Abstract
Context:
Time allowing, euhydration can be achieved in the vast majority of individuals by drinking and eating normal beverages and meals. Important to the competitive athlete is prevention and treatment of dehydration and exercise-associated muscle cramps, as they are linked to a decline in athletic performance. Intravenous (IV) prehydration and rehydration has been proposed as an ergogenic aid to achieve euhydration more effectively and efficiently.
Evidence Acquisition:
PubMed database was searched in November 2011 for all English-language articles related to IV utilization in sport using the keywords intravenous, fluid requirements, rehydration, hydration, athlete, sport, exercise, volume expansion, and performance.
Results:
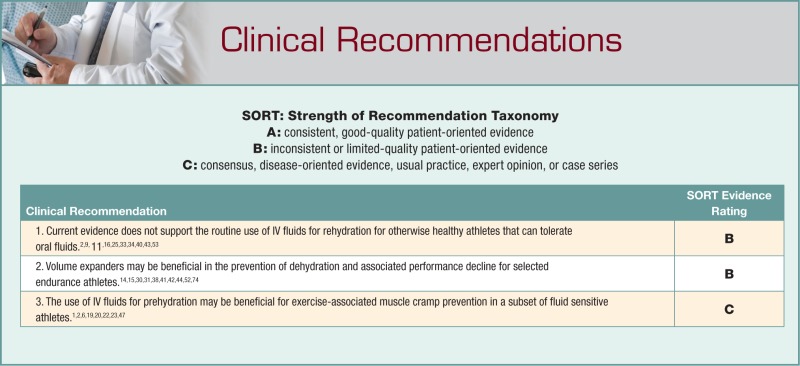
Limited evidence exists for prehydration with IV fluids. Although anecdotal evidence does exist, at this time there are no high-level studies confirming that IV prehydration prevents dehydration or the onset of exercise-associated muscle cramps. Currently, there are no published studies describing IV fluid use during the course of an event, at intermission, or after the event as an ergogenic aid.
Conclusion:
The use of IV fluid may be beneficial for a subset of fluid-sensitive athletes; this should be reserved for high-level athletes with strong histories of symptoms in well-monitored settings. Volume expanders may also be beneficial for some athletes. IV fluids and plasma binders are not allowed in World Anti-Doping Agency–governed competitions. Routine IV therapy cannot be recommended as best practice for the majority of athletes.
Keywords: intravenous fluids, rehydration, hydration, athlete, volume expander
Traditionally, the use of intravenous (IV) administration of fluids has been reserved for the treatment of clinical dehydration and in the setting of presumed heat illness in the collapsed athlete.12,26,56 Treatment of exercise-associated hyponatremia with hypertonic IV infusion to correct plasma sodium levels is also a standard and accepted use of IV fluid infusions.35,57,69,70 Additionally, athletes who present for medical care with hypernatremia who cannot tolerate oral fluids can benefit from IV fluids.28
In clinical practice, the use of IV fluids is more widespread, in both the prevention and treatment of exercise-related conditions. With modern sports’ premium on winning, it only follows that individuals and teams look for performance advantages.22 This mind-set has led to an expanded role for IV hydration outside the context of medical emergencies to include prevention and rapid treatment of dehydration and exercise-associated muscle cramps (EAMC). Important to the competitive athlete is prevention of dehydration as it is linked to a decline in athletic performance.7 Among elite triathletes, muscle cramping is one of the most common reasons cited for not finishing.63
Safety of the athlete is always a primary concern of the treating physician, and avoiding harm is imperative. Comparing IV versus oral hydration methodologies reveals the following differences. First, IV hydration has increased risks relative to oral hydration (Table 1).36,72 Even though severe complications are relatively low, one must consider infection, bleeding, soft tissue infiltration, and air embolism as potential complications that are nonexistent with oral hydration.8,36,72 Second, physiologically, IV hydration bypasses the oropharyngeal reflex and the associated cascade of digestive enzymes and hormones. The potential consequences of these differences are poorly understood in the context of athletic performance.
Table 1.
| Infection/thrombophlebitis |
| Bleeding, hematoma/arterial puncture |
| Soft tissue infiltration/extravasation |
| Air embolism |
| Needle stick to provider |
In addition to the safety of IV rehydration, the practitioner must consider legal and ethical questions.8 According to World Anti-Doping Agency regulations, the routine practice of administering IV fluids (>50 mL per 6 hours) to healthy individuals is prohibited. The code states the following in section M2, numeral 2: “Intravenous infusions and/or injections of more than 50 mL per 6 hour period are prohibited except for those legitimately received in the course of hospital admissions or clinical investigations.”75 There are numerous sports and governing bodies that are not subject to the World Anti-Doping Agency’s jurisdiction, including the National Collegiate Athletic Association and most professional leagues in the United States. The association does not have IV utilization guidelines, nor does it include IV fluids among the current banned substances for sports other than wrestling.73 For National Collegiate Athletic Association wrestling, “artificial means of rehydration (that is, intravenous hydration) are also prohibited to allow participation and use of such is a violation of weight-management rules.”48
Homeostasis
Heat is produced by the metabolic demand of the contractile elements of muscle during exercise.1,2 This heat is transferred from the exercising muscles through the circulatory system and subsequently needs to be dissipated to the environment.22,32,45 Activation of the capillaries supplying the skin is the primary means of this action.1 It follows that heat may then be transferred by radiation, convection, conduction, and evaporative heat loss.45 Vaporization of sweat accounts for 80% of heat loss in hot, dry atmospheric conditions. This mechanism of water loss is the major contributor for exercise-associated dehydration.45,67
Factoring both water and electrolyte loss is extremely important to an athlete.7 The rate of water loss can be quantified through measurement of sweat rate.47 Pre- and postexercise body weight measurements are the most common means to estimate overall water loss but are condition specific.1,2,45 More elaborate indices of dehydration can be measured using blood and urine samples, but these tests are often impractical or unavailable to most athletes.55 Sweat composition is another parameter that is difficult to directly measure. Furthermore, sweat composition is highly variable, as body weight, genetics, heat acclimatization, and metabolic efficiency all influence the sweat rate and composition.32,64
It appears that 1% to 2% body weight loss is well tolerated by the exercising athlete.2,47 Dehydration, defined as greater than 2% loss of body weight, can negatively affect performance.2,8,29,47 In highly trained endurance athletes, plasma volume and sodium serum concentration were preserved despite a 5% body weight loss.27 In Ironman triathletes, dehydration to 5% body weight loss did not correlate with occurrence of medical complications.65,66 As degree of dehydration increases, more physiological detrimental effects may occur (Table 2). This finding is more pronounced in the endurance athlete performing in hot and humid conditions.45,67 Progressive dehydration can lead to diminished cognitive function and may, in severe cases (>12%), cause death.
Table 2.
Dehydration and clinical effects on performance.67
| 0%-2% | No effect on performance |
| 2% | Decrease in aerobic capacity, especially in warm environmental conditions |
| 3%-5% | Decrease in aerobic capacity continues, loss of anaerobic capacity begins |
| 5%-7% | Cognitive function begins to deteriorate |
| >7% | Severe electrolyte disturbances, continued cognitive decline, progressive along continuum until possible death |
Fluid Requirements
Preexercise
Prior to exercise, it is highly recommended to address an athlete’s fluid status.47 There are multiple published guidelines regarding prehydration.7,23 The American College of Sports Medicine has published a position statement including specific recommendations for preexercise hydration.2 Its recommendations include the following: hydration should begin hours prior to exercise, especially if known deficits are present, and fluids should be consumed at a slow, steady rate, with 5 to 7 mL/kg taken 4 hours prior to exercise. If urine output is insufficient, the color is dark, or the specific gravity is greater than 1.020,4,50,55 it is recommended to consume an additional 3 to 5 mL/kg 2 hours prior to exercise.2,3
Absorption rate is influenced by the osmolality of the fluid.24 In a study by Gisofli, the concentration of sodium (0, 20, 50 mEq) was varied to determine if absorption was based on the sodium ion. Sodium concentration did not produce significant changes in the rate of absorption but was primarily dependent on carbohydrate concentration.24 Subjects ingested 1100 mL per hour of drink, with an average absorption rate of 550 mL per hour. This represented 50% of the ingested fluids per hour. The sweat rate was also measured during this time and was 634 mL per hour. Therefore, absorbed fluid represented 86% of fluid loss through sweat. Again, there were no differences among varying sodium concentrations.24 This study represents a model for orally ingested fluids availability for utilization by the exercising athlete.
Rehydration
Time allowing, euhydration can be achieved in the vast majority of individuals by drinking and eating normal beverages and meals.29 If rapid recovery from dehydration is desired, one should ingest 1.5 L of fluid for each kilogram of body weight lost. Replacing 150% of body weight loss over 60 minutes has been tolerated without complications.68 Even though the majority of cases of dehydration can be treated via oral consumption, IV treatment of severe dehydration (>7% body weight loss), exertional heat illness, nausea, emesis, or diarrhea, and in those who cannot ingest oral fluids for other reasons, is clinically indicated.2,3,7,23,68 Otherwise, as the American College of Sports Medicine consensus guidelines state, “IV fluids do not provide an advantage over drinking oral fluids and electrolytes.”2
IV Fluid Hydration Before and During Exercise
Performance Data
Limited evidence exists for prehydration with IV fluids. At the time of this publication, only 1 clinical trial has been published comparing the exercise performance of a group prehydrated with rapidly infused IV (normal saline) and euhydrated (oral) subjects.34 Ten moderately fit first responders wearing chemical protective clothing exercised on a treadmill. Hyperhydration occurred prior to exercise on the treadmill. No significant differences between the 2 groups were found for maximum heart rate, maximum core temperature, and exercise duration.34
The use of IV fluid for prehydration is difficult to quantify. Anecdotally, IV hydration is common among some teams. A recent survey of the National Football League teams revealed that 75% (24 of 32) of the teams utilized IV infusion of fluids for prehydration in at least some otherwise healthy individuals.22 The most common reason cited was the prevention of muscle cramps (23 of 24 teams). Of teams that administered IV fluids prior to competing, there was an average of 5 to 7 athletes per team receiving IV infusions.22 Prior to this survey, the use of IV fluid hydration had not been evaluated in other cohorts of athletes.13,22,51
Timing of IV and the type of fluids utilized prior to competition had not been studied regarding exercise performance. In the National Football League, an average of 1.5 L of normal saline was administered approximately 2.5 hours prior to competition.22 Further research needs to be completed before any recommendation can be made regarding the type of fluids administered to otherwise healthy athletes (Table 3).
Table 3.
Fluids used for intravenous hydration.
| 0.9% normal saline |
| 0.45% normal saline |
| Lactated ringer’s |
| D5 0.45% normal saline |
The effect of an IV infusion during exercise has been studied.16 Although impractical in the competing athlete, the effect of an IV saline infusion versus no infusion during cycling has been compared. Nine males exercised to exhaustion at 84.0% ± 3.14% of maximum O2 consumption on a cycle ergometer while receiving no fluids or an infusion of 0.9% normal saline (mean volume, 1280.3 ± 107.3 mL). Measured variables included core and skin temperatures, time to exhaustion, blood samples, and expired gases (breath by breath).16 Recorded measurements included hydrogen ion concentration, blood lactate level, peak O2 uptake, carbon dioxide production, and end-tidal partial pressure of carbon dioxide. A decreased core temperature (38.5 ± 0.2 versus 39.0 ± 0.2) and heart rate (186.0 ± 5.1 versus 194.1 ± 3.9) was found for the IV group, but this did not translate to improved performance as measured by endurance time. No other significant differences were found between groups.16
The effects of a saline infusion during exercise on a cycle ergometer at 60% of maximum aerobic power for 50 minutes in warm and cool environments have been investigated.49 The control group received no infusion, and measured outcomes included forearm blood flow, heart rate, and esophageal temperature. Restoration of plasma volume via IV infusion decreased heart rate by 6 beats per minute at the 50-minute mark in the warm environment. No difference was found in the cold environment. Importantly, no performance data was reported.49
Similarly, markers of cardiovascular drift that included stroke volume, heart rate, and rectal temperature have been studied in 10 endurance-trained athletes who cycled in a 22°C room for 2 hours.25 The study group received an IV infusion, and a control group received no fluid replacement. There was no oral fluid replacement group in the study. No difference between the groups was demonstrated at 1 hour of exercise. However, after 2 hours of exercise, the rectal temperature was 0.6° higher in the group not receiving IV infusion. Also, stroke volume and cardiac output were 11% to 16% lower in the control group versus the IV infusion group.25
Exertional Muscle Cramp Prevention
Exercise-associated muscle cramps are a major problem during competition for many athletes, including team, individual, and endurance athletes.63 Some controversy exists regarding the etiology of EAMC; the cause is likely multifactorial. Recent evidence suggests the etiology of EAMC is related to muscle fatigue and neuronal excitability.60,61 Several studies have shown no correlation between hydration status or electrolyte concentrations with EAMC.37,62,71 However, there may be a subset of muscle cramping that is associated with a loss of both body fluid and sodium. These individuals are the so-called heavy sweaters.6,19,20,47 Although anecdotal evidence does exist, at this time there are no high-level studies confirming IV prehydration prevents EAMC.1,2,23 Further studies need to be performed assessing the efficacy of IV fluids in the prevention of muscle cramping.1
IV Volume Expanders
Hyperhydration through the use of plasma volume expanders may be accomplished via oral or IV routes.18,52 Glycerol is the primary agent for oral hyperhydration.14,30,38,42,44
Glycerol hyperhydration and rehydration may benefit endurance athletes performing in hot and humid environmental conditions.52 Glycerol hyperhydration allows an excess of 1.5 L of hydration prior to an event.52 Current recommendations for endurance athletes intending to hyperhydrate with glycerol are 1.2 g/kg in 26 mL/kg of fluid over a period of 60 minutes, ending 30 minutes prior to exercise.52 Side effects from glycerol include nausea, gastrointestinal discomfort, and light-headedness, which sometimes preclude its utilization.52 There are IV formulations with comparable solutes for plasma volume expansion.18
The infusion of 6% dextran solution (403 ± 21 mL) on stroke volume during submaximal exercise resulted in an 11% increase in stroke volume in the untrained men but no increase in endurance-trained men.31 Infusion of dextran above 400 mL did not result in a further increase in stroke volume.
In a follow-up study, maximal oxygen uptake and exercise time to fatigue were measured after untrained men were infused with either 200 to 300 mL or 500 to 600 mL of 6% dextran.15 The elevation of plasma volume by 200 to 300 mL via dextran infusion resulted in 15% increase in stroke volume, 4% increase in VO2 max, and an increase in the exercise time to fatigue. In contrast, further expansion of plasma volume to 500 to 600 mL resulted in excessive hemodilution and return to baseline VO2 max and exercise time to exhaustion.15
IV infusion of 6% dextran was also studied in elite endurance-trained cyclists chosen to reflect high baseline blood volumes via training adaptations.74 Infusion of 6% dextran increased blood volume (547 ± 61 mL). No change in maximal oxygen intake (VO2 max) or endurance performance (time to exhaustion at 95% VO2 max) was found. Highly trained athletes may already be at the optimum blood volume, which is at or near the limits of their diastolic reserve capacity.74 Hypervolemia can be induced through either training adaptations or acute volume expansion with 6% dextran in euvolemic subjects.41 Both hypervolemic states showed improved cycling time trial performance, but no difference was seen between the hyperhydrated states.41
Albumin has been investigated for the purpose of volume expansion.59 Seven unacclimatized male subjects received either an albumin infusion (50 g in 200 mL) or normal saline (200 mL) on 2 separate occasions and performed 90-minute walks at 45% VO2 max in a warm environment (45°C and 20% room humidity). The albumin infusion increased plasma volume 13% over the saline infusion. There were lower heart rates in the albumin infusion group at 25 minutes and 40 minutes. No differences were found in performance time, final heart rate, or rectal temperature between the 2 groups.59
Despite the potential advantages for endurance athletes, the use of volume expanders by both oral and IV routes is prohibited under World Anti-Doping Agency bylaws—under section S5 of World Anti-Doping Agency’s prohibited list: “plasma expanders (eg glycerol; IV administration of albumin, dextran, hydroxyethyl starch and mannitol) . . . and other substances with similar biological effect(s).”75
Rehydration with IV Fluids
Fluid hydration during an event is critical for preventing the unwanted effects of dehydration. Currently, there are no published studies describing IV fluid use during the course of an event, at intermission, or after the event as an ergogenic aid. In these settings, there is a perceived benefit for the convenience and speed of fluid replacement. The speed of replacing plasma volume by IV infusion is primarily a consequence of bypassing gastric emptying, which is volume dependent.3,7,24,46
Large volumes of IV fluid can be given over a short period.10,40 An 18G peripheral IV can provide 50 to 60 mL per minute of IV fluid by gravity.17 No high-level studies have determined the ideal rate for IV fluids hydration in healthy subjects. As with all IV therapy, the speed and amount should be individualized to the clinical condition of the athlete. In emergency trauma situations, replacement of one half the estimated fluid/blood losses may be performed over 30 minutes followed by reassessment of the clinical status.17 Resuscitation may require replacement of up to 3 times the estimated blood loss with a crystalloid fluid.17
The tonicity of IV fluid rehydration has been investigated in 8 men in a dehydration protocol (185 minutes with a 4% body weight loss).39 Rehydration was achieved with 0.9% IV normal saline, 0.45% IV normal saline, or 0.45% oral normal saline over the first 45 minutes of a 100-minute rest period with a goal of reducing the deficit to 2%. The subjects then stood for 20 minutes at 36°C, followed by walking at 50% VO2 max for 90 minutes. Neither the tonicity nor mode of hydration resulted in improved speed of rehydration, greater fluid retention, or improved performance.39
Studies utilizing labeled deuterium oxide (D2O) fluid show that during exercise D2O appears in sweat 10 minutes after oral ingestion.21 A follow-up study compared ingestion of labeled oral fluid versus a combination of oral and IV labeled D2O. After dehydration, subjects were rehydrated and exercised until D2O was measured in sweat. There were no differences in the groups despite an apparent increase in plasma volume afforded by IV rehydration.21
Exertional Muscle Cramp Treatment
There are no published studies on the treatment of EAMC with IV fluids during competition. Muscle cramping is multifactorial, and current evidence indicates fatigue and neural processes.37,61-63,71 However, current best practice recommendations are to replace fluid and salt losses, eliminating potential muscle cramping.1,19 For a large majority of individuals, this can be accomplished by oral intake of fluid and electrolytes.2 There are beneficial anecdotal reports of EAMC treatment in elite and professional-level athletes with IV hydration during the course of an event. In these situations where time is limited, the speed of IV hydration may more rapidly correct deficits.13,22,51
Rehydration and Performance Data
Athletes frequently need to rapidly replace fluid volumes between training sessions or events when there is limited time (2-a-day practices or stacked training sessions). Some athletes have turned to IV hydration for its speed of fluid administration. Studies evaluating the benefits of IV hydration for repeated performances include a dehydration phase via exercise, a rehydration time, and a second exercise phase.53
The hydration routes in acclimated and nonacclimated highly trained cyclists were studied by dehydrating to 4% body weight loss.9 Rehydration occurred to 2% body weight loss with 0.45% oral or IV fluid. A control group received no fluids. Subjects then cycled at 70% VO2 peak to exhaustion in 37°C. No difference was found in exercise time to exhaustion. Plasma volume was better restored during rehydration with IV fluids at preexercise and 5 minutes of exercise. At 15 minutes, there was no difference between IV and oral rehydration.9
The same study design evaluated perceptual responses to exhaustion after IV or oral rehydration.43 Perceived exertion, thirst, and thermal sensations were measured. Central perceived exertion was lower in the oral rehydration group at 5 and 15 minutes. Overall perceived exertion was lower in the oral rehydration group at 15 minutes. Thermal sensation was higher in IV group at 15 minutes. Thirst ratings were lower at 0, 5, and 15 minutes with oral rehydration. Thus, all measures were more favorable in the oral rehydration group.43
In a similar study, 8 males were dehydrated via a 75-minute phase to 1.7 to 1.8 L of fluid loss.40 The negative fluid balance was replaced in 20 minutes by either IV of 0.45% normal saline or oral rehydration. The participants then completed a heat tolerance (treadmill speed of 2.4 m per second and an incline grade of 2.3%) at 37°C and 45% relative humidity. More rapid restoration of plasma volume was accomplished in the IV treatment group with no advantages over oral rehydration in physiological strain, heat tolerance, ratings of perceived effort, or thermal sensations. Sensation of thirst was lower in the oral rehydration group. Performance (heat tolerance time) was not significantly improved in the IV group.40
Castellani also compared IV versus oral rehydration on same day bouts of exercise.11 A 4% decrease in body weight from exercise at 33°C was followed by rehydration with 0.45% normal saline IV or orally with rest for 2 hours. Walking at 50% maximal O2 consumption resumed at 36C. No difference was found in exercise time to exhaustion. IV and oral rehydration methods were equally effective. Heart rates were statistically higher in the oral rehydration group through 75 minutes of exercise, and there were higher increases in norepinephrine plasma concentrations.11
The effects of IV or oral rehydration on perceived exertion and thirst after a dehydration period of 2 to 4 hours producing a 4% body weight reduction have been tested.58 Following rehydration and rest over 2 hours, 8 men walked at VO2 max 50% for 90 minutes at 36°C. Thirst ratings were not different prior to rehydration and exercise. Oral rehydration had improved ratings for physical effort and thirst.58
The effect of IV hydration on recovery following marathon running has been studied.54 IV fluids were administered immediately postmarathon to assess time to recovery in 66 participants. The experimental group received 2.5 L of 2.5% glucose/0.45% sodium chloride solution, whereas the placebo group received 100 mL of 0.9% sodium chloride solution. No significant differences between the groups were found for time to recovery, number of days with pain, number of days with stiffness, sleep disturbance, fatigue, rectal temperature, and loss of appetite.54
In addition to studies performed on athletes, IV versus oral rehydration was investigated in firefighters performing exercise in thermal protective clothing.33 After initial exercise to induce dehydration, rehydration equal to body mass lost was met with water, sport drink, or normal saline IV infusion followed by more exercise. No significant differences were found in core temperatures, heart rates, or performance.
The current data suggest that IV rehydration is faster than oral. There may be physiological benefits of decreased heart rate and norepinephrine in athletes rehydrated via IV route, but the clinical significance is not known. Oral rehydration does decrease thirst better than IV rehydration and may decrease perceived exertion.
Rehydration and Muscle Damage
Muscle damage during exercise in the heat was assessed by myoglobin and creatine kinase.5 Eleven healthy men completed 4 experimental trials comparing oral, IV, oral and IV, and ad libitum rehydration techniques after a 4% body mass reduction. Rehydration to −2% body mass (except in the ad libitum) was followed by a standard exercise challenge of treadmill running, sprinting, and box lifting. Postexercise blood 1 hour and 24 hours showed no differences in circulating myoglobin or creatine kinase.5
Conclusion
Convincing research to support IV fluid administration prior to competition for performance enhancement, dehydration prevention, or muscle cramp prevention does not exist. Current studies do not support the use of IV fluids for rehydration when an athlete can tolerate oral fluids.9,11,33,40,53 IV administration of fluids can rapidly replace plasma volume. In the process, the oropharyngeal reflex and cascade of gastrointestinal hormones are bypassed with unknown consequences to the exercising athlete. The rapid increase in plasma volume is transient, and no measureable difference between IV and oral prehydration exists after 15 minutes of exercise.9,40
The use of IV fluid may be beneficial for a subset of fluid sensitive athletes1,2,6,19,20,22,23,47; this should be reserved for high-level athletes with strong histories of symptoms in well-monitored settings. Volume expanders may also be beneficial for some athletes.52 IV fluids and plasma binders are not allowed in World Anti-Doping Agency–governed competitions.75 Routine IV therapy cannot be recommended as best practice for the majority of athletes.
References
- 1. American College of Sports Medicine; Armstrong LE, Casa DJ, Millard-Stafford M, et al. Exertional heat illness during training and competition: ACSM position stand. Med Sci Sports Exerc. 2007;39(3):556-572 [DOI] [PubMed] [Google Scholar]
- 2. American College of Sports Medicine; Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 2007;39(2):377-390 [DOI] [PubMed] [Google Scholar]
- 3. American Dietetic Association; Dietitians of Canada; American College of Sports Medicine; Rodriguez NR, Di Marco NM, Langley S. American College of Sports Medicine position stand: nutrition and athletic performance. Med Sci Sports Exerc. 2009;41(3):709-731 [DOI] [PubMed] [Google Scholar]
- 4. Armstrong LE, Soto JA, Hacker FT, Jr, Casa DJ, Kavouras SA, Maresh CM. Urinary indices during dehydration, exercise, and rehydration. Int J Sport Nutr. 1998;8(4):345-355 [DOI] [PubMed] [Google Scholar]
- 5. Beasley KN, Lee EC, McDermott BP, et al. The effect of oral vs intravenous rehydration on circulating myoglobin and creatine kinase. J Strength Cond Res. 2010;24(1):60-67 [DOI] [PubMed] [Google Scholar]
- 6. Bergeron MF. Muscle cramps during exercise: is it fatigue or electrolyte deficit? Curr Sports Med Rep. 2008;7:S50-S55 [Google Scholar]
- 7. Casa DJ. Exercise in the heat: II. Critical concepts in rehydration, exertional heat illnesses, and maximizing athletic performance. J Athl Train. 1999;34(3):253-262 [PMC free article] [PubMed] [Google Scholar]
- 8. Casa DJ, Ganio MS, Lopez RM, McDermott BP, Armstrong LE, Maresh CM. Intravenous versus oral rehydration: physiological, performance, and legal considerations. Curr Sports Med Rep. 2008;7(4):S41-S49 [Google Scholar]
- 9. Casa DJ, Maresh CM, Armstrong LE, et al. Intravenous versus oral rehydration during a brief period: responses to subsequent exercise in the heat. Med Sci Sports Exerc. 2000;32(1):124-133 [DOI] [PubMed] [Google Scholar]
- 10. Castellani JW, Maresh CM, Armstrong LE, et al. Intravenous vs oral rehydration: effects on subsequent exercise-heat stress. J Appl Physiol. 2000;89(6):2117-2122 [DOI] [PubMed] [Google Scholar]
- 11. Castellani JW, Maresh CM, Armstrong LE, et al. Intravenous vs oral rehydration: effects on subsequent heat stress. J Appl Physiol. 1997;82(3):799-807 [DOI] [PubMed] [Google Scholar]
- 12. Childress MA, O’Connor FG, Levine BD. Exertional collapse in the runner: evaluation and management in fieldside and office-based settings. Clin Sports Med. 2010;29(3):459-476 [DOI] [PubMed] [Google Scholar]
- 13. Coombes JS, Piet van Rosendal S. Use of intravenous rehydration in the National Football League. Clin J Sport Med. 2011;21(3):185-186 [DOI] [PubMed] [Google Scholar]
- 14. Coutts A, Reaburn P, Mummery K, Holmes M. The effect of glycerol hyperhydration on Olympic distance triathlon performance in high ambient temperatures. Int J Sport Nutr Exerc Metab. 2002;12(1):105-119 [DOI] [PubMed] [Google Scholar]
- 15. Coyle EF, Hopper MK, Coggan AR. Maximal oxygen uptake relative to plasma volume expansion. Int J Sports Med. 1990;11(2):116-119 [DOI] [PubMed] [Google Scholar]
- 16. Deschamps A, Levy RD, Cosio MG, Marliss EB, Magder S. Effect of saline infusion on body temperature and endurance during heavy exercise. J Appl Physiol. 1989;66(6):2799-2804 [DOI] [PubMed] [Google Scholar]
- 17. Doherty GM. Fluid and electrolyte management. In: Doherty GM. ed. Current Diagnosis and Treatment: Surgery. 13th ed. New York, NY: McGraw-Hill; 2010 [Google Scholar]
- 18. Drugs in Sport. 5th ed. New York, NY: Routledge; 2011 [Google Scholar]
- 19. Eichner ER. Heat cramps in sport. Curr Sports Med Rep. 2008;7:178-179 [DOI] [PubMed] [Google Scholar]
- 20. Eichner ER. The role of sodium in “heat cramping”. Sports Med. 2007;37(4-5):368-370 [DOI] [PubMed] [Google Scholar]
- 21. Emmanuel H, Casa DJ, Beasley KN, et al. Appearance of D2O in sweat after oral and oral-intravenous rehydration in men. J Strength Cond Res. 2011;25(8):2092-2099 [DOI] [PubMed] [Google Scholar]
- 22. Fitzsimmons S, Tucker A, Martins D. Seventy-five percent of national football teams use pregame hyperhydration with intravenous fluids. Clin J Sport Med. 2011;21(3):192-199 [DOI] [PubMed] [Google Scholar]
- 23. Ganio MS, Casa DJ, Armstrong LE, Maresh CM. Evidence-based approach to lingering hydration questions. Clin J Sports Med. 2007;26(1):1-16 [DOI] [PubMed] [Google Scholar]
- 24. Gisolfi CV, Lambert GP, Summers RW. Intestinal fluid absorption during exercise: role of sport drink osmolality and [Na+]. Med Sci Sports Exerc. 2001;33(6):907-915 [DOI] [PubMed] [Google Scholar]
- 25. Hamilton MT, Gonzalez-Alonso J, Montain SJ, Coyle EF. Fluid replacement and glucose infusion during exercise prevent cardiovascular drift. J Appl Physiol. 1991;71(3):871-877 [DOI] [PubMed] [Google Scholar]
- 26. Hew-Butler T, Boulter J, Godlonton J, Tucker R, Noakes T. Hypernatremia and intravenous fluid resuscitation in collapsed ultramarathon runners. Clin J Sport Med. 2008;18(3):273-278 [DOI] [PubMed] [Google Scholar]
- 27. Hew-Butler T, Collins M, Bosch A, et al. Maintenance of plasma volume and serum sodium concentration despite body weight loss in ironman triathletes. Clin J Sport Med. 2007;17(2):116-122 [DOI] [PubMed] [Google Scholar]
- 28. Hew-Butler T, Sharwood K, Boulter J, et al. Dysnatremia predicts a delayed recovery in collapsed ultramarathon runners. Clin J Sport Med. 2007;17(4):289-296 [DOI] [PubMed] [Google Scholar]
- 29. Hew-Butler T, Verbalis JG, Noakes TD. Updated fluid recommendation: position statement from the International Marathon Medical Directors Association (IMMDA). Clin J Sport Med. 2006;16(4):283-292 [DOI] [PubMed] [Google Scholar]
- 30. Hitchins S, Martin DT, Burke L, et al. Glycerol hyperhydration improves cycle time trial performance in hot humid conditions. Eur J Appl Physiol Occup Physiol. 1999;80(5):494-501 [DOI] [PubMed] [Google Scholar]
- 31. Hopper MK, Coggan AR, Coyle EF. Exercise stroke volume relative to plasma-volume expansion. J Appl Physiol. 1988;64(1):404-408 [DOI] [PubMed] [Google Scholar]
- 32. Hosey RG, Glazer JL. The ergogenics of fluid and electrolyte balance. Curr Sports Med Rep. 2004;3(4):219-223 [DOI] [PubMed] [Google Scholar]
- 33. Hostler D, Bednez JC, Kerin S, et al. Comparison of rehydration for rehabilitation of firefighters performing heavy exercise in thermal protective clothing: a report from the Fireground Rehab Evaluation (FIRE) trial. Prehosp Emerg Care. 2010;14(2):194-201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hostler D, Gallagher M, Jr, Goss FL, et al. The effect of hyperhydration on physiological and perceived strain during treadmill exercise in personal protective equipment. Eur J Appl Physiol. 2009;105(4):607-613 [DOI] [PubMed] [Google Scholar]
- 35. Hsieh M. Recommendations for treatment of hyponatremia at endurance events. Sports Med. 2004;34(4):231-238 [DOI] [PubMed] [Google Scholar]
- 36. Ingram P, Lavery I. Peripheral intravenous therapy: key risks and implications for practice. Nurs Stand. 2005;19(46):55-64 [DOI] [PubMed] [Google Scholar]
- 37. Jung AP, Bishop PA, Al-Nawwas A, Dale RB. Influence of hydration and electrolyte supplementation on incidence and time to onset of exercise-associated muscle cramps. J Athl Train. 2005;40(2):71-75 [PMC free article] [PubMed] [Google Scholar]
- 38. Kavouras SA, Armstrong LE, Maresh CM, et al. Rehydration with glycerol: endocrine, cardiovascular, and thermoregulatory responses during exercise in the heat. J Appl Physiol. 2006;100(2):442-450 [DOI] [PubMed] [Google Scholar]
- 39. Kenefick RW, Maresh CM, Armstrong LE, Riebe D, Echegaray ME, Castellani JW. Rehydration with fluid of varying tonicities: effects on fluid regulatory hormones and exercise performance in the heat. J Appl Physiol. 2007;102(5):1899-1905 [DOI] [PubMed] [Google Scholar]
- 40. Kenefick RW, O’Moore KM, Mahood NV, Castellani JW. Rapid IV versus oral rehydration: responses to subsequent exercise heat stress. Med Sci Sports Exerc. 2006;38(12):2125-2131 [DOI] [PubMed] [Google Scholar]
- 41. Luetkemeier MJ, Thomas EL. Hypervolemia and cycling time trial performance. Med Sci Sports Exerc. 1994;26(4):503-509 [PubMed] [Google Scholar]
- 42. Magal M, Webster MJ, Sistrunk LE, et al. Comparison of glycerol and water hydration regimens on tennis-related performance. Med Sci Sports Exerc. 2003;35(1):150-156 [DOI] [PubMed] [Google Scholar]
- 43. Maresh CM, Herrera-Soto JA, Armstrong LE, et al. Perceptual responses in the heat after brief intravenous versus oral rehydration. Med Sci Sports Exerc. 2001;33(6):1039-1045 [DOI] [PubMed] [Google Scholar]
- 44. Marino FE, Kay D, Cannon J. Glycerol hyperhydration fails to improve endurance performance and thermoregulation in humans in a warm humid environment. Pflugers Arch. 2003;446(4):455-462 [DOI] [PubMed] [Google Scholar]
- 45. Maughan RJ. Distance running in hot environments: a thermal challenge to the elite runner. Scand J Med Sci Sports. 2010;20(3):95-102 [DOI] [PubMed] [Google Scholar]
- 46. Maughan RJ, Leiper JB. Limitations to fluid replacement during exercise. Can J Appl Physiol. 1999;24(2):173-187 [DOI] [PubMed] [Google Scholar]
- 47. Maughan RJ, Shirreffs SM. Dehydration and rehydration in competitive sport. Scand J Med Sci Sports. 2010;20(3):40-47 [DOI] [PubMed] [Google Scholar]
- 48. NCAA Wrestling Committee 2012 and 2013 wrestling major rules changes. http://fs.ncaa.org/Docs/rules/wrestling/2011/Rules_changes_for_2012_%202013.pdf
- 49. Nose H, Mack GW, Shi XR, Morimoto K, Nadel ER. Effect of saline infusion during exercise on thermal and circulatory regulations. J Appl Physiol. 1990;69(2):609-616 [DOI] [PubMed] [Google Scholar]
- 50. Osterberg KL, Horswill CA, Baker LB. Pregame urine specific gravity and fluid intake by National Basketball Association players during competition. J Athl Train. 2009;44(1):53-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pellman EJ. National Football League teams and pregame hyperhydration with intravenous fluid: some consideration. Clin J Sport Med. 2011;21(3):187-188 [DOI] [PubMed] [Google Scholar]
- 52. Piet van Rosendal S, Osborne MA, Fassett RG, Coombes JS. Guidelines for glycerol use in hyperhydration and rehydration associated with exercise. Sports Med. 2010;40(2):113-119 [DOI] [PubMed] [Google Scholar]
- 53. Piet van Rosendal S, Osborne MA, Fassett RG, Lancashire B, Coombes JS. Intravenous versus oral rehydration in athletes. Sports Med. 2010;40(4):327-346 [DOI] [PubMed] [Google Scholar]
- 54. Polak AA, van Linge B, Rutten FL, Stijnen T. Effect of intravenous fluid administration on recovery after running a marathon. Br J Sports Med. 1993;27(3):205-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Popowski LA, Oppliger RA, Lambert GP, Johnson RF, Johnson AK, Gisolfi CV. Blood and urinary measures of hydration status during progressive acute dehydration. Med Sci Sports Exerc. 2001;33(5):747-753 [DOI] [PubMed] [Google Scholar]
- 56. Pyne S. Intravenous fluids post marathon, when and why? Sports Med. 2007;37(4-6):434-436 [DOI] [PubMed] [Google Scholar]
- 57. Reid SA, King MJ. Serum biochemistry and morbidity among runners presenting for medical care after an Australian mountain marathon. Clin J Sport Med. 2007;17(4):307-310 [DOI] [PubMed] [Google Scholar]
- 58. Riebe D, Maresh CM, Armstrong LE, et al. Effects of oral and intravenous rehydration on ratings of perceived exertion and thirst. Med Sci Sport Exerc. 1997;29(1):117-124 [DOI] [PubMed] [Google Scholar]
- 59. Sawka MN, Hubbard RW, Francesconi RP, Horstman DH. Effects of acute volume expansion on altering exercise-heat performance. Eur J Appl Physiol Occup Physiol. 1983;51(3):303-312 [DOI] [PubMed] [Google Scholar]
- 60. Schwellnus MP. Cause of exercise associated heat cramps (EAMC): altered neuromuscular control, dehydration, or electrolyte depletion? Br J Sports Med. 2009;43(6):401-408 [DOI] [PubMed] [Google Scholar]
- 61. Schwellnus MP, Drew N, Collins M. Muscle cramping in athletes: risk factors, clinical assessment, and management. Clin Sports Med. 2008;27:183-194 [DOI] [PubMed] [Google Scholar]
- 62. Schwellnus MP, Nicol J, Laubscher R, Noakes TD. Serum electrolyte concentrations and hydration status are not associated with exercise associated muscle cramping (EAMC) in distance runners. Br J Sports Med. 2004;38(4):488-492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Shang G, Collins M, Schwellnus MP. Factors associated with a self-reported history of exercise-associated muscle cramps in ironman triathletes: a case-control study. Clin J Sport Med. 2011;21(3):204-210 [DOI] [PubMed] [Google Scholar]
- 64. Sharp RL. Role of sodium in fluid homeostasis with exercise. J Am Coll Nutr. 2006;25(3):231-239 [DOI] [PubMed] [Google Scholar]
- 65. Sharwood KA, Collins M, Goedecke JH, Wilson G, Noakes TD. Weight changes, medical complications, and performance during an Ironman triathlon. Br J Sports Med. 2004;38(6):718-724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sharwood KA, Collins M, Goedecke J, Wilson G, Noakes T. Weight changes, sodium levels, and performance in the South African Ironman Triathlon. Clin J Sport Med. 2002;12(6):391-399 [DOI] [PubMed] [Google Scholar]
- 67. Shirreffs SM. Conference on “Multidisciplinary approaches to nutritional problems.” Symposium on “Performance, exercise and health.” Hydration, fluids and performance. Proc Nutr Soc 2009;68(1):17-22 [DOI] [PubMed] [Google Scholar]
- 68. Shirreffs SM, Maughan RJ. Volume repletion after exercise-induced volume depletion in humans: replacement of water and sodium losses. Am J Physiol. 1998;274(5)(pt 2):F868-F875 [DOI] [PubMed] [Google Scholar]
- 69. Siegel AJ. Hypertonic (3%) sodium chloride for emergent treatment of exercise-associated hypotonic encephalopathy. Sports Med. 2007;37(4-5):459-462 [DOI] [PubMed] [Google Scholar]
- 70. Speedy DB, Rogers IR, Noakes TD, et al. Diagnosis and prevention of hyponatremia at an ultradistance triathlon. Clin J Sport Med. 2000;10(1):52-58 [DOI] [PubMed] [Google Scholar]
- 71. Sulzer NU, Schwellnus MP, Noakes TD. Serum electrolytes in Ironman triathletes with exercise-associated muscle cramping. Med Sci Sports Exerc. 2005;37(7):1081-1085 [DOI] [PubMed] [Google Scholar]
- 72. Tagalakis V, Kahn SR, Libman M, Blostein M. The epidemiology of peripheral vein infusion thrombophlebitis: a critical review. Am J Med. 2002;113:146-151 [DOI] [PubMed] [Google Scholar]
- 73. 2011-2012 NCAA Sports Medicine Handbook. NCAA.org
- 74. Warburton DE, Gledhill N, Jamnik VK, Krip B, Card N. Induced hypervolemia, cardiac function, VO2max, and performance of elite cyclists. Med Sci Sports Exerc. 1999;31(6):800-808 [DOI] [PubMed] [Google Scholar]
- 75. World anti-doping code: the 2012 prohibited list. http://www.wada-ama.org/Documents/World_Anti-Doping_Program/WADP-Prohibited-list/2012/WADA_Prohibited_List_2012_EN.pdf