Abstract
This case demonstrates the potential serious consequences of the female athlete triad and its effects on bone. Displaced femoral neck stress fractures cause significant morbidity, and this case highlights the preventable nature of this injury. The treatment was focused on improving low energy availability, and, although challenging, improvements were made. This injury could have been prevented if the signs and symptoms of her injury had been addressed and there had been better knowledge of her risk factors. This case highlights the need for further education in the sports and health communities.
Keywords: female athlete triad, low energy availability, cross-country, bone mineral density, menstrual dysfunction, hip fracture
Bone stress injuries encompass a spectrum that ranges from lower grade stress reactions to complete stress fractures. They are a common cause of missed training and competition among athletes. Bone stress injuries develop when bone is unable to withstand the repetitive subthreshold mechanical stresses applied to it, such as with endurance running. The etiology of bone stress injuries in athletes is complex and multifaceted. Primary variables that influence bone’s response to loading and, thus, susceptibility to fracture include gait mechanics, training volume and intensity, bone density, and bone quality.6 Bone density and bone quality are determined by long-term effects of genetics, diet, endocrine status, and exercise history.6 Bone metabolism—influenced by short-term effects of nutrient status, energy availability, and endocrine factors—may additionally affect bone’s ability to repair exercise-induced microdamage.8,13,15,16,35
Epidemiologic studies report a higher rate of bone stress injury among endurance runners compared with athletes in ball or power sports.7,19,25,28,33 This higher risk may be due in part to the repetitive unidirectional loading nature of long-distance running, which continuously stresses certain skeletal sites. Runners’ higher rates of bone injury may also be related to their increased prevalence of the female athlete triad,2,3,5,29,34 which exists along a spectrum of low energy availability, amenorrhea, and osteoporosis.29 Low energy availability develops when dietary energy intake is not sufficient to replenish exercise energy expenditure. This may occur intentionally or unintentionally. It leads to multiple hormonal adaptations that negatively affect the menstrual cycle and bone metabolism.29 Low energy availability may also limit postexercise repair of bone microdamage.6,16 Increasing energy intake and/or reducing energy expenditure should be the focus of treatment for athletes presenting with functional hypothalamic amenorrhea resulting from persistent low energy availability.29
During the early- to mid-adolescent years, processes that promote bone mineralization reach a lifetime peak.14 By age 16.9 ± 1.3 years, adolescents have established approximately 90% of their adult bone mineral content.36 Behaviors that influence the accrual and microstructural integrity of bone during adolescence may affect lifetime fracture risk. It is important to recognize the risk factors that can lead to poor bone health and bone stress injury in this population of athletes.
Case Report
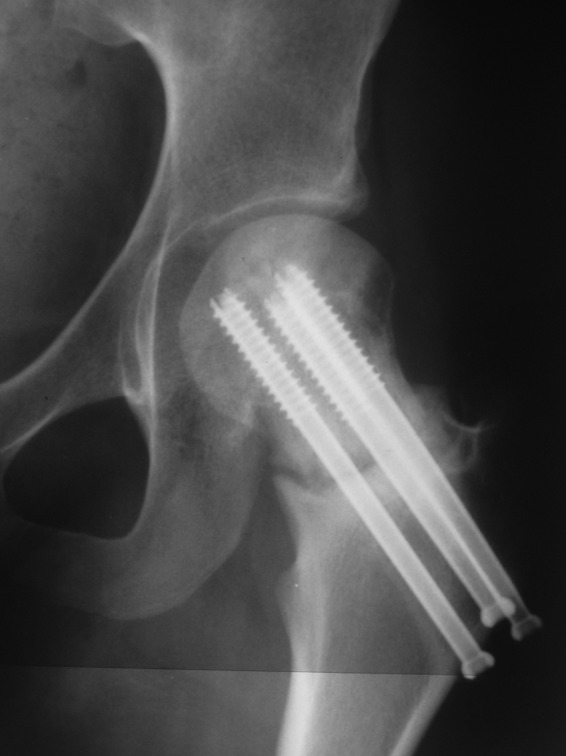
A 15-year-old female cross-country runner presented with a history of 4 weeks of progressively worsening left anterior hip and groin pain. Initially, her pain occurred only upon initiation of running. Over the next 3 weeks, the patient’s pain intensified and was persistent throughout the run. In the week leading up to the acute injury, the patient’s pain was constant and caused her to limp. On the day of a cross-country race, she was having significant pain but was encouraged by her coach to run through the pain. Upon sprinting 20 ft (6 m) from the finish of the race, she heard a loud crack and fell to the ground in pain. As she and her parents were unaware of the severity of her injury, she saw her pediatrician approximately 24 hours after the injury, who immediately referred her to an orthopaedic surgeon for a displaced femoral neck fracture (Figure 1). She was unable to bear weight, and she had severe pain with any motion of the left hip. She underwent an open reduction internal fixation of the fracture with 3 partially threaded titanium screws (7 mm; Figure 2). She was kept nonweightbearing for 8 weeks and partial weightbearing for 4 weeks. For 7 months postinjury, she used a single crutch because of left hip pain and fatigue with long distances. She was in physical therapy and was referred to the osteoporosis center 5 months after surgery for evaluation and treatment of her risk factors and delayed healing.
Figure 1.

Radiograph of pelvis after injury.
Figure 2.

Radiograph of left hip at 6 months.
This adolescent had started running for her high school cross-country team approximately 15 months before her injury. She trained year-round and had taken only 2 weeks off. In the weeks leading up to her injury, she was running approximately 20 to 30 miles per week in 2-month-old shoes and had not changed her mileage, terrain, or intensity. In the past, the patient had been diagnosed with medial tibial stress syndrome and a right hip flexor strain but had no history of fracture or previous bone stress injury.
After menarche at age 12 years, she experienced a few menstrual cycles approximately 8 months apart with no menses in the past 2 years. This is consistent with secondary functional hypothalamic amenorrhea (abnormal hypothalamic-pituitary-gonadal axis function due to low energy availability).29 One year before her injury, she lost 15 pounds due to restrictive eating and was diagnosed with an eating disorder not otherwise specified. She denied purging behaviors, diet pill or laxative use, or excessive exercise for weight loss purposes. She was seeing a dietitian weekly for 1 year before her injury. There was a family history of osteoporosis in a maternal aunt, maternal grandmother, and maternal grandfather without a history of fracture. At the time of the fracture, she was not taking calcium or vitamin D supplements.
At the osteoporosis center, her height was 5 feet 7 inches (1.7 m); weight, 124 lb (56 kg), and body mass index was 19. There were no physical stigmata of anorexia or bulimia nervosa. Table 1 shows results from laboratory tests and a DXA (dual-energy x-ray absorptiometry) scan 5 months from her injury. Seven months after her injury, testing revealed a lower estradiol of 12.7 (normal, 19-528). Her DXA bone mineral density (BMD) Z-scores were normal for her age (Table 1; normal Z-scores are greater than −1.0 per American College of Sports Medicine definitions).29
Table 1.
Patient’s diagnostic tests postinjury.a
| Diagnostic Test | Result | Normal Range |
|---|---|---|
| Laboratory | ||
| Estradiol, pg/mL | 47 | 19-528 |
| Follicle-stimulating hormone, mIU/mL | 6.0 | 1.4-18.1 |
| Luteinizing hormone, mIU/mL | 6.8 | 0.5-9.0 |
| Calcium, mg/dL | 10.4 | 8.9-10.4 |
| Parathyroid hormone, pg/mL | 21 | 15-65 |
| Thyroid-stimulating hormone, µIU/mL | 1.48 | 0.530-3.590 |
| Vitamin D, 25-OH, ng/mL | 40.6 | 32.0-100.0 |
| Prolactin, ng/mL | 7.1 | 3.0-14.4 |
| Dehydroepiandrosterone, ng/dL | 897 | 162-995 |
| 24-hour urine calcium, mg per 24 h | 204.8 | 100.0-300.0 |
| Anti-gliadin antibody IgG, U/mL | 0.9 | 0.0-10.0 |
| Anti-gliadin antibody IgA, U/mL | 1.5 | 0.0-10.0 |
| DXA scan, Z-scores | ||
| Lumbar spine | −0.4 | |
| Total hip | 0.0 | |
| Femoral neck | 0.4 | |
All tests were done at 5 months postinjury, except the calcium, which was done at 9 months.
Treatment focused on improving the patient’s energy availability to resume menstrual function and optimize healing potential. After further weight loss, she was advised to gain weight to a level ≥ 90% of her ideal body weight through dietary changes and modification of exercise. She was referred to a psychologist specializing in eating disorders. Bone-building nutrients including calcium (1200-1500 mg per day) and vitamin D3 (1000-2000 IU per day) were recommended through diet and supplements.
At 6 months, concern for nonunion on radiographs (Figure 2) prompted magnetic resonance imaging, which showed no evidence of avascular necrosis of the femoral head (Figure 3). At 7 months, she was pain-free with walking and low-impact activities. There was evidence of delayed healing on radiographs at 8 months, prompting use of an external bone stimulator for 30 minutes daily. Improving her energy availability was emphasized through increased caloric consumption and bone-building nutrients along with physical activity adjustments. She was still amenorrheic 1 year out from her injury and failed a progesterone challenge test, suggesting that she still had functional hypothalamic amenorrhea. Radiographs at 12 months showed some improvement in fracture healing (Figure 4).
Figure 3.
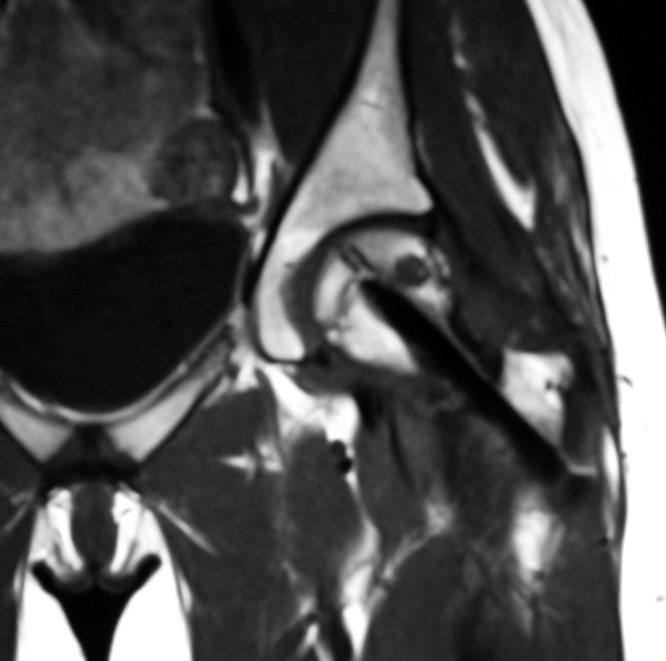
Magnetic resonance imaging of left hip at 6 months.
Figure 4.
Radiograph of left hip at 12 months.
Discussion
This patient exhibited signs and symptoms of the female athlete triad, characterized by low energy availability, functional hypothalamic amenorrhea, and poor bone health.29 Though her BMD values were within the normal range for her chronologic age, she clearly had poor-quality bone. Chronic low energy availability—through disruption of gonadotropin-releasing hormone pulsatility and a subsequent decrease in luteinizing hormone, follicle-stimulating hormone, and estradiol—leads to the reversible suppression of menstrual function known as functional hypothalamic amenorrhea.16,23,24 Therefore, the target of treatment for her menstrual dysfunction was to improve her energy status through diet and exercise modifications.
Previous research studies indicate that, in addition to menstrual dysfunction, chronic energy deficiency leads to hypothalamic and pituitary hormonal disturbances that negatively affect bone metabolism.8,15,16 In a study of regularly menstruating young women, dietary intake and exercise expenditure were controlled for 5 days, yielding either balanced or varying levels of restricted energy availability.16 A dose-related reduction in biomarkers of bone formation was found with energy restriction.16 Bone resorption was increased with more extreme energy restriction.16
Low energy availability that decreases bone formation and increases bone resorption may limit repair of exercise-induced microdamage to bone. Low energy availability is associated with disrupted bone metabolic hormones,4 and it reduces bone mass,9 which increases fracture risk.7,27 Therefore, the antiosteogenic effects of low energy availability combined with the high loading exposure of competitive running may have increased this athlete’s fracture risk. Her femoral neck and lumbar spine BMD Z-score were within the normal range for her age. There is a significant association between BMD and fracture risk in postmenopausal women. Consequently, DXA measurement of bone density is the primary clinical tool for assessing bone strength in this group.17,32 However, quantitative bone mass and qualitative indicators of bone quality determine bone’s strength and resistance to fracture.21,22 Fracture prediction incorporates both measurements of bone mass or density in combination with a clinically significant fracture history.31,32 This case suggests that BMD alone may not be adequate in assessing fracture risk in adolescents, since a normal BMD z-scores may not necessarily rule out the risk of a bone stress injury.
Persistent low energy availability can reduce muscle mass and glycogen stores and increase muscle fatigue.6 Repetitive loading from running without muscle strength to adequately absorb forces could increase bone microdamage without allowing time for repair.6 Low energy intake with inadequate bone-building micronutrients may have contributed to the fracture.14,36 Failing to augment her energy status and resume normal menstruation may have affected her fracture healing potential, since she had not fully recovered 12 months postinjury.
Oral contraceptive or bisphosphonate therapies were not used as treatments in this case. While oral contraceptives increase estrogen levels, research does not support their effectiveness in improving bone mass among adolescent athletes with low energy availability who do not improve their energy status.11,20,26 Bisphosphonates have been shown to prevent reductions in bone mass and improve fracture risk in postmenopausal women. However, because of potential teratogenic effects, even years after discontinuing use, bisphosphonates are not routinely used in female adolescents and women of childbearing age.1
Complete displaced femoral neck stress fractures are rare, though devastating.12,30 Femoral neck stress fractures are compression sided (medial), tension sided (lateral), or displaced (12%).10 Displaced femoral neck stress fractures lead to a 60% reduction in patient activity in sports and a 30% incidence of avascular necrosis.18 Factors that increase the risk of complications include time between fracture and surgery, reduction alignment, and type of fixation.18
This patient presented with a significant injury that could have been prevented. The long-term consequences of the injury in this case are not known but will likely carry significant implications. The underlying issues that contributed to her injury are not completely resolved. This case emphasizes the importance of knowing the risk factors for femoral neck stress fractures and the serious negative consequences of the female athlete triad with need for continued education of athletes, coaches, health care providers, and the general community.
References
- 1. Bachrach LK, Ward LM. Clinical review 1: bisphosphonate use in childhood osteoporosis. J Clin Endocrinol Metab. 2009;94(2):400-409 [DOI] [PubMed] [Google Scholar]
- 2. Barrack MT, Rauh MJ, Nichols JF. Cross-sectional evidence of suppressed bone mineral accrual among female adolescent runners. J Bone Miner Res. 2010;25(8):1850-1857 [DOI] [PubMed] [Google Scholar]
- 3. Barrack MT, Rauh MJ, Nichols JF. Prevalence of and traits associated with low BMD among female adolescent runners. Med Sci Sports Exerc. 2008;40(12):2015-2021 [DOI] [PubMed] [Google Scholar]
- 4. Barrack MT, Van Loan MD, Rauh MJ, Nichols JF. Physiologic and behavioral indicators of energy deficiency in female adolescent runners with elevated bone turnover. Am J Clin Nutr. 2010;92(3):652-659 [DOI] [PubMed] [Google Scholar]
- 5. Beals KA, Hill AK. The prevalence of disordered eating, menstrual dysfunction, and low bone mineral density among US collegiate athletes. Int J Sport Nutr Exerc Metab. 2006;16(1):1-23 [DOI] [PubMed] [Google Scholar]
- 6. Bennell K, Matheson G, Meeuwisse W, Brukner P. Risk factors for stress fractures. Sports Med. 1999;28(2):91-122 [DOI] [PubMed] [Google Scholar]
- 7. Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes: a twelve-month prospective study. Am J Sports Med. 1996;24(6):810-818 [DOI] [PubMed] [Google Scholar]
- 8. Chan JL, Mantzoros CS. Role of leptin in energy-deprivation states: normal human physiology and clinical implications for hypothalamic amenorrhoea and anorexia nervosa. Lancet. 2005;366(9479):74-85 [DOI] [PubMed] [Google Scholar]
- 9. De Souza MJ, West SL, Jamal SA, Hawker GA, Gundberg CM, Williams NI. The presence of both an energy deficiency and estrogen deficiency exacerbate alterations of bone metabolism in exercising women. Bone. 2008;43(1):140-148 [DOI] [PubMed] [Google Scholar]
- 10. Fullerton LR., Jr. Femoral neck stress fractures. Sports Med. 1990;9(3):192-197 [DOI] [PubMed] [Google Scholar]
- 11. Golden NH, Lanzkowsky L, Schebendach J, Palestro CJ, Jacobson MS, Shenker IR. The effect of estrogen-progestin treatment on bone mineral density in anorexia nervosa. J Pediatr Adolesc Gynecol. 2002;15(3):135-143 [DOI] [PubMed] [Google Scholar]
- 12. Haddad FS, Bann S, Hill RA, Jones DH. Displaced stress fracture of the femoral neck in an active amenorrhoeic adolescent. Br J Sports Med. 1997;31(1):70-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Heaney RP. Calcium, dairy products and osteoporosis. J Am Coll Nutr. 2000;19(2)(suppl):83S-99S [DOI] [PubMed] [Google Scholar]
- 14. Heaney RP, Abrams S, Dawson-Hughes B, et al. Peak bone mass. Osteoporos Int. 2000;11(12):985-1009 [DOI] [PubMed] [Google Scholar]
- 15. Hilton LK, Loucks AB. Low energy availability, not exercise stress, suppresses the diurnal rhythm of leptin in healthy young women. Am J Physiol Endocrinol Metab. 2000;278(1):E43-E49 [DOI] [PubMed] [Google Scholar]
- 16. Ihle R, Loucks AB. Dose-response relationships between energy availability and bone turnover in young exercising women. J Bone Miner Res. 2004;19(8):1231-1240 [DOI] [PubMed] [Google Scholar]
- 17. Jackson RD, Donepudi S, Mysiw WJ. Epidemiology of fracture risk in the Women’s Health Initiative. Curr Osteoporos Rep. 2008;6(4):155-161 [DOI] [PubMed] [Google Scholar]
- 18. Johansson C, Ekenman I, Tornkvist H, Eriksson E. Stress fractures of the femoral neck in athletes: the consequence of a delay in diagnosis. Am J Sports Med. 1990;18(5):524-528 [DOI] [PubMed] [Google Scholar]
- 19. Kelsey JL, Bachrach LK, Procter-Gray E, et al. Risk factors for stress fracture among young female cross-country runners. Med Sci Sports Exerc. 2007;39(9):1457-1463 [DOI] [PubMed] [Google Scholar]
- 20. Klibanski A, Biller BM, Schoenfeld DA, Herzog DB, Saxe VC. The effects of estrogen administration on trabecular bone loss in young women with anorexia nervosa. J Clin Endocrinol Metab. 1995; 80(3):898-904 [DOI] [PubMed] [Google Scholar]
- 21. Leslie WD, Pahlavan PS, Tsang JF, Lix LM. Prediction of hip and other osteoporotic fractures from hip geometry in a large clinical cohort. Osteoporos Int. 2009;20(10):1767-1774 [DOI] [PubMed] [Google Scholar]
- 22. Licata A. Bone density vs bone quality: what’s a clinician to do? Cleve Clin J Med. 2009;76(6):331-336 [DOI] [PubMed] [Google Scholar]
- 23. Loucks AB, Thuma JR. Luteinizing hormone pulsatility is disrupted at a threshold of energy avialability in regularly menstruating women. J Clin Endocrinol Metab. 2003(88):297-311 [DOI] [PubMed] [Google Scholar]
- 24. Loucks AB, Verdun M, Heath EM. Low energy availability, not stress of exercise, alters LH pulsatility in exercising women. J Appl Physiol. 1998;84(1):37-46 [DOI] [PubMed] [Google Scholar]
- 25. Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes: a study of 320 cases. Am J Sports Med. 1987;15(1):46-58 [DOI] [PubMed] [Google Scholar]
- 26. Munoz MT, Morande G, Garcia-Centenera JA, Hervas F, Pozo J, Argente J. The effects of estrogen administration on bone mineral density in adolescents with anorexia nervosa. Eur J Endocrinol. 2002;146(1):45-50 [DOI] [PubMed] [Google Scholar]
- 27. Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Ann Intern Med. 1990;113(10):754-759 [DOI] [PubMed] [Google Scholar]
- 28. Nattiv A. Stress fractures and bone health in track and field athletes. J Sci Med Sport. 2000;3(3):268-279 [DOI] [PubMed] [Google Scholar]
- 29. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine position stand: the female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867-1882 [DOI] [PubMed] [Google Scholar]
- 30. Okamoto S, Arai Y, Hara K, Tsuzihara T, Kubo T. A displaced stress fracture of the femoral neck in an adolescent female distance runner with female athlete triad: a case report. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rauch F, Plotkin H, DiMeglio L, et al. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2007 Pediatric Official Positions. J Clin Densitom. 2008;11(1):22-28 [DOI] [PubMed] [Google Scholar]
- 32. Simonelli C, Adler RA, Blake GM, et al. Dual-energy x-ray absorptiometry technical issues: the 2007 ISCD official positions. J Clin Densitom. 2008;11(1):109-122 [DOI] [PubMed] [Google Scholar]
- 33. Sullivan D, Warren RF, Pavlov H, Kelman G. Stress fractures in 51 runners. Clin Orthop Relat Res. 1984;187:188-192 [PubMed] [Google Scholar]
- 34. Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. 2004;14(1):25-32 [DOI] [PubMed] [Google Scholar]
- 35. Taylor JG, Bushinsky DA. Calcium and phosphorus homeostasis. Blood Purif. 2009;27(4):387-394 [DOI] [PubMed] [Google Scholar]
- 36. Weaver CM. Adolescence: the period of dramatic bone growth. Endocrine. 2002;17(1):43-48 [DOI] [PubMed] [Google Scholar]


