Abstract
Context:
Patellofemoral pain syndrome (PFPS) is one of the most common overuse injuries.
Objective:
To assess the collective evidence of predisposing factors to PFPS.
Data Sources:
MEDLINE (1960–June 2010), EMBASE (1980–June 2010), and CINAHL (1982–June 2010).
Study Selection:
Studies were included if patients were asymptomatic at baseline testing (free of PFPS) and were prospectively followed for the development of the disorder. Only studies that assessed at least 1 variable that can be measured at a typical clinic were included. After duplicates were removed, 973 studies were assessed from their titles or abstracts, 20 from the full text, and from these, 7 met the inclusion criteria.
Data Extraction:
Data were extracted for age, weight, height, sample size, patient type (military vs civilian), follow-up periods, diagnostic methods, and diagnostic criteria. Means and standard deviations were extracted for all outcome variables.
Results:
Meta-analyses were performed for height, weight, leanness, Q angle, number of sit-ups, knee extension strength, and peak knee valgus angle during landing. Lower knee extension strength was the only variable that was predictive of PFPS (P < 0.01). Other variables that were identified as predictive of PFPS by single studies were vertical jump, push-ups, knee flexion and hip abduction strength, thumb-to-forearm flexibility, quadriceps and gastrocnemius flexibility, genu varum, navicular drop, knee valgus moment at initial contact during landing, social support, and palliative reaction.
Conclusions:
It appears that anthropometric variables are not associated with PFPS, while knee extension strength deficits appear to be predictors of PFPS.
Keywords: anterior knee pain, etiology, clinical measures
Patellofemoral pain syndrome (PFPS) is one of the most common diagnoses among young, physically active populations, affecting 1 in 4 athletes, with more than 70% being between 16 and 25 years old.3,4 Although physical therapy is an effective treatment for the majority of patients diagnosed with PFPS, high rates of recurrence have been reported, with two-thirds of these patients symptomatic 1 year after initial diagnosis.4 As a result, PFPS commonly leads to activity modification and extensive, prolonged medical treatment.4 Additionally, a possible link between PFPS and the development of patellofemoral osteoarthritis has been reported.25 Given that more than 10 million athletes participate in organized high school and college sports each year2 and that 25% of them will develop PFPS,3,4 an estimated 2.5 million high school and college students develop this syndrome every year.
Many researchers have tried to explain the causal relationships for this ailment. The general consensus is that the etiology of patellofemoral pain remains enigmatic and multifactorial and may include risk factors both intrinsic (skeletal alignment, soft tissue imbalance, biomechanical influences) and extrinsic (environment, equipment).7,10,30
Powered by the growing health-and-wellness concerns among the general public, more people are participating in physical activities in recent years. With the rising prevalence of overuse injuries such as PFPS among those who are physically active, physical therapists, sports medicine physicians, and athletic trainers have assumed an increasingly important role in prescreening these populations at risk of developing PFPS. There is a need for clinicians to be able to identify physically active people at high risk for developing PFPS. The purpose of this study is to review the prospective cohort studies available and, when possible, to perform meta-analysis on prospective predictors of PFPS.
Methods
Data Sources
MEDLINE (1960–June 2010), EMBASE (1980–June 2010), and CINAHL (1982–June 2010) were searched for prospective cohort studies of predictors of PFPS. Combinations of the terms patella, patellofemoral, anterior knee, and risk or predictor were used. A hand search of references in review articles was also performed to identify additional prospective cohort studies.
Study Selection
Studies were included if patients were asymptomatic at baseline testing (free of PFPS) and were prospectively followed for the development of the disorder. No limits were placed for age, sex, or physical activity level. Two investigators independently screened titles and abstracts, and full texts were obtained if 1 investigator believed that the study could not be excluded by the title and abstract. Only studies that assessed at least 1 variable that can be measured at a typical clinic were included. This definition excluded studies that used isokinetic devices, pressure mapping devices, and motion analysis equipment, which are not routinely accessible to clinicians. However, we included knee valgus angle and moment and knee flexion angle, although measured in biomechanical labs, because recent research has provided user-friendly clinical nomograms that accurately predict these variables with equipment available in the clinic.17 The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) flow diagram for the selection of trials for this review demonstrates the selection process (Figure 1).15
Figure 1.

PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Methodological Assessment
The Pengel scale was used to assess the methodological quality of the selected articles.20 Unlike other available methodological quality scales, the Pengel scale is specific for prospective studies. Six criteria were used to assess methodological quality with the Pengel scale: description of exclusion/inclusion criteria, representativeness of the sample, completeness of follow-up, outcome data, blinding of assessors, and statistical adjustment (Table 1). A score of 0 to 6 was assigned for each study, depending on the number of criteria met.
Table 1.
Methodologic quality of included studies assessed with the Pengel scale.20
| Study | Defined Sample | Representative Sample | Complete Follow-up | Prognosis | Blinded Outcome | Statistical Adjustment | Methodologic Score |
|---|---|---|---|---|---|---|---|
| Boling1 | Yes | No | Yes | Yes | No | No | 3 |
| Milgrom14 | Yes | No | Yes | Yes | No | No | 3 |
| Thijs24 | Yes | No | No | Yes | No | No | 2 |
| Thijs23 | Yes | No | No | Yes | No | No | 2 |
| van Tiggelen26 | Yes | No | No | Yes | No | Yes | 3 |
| Witvrouw30 | Yes | No | No | Yes | No | No | 2 |
| Myer16 | Yes | No | Yes | Yes | No | No | 3 |
Data Extraction
Data were extracted for age, weight, height, sample size, type of patient (military vs civilian), follow-up periods, diagnostic methods, and diagnostic criteria. Additionally, means and standard deviations were extracted for all outcome variables that met the definition of clinical measures. The 2 investigators independently extracted these characteristics, and in cases of disagreement, a discussion ensued until consensus was reached.
Data Analysis
RevMan Software 5.0 (Nordic Cochrane Centre, Cochrane Collaboration, Copenhagen, Denmark) was used for the meta-analysis by entering sample sizes for each group (PFPS and control), means, and standard deviations. When appropriate, analysis was performed across all included studies, as well as subgroup analysis between civilians and military recruits. The mean difference for continuous outcomes (or standardized mean difference, when the units of measurement varied across studies) and 95% confidence intervals with fixed effect were calculated with the inverse variance method and presented in forest plots.
Results
The database search yielded 1688 references from the 3 databases. After duplicate references were removed, 973 unique references remained, 12 of which could not be excluded from the abstract or title. Additionally, 7 potentially relevant articles were identified by the hand search. One additional article16 that was in press at the time of the database search was identified after discussions with experts in the field. Therefore, a total of 20 full-text articles were reviewed for inclusion in this review (Figure 1).
Of the 20 studies, 13 were excluded for the following reasons: 2 were not prospective,5,6 2 included patients who had PFPS at baseline,8,31 7 did not provide specific data for the group that developed PFPS,11-13,22,27-29 1 reported variables that could not be measured at a typical clinic,18 and 1 was a journal club report.9 The remaining 7 articles met the inclusion criteria for this systematic review.
The methodological quality on the Pengel scale was 2.6 of 5 (range, 2-3). None of the studies met the requirement for representative sample and blinded outcome (Table 1). A total of 2401 participants were enrolled in the 7 studies, of whom 234 (9.75%) developed PFPS (see supplemental appendix, available at http://sph.sagepub.com/content/suppl).
A variety of outcome measures in the 7 studies were categorized in anthropometrics (height, weight, body mass index, etc), physical fitness (balance, jump height, number of sit-ups, etc), muscle strength, joint laxity, muscle flexibility, lower leg alignment (leg length discrepancy, foot posture, genu varum/valgum, Q angle, etc), biomechanics (knee valgus angle, etc), and psychological parameters (introversion/extroversion, neuroticism, etc).
Anthropometrics
Six studies14,16,23,24,26,30 reported data on height and weight: 905 in the control group and 177 in the PFPS group. Neither variable was found to be predictive of PFPS (P ≥ 0.57). Heterogeneity analysis did not yield significance (P ≥ 0.40), suggesting that interpretation of the pooled data is appropriate. Subgroup analysis for studies that used the military versus civilian patients did not change the results. Two studies used measures of leanness, such as body mass index23 and ponderal index30: 41 patients in the PFPS group and 343 in the control group. Pooled analysis demonstrated that leanness was not a predictor of PFPS (P = 0.34), while there was no significant heterogeneity (P = 0.64). Witvrouw additionally reported on body fat percentage using the caliper method and the body composition method (endomorphism, ectomorphism, mesomorphism). Neither variable was associated with the development of PFPS.30 Milgrom and Witvrouw both reported no associations between leg length discrepancy and PFPS,14,30 while Milgrom reported no association between thigh circumference, calf circumference, tibial length, foot width, or foot length and the development of PFPS.14
Physical Fitness
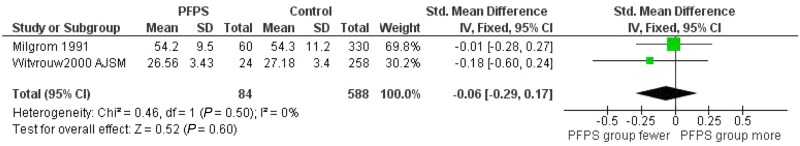
Two studies14,30 reported on the number of sit-ups: 84 patients in the PFPS and 588 in the control group. Number of sit-ups did not predict PFPS (P = 0.60; heterogeneity, P = 0.50) (Figure 2). Milgrom measured the number of sit-ups in 1 minute,14 while Witvrouw measured the total number of sit-ups.30 Witvrouw reported on a large number of fitness variables, such as balance, vertical and broad jump, bent arm hang, shuttle run, plate tapping, arm pull, leg lifts, sit and reach, and maximal oxygen uptake. The only association was between lower performance on vertical jump and the development of PFPS.30 Milgrom reported that the 2-km run time was not associated with PFPS but that the number of push-ups was a predisposing factor to PFPS.14
Figure 2.
Meta-analysis on the number of sit-ups.
Muscle Strength
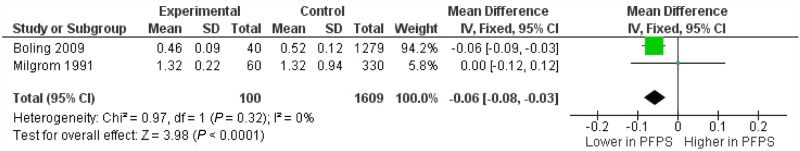
Boling and Milgrom compared knee extension isometric strength: 100 patients in the PFPS group and 1609 in the control group.1,14 Boling identified lower knee extension isometric strength as a predictor for PFPS,1 while Milgrom found the opposite effect.14 Boling normalized values to body weight for knee extension, knee flexion and hip extension, internal rotation, external rotation, and abduction. Milgrom reported no association between knee extension strength when normalized to body weight and the development of PFPS; when measurements were not normalized to body weight, greater strength predisposed patients to PFPS.14 The pooled analysis based on data from these 2 studies found that lower knee extension strength is a predictor of PFPS (P < 0.01; heterogeneity, P = 0.32) (Figure 3). Also, Boling reported that decreased muscle strength for knee flexion and hip abduction were also associated with PFPS.1
Figure 3.
Meta-analysis on knee extension strength.
Joint Laxity
Witvrouw performed a variety of joint laxity tests, such as the range of motion for little finger extension, elbow extension, knee extension, and thumb to forearm.30 Witvrouw additionally reported on medial, lateral, and total patellar mobility and shoulder mobility. Greater flexibility of thumb to forearm was associated with the development of PFPS, but none of the other variables demonstrated an association. Milgrom reported that range of motion for hip external rotation was not associated with PFPS.14
Muscle Flexibility
Witvrouw concluded that decreased quadriceps and gastrocnemius flexibility was significantly associated with PFPS, while hamstrings flexibility was not.30
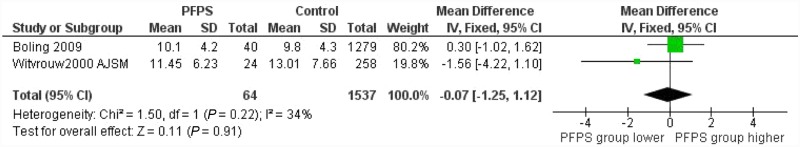
Lower Leg Alignment
Q angle was not a predictor of PFPS based on the pooled analysis (P = 0.91; heterogeneity, P = 0.22)1,30 (Figure 4). Different methodology used for tibiofemoral alignment (genu varum/valgum) precludes data pooling.14,16,30 A strong association between genu varum and PFPS in male military recruits was found when reported as a continuous variable (medial tibial intercondylar distance) or a categorical variable (negative, small, and large).14 Means and standard deviations of the categorical variable were not reported, thereby precluding pooled analysis with the Witvrouw study, which found no association between tibiofemoral alignment and PFPS when treated as categorical variable.30 Static knee valgus was not associated with PFPS.16
Figure 4.
Meta-analysis on Q angle.
Three studies investigated foot position. Thijs used the foot posture index (neutral, pronated, and supinated) and found no association with PFPS.23 Patients with higher navicular drop values were more likely to develop PFPS.1 Podograph and goniometer were used for foot arch evaluation of rearfoot and forefoot alignment. No difference was found between PFPS and non-PFPS patients.30
Biomechanical Variables
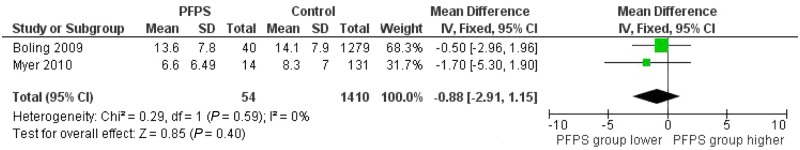
Two studies measured peak knee valgus angle during drop landing tasks.1,16 Pooled analysis showed that the combined effect was not predictive of PFPS (P = 0.40) without significant heterogeneity (P = 0.59). One study found a trend for decreased peak knee flexion during landing as a predictor of PFPS (P = 0.06).1 Knee valgus moment at initial contact was predictive of PFPS.16
Psychological Parameters
Out of 11 psychological variables, seeking less social support and difficulty relaxing when confronted with a problem (palliative reaction) were predictors of PFPS in a single study.30
Discussion
The main finding of this meta-analysis is that, despite the high incidence of PFPS among physically active populations and the abundance of factors that may predispose to this disorder, there are few prospective cohort studies, especially among civilian populations. Pooling data for meta-analysis purposes was not possible for most variables.
Limited quadriceps and gastrocnemius flexibility, knee extension weakness, and excessive knee valgus during landing may predict PFPS development. These variables appear to be more suggestive than anthropometric variables (height, weight), measures of leanness, or lower extremity static alignment (Q angle) in identifying those at higher risk for PFPS. Knee valgus moment at initial contact during landing from a jump may be a predictor of PFPS in female athletes.16 In contrast, peak knee valgus angle does not appear to be related to the development of PFPS (Figure 5). A possible explanation for this finding may be that peak knee valgus angle occurs at the end of the landing cycle,19 when most of the ground reaction force has been absorbed.
Figure 5.
Meta-analysis on knee valgus angle during landing from a jump.
There is a distinct difference between predictors and pathogenetic factors. Predictors increase the likelihood of developing PFPS. Pathogenetic factors, however, are directly implicated in the development and cause of the disorder. Historically, a number of factors that lead to lateral patella tracking (Q angle, subtalar hyperpronation, shortened iliotibial band and lateral retinaculum, decreased strength or timing of the medial quadriceps and the gluteus medius) have been implicated in the pathogenesis of PFPS.21 However, the purpose of the current study was to identify factors that increase the likelihood of PFPS (predictors) and not those that directly contribute to the pathogenesis of the disorder.
In contrast to the 2 studies1,14 that found conflicting knee extension strength results, this meta-analysis identified knee extension weakness as a predictor of PFPS (Figure 3). Similarly, those with limited flexibility of the gastrocnemius and quadriceps were more likely to develop PFPS.30 A direct link between decreased quadriceps flexibility and PFPS can be argued, as a shortened quadriceps may result in increased contact forces between the retropatellar cartilage and the trochlear groove.
Most measures of physical fitness, psychological parameters, and generalized laxity were not predictive of PFPS. Interestingly, lower performance on vertical jump,30 higher performance on number of push-ups,14 and thumb-to-forearm laxity30 were predisposing factors to PFPS. However, this may represent a finding related more to chance and the high number of statistical comparisons with no appropriate adjustment rather than a true association between these measures and PFPS.
In conclusion, this meta-analysis found few published prospective cohort studies on PFPS, especially among nonmilitary populations. Anthropometric variables do not predict PFPS. In this small sample of studies, limited quadriceps and gastrocnemius flexibility, knee extension weakness, and faulty landing mechanics predict development of PFPS. PFPS is a multifactorial disorder. Clinicians screening populations at high risk for PFPS should evaluate strength, flexibility, and dynamic alignment.
References
- 1. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108-2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cantu RC, Mueller FO. The prevention of catastrophic head and spine injuries in high school and college sports. Br J Sports Med. 2009;43(13):981-986 [DOI] [PubMed] [Google Scholar]
- 3. DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14(3):218-224 [DOI] [PubMed] [Google Scholar]
- 4. Devereaux M, Lachmann S. Patello-femoral arthralgia in athletes attending a sports injury clinic. Br J Sports Med. 1984;18(1):18-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dorotka R, Boj EJ, Kypta A, Kollar B. [Patellofemoral pain syndrome in young men compared to a normal population exposed to the same physical strain]. Z Orthop Ihre Grenzgeb. 2002;140(1):48-51 [DOI] [PubMed] [Google Scholar]
- 6. Earl JE, Hertel J, Denegar CR. Patterns of dynamic malalignment, muscle activation, joint motion, and patellofemoral-pain syndrome. J Sport Rehab. 2005;14(3). [Google Scholar]
- 7. Fairbank J, Pynsent P, Van Poortvliet J, Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg Br. 1984;66(5):685-693 [DOI] [PubMed] [Google Scholar]
- 8. Fulkerson JP. The etiology of patellofemoral pain in young active patients: a prospective study. Clin Orthop Relat Res. 1983;179:129-133 [PubMed] [Google Scholar]
- 9. Hart L, Mohtadi N. Risk factors for patellofemoral pain syndrome in athletic young adults. Clin J Sport Med. 2001;11(2):127 [Google Scholar]
- 10. Huberti H, Hayes W. Patellofemoral contact pressures: the influence of Q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715-724 [PubMed] [Google Scholar]
- 11. Kowal DM. Nature and causes of injuries in women resulting from an endurance training program. Am J Sports Med. 1980;8(4):265-269 [DOI] [PubMed] [Google Scholar]
- 12. Lun V, Meeuwisse WH, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. Br J Sports Med. 2004;38(5):576-580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Macera C, Pate R, Powell K, Jackson K, Kendrick J, Craven T. Predicting lower-extremity injuries among habitual runners. Arch Intern Med. 1989;149:2565-2568 [PubMed] [Google Scholar]
- 14. Milgrom C, Finestone A, Eldad A, Shlamkovitch N. Patellofemoral pain caused by overactivity: a prospective study of risk factors in infantry recruits. J Bone Joint Surg Am. 1991;73(7):1041-1043 [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Myer G, Ford K, Barber Foss K, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon). 2010;25(7):700-707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38(10):2025-2033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Noehren B, Davis I. Prospective Study of the Biomechanical Factors Associated With Patellofemoral Pain Syndrome. Palo Alto, CA: American Society of Biomechanics; 2007 [Google Scholar]
- 19. Pappas E, Hagins M, Sheikhzadeh A, Nordin M, Rose D. Peak biomechanical variables during bilateral drop landings: comparisons between sex (female/male) and fatigue (pre-fatigue/post-fatigue). N Am J Sports Phys Ther. 2009;4(2):83-91 [PMC free article] [PubMed] [Google Scholar]
- 20. Pengel LHM, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. BMJ. 2003;327(7410):323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42-51 [DOI] [PubMed] [Google Scholar]
- 22. Stefanyshyn DJ, Stergiou P, Lun VMY, Meeuwisse WH, Worobets JT. Knee angular impulse as a predictor of patellofemoral pain in runners. Am J Sports Med. 2006;34(11):1844-1851 [DOI] [PubMed] [Google Scholar]
- 23. Thijs Y, De Clercq D, Roosen P, Witvrouw E. Gait-related intrinsic risk factors for patellofemoral pain in novice recreational runners. Br J Sports Med. 2008;42(6):466-471 [DOI] [PubMed] [Google Scholar]
- 24. Thijs Y, Van Tiggelen D, Roosen P, De Clercq D, Witvrouw E. A prospective study on gait-related intrinsic risk factors for patellofemoral pain. Clin J Sport Med. 2007;17(6):437-445 [DOI] [PubMed] [Google Scholar]
- 25. Utting MR, Davies G, Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12(5):362-365 [DOI] [PubMed] [Google Scholar]
- 26. van Tiggelen D, Cowan S, Coorevits P, Duvigneaud N, Witvrouw E. Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37(6):1099-1105 [DOI] [PubMed] [Google Scholar]
- 27. Walter S, Hart L, McIntosh J, Sutton J. The Ontario Cohort Study of Running-Related Injuries. Arch Intern Med. 1989;149:2561-2564 [PubMed] [Google Scholar]
- 28. Wen D, Puffer J, Schmalzried T. injuries in runners: a prospective study of alignment. Clin J Sport Med. 1998;8(3):187-194 [DOI] [PubMed] [Google Scholar]
- 29. Willems T, Clercqb D, Delbaerea K, Vanderstraetena G, De Cockb A, Witvrouw E. A prospective study of gait related risk factors for exercise-related lower leg pain. Gait Posture. 2006;23:91-98 [DOI] [PubMed] [Google Scholar]
- 30. Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: a two-year prospective study. Am J Sports Med. 2000;28(4):480-489 [DOI] [PubMed] [Google Scholar]
- 31. Yates C, Grana WA. Patellofemoral pain: a prospective study. Orthopedics. 1986;9(5):663-667 [DOI] [PubMed] [Google Scholar]