Abstract
Context:
Chronic lower leg pain in athletes can be a frustrating problem for patients and a difficult diagnosis for clinicians. Myriad approaches have been suggested to evaluate these conditions. With the continued evolution of diagnostic studies, evidence-based guidance for a standard approach is unfortunately sparse.
Evidence Acquisition:
PubMed was searched from January 1980 to May 2011 to identify publications regarding chronic lower leg pain in athletes (excluding conditions related to the foot), including differential diagnosis, clinical presentation, physical examination, history, diagnostic workup, and treatment.
Results:
Leg pain in athletes can be caused by many conditions, with the most frequent being medial tibial stress syndrome; chronic exertional compartment syndrome, stress fracture, nerve entrapment, and popliteal artery entrapment syndrome are also considerations. Conservative management is the mainstay of care for the majority of causes of chronic lower leg pain; however, surgical intervention may be necessary.
Conclusion:
Chronic lower extremity pain in athletes includes a wide differential and can pose diagnostic dilemmas for clinicians.
Keywords: chronic leg pain, medial tibial stress syndrome, chronic exertional compartment syndrome, nerve entrapment, popliteal artery entrapment syndrome
Chronic leg pain is a common condition in competitive and recreational athletes, and the onset is frequently insidious. The causes of lower leg pain are numerous, with diagnoses varying in frequency and severity, making the differential relatively broad. Moreover, symptoms are often ambiguous, necessitating a thorough knowledge of anatomy and biomechanics of the lower extremity.16
Second only to the knee, the lower leg accounts for approximately one-third of running injuries in long-distance runners.35,57
Differential Diagnosis
There is a wide range of diagnoses for exercise-induced leg pain in the weightbearing athlete: medial tibial stress syndrome (MTSS), chronic exertional compartment syndrome (CECS), stress fracture, nerve entrapment, and popliteal artery entrapment syndrome (PAES) are the most common (Table 1).16,19
Table 1.
| Vascular | Popliteal artery entrapment syndrome Endofibrotic disease (primarily external iliac artery) Popliteal artery aneurysm Cystic adventitial disease Peripheral arterial dissection Intermittent claudication Deep vein thrombosis |
| Bone/periosteum | Stress fracture (tibia, fibula) Medial tibial stress syndrome Metabolic bone disease |
| Muscle/tendon | Muscle strains Tendinopathy Chronic exertional compartment syndrome |
| Nerve entrapment | Peripheral neuropathies Lumbar radiculopathy |
| Infection | Osteomyelitis |
| Malignancy | Muscle or bone neoplasm |
Studies show that MTSS accounts for 6% to 16% of all running injuries; it can represent up to 50% of lower leg injuries in select populations, such as military personnel.33,63 CECS may be difficult to diagnose, but it is most common in runners in the anterior and lateral compartments.14 In a retrospective review of 150 athletes with exercise-induced leg pain, 33% were diagnosed with CECS, 25% with stress fractures, 13% with MTSS, and 10% with nerve entrapment syndromes.16
Medial Tibial Stress Syndrome
MTSS (shin splints) is a repetitive-stress overuse injury commonly affecting weightbearing athletes. Several intrinsic risk factors for MTSS have been identified: hyperpronation, body mass index, female sex, hip internal/external rotation, and hyperplantarflexion.15,29,48,63 In a prospective study of 35 male participants recruited from 2 Dutch Army bases, Moen et al found that increased hip internal rotation, increased plantar flexion, and a positive navicular drop (assessing pronation) were associated with MTSS, while a higher body mass index was associated with a longer duration to full recovery.41
The cause may be periostitis of the tibia due to tibial strain, but more recent evidence points toward a spectrum of tibial stress injuries contributing to MTSS: periostitis, tendinopathy, and stress reaction of the tibia, as well as dysfunction of the tibialis posterior, tibialis anterior, and soleus muscles.3,8,17,23 In a cadaveric study, traction-induced muscle injury theories of the superficial and deep posterior compartments were not supported by anatomic evidence; the mean distal muscle attachments to the medial tibial border were superior to the distal third of the tibia in the posterior compartments. In contrast, the deep crural fascia of all but 3 of 16 specimens attached along the entire length of the medial tibia.54 MTSS and tibial stress fractures may be a continuum of bone stress reactions.8,23
Stress Fractures
Stress fractures of the lower extremity account for up 80% to 95% of all stress fractures, with the majority involving the tibia; they are caused by repetitive loading with resulting bony microfracture.8,12,33,53,55,58 Stress fractures of the anterior tibia and medial malleolus are high-risk fractures necessitating nonweightbearing, longer periods before return to play, and/or surgical treatment.11
Chronic Exertional Compartment Syndrome
CECS is a condition of increased pressure in the fascial compartments (muscles and neurovascular structures bound by fascia and bone) related to exercise leads to recurrent episodes of pain.10,14,62 The anterior compartment is most commonly involved (45%) with the lateral, deep, and superficial compartments less common (Figure 1).10,47,62 Symptoms are bilateral 85% to 95% of the time.55 The pathophysiology of CECS is multifactorial. Factors may include constraints of a fixed muscular compartment, normal or abnormal muscle swelling that occurs with activity, abnormally thickened fascia, normal muscle hypertrophy in response to resistance training, or dynamic contraction patterns during gait.14 Low muscle capillary supply is a pathogenic factor in chronic compartment syndrome.18 Biopsies from the tibialis anterior muscle from 9 patients during fasciotomy and 1 year later revealed lower capillary density compared with controls.18
Figure 1.
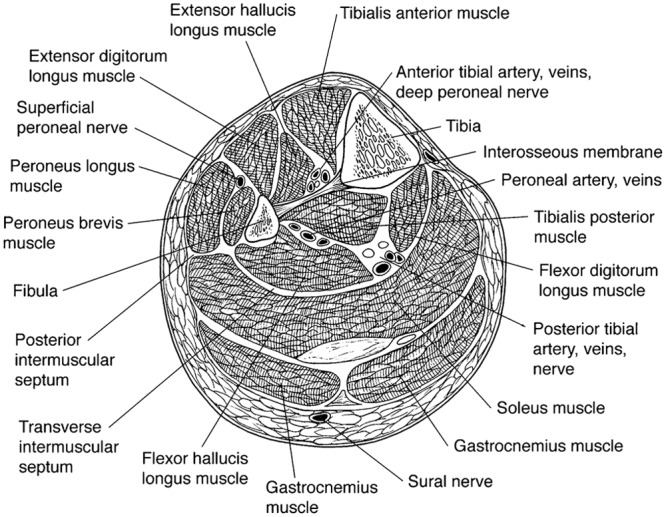
Cross-section of the lower left leg showing its 4 compartments: anterior at upper left; lateral at center left; deep posterior at center; superficial posterior at bottom right.
Used with permission from: Fraipont MJ, Adamson GJ. Chronic exertional compartment syndrome. J Am Acad Orthop Surg. 2003;11:268-276.
Peripheral Nerve Entrapment
The typical presentation is burning pain brought about by activity and exacerbated by continued exercise, with motor and/or sensory symptoms being regional.34,37 However, nerve entrapment symptoms do not always present with clear neurologic signs of motor weakness, sensory loss, or change in reflexes; diagnosis is often delayed. The common peroneal, superficial peroneal, and saphenous nerves are most commonly at risk for entrapment, with trauma being a primary cause (Figures 2-4, Table 2).37,51
Figure 2.

Drawing shows the common peroneal nerve and its branches at the knee. The common peroneal nerve wraps around the fibular neck and under the peroneus longus muscle to trifurcate into the recurrent articular branch to the knee capsule, the superficial peroneal nerve, and the dorsal peroneal nerve.
Used with permission from: Donavan A, et al. MR imaging of entrapment neuropathies of the lower extremity. Radiographics. 2010;30:1001-1019.
Figure 4.
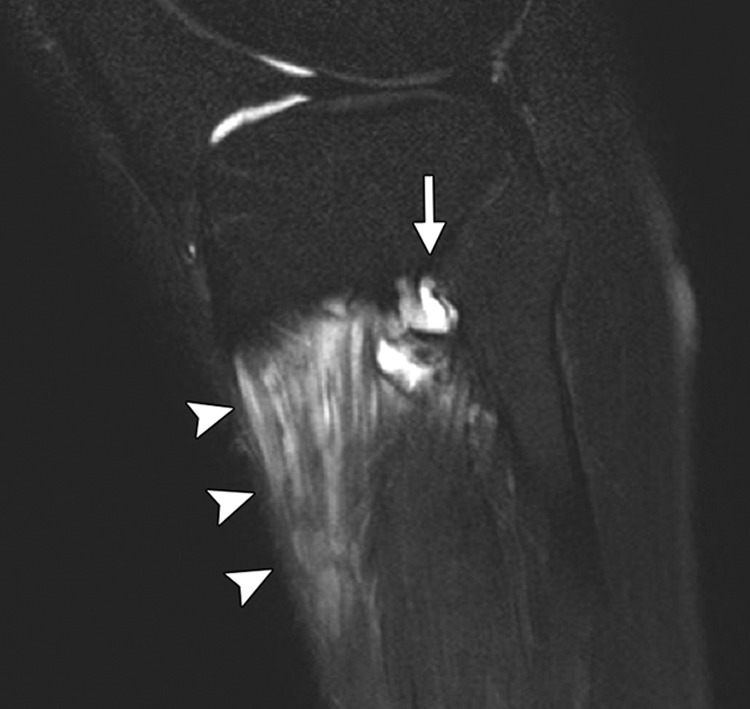
Common peroneal neuropathy secondary to a ganglion of the proximal tibiofibular joint. Sagittal magnetic resonance image shows a ganglion arising from the proximal tibiofibular joint (arrow) with associated denervation-related increased signal intensity of the anterior tibial and extensor digitorum longus muscles (arrowheads).
Used with permission from: Donavan A, et al. MR imaging of entrapment neuropathies of the lower extremity. Radiographics. 2010;30:1001-1019.
Table 2.
| Nerve Entrapment Syndrome | Relevant Anatomy | Common Cause | Clinical Presentation |
|---|---|---|---|
| Saphenous nerve | Largest branch of the femoral nerve arising from L1, L2, L3; the nerve leaves the femoral triangle to enter the adductor canal with the femoral artery and vein | The nerve can be injured in the adductor canal by local trauma, infection, or inflammation; the nerve may also be injured at the knee due to arthroscopy, trauma, or pes anserine bursitis | Medial knee and/or leg pain |
| Common peroneal nerve | As the nerve enters the peroneal (fibular) tunnel, it divides into deep and superficial branches | Compression at the peroneal tunnel from sources such as casts, surgery, osteophytes, and cysts or by sitting in a prolonged crossed-legged position | Sensory disturbances in the lateral lower leg and foot with possible foot drop and pain at site of compression |
| Sural nerve | Begins with its main component from the tibial nerve in the popliteal fossa and runs distally between the 2 heads of the gastrocnemius | Compression from mass lesions, scar tissue, ganglia, surgical trauma, or extrinsic compression from casts or tight ski boots | Shooting pain in the cutaneous distribution of the nerve (lateral aspect of ankle/foot) |
| Superficial peroneal nerve | Travels in the lateral compartment and supplies the peroneus longus and brevis muscles; pierces the deep fascia and emerges into the subcutaneous fat at approximately 10 to 15 cm above the tip of the lateral malleolus | Local trauma or compression is the most common underlying cause; nontraumatic causes are commonly due to anatomic variations, such as fascial defects with or without muscle herniation about the lateral lower leg | Numbness or paresthesia in the distribution of the nerve or lateral leg pain; more typically present with vague pain over the dorsum of the foot; symptoms increase with activity |
Figure 3.
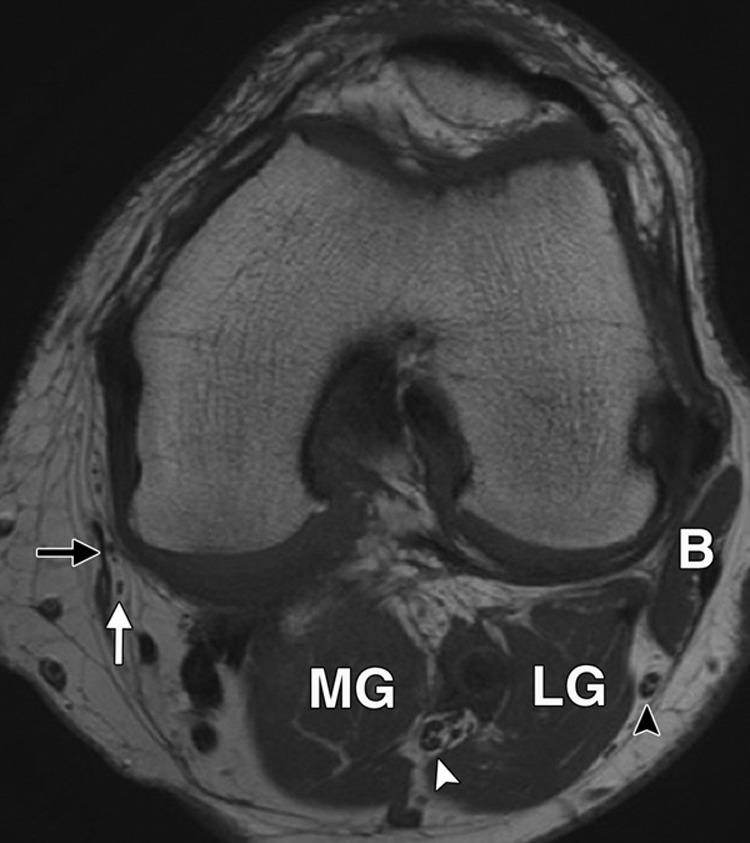
Normal anatomy of the tibial, common peroneal, and saphenous nerves at the level of the knee. Axial magnetic resonance image shows the tibial nerve (white arrowhead) between the lateral head (LG) and medial head (MG) of the gastrocnemius muscle. The common peroneal nerve (black arrowhead) is seen between the lateral gastrocnemius muscle and biceps femoris muscle (B). The saphenous nerve branches (white arrow) are seen lateral to the sartorius muscle (black arrow).
Used with permission from: Donavan A, et al. MR imaging of entrapment neuropathies of the lower extremity. Radiographics. 2010;30:1001-1019.
Popliteal Artery Entrapment Syndrome
Exercise-related arterial entrapment syndromes of the lower extremity are relatively rare, but most commonly include PAES.6,47 PAES is an uncommon overuse injury and is often confused with CECS and can even coexist with CECS.56 A frequent cause of PAES is compression of the popliteal artery by surrounding musculotendinous structures as it exits the popliteal fossa; the most common variant involves an accessory medial head of the gastrocnemius passing posterior to the popliteal artery.6,13,20 Popliteal compression can also be caused by fibrous bands of the gastrocnemius or the popliteus muscle or an aberrant course of the popliteal artery.20 PAES can also be functional, with vascular testing results often normal.56
Other potential vascular causes of lower extremity pain in athletes to consider include endofibrosis (intimal hyperplasia), popliteal artery aneurysm, cystic adventitial disease, and peripheral arterial dissections.47
Diagnosis
History
An activity history may be useful in determining if the condition is secondary to a training error. It is important to determine the number of sessions per week and the duration and intensity of each activity. An abrupt increase in these variables may be a contributing factor, as well as a recent change in training surface or footwear.23,44,59
Risk factors for stress fractures include female sex, white race, irregular menses, eating disorder, osteoporosis or osteopenia, and previous stress fractures.9,23,32
Physical Examination
Specific examination tests for MTSS, stress fractures, CECS, and PAES can assist the clinician in narrowing the differential diagnosis and deciding if further diagnostic tests are necessary.
Evaluation and Testing
MTSS: Magnetic Resonance Imaging and Bone Scan
Radiograph results are normal with MTSS. Magnetic resonance imaging (MRI) and bone scans usually show abnormally high signal along the posterior medial tibial surface or the classic train-track appearance of nucleotide uptake on a nuclear medicine bone scan.5 MRI demonstrates superior sensitivity and specificity in early tibial stress injuries.7,24
Stress Fractures: Radiographs and MRI
Plain radiographs are usually negative for early stress fractures. The sensitivity of radiographs may be as low as 10% (Figure 5).23 Abnormalities are usually seen after 2 to 8 weeks of symptoms.11,23 Bone scan is a more sensitive but less specific method in detecting stress injuries.26,61,64 Computed tomography can be helpful in distinguishing conditions that mimic stress fractures on bone scan, such as malignancies. It can differentiate stress fractures from stress reactions.23,27 MRI, however, shows edema (Figure 6), often within about 3 days of symptom onset, and is more sensitive and specific than computed tomography or bone scan for diagnosing stress fractures of the tibia.24
Figure 5.

Lateral plain radiograph of the tibia showing an anterolateral stress fracture. This high-risk tension-sided stress fracture may be associated with prolonged nonunion.
Figure 6.
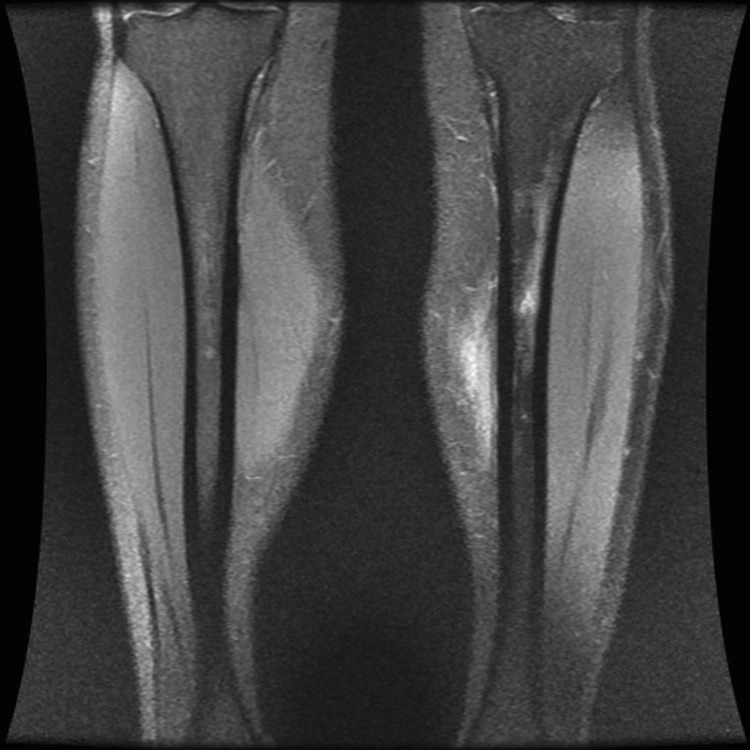
Coronal magnetic resonance imaging of bilateral lower extremities demonstrating an early stress reaction of the left tibia as evidenced by the development of edema in the proximal tibia.
CECS: Compartment Pressure Testing
Compartment pressure testing is the gold standard for CECS.30,36,45 Preexertional and postexertional measurements are needed.56 The postexertional measurements should be taken within 5 minutes of the exercise; the athlete should be symptomatic at the time of measurement.46 A positive compartment pressure test is a preexercise resting pressure of 15 mmHg or greater and/or a 1-minute postexercise pressure of 30 mmHg or greater and/or a 5-minute postexercise pressure of 20 mmHg or greater.46
PAES: Ankle-Brachial Index and Angiography
Initial screening with the ankle-brachial index (ie, ratio of the blood pressure in the lower legs to the blood pressure in the arms) can be helpful before vascular studies of the lower extremity. Because this entrapment may be functional, it is recommended that the ankle-brachial index be done with the ankle in only the neutral, forced dorsiflexion, and forced plantarflexion positions. An ankle-brachial index of less than 0.9 is abnormal. The sensitivity of the ankle-brachial index is 90% and the specificity is 98% for significant stenosis of greater than 50% in major leg arteries.38 Although direct angiography has been considered the gold standard, both computed tomography angiography and magnetic resonance angiography are quite useful in detecting this condition and are less invasive (Figure 7).4
Figure 7.
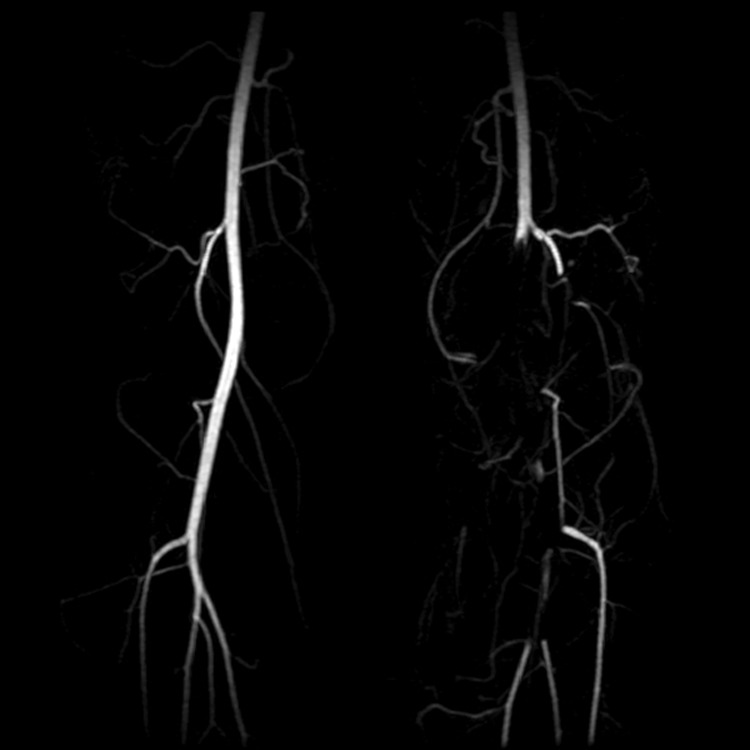
Magnetic resonance angiogram demonstrating occlusion of the left popliteal artery due to popliteal artery entrapment syndrome.
Peripheral Nerve Entrapment: Electrodiagnostic Studies
Electromyography and nerve conduction velocities can be helpful in diagnosing nerve entrapment and the level of the lesion.37 The condition must be present for at least 3 to 4 weeks for the studies to become positive.55,60
Treatment
Medial Tibial Stress Syndrome
The treatment of MTSS has been examined in 3 randomized controlled trials, showing that rest is equal to ice, nonsteroidal anti-inflammatory drugs, proper conditioning, physical therapy for stretching and strengthening of the calf musculature, rigid orthotics to correct foot hyperpronation, and activity modification.43 The use of neoprene or semirigid orthotics may help prevent MTSS.43 Newer conservative measures include extracorporeal shockwave therapy, which may speed recovery.42,50 A pneumatic leg brace is not as effective as rehabilitation and rest.40 Most cases of MTSS usually do not preclude participation in sports activities.25
Stress Fractures
The treatment depends on the fracture risk. Fibular and posteromedial tibial stress fractures are considered low risk and can be treated conservatively with ice, pain medicine, a walking boot, cross training, and limiting impact activities. Anterior tibia or medial malleolar stress fractures are high risk and should be treated aggressively with nonweightbearing, casting, and/or bone stimulator for extended periods (3 months). In competitive athletes, internal fixation may be considered to increase healing potential and quicker return to activity.31 Pneumatic bracing may speed rehabilitation following tibial stress fractures.1,2 Preventative measures hinge on appropriate training intensity and duration for each athlete; shock-absorbing inserts in footwear may help prevent stress fractures.49
Chronic Exertional Compartment Syndrome
Nonsurgical measures of CECS of the lower extremity include intermittent massage with stretching, taping, orthotics, and nonsteroidal anti-inflammatory drugs.14 The only evidence-based treatment is activity modification and rest.10
The treatment of CECS that fails conservative care is typically surgical.21 Patients with anterior or lateral compartment symptoms tend to have better outcomes: greater than 80% success rate as compared with deep posterior CECS, which has a success rate of about 50%.10,28 Postoperative care includes an approximate 12-week rehabilitation starting with protection and mobility, early light strengthening, scar massage with mobility and desensitization, progression of strengthening exercises, and concluding with impact and sport-specific training.52
Popliteal Artery Entrapment Syndrome
The treatment of PAES is by surgical removal of the compressing structure and either venous bypass or interposition graft, but it may be different from case to case.56 Endovascular revascularization followed by release of arterial compression is a feasible alternative.39
Peripheral Nerve Entrapment
Conservative management—including modifying precipitating activity, biomechanical correction, physical therapy, massage, and nonsteroidal anti-inflammatory drugs—is the mainstay of treatment for most nerve entrapment syndromes.34,37,51 While nonoperative management is usually successful in most nerve entrapment syndromes (common peroneal and saphenous nerve), some may require surgical intervention (superficial peroneal).37,51
Summary
The most common causes of chronic lower leg pain in athletes are MTSS, stress fractures, CECS, nerve entrapment syndromes, and PAES. Symptom overlap can make evaluation and treatment difficult. A thorough history and physical examination is essential. Conservative management is the initial treatment for most chronic lower leg pain. Surgical intervention may be necessary in some high-risk stress fractures, PAES, nerve entrapment syndromes, and CECS.
Treatment of stress fractures is based on risk classification. Prolonged immobilization and nonweightbearing or surgery for high-risk fractures may be indicated. Avoidance of high-impact activity for low-risk stress fractures is advised.
References
- 1. Allen CS, Flynn TW, Kardouni JR, et al. The use of a pneumatic leg brace in soldiers with tibial stress fractures-a randomized clinical trial. Mil Med. 2004;169:880-884 [DOI] [PubMed] [Google Scholar]
- 2. Allen CS, Hemphill NH, Kardouni JR, et al. A randomized controlled trial of a pneumatic leg brace versus traditional treatment in individuals with tibial stress fractures. J Orthop Sports Phys Ther. 2002;32:A3 [Google Scholar]
- 3. Anderson M, Ugalde V, Batt M, Gacayan J. Shin splints: MR appearance in a preliminary study. Radiology. 1997;204:177-180 [DOI] [PubMed] [Google Scholar]
- 4. Anil G, Tay KH, Howe TC, Tan BS. Dynamic computed tomography angiography: role in the evaluation of popliteal artery entrapment syndrome. Cardiovasc Intervent Radiol. 2011;34:259-270 [DOI] [PubMed] [Google Scholar]
- 5. Aoki Y, Yasuda K, Tohyama H, Ito H, Minami A. Magnetic resonance imaging in stress fractures and shin splints. Clin Orthop Relat Res. 2004;421:260-267 [DOI] [PubMed] [Google Scholar]
- 6. Baltopoulous P, Filippou DK, Sigala F. Popliteal artery entrapment syndrome: anatomic or functional syndrome? Clin J Sport Med. 2004;14:8-12 [DOI] [PubMed] [Google Scholar]
- 7. Batt ME, Ugalde V, Anderson MW, Shelton DK. A prospective controlled study of diagnostic imaging for acute shin splints. Med Sci Sports Exerc. 1998;30:1564-1571 [DOI] [PubMed] [Google Scholar]
- 8. Beck B. Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med. 1998;26:265-279 [DOI] [PubMed] [Google Scholar]
- 9. Bennell KL, Matheson G, Meeuwisse W, et al. Risk factors for stress fractures. Sports Med. 1999;28:91-122 [DOI] [PubMed] [Google Scholar]
- 10. Blackman PG. A review of chronic exertional compartment syndrome in the lower leg. Med Sci Sports Exerc. 2000;32(suppl 3):S4-S10 [DOI] [PubMed] [Google Scholar]
- 11. Boden BP, Osbahr DC. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8:344-353 [DOI] [PubMed] [Google Scholar]
- 12. Boden BP, Osbahr DC, Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100-111 [DOI] [PubMed] [Google Scholar]
- 13. Bradshaw C. Exercise-related lower leg pain: vascular. Med Sci Sports Exerc. 2000;32(suppl 3):S34-S36 [DOI] [PubMed] [Google Scholar]
- 14. Brennan FH, Kane SF. Diagnosis, treatment options, and rehabilitation of chronic lower leg exertional compartment syndrome. Curr Sports Med Rep. 2003;2:247-250 [DOI] [PubMed] [Google Scholar]
- 15. Burne SG, Khan KM, Boudville PB, et al. Risk factors associated with exertional tibial pain: a twelve month prospective clinical study. Br J Sports Med. 2004;38:441-445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clanton TO, Solcher BW. Chronic leg pain in the athlete. Clin Sports Med. 1994;13:743-759 [PubMed] [Google Scholar]
- 17. Detmer D. Chronic shin splints: classification and management of medial tibial stress syndrome. Sports Med. 1986;3:436-446 [DOI] [PubMed] [Google Scholar]
- 18. Edmundsson D, Toolanen G, Thornell L-E, Stal P. Evidence for low muscle capillary supply as a pathogenic factor in chronic compartment syndrome. Scand J Med Sci Sports. 2010;20:805-813 [DOI] [PubMed] [Google Scholar]
- 19. Edwards PH, Wright ML, Hartman JF. A practical approach for the differential diagnosis of chronic leg pain in the athlete. Am J Sports Med. 2005;33:1241-1249 [DOI] [PubMed] [Google Scholar]
- 20. Ehsan O, Darwish A, Edmundson C, et al. Non-traumatic lower limb vascular complications in endurance athletes: review of literature. Eur J Vasc Endovasc Surg. 2004;28:1-8 [DOI] [PubMed] [Google Scholar]
- 21. Fraipont MJ, Adamson GJ. Chronic exertional compartment syndrome. J Am Acad Orthop Surg. 2003;11:268-276 [DOI] [PubMed] [Google Scholar]
- 22. Fredericson M, Bergman G, Hoffman K, Dillingham M. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23:427-481 [DOI] [PubMed] [Google Scholar]
- 23. Fredericson M, Jennings F, Beaulieu C, Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17:309-325 [DOI] [PubMed] [Google Scholar]
- 24. Gaeta M, Minutoli F, Scribano E, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235:553-561 [DOI] [PubMed] [Google Scholar]
- 25. Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med. 2009;2:127-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Geslin GE, Thrall JH, Espinosa JL, et al. Early detection of stress fractures using Tc-99m-polyphosphate. Radiology. 1976;121:683-687 [DOI] [PubMed] [Google Scholar]
- 27. Hoch AZ, Pepper M, Akuthota V. Stress fractures and knee injuries in runners. Phys Med Rehabil Clin N Am. 2005;16:749-777 [DOI] [PubMed] [Google Scholar]
- 28. Howard JL. Evaluation of outcomes in patients following surgical treatment of CECS of the leg. Clin J Sport Med. 2000;10:176-184 [DOI] [PubMed] [Google Scholar]
- 29. Hubbard TJ, Carpenter EM, Cordova ML. Contributing factors to medial tibial stress syndrome; a prospective investigation. Med Sci Sports Exerc. 2009;41:490-496 [DOI] [PubMed] [Google Scholar]
- 30. Hutchinson M, Ireland M. Chronic exertional compartment syndrome: gauging pressure. Phys Sportsmed. 1999;27:101. [DOI] [PubMed] [Google Scholar]
- 31. Kaeding CC, Yu JR, Wright R, Amendola A, Spindler KP. Management and return to play of stress fractures. Clin J Sport Med. 2005;15:442-447 [DOI] [PubMed] [Google Scholar]
- 32. Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk factors for recurrent stress fractures in athletes. Am J Sports Med. 2001;29:304-310 [DOI] [PubMed] [Google Scholar]
- 33. Kortebein PM, Kaufman KR, Basford JR, Stuart MJ. Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(suppl 3):27S-33S [DOI] [PubMed] [Google Scholar]
- 34. Leach RE, Purnell MB, Saito A. Peroneal nerve entrapment in runners. Am J Sports Med. 1989;17:287-291 [DOI] [PubMed] [Google Scholar]
- 35. MacIntyre JG, Taunton JE, Clement DB, et al. Running Injuries: a clinical study of 4,173 cases. Clin J Sport Med. 1991;1:81-87 [Google Scholar]
- 36. Matsen FA, 3rd, Mayo KA, Sheridan GW, Krugmire RB., Jr Monitoring of intramuscular pressure. Surgery. 1976;79:702-709 [PubMed] [Google Scholar]
- 37. McCrory P, Bell S, Bradshaw C. Nerve entrapment of the lower leg, ankle and foot in sport. Sports Med. 2002;32:371-391 [DOI] [PubMed] [Google Scholar]
- 38. McDermott MM, Criqui MH, Liu K, et al. Lower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease. J Vasc Surg. 2000;32:1164-1171 [DOI] [PubMed] [Google Scholar]
- 39. Meier TO, Schneider E, Amann-Vesti B. Long-term follow-up of patients with popliteal artery entrapment syndrome treated by endoluminal revascularization. Vasa. 2010;39:189-195 [DOI] [PubMed] [Google Scholar]
- 40. Moen MH, Bongers T, Bakker EWP, et al. The additional value of a pneumatic brace in the treatment of recruits with medial tibial stress syndrome; a randomized study. JR Army Med Corps. 2010;156:236-240 [DOI] [PubMed] [Google Scholar]
- 41. Moen MH, Bongers T, Bakker W, et al. Risk factors and prognostic indicators for medial tibial stress syndrome [published online ahead of print June 18, 2010]. Scand J Med Sci Sports. [DOI] [PubMed] [Google Scholar]
- 42. Moen MH, Rayer S, Schipper M, et al. Shockwave treatment for medial tibial stress syndrome in athletes; a prospective controlled study [published online ahead of print February 3, 2011]. Br J Sports Med. [DOI] [PubMed] [Google Scholar]
- 43. Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: a critical review. Sports Med. 2009;39:523-546 [DOI] [PubMed] [Google Scholar]
- 44. Murphy DF, Connolly DAJ, Beynnon BD. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37:13-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Peck E, Finnoff JT, Smith J, Curtiss H, Muir J, Hollman JH. Accuracy of palpation-guided needle tip placement into deep and superficial posterior leg compartments [published online ahead of print May 26, 2011]. Am J Sports Med. [DOI] [PubMed] [Google Scholar]
- 46. Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18:35-40 [DOI] [PubMed] [Google Scholar]
- 47. Pham TT, Kapur R, Harwood MI. Exertional leg pain: teasing out arterial entrapments. Curr Sports Med Rep. 2007;6:371-375 [PubMed] [Google Scholar]
- 48. Plisky MS, Rauh MJ, Heiderscheit B, Underwood FB, Tank RT. Medial tibial stress syndrome in high school cross-country runners: incidence and risk factors. J Orthop Sports Phys Ther. 2007;37:40-47 [DOI] [PubMed] [Google Scholar]
- 49. Rome K, Handoll HH, Ashford RL. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005;2:CD000450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rompe JD, Cacchio A, Furia JP, Maffulli N. Low-energy extracorporeal shock wave therapy as a treatment for medial tibial stress syndrome. Am J Sports Med. 2010;38:125-132 [DOI] [PubMed] [Google Scholar]
- 51. Schon LC. Nerve entrapment, neuropathy, and nerve dysfunction in athletes. Orthop Clin North Am. 1994;25:47-59 [PubMed] [Google Scholar]
- 52. Schubert AG. Exertional compartment syndrome: review of the literature and proposed rehabilitation guidelines following surgical release. Int J Sports Phys Ther. 2011;6:126-141 [PMC free article] [PubMed] [Google Scholar]
- 53. Sterling JC, Edelstein DW, Calvo RD, Webb R., II Stress fractures in the athlete: diagnosis and management. Sports Med. 1992;14:336-346 [DOI] [PubMed] [Google Scholar]
- 54. Stickley CD, Hetzler RK, Kimura IF, Lozanoff S. Crural fascia and muscle origins related to medial tibial stress syndrome symptom location. Med Sci Sports Exerc. 2009;41:1991-1996 [DOI] [PubMed] [Google Scholar]
- 55. Touliopolous S, Hershman EB. Lower leg pain: diagnosis and treatment of compartment syndromes and other pain syndromes of the leg. Sports Med. 1999;27:193-204 [DOI] [PubMed] [Google Scholar]
- 56. Turnipseed WD. Functional popliteal artery entrapment syndrome: a poorly understood and often missed diagnosis that is frequently mistreated. J Vasc Surg. 2009;49:1189-1195 [DOI] [PubMed] [Google Scholar]
- 57. Van Gent RN, Siem D, van Middlekoop M, van Os AG, Bierma-Zeinstra SMA, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41:469-480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Verma RB, Sherman O. Athletic stress fractures, part I: history, epidemiology, physiology, risk factors, radiography, diagnosis, and treatment. Am J Orthop (Belle Mead NJ). 2001;30:798-806 [PubMed] [Google Scholar]
- 59. Wen DY. Risk factors for overuse injuries in runners. Curr Sports Med Rep. 2007;6:307-313 [PubMed] [Google Scholar]
- 60. Wilbourne A. Electrodiagnostic testing of neurologic injuries in athletes. Clin Sports Med. 1990;9:229-245 [PubMed] [Google Scholar]
- 61. Wilcox JR, Moniot AL, Green JP. Bone scanning in the evaluation of exercise related stress injuries. Radiology. 1977;123:699-703 [DOI] [PubMed] [Google Scholar]
- 62. Wilder RP, Sethi S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55-81 [DOI] [PubMed] [Google Scholar]
- 63. Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004;32:722-780 [DOI] [PubMed] [Google Scholar]
- 64. Zwas ST, Elkanovitch R, Frank G. Interpretation and classification of bone scintigraphic findings in stress fractures. J Nucl Med. 1987;28:452-457 [PubMed] [Google Scholar]


