZM, Bennett T, Phillips HL, Gouvier WD. Stress as a diagnostic challenge for postconcussive symptoms: sequelae of mild traumatic brain injury or physiological stress response. Clin Neuropsychol. 2001;15(3):289-304 [DOI] [PubMed] [Google Scholar]
- 46. Heitger MH, Jones RD, Macleod AD, Snell DL, Frampton CM, Anderson TJ. Impaired eye movements in post-concussion syndrome indicate suboptimal brain function beyond the influence of depression, malingering or intellectual ability. Brain. 2009;132(pt 10):2850-2870 [DOI] [PubMed] [Google Scholar]
- 47. Helmick K. Cognitive rehabilitation for military personnel with mild traumatic brain injury and chronic post-concussional disorder: results of April 2009 consensus conference. NeuroRehabilitation. 2010;26(3):239-255 [DOI] [PubMed] [Google Scholar]
- 48. Hicks RR, Smith DH, Lowenstein DH, Saint Marie R, McIntosh TK. Mild experimental brain injury in the rat induces cognitive deficits associated with regional neuronal loss in the hippocampus. J Neurotrauma. 1993;10(4):405-414 [DOI] [PubMed] [Google Scholar]
- 49. Ho MR, Bennett TL. Efficacy of neuropsychological rehabilitation for mild-moderate traumatic brain injury. Arch Clin Neuropsychol. 1997;12(1):1-11 [PubMed] [Google Scholar]
- 50. Hovda DA, Lee SM, Smith ML, et al. The neurochemical and metabolic cascade following brain injury: moving from animal models to man. J Neurotrauma. 1995;12(5):903-906 [DOI] [PubMed] [Google Scholar]
- 51. Hovda DA, Yoshino A, Kawamata T, Katayama Y, Becker DP. Diffuse prolonged depression of cerebral oxidative metabolism following concussive brain injury in the rat: a cytochrome oxidase histochemistry study. Brain Res. 1991;567(1):1-10 [DOI] [PubMed] [Google Scholar]
- 52. Iverson GL. Misdiagnosis of the persistent postconcussion syndrome in patients with depression. Arch Clin Neuropsychol. 2006;21(4):303-310 [DOI] [PubMed] [Google Scholar]
- 53. Iverson GL, Gaetz M, Lovell MR, Collins MW. Cumulative effects of concussion in amateur athletes. Brain Inj. 2004;18(4):1. [DOI] [PubMed] [Google Scholar]
- 54. Iverson GL, Gaetz M, Lovell MR, Collins MW. Cumulative effects of concussion in amateur athletes. Brain Inj. 2004;18(5):433-443 [DOI] [PubMed] [Google Scholar]
- 55. Johnston KM, McCrory P, Mohtadi NG, Meeuwisse W. Evidence-based review of sport-related concussion: clinical science. Clin J Sport Med. 2001;11(3):150-159 [DOI] [PubMed] [Google Scholar]
- 56. Junger EC, Newell DW, Grant GA, et al. Cerebral autoregulation following minor head injury. J Neurosurg. 1997;86(3):425-432 [DOI] [PubMed] [Google Scholar]
- 57. Katayama Y, Becker DP, Tamura T, Hovda DA. Massive increases in extracellular potassium and the indiscriminate release of glutamate following concussive brain injury. J Neurosurg. 1990;73(6):889-900 [DOI] [PubMed] [Google Scholar]
- 58. Kawamata T, Katayama Y, Hovda DA, Yoshino A, Becker DP. Administration of excitatory amino acid antagonists via microdialysis attenuates the increase in glucose utilization seen following concussive brain injury. J Cereb Blood Flow Metab. 1992;12(1):12-24 [DOI] [PubMed] [Google Scholar]
- 59. King ML, Lichtman SW, Seliger G, Ehert FA, Steinberg JS. Heart-rate variability in chronic traumatic brain injury. Brain Inj. 1997;11(6):445-453 [DOI] [PubMed] [Google Scholar]
- 60. Korn A, Golan H, Melamed I, Pascual-Marqui R, Friedman A. Focal cortical dysfunction and blood-brain barrier disruption in patients with postconcussion syndrome. J Clin Neurophysiol. 2005;22(1):1-9 [DOI] [PubMed] [Google Scholar]
- 61. Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39(5):364-377 [DOI] [PubMed] [Google Scholar]
- 62. Kutcher JS, Eckner JT. At-risk populations in sports-related concussion. Curr Sports Med Rep. 2010;9(1):16-20 [DOI] [PubMed] [Google Scholar]
- 63. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378 [DOI] [PubMed] [Google Scholar]
- 64. Lau B, Lovell MR, Collins MW, Pardini J. Neurocognitive and symptom predictors of recovery in high school athletes. Clin J Sport Med. 2009;19(3):216-221 [DOI] [PubMed] [Google Scholar]
- 65. Leddy JJ, Baker JG, Kozlowski K, Bisson L, Willer B. Reliability of a graded exercise test for assessing recovery from concussion. Clin J Sport Med. 2011;21(2):89-94 [DOI] [PubMed] [Google Scholar]
- 66. Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med. 2010;20(1):21-27 [DOI] [PubMed] [Google Scholar]
- 67. Leddy JJ, Kozlowski K, Fung M, Pendergast DR, Willer B. Regulatory and autoregulatory physiological dysfunction as a primary characteristic of post concussion syndrome: Implications for treatment. Neurorehabilitation. 2007;22(3):199-205 [PubMed] [Google Scholar]
- 68. Levin HS, Mattis S, Ruff RM, et al. Neurobehavioral outcome following minor head injury: a three-center study. J Neurosurg. 1987;66(2):234-243 [DOI] [PubMed] [Google Scholar]
- 69. Levy M, Koeppen B, Stanton B. Berne and Levy Principles of Physiology. Philadelphia, PA: Elsevier Mosby; 2006 [Google Scholar]
- 70. Longhi L, Saatman KE, Fujimoto S, et al. Temporal window of vulnerability to repetitive experimental concussive brain injury. Neurosurgery. 2005;56(2):364-374 [DOI] [PubMed] [Google Scholar]
- 71. Lovell MR, Collins MW, Iverson GL, et al. Recovery from mild concussion in high school athletes. J Neurosurgery. 2003;98(2):296-301 [DOI] [PubMed] [Google Scholar]
- 72. Luis CA, Vanderploeg RD, Curtiss G. Predictors of postconcussion symptom complex in community dwelling male veterans. J Int Neuropsychol Soc. 2003;9(7):1001-1015 [DOI] [PubMed] [Google Scholar]
- 73. Majerske CW, Mihalik JP, Ren D, et al. Concussion in sports: postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008;43(3):265-274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. McCauley SR, Boake C, Levin HS, Contant CF, Song JX. Postconcussional disorder following mild to moderate traumatic brain injury: anxiety, depression, and social support as risk factors and comorbidities. J Clin Exp Neuropsychol. 2001;23(6):792-808 [DOI] [PubMed] [Google Scholar]
- 75. McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556-2563 [DOI] [PubMed] [Google Scholar]
- 76. McCrory P. Does second impact syndrome exist? Clin J Sport Med. 2001;11(3):144-149 [DOI] [PubMed] [Google Scholar]
- 77. McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004 Clin J Sport Med. 2005;15(2):48-55 [DOI] [PubMed] [Google Scholar]
- 78. McCrory P, Johnston KM, Mohtadi NG, Meeuwisse W. Evidence-based review of sport-related concussion: basic science. Clin J Sport Med. 2001;11(3):160-165 [DOI] [PubMed] [Google Scholar]
- 79. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med 2009;19(3):185-200 [DOI] [PubMed] [Google Scholar]
- 80. Mittenberg W, Canyock EM, Condit D, Patton C. Treatment of post-concussion syndrome following mild head injury. J Clin Exp Neuropsychol. 2001;23(6):829-836 [DOI] [PubMed] [Google Scholar]
- 81. Mittenberg W, Tremont G, Zielinski RE, Fichera S, Rayls KR. Cognitive-behavioral prevention of postconcussion syndrome. Arch Clin Neuropsychol. 1996;11(2):139-145 [PubMed] [Google Scholar]
- 82. Napadow V, Dhond R, Conti G, Makris N, Brown EN, Barbieri R. Brain correlates of autonomic modulation: combining heart rate variability with fMRI. Neuroimage. 2008;42(1):169-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Nilsson P, Hillered L, Ponten U, Ungerstedt U. Changes in cortical extracellular levels of energy-related metabolites and amino acids following concussive brain injury in rats. J Cereb Blood Flow Metab. 1990;10(5):631-637 [DOI] [PubMed] [Google Scholar]
- 84. Ommaya AK, Gennarelli TA. Cerebral concussion and traumatic unconsciousness: correlation of experimental and clinical observations of blunt head injuries. Brain. 1974;97(4):633-654 [DOI] [PubMed] [Google Scholar]
- 85. Oppenheimer DR. Microscopic lesions in the brain following head injury. J Neurol Neurosurg Psychiatry. 1968;31(4):299-306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Palmese CA, Raskin SA. The rehabilitation of attention in individuals with mild traumatic brain injury, using the APT-II programme. Brain Inj. 2000;14(6):535-548 [DOI] [PubMed] [Google Scholar]
- 87. Peterson CL, Ferrara MS, Mrazik M, Piland S, Elliott R. Evaluation of neuropsychological domain scores and postural stability following cerebral concussion in sports. Clin J Sport Med. 2003;13(4):230-237 [DOI] [PubMed] [Google Scholar]
- 88. Pomeranz B, Macaulay RJ, Caudill MA, et al. Assessment of autonomic function in humans by heart rate spectral analysis. Am J Physiol. 1985;248(1)(pt 2):H151-H153 [DOI] [PubMed] [Google Scholar]
- 89. Ponsford J, Willmott C, Rothwell A, et al. Cognitive and behavioral outcome following mild traumatic head injury in children. J Head Trauma Rehabil. 1999;14(4):360-372 [DOI] [PubMed] [Google Scholar]
- 90. Ponsford J, Willmott C, Rothwell A, et al. Factors influencing outcome following mild traumatic brain injury in adults. J Int Neuropsychol Soc. 2000;6(5):568-579 [DOI] [PubMed] [Google Scholar]
- 91. Ponsford J, Willmott C, Rothwell A, et al. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics. 2001;108(6):1297-1303 [DOI] [PubMed] [Google Scholar]
- 92. Ponsford J, Willmott C, Rothwell A, et al. Impact of early intervention on outcome following mild head injury in adults. J Neurol Neurosurg Psychiatry. 2002;73(3):330-332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Preiss-Farzanegan SJ, Chapman B, Wong TM, Wu J, Bazarian JJ. The relationship between gender and postconcussion symptoms after sport-related mild traumatic brain injury. PM R. 2009;1(3):245-253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Randolph C, McCrea M, Barr WB. Is neuropsychological testing useful in the management of sport-related concussion? J Athl Train. 2005;40(3):139-152 [PMC free article] [PubMed] [Google Scholar]
- 95. Rimel RW, Giordani B, Barth JT, Boll TJ, Jane JA. Disability caused by minor head injury. Neurosurgery. 1981;9(3):221-228 [PubMed] [Google Scholar]
- 96. Rohling ML, Faust ME, Beverly B, Demakis G. Effectiveness of cognitive rehabilitation following acquired brain injury: a meta-analytic re-examination of Cicerone et al’s (2000, 2005) systematic reviews. Neuropsychology. 2009;23(1):20-39 [DOI] [PubMed] [Google Scholar]
- 97. Saija A, Hayes RL, Lyeth BG, Dixon CE, Yamamoto T, Robinson SE. The effect of concussive head injury on central cholinergic neurons. Brain Res. 1988;452(1-2):303-311 [DOI] [PubMed] [Google Scholar]
- 98. Sano K, Yoshioka M, Ogashiwa M, et al. Autonomic, somatomotor and electroencephalographic responses upon stimulation of the hypothalamus and the rostral brain stem in man. Confin Neurol. 1967;29(2):257-261 [DOI] [PubMed] [Google Scholar]
- 99. Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A. Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a systematic review. JAMA. 2007;298(12):1429-1438 [DOI] [PubMed] [Google Scholar]
- 100. Segalowitz SJ, Mahaney P, Santesso DL, MacGregor L, Dywan J, Willer B. Retest reliability in adolescents of a computerized neuropsychological battery used to assess recovery from concussion. NeuroRehabilitation. 2007;22(3):243-251 [PubMed] [Google Scholar]
- 101. Shetter AG, Demakas JJ. The pathophysiology of concussion: a review. Adv Neurol. 1979;22:5-14 [PubMed] [Google Scholar]
- 102. Stalnacke BM, Bjornstig U, Karlsson K, Sojka P. One-year follow-up of mild traumatic brain injury: post-concussion symptoms, disabilities and life satisfaction in relation to serum levels of S-100B and neurone-specific enolase in acute phase. J Rehabil Med. 2005;37(5):300-305 [DOI] [PubMed] [Google Scholar]
- 103. Strebel S, Lam AM, Matta BF, Newell DW. Impaired cerebral autoregulation after mild brain injury. Surg Neurol. 1997;47(2):128-131 [DOI] [PubMed] [Google Scholar]
- 104. Taylor AR. Post-concussional sequelae. Br Med J. 1967;3(5557):67-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Taylor AR, Bell TK. Slowing of cerebral circulation after concussional head injury: a controlled trial. Lancet. 1966;2(7456):178-180 [DOI] [PubMed] [Google Scholar]
- 106. Teasdale TW, Engberg A. Duration of cognitive dysfunction after concussion, and cognitive dysfunction as a risk factor: a population study of young men. BMJ. 1997;315(7108):569-572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Thomas M, Haas TS, Doerer JJ, et al. Epidemiology of sudden death in young, competitive athletes due to blunt trauma. Pediatrics. 2011;128(1): e1-e8 [DOI] [PubMed] [Google Scholar]
- 108. Tiersky LA, Anselmi V, Johnston MV, et al. A trial of neuropsychologic rehabilitation in mild-spectrum traumatic brain injury. Arch Phys Med Rehabil. 2005;86(8):1565-1574 [DOI] [PubMed] [Google Scholar]
- 109. Treleaven J, Jull G, Sterling M. Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med. 2003;35(1):36-43 [DOI] [PubMed] [Google Scholar]
- 110. Tyler GS, McNeely HE, Dick ML. Treatment of post-traumatic headache with amitriptyline. Headache. 1980;20(4):213-216 [DOI] [PubMed] [Google Scholar]
- 111. Vagnozzi R, Signoretti S, Cristofori L, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain. 2010;133(11):3232-3242 [DOI] [PubMed] [Google Scholar]
- 112. Vagnozzi R, Signoretti S, Tavazzi B, et al. Temporal window of metabolic brain vulnerability to concussion: a pilot 1H-magnetic resonance spectroscopic study in concussed athletes. Part III. Neurosurgery. 2008;62(6):1286-1295 [DOI] [PubMed] [Google Scholar]
- 113. van Ravenswaaij-Arts CM, Kollee LA, Hopman JC, Stoelinga GB, van Geijn HP. Heart rate variability. Ann Intern Med. 1993;118(6):436-447 [DOI] [PubMed] [Google Scholar]
- 114. Wade DT, King NS, Wenden FJ, Crawford S, Caldwell FE. Routine follow up after head injury: a second randomised controlled trial. J Neurol Neurosurg Psychiatry. 1998;65(2):177-183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Ward AA., Jr The physiology of concussion. Clin Neurosurg. 1964;12:95-111 [DOI] [PubMed] [Google Scholar]
- 116. Wilde EA, McCauley SR, Hunter JV, et al. Diffusion tensor imaging of acute mild traumatic brain injury in adolescents. Neurology. 2008;70(12):948-955 [DOI] [PubMed] [Google Scholar]
- 117. Willer B, Leddy JJ. Management of concussion and post-concussion syndrome. Curr Treat Options Neurol. 2006;8(5):415-426 [DOI] [PubMed] [Google Scholar]
- 118. Yamaki T, Murakami N, Iwamoto Y, et al. Cognitive dysfunction and histological findings in rats with chronic-stage contusion and diffuse axonal injury. Brain Res Brain Res Protoc. 1998;3(1):100-106 [DOI] [PubMed] [Google Scholar]