Abstract
Context:
There is a wide spectrum of hamstring-related injuries that can occur in the athlete. Accurate diagnosis is imperative to prevent delayed return to sport, injury recurrence, and accurate clinical decision making regarding the most efficacious treatment.
Evidence Acquisition:
This review highlights current evidence related to the diagnosis and treatment of hamstring-related injuries in athletes. Data sources were limited to peer-reviewed publications indexed in MEDLINE from 1988 through May 2011.
Results:
An accurate diagnostic process for athletes with posterior thigh–related complaints should include a detailed and discriminative history, followed by a thorough clinical examination. Diagnostic imaging should be utilized when considering hamstring avulsion or ischial apophyseal avulsion. Diagnostic imaging may also be needed to further define the cause of referred posterior thigh pain.
Conclusions:
Differentiating acute hamstring strains, hamstring tendon avulsions, ischial apophyseal avulsions, proximal hamstring tendinopathies, and referred posterior thigh pain is critical in determining the most appropriate treatment and expediting safe return to play.
Keywords: athletes, tendinopathy, avulsion, referred posterior thigh pain, ischial apophyseal avulsions
Acute hamstring strains, complete and partial proximal hamstring tendon avulsions, ischial apophyseal avulsions, hamstring tendinopathy, and referred posterior thigh pain make up the wide spectrum of hamstring-related injuries among athletes.
Acute Hamstring Strains
Acute hamstring strains occur with sudden onset19,52,56 in high-speed skilled movements and in end-range hip flexion with knee extension stretching movements.30 Data from a National Football League team was published for preseason training camp from 1998 to 2007. Acute hamstring strains were the second-most common injury, second only to knee sprains. Injury rates varied by position, with acute strains being the most common injury among running backs, defensive backs, and wide receivers, accounting for 22%, 14%, and 12% of injuries in those groups, respectively.20 These positions require sprinting with frequent directional changes and acceleration and deceleration. Hamstring strains are one of the most common injuries in track and field, soccer, rugby, and Australian Rules football.* Dance, which requires extensive lengthening of the hamstrings, also produces acute hamstring strains.3,4
The injury typically occurs in the bicep femoris and along an intramuscular tendon and in the adjacent muscle fibers.6,34,56,59 Injuries occur in the semimembranosus, along the proximal free tendon, in slower speed injuries.6-8
The most significant risk factor for an acute hamstring strain is a previous hamstring strain.19,24,29,31,42,63 Athletes with a previous hamstring strain are twice as likely to sustain a hamstring strain.19 One study of 74 soccer players training 6 to 7 days per week for a 10-month season, found that a previous hamstring strain was not a risk factor for future hamstring strain.21 Age,24,26,29,58 decreased hip flexor flexibility,24 hamstring strength deficits or imbalances,16,21,49 and higher body weight23 are risk factors for hamstring strains. Deficits in hamstring flexibility have not been shown to be a risk factor for acute hamstring strains.24,26,27
Clinical Evaluation
During clinical examination, athletes with an acute hamstring strain will likely demonstrate altered gait mechanics,59 local tenderness to palpation at the site of injury,36,52 pain with resisted knee flexion and/or hip extension,36,52 and pain with passive hip flexion with knee extension.36,52
An athlete’s ability to return to sport may be predicted by the ability to walk without pain. Elite Australian Rules football players taking more than 1 day to return to pain-free walking were 4 times more likely to take longer than 3 weeks to return to sport when compared with those walking pain-free within 1 day.59
Active knee extension deficit was not a significant predictor of time to return to sport or injury recurrence.59 Hamstring stretching 1 or 4 times per day in athletes with acute hamstring injuries and active knee extension deficits greater than 10° showed that stretching 4 times per day returned range of motion to normal values in a mean time of 7.3 days versus 5.6 days.37 The time required for return to sport was also statistically significantly, 15.0 versus 13.3 days.37 A major limitation of this study is that no reinjury data were provided, especially in light of the relatively small clinical difference in return to sport time.
To date, functional testing has not demonstrated a discriminating ability for return-to-play decision making following hamstring injury. Significant differences were not found in hop for height, hop for distance or crossover hop tests in comparing patients with acute hamstring strains who reinjured and those who did not.52 Hop tests likely do not represent the most provocative movements for an athlete recovering from an acute hamstring strain.
The active hamstring flexibility test was developed to determine safe return to sport for athletes with an acute hamstring strain.5 The athlete is positioned supine with one leg strapped to a plinth and with the other “active” leg in a knee extension splint. This leg is taken through a ballistic straight-leg raise to maximal range of motion. Hip range of motion is compared with the uninjured side, while apprehension and insecurity are monitored. Before the active hamstring flexibility test, patients must demonstrate normal hamstring strength on manual muscle testing, prone, at 90°, 45°, and 0° of knee flexion. Compared with the injured leg, the uninjured leg demonstrated an average increase in active flexibility of 23%. Median values based on a visual analog scale (0-100) for insecurity was 52 for the injured leg (range, 28-98) and 0 for the uninjured leg. Although these measures are reliable, there are no data yet to determine if these differences are predictive for reinjury or player performance.5 If athletes are insecure about their return to sport, the test should be repeated in 2 weeks and return to sport should be delayed.5
Diagnostic Evaluation
Some studies have shown that magnetic resonance imaging (MRI) parameters defining the size of injury correlate to time lost from sport.15,50,53 Another study predicted comparable return from a clinical examination.50 Reinjury risk in the same season34,57 was not predicted by percentage transverse cross-sectional area and volume, but was predictive of reinjury in the subsequent season in Australian Rules football players.57
Treatment
One of the most challenging and frustrating aspects of acute hamstring injuries is the high rate of injury recurrence, especially in the first few weeks of return to sport.36,43,52,59 Acute hamstring strains in the previous season were almost 20 times more likely to suffer a reinjury within the first 3 weeks of return to play when compared with acute hamstring strains without previous injury.59 Recurrent injuries also have a longer convalescent period.11
Recent evidence suggests that hamstring strain recurrence rates can be lowered through a progressive agility and trunk stabilization program.52 A prospective study showed that 70% of athletes who completed a traditional rehabilitation program (hamstring stretching and strengthening exercises) suffered a reinjury in the subsequent year of competition. Only 7.7% of those who completed the progressive agility and trunk stabilization program were reinjured.52 There is a lack of evidence to support stretching as a valuable treatment modality for prevention of injury recurrence or return of player performance.52
As stated above, one study found that an active knee extension deficit was not a significant predictor of time to return to sport or injury recurrence.59 Injured athletes may demonstrate a significant deficit in active ballistic flexibility with no difference in slow passive flexibility.5
The length of muscle tendon for optimum tension can shorten after a hamstring injury, thus making muscle more susceptible to reinjury.9 Scar tissue forms and links up with muscle fibers, increasing the passive stiffness of the muscle tendon unit and making it more susceptible to injury during large eccentric forces. Optimum tension can be altered by eccentric training,10,44 but there is no proof that eccentric strengthening during the rehabilitation of acute hamstring strains will lengthen injured muscle. Several studies have found a positive benefit for injury prevention using eccentric hamstring strengthening;1,2,11,25 Nordic curls do develop hamstring strength effectively.38
Hamstring Tendon Avulsions
Complete and partial avulsions of the proximal hamstring tendon from the ischial origin are common during sporting activities that generate forceful hip flexion moments while the knee is extending.14,32,33,48,60 Waterskiing and bull riding are common mechanisms for this injury pattern.14,17,47,60
Clinical and Diagnostic Evaluation
Individuals with avulsion of the proximal hamstring tendon often present with a significant gait abnormality, unable to fully extend and bear weight on the involved side. Large hematomas with palpable defects and significant ecchymosis often result from this injury.33,48,60 Active or resisted knee flexion may even produce a distal bulge in the retracted muscles.48 Occasionally, a large hematoma may also cause compression on the sciatic nerve, resulting in tingling sensations in the posterior thigh.33
Treatment
These injuries are often treated with open surgical repair, if there is a complete avulsion of all 3 tendons or disruption of the conjoint tendon with greater than 2.5 to 3 cm of retraction (Figure 1).28,33 There may be need for hematoma evacuation and/or sciatic neurolysis, depending on timing and the findings at the time of surgery (Figures 2 and 3).14,28,32,33,60
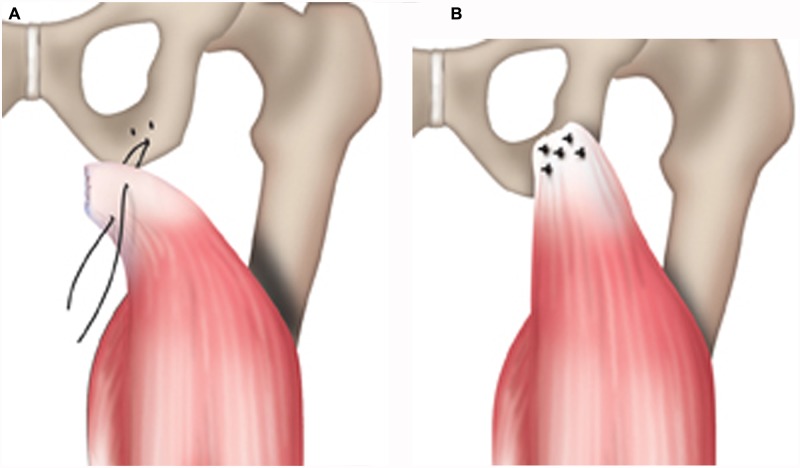
Figure 1.
A, suture anchors in the ischial tuberosity, with Panacryl, Ethibond, or synthetic braided sutures; B, proximal tendon approximated to the ischial tuberosity and secured via suture anchors and suture fixation.
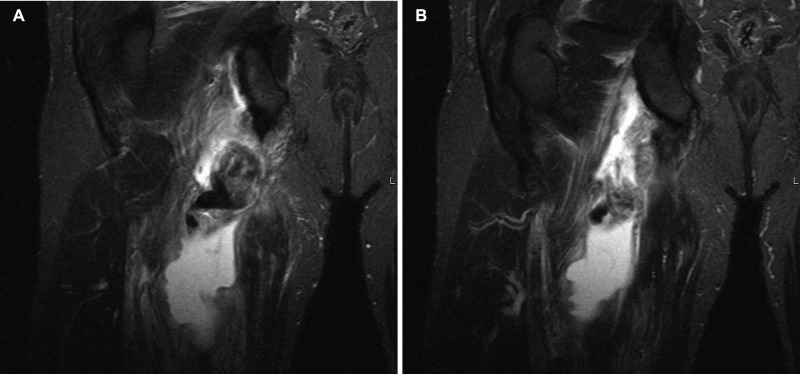
Figure 2.
Coronal inversion-recovery images of illustrative case for hamstring tendon avulsion. Note the fluid extending all the way to the ischial tuberosity and the dark tendon stumps retracting inferior.
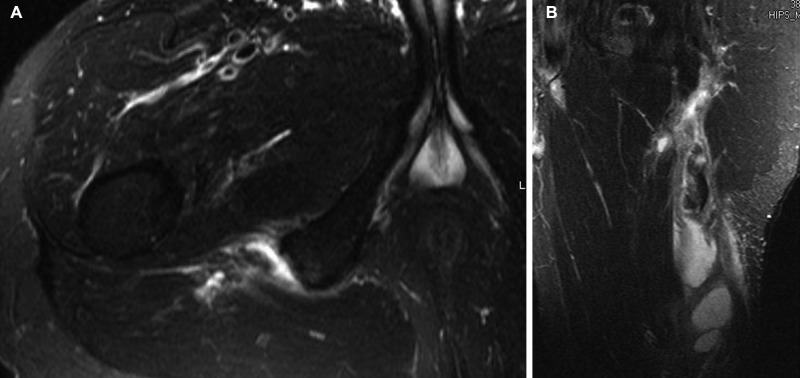
Figure 3.
Axial T2 images (A) and sagittal inversion-recovery images (B) of illustrative case for hamstring tendon avulsion. Note the fluid extending all the way to the ischial tuberosity on the sagittal view and the loss of conjoint tendon and semimembranosus on the axial view.
Most postoperative rehabilitation programs start with gentle range of motion and gait training exercises while protecting the repair to allow adequate healing during the first 6 weeks by avoiding hamstring stretching or significant tension.48,60 The weightbearing status is generally progressed from touchdown weightbearing or nonweightbearing to full weightbearing over the course of 6 to 8 weeks.33,48 This is followed by a progressive supervised strengthening program.
Return to sport after open surgical repair likely depends on the nature of the sport, severity of initial injury, timeliness of surgical intervention, and compliance with the postoperative rehabilitation program, with 65% to 80% of athletes able to return in some capacity.14,28,32,33,60
The University of Wisconsin Sports Medicine program utilizes a 4-phase postoperative rehabilitation program. Phase 1 consists of range of motion and gait training exercises while protecting the repair to allow adequate healing over 6 weeks, followed by a progressive supervised strengthening program. Phase 2 and 3 progressions emphasize speed and amplitude of movement, as well as force distribution. Early in the strengthening phase, most hip and knee exercises are done with both legs in a simultaneous short arc of motion. Late in phase 3, most exercises are single leg. In the final phase of rehabilitation, the focus shifts to high-speed movement and the development of power for the return to sport.
When patients are within 25% strength on the uninvolved side, we allow progression to sport-specific rehabilitation. Specific exercises in this phase include single-leg dead lifts with dumbbell rotation punches, medicine ball explosive throws, partial drop Nordic curls, single-leg bridging on a physioball, skating bounds, core planks, and an interval skating program. An isokinetic ratio of high-speed quadriceps concentric strength to low-speed hamstring eccentric strength can be used to assess return to sport.
Ischial Apophyseal Avulsions
In young athletes, sprinting and stretching may cause an ischial apophyseal avulsion.28,62 It is most likely to occur early (13-16 years), when the apophysis has the least amount of bony bridging or fusion.28,51,62
Clinical and Diagnostic Evaluation
Patients with ischial apophyseal avulsion have ischial tenderness and pain, especially when sitting.28 An anteroposterior radiograph of the pelvis can demonstrate this avulsion (Figure 4).28 Computed tomography and magnetic resonance scans may be utilized for further evaluation of healing or surgical planning (Figures 5-8).
Figure 4.

Radiograph, anteroposterior view, demonstrating a right ischial apophyseal avulsion.
Figure 5.

Computed tomography scan, axial view, demonstrating a right ischial apophyseal avulsion with approximately 10 mm of displacement.
Figure 8.

Coronal slice of T1 magnetic resonance scan demonstrating a right ischial apophyseal avulsion.
Figure 6.

Computed tomography scan, sagittal view, demonstrating a right ischial apophyseal avulsion.
Figure 7.
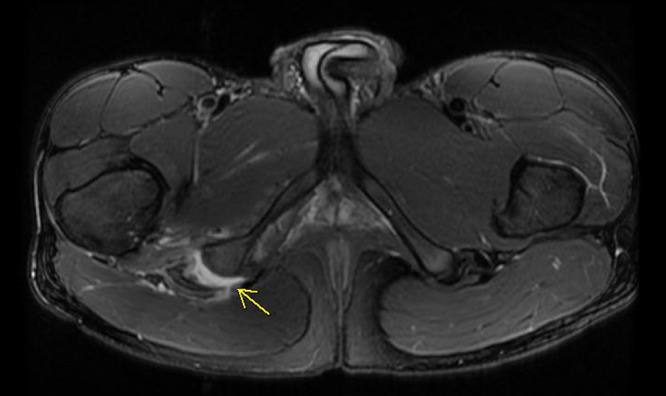
Axial slice of T1 magnetic resonance scan demonstrating a right ischial apophyseal avulsion.
Treatment
Ischial apophyseal avulsion fractures that are displaced less than 1 cm can be treated conservatively by avoiding hamstring stretching and tension for several weeks to prevent further displacement and allow healing.28 Surgical fixation may be indicated if the displacement is greater than 1 to 1.5 cm or for chronic nonunion cases (Figure 9).28
Figure 9.

Postoperative anteroposterior pelvis radiograph showing the internal fixation of the ischial tuberosity avulsion fracture.
Proximal Hamstring Tendinopathy
Proximal hamstring tendinopathy was initially referred to as “hamstring syndrome” with symptoms after direct compression on the sciatic nerve.45 Degenerative tendinopathy may include sciatic nerve compression, traction, or irritation.13 The onset of proximal hamstring tendinopathy is often insidious after partial hamstring tears.13,35,45,46,64 Initially described in sprinters,45 recent evidence suggests that it is more common in long- and middle-distance runners, soccer players, and cross-country skiers.13,22,35,45 This condition affects middle-age male athletes most frequently (29-37 years).35,64,65 Pain is experienced during activity and with sitting on firm surfaces or prolonged sitting in the proximal hamstring region.13,22,35,45
Clinical and Diagnostic Evaluation
Most patients with proximal hamstring tendinopathy have tenderness to palpation on ischial tuberosity and proximal attachment13,22,35,45,64 and near-normal hamstrings and gluteals with manual muscle testing. There is often local discomfort with flexibility testing, even in the absence of a significant deficit.35,45 The hamstring-stretch test, in which the examiner rapidly flexes the hip and extends the knee of a patient in supine, is positive if it evokes pain in the proximal hamstring region.13 Two other tests have a similar purpose: the Puranen-Orava test quickly stretches the hamstrings from a standing position45 and the bent-knee stretch test stretches the proximal hamstrings in supine.22
MRI findings may include tendon thickening, partial tearing, intrasubstance signal heterogeneity, and/or reactive edema of the ischial tuberosity.13,22,35,65 Increased signal within the tendon is usually present on T 1-weighted images without significant abnormality on T 2-weighted images; focal partial tears have increased signal in the tendon in both sequences.22 Ultrasound imaging is becoming increasingly popular. Proposed advantages for imaging include decreased cost, real-time imaging, and spatial resolution allowing for targeted injection therapies.65 Disadvantages include the inability to visualize bone marrow edema and potentially decreased sensitivity.65
Treatment
Treatments have included eccentric strengthening or stretching, anti-inflammatory medications (oral or injectable), shockwave therapy, and regenerative therapies, such as autologous injections and surgical debridement or tenotomy.
Pelvic alignment, soft tissue mobilization, hamstring stretching, and progressive core and hamstring strengthening may improve symptoms22; however, surgery may be indicated.13,35,45,64
There is limited evidence for shockwave therapy13; a recent randomized controlled trial demonstrated potential benefit. Forty professional athletes with proximal hamstring tendinopathy were divided into 2 groups, one receiving shockwave therapy and 1 receiving nonsteroidal anti-inflammatory drugs, ultrasound, and physical therapy exercises. After 3 months, 80% of the athletes in the shockwave therapy group were able to return to their preinjury level of sport, compared with none of the athletes in the control group.13 There was also a significant reduction in pain in the shockwave therapy group.13
In a group of patients with high hamstring tendinopathy that received a corticosteroid injection, only 23% obtained symptomatic relief lasting longer than 6 months.65 Seventy-one percent of those that followed up did return to presymptom level of sport; only 38 of 65 returned for follow-up.
Regenerative therapies consist primarily of growth factors in autologous whole blood or platelet-rich plasma. A recent review concluded that there was strong evidence that autologous blood injections do not decrease pain or improve function when compared with other therapies. There was only limited evidence that platelet-rich plasma injections are beneficial for the treatment of tendinopathy.18 These studies did not evaluate proximal hamstring tendinopathy.
When conservative attempts fail, surgical options are often sought. A transverse tenotomy of the thickened semimembranosus tendon has been utilized, 3 to 4 cm distal to the origin with subsequent suture fixation to the bicep femoris.35 Of 90 patients, 80 had good to excellent results and were able to return to previous sports at an average of 5 months.35 Separating the proximal hamstring tendons to relieve tension may also elevate symptoms; 52 of 59 patients were able to return to running without pain.45
Referred Posterior Thigh Pain
A subset of athletes have referred pain in the posterior thigh without local injury to the hamstring muscle complex.30 Causes of posterior thigh pain include piriformis syndrome, lumbar disc herniation or lumbar facet syndrome causing nerve root compression, sacroiliac joint dysfunction, and spondylogenic lesions.12,22,45,46 Patients with referred posterior thigh pain will commonly have variable symptoms proximal to the ischial tuberosity and distal to the knee. These symptoms may vary, including muscle cramping and tightness, numbness, tingling, pain, and shooting pain.12,22
Clinical and Diagnostic Evaluation
Clinical examination may reveal reduced range of motion or pain provocation with movement of the lumbar spine, tenderness or stiffness over the lumbar intervertebral or sacral iliac joints, a positive slump test, or a positive lumbar quadrant test.12 MRI-negative hamstring injuries should not be confused with referred posterior thigh pain. Hamstring strains may not demonstrate T2 hyperintensity on MRI exam.50,58 These athletes usually return to sport quickly.
Illustrative Case
A 34-year-old woman presented with a 1-year gradual hamstring symptoms on the left side. She described a dull pain in the posterior thigh with sitting and lateral lower leg discomfort, but she did not have low back pain. About 30 minutes of running, her left leg would feel weak, and she developed pain (4/10) in the posterior thigh and distal gluteal area. She stated that she would have a gradual increase in tightness, especially after activity and running. On clinical examination, she had a positive lower limb tension test and slump sit test on the left. Active knee extension testing demonstrated symmetrical hamstring flexibility bilaterally. Manual muscle testing showed 5 of 5 strength for medial and lateral hamstring, gluteus maximus, and medial and lateral hip rotators.
Based on history and clinical examination, referred posterior thigh pain was suspected. MRI showed a L5-S1 central disc protrusion with contact of the left S1 nerve roots. She underwent 3 S1 epidural steroid injections and 6 weeks of physical therapy. These treatments provided significant improvement, and she completed an Ironman Triathlon 2 months later.
Conclusion
An accurate diagnosis is an essential component in providing appropriate treatment and guidance for return to sport for patients with hamstring-related injuries.
Footnotes
References
- 1. Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1):40-48 [DOI] [PubMed] [Google Scholar]
- 2. Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13(4):244-250 [DOI] [PubMed] [Google Scholar]
- 3. Askling C, Lund H, Saartok T, Thorstensson A. Self-reported hamstring injuries in student-dancers. Scand J Med Sci Sports. 2002;12(4):230-235 [DOI] [PubMed] [Google Scholar]
- 4. Askling C, Tengvar M, Saartok T, Thorstensson A. Sports related hamstring strains: two cases with different etiologies and injury sites. Scand J Med Sci Sports. 2000;10(5):304-307 [DOI] [PubMed] [Google Scholar]
- 5. Askling CM, Nilsson J, Thorstensson A. A new hamstring test to complement the common clinical examination before return to sport after injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(12): 1798-1803 [DOI] [PubMed] [Google Scholar]
- 6. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2006;35(2):197-206 [DOI] [PubMed] [Google Scholar]
- 7. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med. 2007;35(10):1716-1724 [DOI] [PubMed] [Google Scholar]
- 8. Askling CM, Tengvar M, Saartok T, Thorstensson A. Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. Am J Sports Med. 2008;36(9):1799-1804 [DOI] [PubMed] [Google Scholar]
- 9. Brockett CL, Morgan DL, Proske U. Human hamstring muscles adapt to eccentric exercise by changing optimum length. Med Sci Sports Exerc. 2001;33(5):783-790 [DOI] [PubMed] [Google Scholar]
- 10. Brockett CL, Morgan DL, Proske U. Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc. 2004;36(3):379-387 [DOI] [PubMed] [Google Scholar]
- 11. Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297-1306 [DOI] [PubMed] [Google Scholar]
- 12. Brunker P, Kahn K, eds. Clinical Sports Medicine. 2nd ed. Sydney, Australia: McGraw-Hill; 2001 [Google Scholar]
- 13. Cacchio A, Rompe JD, Furia JP, Susi P, Santilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med. 2011;39(1):146-153 [DOI] [PubMed] [Google Scholar]
- 14. Chakravarthy J, Ramisetty N, Pimpalnerkar A, Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005;39(8):569-572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183(4):975-984 [DOI] [PubMed] [Google Scholar]
- 16. Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;6(8):1469-1475 [DOI] [PubMed] [Google Scholar]
- 17. Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26(6):785-788 [DOI] [PubMed] [Google Scholar]
- 18. de Vos RJ, van Veldhoven PL, Moen MH, Weir A, Tol JL, Maffulli N. Autologous growth factor injections in chronic tendinopathy: a systematic review. Br Med Bull. 2010;95:63-77 [DOI] [PubMed] [Google Scholar]
- 19. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for hamstring injuries among male soccer players: a prospective cohort study. Am J Sports Med. 2010;38(6):1147-1153 [DOI] [PubMed] [Google Scholar]
- 20. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597-1603 [DOI] [PubMed] [Google Scholar]
- 21. Fousekis K, Tsepis E, Poulmedis P, Athanasopoulos S, Vagenas G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players. Br J Sports Med. 2010;45(9):709-714 [DOI] [PubMed] [Google Scholar]
- 22. Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. Phys Sportsmed. 2005;33(5):32-43 [DOI] [PubMed] [Google Scholar]
- 23. Gabbe BJ, Bennell KL, Finch CF. Why are older Australian football players at greater risk of hamstring injury? J Sci Med Sport. 2006;9(4): 327-333 [DOI] [PubMed] [Google Scholar]
- 24. Gabbe BJ, Bennell KL, Finch CF, Wajswelner H, Orchard JW. Predictors of hamstring injury at the elite level of Australian football. Scand J Med Sci Sports. 2006;16(1):7-13 [DOI] [PubMed] [Google Scholar]
- 25. Gabbe BJ, Branson R, Bennell KL. A pilot randomised controlled trial of eccentric exercise to prevent hamstring injuries in community-level Australian football. J Sci Med Sport. 2006;9(1-2):103-109 [DOI] [PubMed] [Google Scholar]
- 26. Gabbe BJ, Finch CF, Bennell KL, Wajswelner H. Risk factors for hamstring injuries in community level Australian football. Br J Sports Med. 2005;39(2):106-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gabbe BJ, Finch CF, Wajswelner H, Bennell KL. Predictors of lower extremity injuries at the community level of Australian football. Clin J Sport Med. 2004;14(2):56-63 [DOI] [PubMed] [Google Scholar]
- 28. Gidwani S, Bircher MD. Avulsion injuries of the hamstring origin: a series of 12 patients and management algorithm. Ann R Coll Surg Engl. 2007;89(4):394-399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hagel B. Hamstring injuries in Australian football. Clin J Sport Med. 2005;15(5):400. [DOI] [PubMed] [Google Scholar]
- 30. Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40(2):67-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jonhagen S, Nemeth G, Eriksson E. Hamstring injuries in sprinters: the role of concentric and eccentric hamstring muscle strength and flexibility. Am J Sports Med. 1994;22(2):262-266 [DOI] [PubMed] [Google Scholar]
- 32. Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30(5):742-747 [DOI] [PubMed] [Google Scholar]
- 33. Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34(1):119-123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Koulouris G, Connell DA, Brukner P, Schneider-Kolsky M. Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. Am J Sports Med. 2007;35(9):1500-1506 [DOI] [PubMed] [Google Scholar]
- 35. Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009;37(4):727-734 [DOI] [PubMed] [Google Scholar]
- 36. Malliaropoulos N, Isinkaye T, Tsitas K, Maffulli N. Reinjury after acute posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med. 2010;39(2):304-310 [DOI] [PubMed] [Google Scholar]
- 37. Malliaropoulos N, Papalexandris S, Papalada A, Papacostas E. The role of stretching in rehabilitation of hamstring injuries: 80 athletes follow-up. Med Sci Sports Exerc. 2004;36(5):756-759 [DOI] [PubMed] [Google Scholar]
- 38. Mjolsnes R, Arnason A, Osthagen T, Raastad T, Bahr R. A 10-week randomized trial comparing eccentric vs concentric hamstring strength training in well-trained soccer players. Scand J Med Sci Sports. 2004;14(5):311-317 [DOI] [PubMed] [Google Scholar]
- 39. Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15(6):436-441 [DOI] [PubMed] [Google Scholar]
- 40. Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25(1):81-85 [DOI] [PubMed] [Google Scholar]
- 41. Orchard J, Steet E, Walker C, Ibrahim A, Rigney L, Houang M. Hamstring muscle strain injury caused by isokinetic testing. Clin J Sport Med. 2001;11(4):274-276 [DOI] [PubMed] [Google Scholar]
- 42. Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29(3):300-303 [DOI] [PubMed] [Google Scholar]
- 43. Orchard JW, Best TM. The managment of muscle strain injuries:an early return versus the risk of recurrence. Clin J Sport Med. 2002;12(1):3-5 [DOI] [PubMed] [Google Scholar]
- 44. Proske U, Morgan DL, Brockett CL, Percival P. Identifying athletes at risk of hamstring strains and how to protect them. Clin Exp Pharmacol Physiol. 2004;31(8):546-550 [DOI] [PubMed] [Google Scholar]
- 45. Puranen J, Orava S. The hamstring syndrome: a new diagnosis of gluteal sciatic pain. Am J Sports Med. 1988;16(5):517-521 [DOI] [PubMed] [Google Scholar]
- 46. Saikku K, Vasenius J, Saar P. Entrapment of the proximal sciatic nerve by the hamstring tendons. Acta Orthop Belg. 2010;76(3):321-324 [PubMed] [Google Scholar]
- 47. Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers: functional outcome and prevention. Am J Sports Med. 1996;24(2):130-136 [DOI] [PubMed] [Google Scholar]
- 48. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36(6):1110-1115 [DOI] [PubMed] [Google Scholar]
- 49. Schache AG, Crossley KM, Macindoe IG, Fahrner BB, Pandy MG. Can a clinical test of hamstring strength identify football players at risk of hamstring strain? Knee Surg Sports Traumatol Arthrosc. 2010;19(1):38-41 [DOI] [PubMed] [Google Scholar]
- 50. Schneider-Kolsky ME, Hoving JL, Warren P, Connell DA. A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries. Am J Sports Med. 2006;34(6):1008-1015 [DOI] [PubMed] [Google Scholar]
- 51. Servant CT, Jones CB. Displaced avulsion of the ischial apophysis: a hamstring injury requiring internal fixation. Br J Sports Med. 1998;32(3):255-257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):116-125 [DOI] [PubMed] [Google Scholar]
- 53. Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol. 2002; 179(6):1621-1628 [DOI] [PubMed] [Google Scholar]
- 54. Verrall GM, Kalairajah Y, Slavotinek JP, Spriggins AJ. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1-2):87-90 [DOI] [PubMed] [Google Scholar]
- 55. Verrall GM, Slavotinek JP, Barnes PG. The effect of sports specific training on reducing the incidence of hamstring injuries in professional Australian Rules football players. Br J Sports Med. 2005;39(6):363-368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury: comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain. Am J Sports Med. 2003;31(6):969-973 [DOI] [PubMed] [Google Scholar]
- 57. Verrall GM, Slavotinek JP, Barnes PG, Fon GT, Esterman A. Assessment of physical examination and magnetic resonance imaging findings of hamstring injury as predictors for recurrent injury. J Orthop Sports Phys Ther. 2006;36(4):215-224 [DOI] [PubMed] [Google Scholar]
- 58. Verrall GM, Slavotinek JP, Barnes PG, Fon GT, Spriggins AJ. Clinical risk factors for hamstring muscle strain injury: a prospective study with correlation of injury by magnetic resonance imaging. Br J Sports Med. 2001;35(6):435-439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Warren P, Gabbe BJ, Schneider-Kolsky M, Bennell KL. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br J Sports Med. 2010;44(6):415-419 [DOI] [PubMed] [Google Scholar]
- 60. Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90(11): 2365-2374 [DOI] [PubMed] [Google Scholar]
- 61. Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of hamstring injuries. Br J Sports Med. 2004;38(1):36-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wootton JR, Cross MJ, Holt KW. Avulsion of the ischial apophysis: the case for open reduction and internal fixation. J Bone Joint Surg Br. 1990;72(4):625-627 [DOI] [PubMed] [Google Scholar]
- 63. Worrell TW. Factors associated with hamstring injuries: an approach to treatment and preventative measures. Sports Med. 1994;17(5):338-345 [DOI] [PubMed] [Google Scholar]
- 64. Young IJ, van Riet RP, Bell SN. Surgical release for proximal hamstring syndrome. Am J Sports Med. 2008;36(12):2372-2378 [DOI] [PubMed] [Google Scholar]
- 65. Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010;195(4):993-998 [DOI] [PubMed] [Google Scholar]