Abstract
Context:
Elbow tendinopathy is a common cause of pain and disability among patients presenting to orthopaedic surgeons, primary care physicians, physical therapists, and athletic trainers. Prompt and accurate diagnosis of these conditions facilitates a directed treatment regimen. A thorough understanding of the natural history of these injuries and treatment outcomes will enable the appropriate management of patients and their expectations.
Evidence Acquisitions:
The PubMed database was searched in December 2011 for English-language articles pertaining to elbow tendinopathy.
Results:
Epidemiologic data as well as multiple subjective and objective outcome measures were investigated to elucidate the incidence of medial epicondylitis, lateral epicondylitis, distal biceps and triceps ruptures, and the efficacy of various treatments.
Conclusions:
Medial and lateral epicondylitis are overuse injuries that respond well to nonoperative management. Their etiology is degenerative and related to repetitive overuse and underlying tendinopathy. Nonsteroidal anti-inflammatory drugs and localized corticosteroid injections yield moderate symptomatic relief in short term but do not demonstrate benefit on long-term follow-up. Platelet-rich plasma injections may be advantageous in cases of chronic lateral epicondylitis. If 6 to 12 months of nonoperative treatment fails, then surgical intervention can be undertaken. Distal biceps and triceps tendon ruptures, in contrast, have an acute traumatic etiology that may be superimposed on underlying tendinopathy. Prompt diagnosis and treatment improve outcomes. While partial ruptures confirmed with magnetic resonance imaging can be treated nonoperatively with immobilization, complete ruptures should be addressed with primary repair within 3 to 4 weeks of injury.
Keywords: tendinopathy, lateral epicondylitis, medial epicondylitis, distal biceps rupture, distal triceps rupture
It is important for orthopaedic surgeons, primary care physicians, physical therapists, and athletic trainers to be well versed in the examination, differential diagnosis, evaluation, and treatment options for patients presenting with elbow pain. Tendinopathy accounts for the majority of these visits.91 Injuries may be acute and traumatic, such as a distal biceps or triceps ruptures, or chronic and related to overuse, such as lateral epicondylitis. Regardless of the etiology, elbow tendinopathy represents an important set of pathologies that account for lost recreation time, decreased quality of life, and work-related disability claims. As an example, medial and lateral epicondylitis was responsible for 11.7% of work-related injury claims in Washington State from 1987 to 1995, resulting in an average direct workers’ compensation cost of $6,593 per case.78
Elbow tendinopathy has widespread social, financial, and clinical implications. Walker-Bone et al91 assessed the effect of medial and lateral epicondylitis on workplace absences in a cross-sectional sample of 9696 working-aged adults. Among this cohort, diagnoses of medial and lateral epicondylitis occurred in 0.6% and 0.7% of patients, respectively. Five percent of patients reported taking a sick day due to their elbow pain within the preceding year.
Conservative treatment is effective in the majority of patients with epicondylitis; however, the course leading to recovery can be prolonged (6-12 months) resulting in significant frustration for patients and their treating physicians alike. It is important to set proper expectations with patients embarking on initial treatment. This approach is reliant on a thorough understanding of the etiology, mechanism, treatment options, and expected outcomes.
This review article focuses on 4 types of elbow pathology characterized by underlying tendinopathy—lateral epicondylitis, medial epicondylitis, distal biceps ruptures, and distal triceps ruptures. A PubMed database search was performed in December 2011 for English-language articles pertaining to these conditions.
Lateral Epicondylitis
Epidemiology
Lateral epicondylitis, also known as tennis elbow, is significantly more common than medial epicondylitis92 and has an annual prevalence of 1% to 2% in the general public.76 As its eponym implies, lateral epicondylitis has a high association with tennis, particularly one-handed backhand strokes. Nearly 40% to 50% of recreational tennis players will suffer this condition during their lifetime.45,56
This condition, however, is not unique to tennis players. In fact, any sport or occupation that demands repetitive wrist extension can result in this injury. Several authors have reported occupations with high incidence rates, including politicians, municipal utility employees,72 and nursery school cooks.64 Kurppa et al52 evaluated the incidence of epicondylitis in workers at a meat-processing factory and reported a rate of 1% for those in nonlabor positions, while female sausage makers, meat packers, and male meat cutters had rates of 11.3%, 7.0%, and 6.4%, respectively.
In addition to repetitive activities, obesity and smoking52,72,76 have been implicated as independent risk factors. Current smokers have an adjusted odds ration of 3.4.76 Patients between the ages of 35 and 54 years are most commonly affected, and there is an equal gender distribution.41,76
Pathophysiology
The extensor carpi radialis brevis (ECRB) is the most commonly affected tendon, although other tendons in the extensor bundle, such as the extensor digitorum communis, may be involved. Injury results from the repetitive microtrauma generated through overuse contraction of the wrist extensors.
The terms lateral epicondylitis and tendinitis are misleading because they suggest an inflammatory process. Rather, the pathophysiology of this process is degenerative in nature.50 The term angioblastic tendinosis has been used to describe the offending process. Injury occurs as a result of microtrauma.50 The body responds in an effort to repair the damaged tissue by upregulation of local angiogenesis in conjunction with fibroblast proliferation. Kraushaar and Nirschl50 evaluated surgical specimens collected from 9 patients who failed conservative management for lateral epicondylitis, using histology and electron microscopy, and they compared these with cadaveric specimens. They found a paucity of evidence to suggest inflammatory response—general absence of polymorphonuclear leukocytes, lymphocytes, and macrophages. They noted areas of poorly organized collagen fibers and matrix with microvasculature suggestive of a regenerative process. It should be noted that it is rare to obtain biopsy specimens in the early stages of epicondylitis; thus, it remains unclear if an initial inflammatory response to localized trauma occurs.
Four stages of lateral epicondylitis have been described, beginning with early inflammatory reaction, followed by angiofibroblastic degeneration, structural failure, and ultimately, fibrosis or calcification.61 Persistent microtrauma resulting in failed attempts at healing produces tendinosis. Surgical repair focuses on debridement of tendinosis and direct repair of the ECRB tendon.
Clinical Evaluation
A thorough but focused history and physical examination are critical to timely and accurate diagnosis. Historical factors should be solicited, such as occupation, hand dominance, recreational activities, duration of symptoms, prior episodes of epicondylitis or treatment modalities, and tobacco use. Patients frequently describe pain and/or a burning sensation about the lateral humeral epicondyle that is exacerbated by activities that require resisted wrist extension, such as pouring a gallon of milk. Grip weakness is another complaint, with patients reporting pain and difficulty while shaking hands.
Tenderness to palpation at the lateral epicondyle and along the common extensor tendon is a hallmark of lateral epicondylitis. Swelling and ecchymosis are not typically present, and grip strength is usually reduced. Dorf22 compared grip strength with the elbow in varying positions of flexion in a cohort of 81 patients diagnosed with lateral epicondylitis. With the elbow in extension, the affected side had 50% grip strength when compared to the unaffected side. The chair test32 has been described as a useful provocative test. The patient is asked to lift a chair with the shoulder adducted, elbows extended, and forearms pronated. Other tests, such as lifting a coffee cup or a gallon of milk, can also be provocative. Any test that generates a patient’s symptoms through resisted wrist extension can be an effective diagnostic tool. Reproduction of symptoms indicates a positive test result. Resisted extension of the middle finger can often re-create symptoms.
If the diagnosis of lateral epicondylitis is clear on physical examination and history, then diagnostic imaging is not indicated. If uncertainty exists, imaging and diagnostic tests can be useful for exploring the differential diagnosis, including radiocapitellar chondromalacia, posterolateral elbow instability, plica, loose bodies, malignancy, cervical radiculopathy (C6 or C7), or compression of the posterior interosseous nerve at the arcade of Frosche (supinator syndrome).83 Posterior interosseus nerve compression can be accurately evaluated with a targeted diagnostic injection of local anesthetic.
Magnetic resonance imaging (MRI) is helpful in evaluating the soft tissues of the elbow in patients who have failed appropriate conservative treatment and aids in both diagnosis and surgical planning. Review of MRI findings from 24 patients with epicondylitis reported increased intratendon signal on both T1 and T2 pulse sequences58 with occasional bone marrow edema pattern in the epicondyle. Other studies have shown thickening, edema, and tears of the common extensor tendon.56,74 MRI of patients with lateral epicondylitis and a control population demonstrated intratendinous signal changes in 92% of patients and 16% of controls.58 MRI is not recommended as a screening tool, but it can play a significant role in surgical planning. In chronic refractory lateral epicondylitis, a direct correlation of MRI results and intraoperative and histologic findings has been reported.71
Figure 1.

Coronal proton density (A) and gradient recalled acquisition (B) MR sequences demonstrate degeneration of the origin of the extensor carpi radialis brevis tendon (arrow) with a high-grade partial intrasubstance tear (arrowhead). Images courtesy of Hollis G. Potter, MD.
Figure 2.

MRI of the left elbow demonstrates extracapsular soft tissue edema (arrow) on a coronal inversion recovery sequence (A). A high-grade proximal tear is noted in the extensor carpi radialis brevis tendon (arrowhead) on the coronal proton density sequence (B). Images courtesy of Hollis G. Potter, MD.
Treatment
Nonoperative management of lateral epicondylitis will result in successful resolution of symptoms in 90% of patients.18,42 Conservative care may include activity modification, nonsteroidal anti-inflammatory medications, physiotherapy, corticosteroid injections, shockwave therapy, and benign neglect. Tendinitis may occur in the early stage of epicondylitis and may be responsive to anti-inflammatory measures. Later stages represent tendinosis and are less responsive to the same measures. Treatment effect on the condition’s natural history, however, remains inconclusive., In chronic lateral epicondylitis, platelet-rich plasma (PRP) has been shown to effectively reduce pain and symptoms35,43,60,66,85 in several short-term studies. Failure to improve with conservative treatment and continued activity limitations may lead to consideration for surgical treatment.
Figure 3.

Coronal gradient recalled acquisition (A) and sagittal proton density (B) MR sequences, performed to “rule out lateral epicondylitis”, demonstrate only mild tendinosis (A - arrow) of the extensor carpi radialis brevis without discrete tear. Full-thickness cartilage loss, however, with bone-on-bone apposition at the radiocapitellar joint (B – arrowhead) was identified as the source of the patient’s symptoms. Images courtesy of Hollis G. Potter, MD.
Activity modification is a necessary component of any treatment protocol, especially given the overuse etiology of this condition. Patients should be counseled to refrain from inciting activities and motions. Rest, ice, compression, and elevation (or RICE) of the affected arm can be helpful during this initial phase. Modifications can be made in technique, such as the use of a 2-handed backhand to reduce the stress encountered by the extensors.34
Bracing (forearm straps and cock-up wrist splints) can redirect the extensor force vector and may provide symptom relief,8 by reduction in extensor muscle activity.38 Cock-up wrist splints reduce extensor contraction by limiting wrist flexion and extension allowing the extensors to rest. A prospective randomized study33 comparing the effects of counterforce bracing and cock-up wrist splints at 6 weeks reported superior subjective pain improvement in the splinted group.
While the underlying pathology of lateral epicondylitis at the end stage is not inflammatory, the use of nonsteroidal anti-inflammatory drugs (NSAID) may be a useful adjunct to activity modification.7 There is a lack of data to support their oral use.42,54 In contrast, Brunham et al7 noted short-term relief associated with a topical NSAID in their randomized double-blind crossover study.
Physical therapy is another important component to conservative treatment of lateral epicondylitis.9 Traditionally, physiotherapy was aimed at stretching and strengthening the extensors of the forearm.62 More current therapeutic modalities include eccentric muscle training.19,59 It should be noted, however, that while eccentric training “did not cause subjects to worsen,”59 there remains limited evidence to support this modality in the elbow over stretching alone.
Corticosteroid injections result in improved short-term patient outcomes, with equivocal results at 12 months. Hay and colleagues42 randomized patients with lateral epicondylitis to 3 treatment arms (placebo, oral NSAID, and corticosteroid injections). They found that the best short-term (4-week) symptomatic improvements occurred in patients who received the corticosteroid injection, while some improvement occurred in those who received the oral NSAID when compared with placebo. At 1-year follow-up, patient outcomes were similar among 3 groups.
The efficacy of extracorporeal shock wave (ECSW) therapy remains a source of debate. Three randomized double-blinded studies have reported contrasting results. Pettrone and McCall67 reported statistically significant pain improvement at 12 weeks in those treated with ECSW when compared with placebo and concluded that ECSW was a safe and effective treatment for tennis elbow. Two additional studies describe ECSW and placebo as similarly ineffective in treating lateral epicondylitis.13,40
More recently, injection of PRP has been investigated as a possible treatment. Investigators conducted a trial on patients with chronic lateral epicondylitis, in which 100 patients were randomized to either PRP or corticosteroid injection. Improved pain relief and rates of success in the PRP group were demonstrated at 1 year66 and 2 years35 posttreatment. Other studies with lower levels of evidence43,60 and short term follow-up85 have reported similar positive effects of PRP.
Surgical intervention is reserved for those patients who remain symptomatic for greater than 6 months, despite myriad conservative measures. Clarke et al15 used ultrasound to evaluate the size of the intrasubstance tear and correlated it with patient outcome. Patients with large tears were more likely to have a negative response to conservative treatment as measured by scores on the Patient-Rated Tennis Elbow Evaluation at 6 months postdiagnosis, suggesting a lower threshold for surgery in those with large tears. Despite this, the gold standard remains 6 to 12 months of conservative care prior to surgical intervention.
In cases where nonoperative measures fail, surgical options include percutaneous, open, and arthroscopic techniques. Percutaneous treatment involves release of the extensor tendon origin at the lateral epicondyle. This technique has been advocated as safe, reliable, and cost-effective.4,39,48,94 Othman reported similar outcomes for arthroscopic and percutaneous techniques at 12 months’ follow-up.65
Arthroscopic techniques to address recalcitrant lateral epicondylitis involve release of the common extensor tendon. Advocates of this approach cite quick recovery time, including return to work3 and the ability to evaluate and treat concomitant intra-articular pathology.55 Baker and Baker3 reported an 87% patient satisfaction rate in 42 patients treated arthroscopically at long-term follow-up (average, 10.1 years). Despite the generally positive results, the learning curve, as well as the risk of inadvertent neurovascular injury51 or release of the lateral ulnar collateral ligament,79 is not insignificant.
In our experience, open techniques may offer the most reliable, operator-independent, and safe treatment option for refractory lateral epicondylitis. Open treatment involves a small lateral incision with dissection and identification of focus of tendinopathy. The diseased tissue is removed, and decortication of the insertion site on the lateral epicondyle is performed. A suture anchor repair may be performed of ECRB tendon to bone. Several authors have reported good to excellent results with this approach.17,24 Coleman et al17 described a single surgeon’s 15-year experience treating refractory cases of lateral epicondylitis. In 158 consecutive patients treated with open technique, 94.6% of patients had good to excellent results at an average of 9.8 years’ follow-up. Dunn et al24 reported their long-term results in 139 cases of tennis elbow with 84% rated as good or excellent, 92% with normal elbow range of motion, and an overall patient satisfaction of 8.9 of 10. Thornton et al86 explored the utility of suture anchor repair of the ECRB tendon to the lateral epicondyle following open debridement of tendinosis. They found normal grip and pinch strength, full range of motion, and near resolution of preoperative pain.
Postoperative rehabilitation follows a sequential pattern of protection of the repair, stretching, then strengthening. Patients are initially placed in a sling for comfort. A cock-up wrist splint is used to protect the repair and to permit more active use of the elbow. Range of motion of the elbow is instituted postoperative day 1 with a goal of full elbow extension at 10 to 14 days postoperatively. The first 6 weeks following surgery are focused on recovery of range of motion of the wrist and elbow, which is performed as a home-based program. Formal physical therapy is instituted at 6 weeks to restore terminal range of motion and restore full strength.
Medial Epicondylitis
Epidemiology
Medial epicondylitis is commonly referred to as “golfer’s elbow” but can be found in athletes and in workers in occupations that demand repetitive wrist flexion activities. Medial epicondylitis is less common than lateral epicondylitis, with a reported prevalence less than 1% in the general population76,92 but as high as 6% in some professions.21 The demographics of at-risk patients are very similar to those at risk of lateral epicondylitis and include ages 30 to 50 years, laborers, those performing repetitive tasks demanding wrist flexion, smokers, and patients with obesity.
In throwing athletes, particularly baseball players, the elbow’s medial structures endure the most stress and account for up to 97% of all elbow injuries.12 Medial epicondylitis and apophysitis (in the skeletally immature thrower) may result from repetitive stress to the flexor pronator mass during the valgus-loading acceleration phase of throwing.36
Pathophysiology
The pathogenesis of medial epicondylitis parallels that of lateral epicondylitis, beginning with repetitive microtrauma to the wrist flexors originating at their insertion on the medial epicondyle. The muscles most commonly involved include the pronator teres and flexor carpi radialis but can include any of the other flexors.63 Histologic studies demonstrate patterns of angiofibroblastic degeneration similar to those seen in lateral epicondylitis.63
Clinical Evaluation
Patients with medial epicondylitis have many of the same risk factors as those with lateral epicondylitis. Van Rijn and colleagues88 performed a systematic review of the literature and reported that handling objects greater than 5 kg for 2 hours per day, objects greater than 10 kg more than 10 times per day, and repetitive movements and vibrating tools for greater than 2 hours per day were associated with medial epicondylitis.
A history of medial elbow pain in the setting of repetitive wrist flexion and forearm pronation activities is suspicious for the diagnosis, though a subset of patients will describe a more diffuse nature of their symptoms.68 This may, in part, be related to a relatively high rate of concomitant ulnar neuritis.53
Examination should focus on tenderness over the origin of the flexor pronator mass. Resisted pronation and/or wrist flexion will reproduce symptoms in most affected patients. Grip strength is decreased in patients with medial epicondylitis compared with control subjects, although the magnitude of impairment is less than that seen in patients with lateral epicondylitis.69 The examiner should assess the competency of the medial collateral ligament with a valgus stress test, which should be painless in the absence of medial collateral ligament insufficiency. A careful neurologic examination should be performed to look for evidence of ulnar neuritis, including Tinel sign (radiating pain with percussion at the cubital tunnel), cubital tunnel compression testing, 2-point discrimination testing of the fifth digit, and assessment of hypothenar atrophy in advanced cases.
Imaging studies, such as plain radiographs, may show calcifications or traction osteophytes at the flexor-pronator origin. Kijowski et al49 assessed MRI findings from 13 patients with clinically diagnosed medial epicondylitis and reported thickening and increased signal intensity within the common flexor tendon and surrounding soft tissue edema seen in both T1- and T2-weighted images compared with age-matched controls. Clinical evaluation remains adequate for diagnosis in most cases. MRI may be more useful when used to rule out other pathologies, such as osteochondritis dissecans lesions, medial collateral ligament insufficiency, or loose bodies.
Treatment
Treatment for medial epicondylitis parallels those described for lateral epicondylitis. Nonoperative management is the mainstay of treatment.14 Conservative measures include rest, activity modification, nonsteroidal anti-inflammatory medications, physiotherapy, corticosteroid injections. Corticosteroid injections improved symptoms at 6 weeks but showed no difference when compared with controls at 3 and 12 months.81 When a patient is injected for medial epicondylitis, particular caution must be taken to protect the ulnar nerve because of its proximity.82 PRP injections may hold some benefit for patients with chronic golfer’s elbow, but well-designed studies are lacking.
Surgery is reserved for those who fail 6 to 12 months of conservative management. Unlike lateral epicondylitis, an arthroscopic technique is not used. The open procedure involves debridement of tendinosis found deep to and in the interval between the pronator teres and flexor carpi radialis. The bony surface of the medial epicondyle is decorticated to enhance local vascularity. As noted previously, there is a high rate of concomitant ulnar neuritis. If present, the cubital tunnel should be decompressed and the ulnar nerve transposed.
Cases in which ulnar neuritis accompanies medial epicondylitis have a less favorable outcome when treated surgically than those with isolated medial epicondylitis. Kurvers et al53 noted ulnar neuritis in 24 of 38 elbows. Subjective outcome scores were lower if ulnar neuritis was present preoperatively (P < 0.05). In their series, 3 of 24 patients with preexisting ulnar neuritis were symptom free at final follow-up compared with 11 of 16 with isolated medial epicondylitis. This finding has been corroborated in other published studies.12,29,36,63
Patients with refractory symptoms treated surgically will likely see improvement in pain but may not return to their sporting activities. Ollivierre et al63 reported on 50 cases of surgical treatment for medial epicondylitis. At an average of 37 months of follow-up, objective strength testing showed improvement with relief of preoperative pain. Of note, however, 20% of patients did not return to their previous recreational sporting activities.
Distal Biceps Rupture
Epidemiology
True distal biceps tendinitis is rare. More common are partial ruptures. Bourne and Morrey6 originally described this entity in their case series of 3 patients with varying duration (1 day to 1 year) of symptoms. All the patients were noted to have partial tendon rupture with surrounding granulation, and scar tissue was noted at the time of surgery.
Complete rupture of the distal biceps tendon from its insertion at the radial tuberosity is most common. Safran and Graham73 reported an overall incidence of 1.2 distal biceps ruptures per 100 000 patients per year. These injuries typically occur in the dominant arm46,73 of men between the ages of 40 and 50 years.37
Risk factors include smoking, anabolic steroid use, and previous distal biceps rupture. Smokers have a 7.5-times greater risk than nonsmokers.73 While bilateral injuries make up a rare subset of patients, Green and colleagues37 found of an 8% cumulative incidence of bilateral ruptures among patients in their series of 321 consecutive patients. When compared with the 0.0012% incidence in the general population, it was deduced that prior distal biceps tendon rupture is an independent risk factor for subsequent contralateral injury.
Figure 4.

MRI was performed including sagittal (A, C) and axial (B, D) proton density sequences of the left elbow. A high-grade insertional partial tear of the biceps tendon at the radial tuberosity was identified (A, B – arrows). A large septate ganglion (C, D – arrowheads) was noted communicating with the bicipitoradial bursa, compressing the posterior interosseous nerve (D – star) at the supinator muscle. Images courtesy of Hollis G. Potter, MD.
Though far less common, some authors26,46 have reported partial and complete ruptures in women. Jockel et al46 described 13 female patients with partial and complete distal biceps tendons and found that the majority of such injuries occur at a more advanced age (67 years), are partial tears, and occur secondary to atraumatic mechanisms.
Pathophysiology
An understanding of the local neurovascular structures and the function of the biceps tendon are critical. The biceps muscle acts to flex the elbow and supinate the forearm. It has 2 origins (heads): the long head, which inserts on the supraglenoid tubercle, and the short head, which meshes with the coracobrachialis and the pectoralis minor tendon to form the conjoint tendon inserting on the coracoid process. The biceps muscle has a common tendinous insertion at the radial tuberosity. The lacertus fibrosus (bicipital aponeurosis) emanates from the biceps muscle belly at the level of the musculotendinous junction and crosses distally and medially to insert along the subcutaneous border of the ulna. Several neurovascular structures, including the lateral antebrachial cutaneous nerve, median nerve, brachial artery and vein, and radial recurrent artery, pass in close proximity to the biceps insertion. The spatial arrangement of these structures is critical when planning and carrying out surgical repair.
Rupture of the distal biceps tendon is classically an acute injury occurring during placement of a large eccentric load. This load is applied with the elbow in 90° of flexion, with resulting avulsion of the biceps tendon from the radial tuberosity. Though some authors have reported intratendinous and musculotendinous sites of injury, this represents the exception rather than the rule.75 Competency of the lacertus fibrosus is variable following avulsion injury. If it remains intact, it may act as a checkrein to proximal migration of the tendon and muscle belly.
Clinical Evaluation
History should be obtained for the aforementioned risk factors—prior distal biceps tendon rupture, hand dominance, tobacco and anabolic steroid use. The mechanism of injury must be clearly elucidated. Patients often describe a sharp, sudden, and painful “pop.” The sharp pain typically dissipates within hours to days and is followed by a dull ache. Patients may describe outright weakness of elbow flexion and supination or rather describe newfound difficulties with activities that require these actions, such as turning a doorknob or lifting objects.
Physical examination includes inspection and palpation. Ecchymosis is present acutely. Patients with complete distal biceps tendon ruptures usually have a visible deformity resulting from biceps muscle retraction proximally. Palpation of the antecubital fossa often reveals a void where the biceps tendon is inserted. Range of motion and strength testing is performed, particularly with respect to flexion and supination.
Plain radiographs are usually unrevealing but can be useful if the mechanism or examination suggests concomitant injuries. MRI may also be helpful if there is question of complete versus incomplete injury. Festa and colleagues25 retrospectively reviewed preoperative MRI studies on 22 cases of partial distal biceps tendon ruptures and 24 cases of complete tendon ruptures. They compared blinded radiologist interpretations with intraoperative findings. Complete injuries had a sensitivity of 100% and specificity of 82.8%. Partial injuries had a sensitivity 59.1% and specificity of 100%.
Treatment
In low-functioning or medically complicated patients, nonoperative measures may be pursued; however, ultimate strength and function will be compromised. Freeman et al27 reported overall satisfactory outcomes in 18 patients who underwent nonoperative treatment for distal biceps ruptures at 38 months of follow-up. A decrease in elbow flexion (88%) and supination (74%) strength was found when compared to the contralateral side. The decrease in supination strength was significant when compared with historical controls, but the difference in elbow flexion strength was not.
Surgical repair of distal biceps ruptures results in improved strength and function. Frazier et al26 reported a case series of 17 patients with unilateral partial biceps tendon ruptures. The average isometric and dynamic elbow flexion was comparable to the contralateral side. There was minimal decrease of isometric (6%) and dynamic (10%) supination with 1 partial rerupture at 4 years. Patients with acute distal biceps tendon ruptures should undergo surgical repair within 1 month of injury. Delay increases the technical difficulty of the repair secondary to scar formation and tendon retraction. Partial biceps tendon ruptures can be initially treated with activity modification and physical therapy for 3 to 6 months. If conservative measures fail, surgical repair should be considered.
Surgical options include both single-incision and 2-incision techniques. Several methods of fixation have been used to anchor the distal biceps tendon to the radial tuberosity, including transosseous bone tunnels, suture anchors, interference screws, and the EndoButton. Chavan et al11 compared surgical techniques as well as methods of fixation in their systematic review of the literature. They reported that biomechanical data suggest superiority of EndoButton fixation and better results with use of a single-incision technique. The 2-incision technique was associated with significant loss of forearm motion and high rates of patient dissatisfaction (31%).
Surgery is not without risk. Bisson and coinvestigators5 described a 27% complication rate among the 45 patients who underwent surgical distal biceps repair. The 2 most common complications included nerve dysfunction (15%) and radioulnar synostosis (7%). Other reported complications were heterotopic ossification, rerupture, and reflex sympathetic dystrophy.
At the conclusion of surgery, patients are placed in a hinged elbow brace, which is locked at 90° of elbow flexion. Passive elbow flexion is permitted on postoperative day 1 from 90 to increased flexion. No passive or active extension is permitted. Forearm passive pronation and supination are instituted on postoperative day 1. At 10 days postoperatively, an extension stop is placed on the brace based on tension-free range of motion assessed following the surgical repair. Physical therapy is instituted to include active elbow extension and passive flexion with a goal of full range of motion by 6 weeks postoperatively. Passive pronation and supination of the forearm are encouraged to minimize scar formation and restore forearm rotation. At 6 weeks, the patient may begin graduated strengthening exercises with a trained physical therapist.
Distal Triceps Rupture
Epidemiology
Triceps tendinopathy and rupture constitute the least common type of elbow tendinopathy.1 Triceps tendinitis and partial and complete ruptures exist on a continuum with a male predominance. Triceps ruptures have been described in patients of all ages and can be associated with total elbow arthroplasty.10 These injuries also occur in younger active patients, with case reports describing the injury in professional weight lifters,2,44,80 softball players,77 skiers,77 soccer players,77 and professional football players.57
Figure 5.
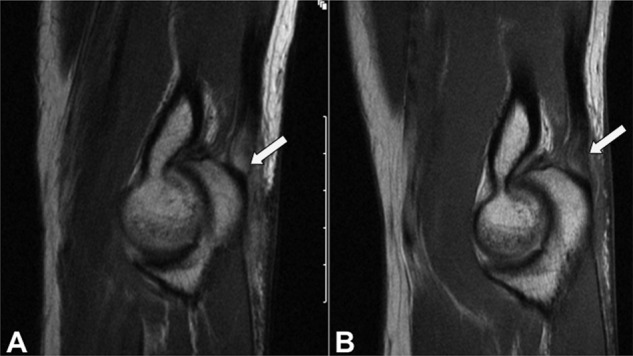
Sagittal proton density MRI sequence (A) demonstrates an acute partial tear of the triceps insertion (arrow) superimposed on preexisting tendinosis. One year later (B), a repeat MRI shows improved appearance of the triceps tendon but residual tendinosis (arrow). Images courtesy of Hollis G. Potter, MD.
Pathophysiology
Triceps tendinopathy most commonly occurs at the tendon-osseous junction at the olecranon77 but can occur within the tendon substance or at the musculotendinous junction. Systemic risk factors that weaken tendons have been reported, such as metabolic conditions47 and endocrine disorders such as diabetes mellitus90 and hypoparathyroidism.20 Local factors that may weaken or traumatize the, including corticosteroid injection,80 anabolic steroids,80 overtraining, and olecranon bursitis, have been implicated in tendon rupture.77 There are no case reports of triceps rupture in the setting of fluoroquinolone use.
The most common site of triceps injury is avulsion from the olecranon. The mechanism is the result of an acute injury, such as a fall onto an outstretched hand with resulting violent eccentric load absorbed by the triceps.
Clinical Evaluation
Triceps tendinosis is a chronic condition stemming from overuse and repetitive heavy lifting. Patients routinely describe pain and/or weakness with activities of elbow extension. Tenderness to palpation occurs at the triceps insertion on the olecranon. In the setting of chronic repetitive injury, plain radiographs may reveal a traction osteophyte on the olecranon.
As mentioned, triceps avulsions from the olecranon or intratendinous ruptures are the result of a traumatic injury. Physical examination may reveal swelling, tenderness, ecchymosis, and a palpable defect just proximal to the olecranon. Strength testing will show weakness of elbow extension, but it is important to note that the ability of a patient to extend his or her elbow does not exclude triceps rupture, because elbow extension can be preserved in cases of partial tears or though the lateral expansion of the triceps fascia. Viegas described a modification of the Thompson test (used to detect Achilles tendon ruptures) in which squeezing the triceps muscle belly does not produce expected elbow extension.89
Imaging is an essential component of evaluation. Plain radiographs must be obtained. Osseous flecks, referred to as the “flake sign,” are pathognomonic for triceps avulsion injuries.70 Evidence of other or concomitant osseous injury or malalignment may also be evident on plain radiographs. MRI16,31 or ultrasound23,84 can be helpful in differentiating between partial and complete injury.
Treatment
Patients with triceps tendinosis are initially managed nonoperatively with activity modification, nonsteroidal anti-inflammatory medications, and physical therapy for stretching and range of motion. Symptomatic resolution may take months. Operative management, consisting of olecranon osteophyte excision and triceps repair,30 is reserved for refractory cases that fail conservative management.28
Incomplete tears (< 50%) can be managed conservatively with splint immobilization for 4 weeks in 30° of flexion.93 Partial tears, even in high-performance athletes, can be treated with success. Mair et al57 reported successful healing of 6 of 10 partial triceps tears in professional football players with no lingering effects, such as pain or dysfunction after healing.
In cases of acute triceps avulsion, timely surgical repair is advocated.87 Cases of incomplete tears where conservative measures have failed should also be treated operatively. Surgical technique involves primary repair of the avulsed triceps tendon using a Krakow suture pattern to the olecranon via bone tunnels.87 In general, surgical repair yields good results and return to activities.2,80,87
Summary
Elbow tendinopathy is a common cause of pain and disability among patients presenting to orthopaedic and primary care physicians. Prompt and accurate diagnosis of these conditions facilitates directed therapeutic regimens. A thorough understanding of the natural history of these injuries, in addition to treatment-related outcomes, should enable the physician to appropriately manage expectations.
Medial and lateral epicondylitis are typically overuse injuries and respond well to conservative management. Their etiology is noninflammatory, with histology characterized by a degenerative process. NSAID therapy and localized corticosteroid injections have demonstrated moderate symptomatic relief in short-term but not long-term follow-up. PRP injections are advantageous in cases of chronic lateral epicondylitis. In general, 6 to 12 months of nonoperative treatment should be trialed prior to surgical intervention.
Distal biceps and triceps tendon ruptures occur most commonly secondary to an acute traumatic event but may be superimposed on underlying tendinopathy. Prompt diagnosis and treatment improve outcomes. Partial ruptures are confirmed with MRI and may initially be treated nonoperatively with immobilization. Complete ruptures are usually addressed with primary repair and have shown best results when performed within 3 to 4 weeks of injury.
References
- 1. Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruption of muscles and tendons: an analysis of 1014 cases. Surgery. 1959;45(3):406-414 [PubMed] [Google Scholar]
- 2. Bach BR, Warren RF, Wickiewicz TL. Triceps rupture: a case report and literature review. Am J Sports Med. 1987;15(3):285-289 [DOI] [PubMed] [Google Scholar]
- 3. Baker CL, Baker CL. Long-term follow-up of arthroscopic treatment of lateral epicondylitis. Am J Sports Med. 2008;36(2):254-260 [DOI] [PubMed] [Google Scholar]
- 4. Baumgard SH, Schwartz DR. Percutaneous release of the epicondylar muscles for humeral epicondylitis. Am J Sports Med. 1982;10(4):233-236 [DOI] [PubMed] [Google Scholar]
- 5. Bisson L, Moyer M, Lanighan K, Marzo J. Complications associated with repair of a distal biceps rupture using the modified two-incision technique. J Shoulder Elbow Surg. 2008;17(1):67S-71S [DOI] [PubMed] [Google Scholar]
- 6. Bourne MH, Morrey BF. Partial rupture of the distal biceps tendon. Clin Orthop Relat Res. 1991;271:143-148 [PubMed] [Google Scholar]
- 7. Burnham R, Gregg R, Healy P, Steadward R. The effectiveness of topical diclofenac for lateral epicondylitis. Clin J Sport Med. 1998;8(2):78-81 [DOI] [PubMed] [Google Scholar]
- 8. Burton AK. Grip strength and forearm straps in tennis elbow. Br J Sports Med. 1985;19(1):37-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19-29 [DOI] [PubMed] [Google Scholar]
- 10. Celli A, Arash A, Adams RA, Morrey BF. Triceps insufficiency following total elbow arthroplasty. J Bone Joint Surg Am. 2005;87(9):1957-1964 [DOI] [PubMed] [Google Scholar]
- 11. Chavan PR, Duquin TR, Bisson LJ. Repair of the ruptured distal biceps tendon: a systematic review. Am J Sports Med. 2008;36(8):1618-1624 [DOI] [PubMed] [Google Scholar]
- 12. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9(2):99-113 [DOI] [PubMed] [Google Scholar]
- 13. Chung B, Wiley JP. Effectiveness of extracorporeal shock wave therapy in the treatment of previously untreated lateral epicondylitis: a randomized controlled trial. Am J Sports Med. 2004;32(7):1660-1667 [DOI] [PubMed] [Google Scholar]
- 14. Ciccotti MG, Ramani MN. Medial epicondylitis. Tech Hand Up Extrem Surg. 2003;7(4):190-196 [DOI] [PubMed] [Google Scholar]
- 15. Clarke AW, Ahmad M, Curtis M, Connell DA. Lateral elbow tendinopathy: correlation of ultrasound findings with pain and functional disability. Am J Sports Med. 2010;38(6):1209-1214 [DOI] [PubMed] [Google Scholar]
- 16. Clifford PD, Posada A, Hancock CR. Isolated long-head triceps brachii tendon avulsion in a surfer detected at MR imaging. Skeletal Radiol. 2009;38(1):77-80 [DOI] [PubMed] [Google Scholar]
- 17. Coleman B, Quinlan JF, Matheson JA. Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elbow Surg. 2010;19(3):363-367 [DOI] [PubMed] [Google Scholar]
- 18. Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg Am. 1973;55(6):1177-1182 [PubMed] [Google Scholar]
- 19. Croisier JL, Foidart-Dessalle M, Tinant F, Crielaard JM, Forthomme B. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med. 2007;41(4):269-275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. de Waal Malefijt MC, Beeker TW. Avulsion of the triceps tendon in secondary hyperparathyroidism: a case report. Acta Orthop Scand. 1987;58(4):434-435 [DOI] [PubMed] [Google Scholar]
- 21. Descatha A, Leclerc A, Chastang JF, Roquelaure Y; Study Group on Repetitive Work. Medial epicondylitis in occupational settings: prevalence, incidence and associated risk factors. J Occup Environ Med. 2003;45(9):993-1001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dorf ER, Chhabra AB, Golish SR, McGinty JL, Pannunzio ME. Effect of elbow position on grip strength in the evaluation of lateral epicondylitis. J Hand Surg Am. 2007;32(6):882-886 [DOI] [PubMed] [Google Scholar]
- 23. Downey R, Jacobson JA, Fessell DP, Tran N, Morag Y, Kim SM. Sonography of partial-thickness tears of the distal triceps brachii tendon. J Ultrasound Med. 2011;30(10):1351-1356 [DOI] [PubMed] [Google Scholar]
- 24. Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261-266 [DOI] [PubMed] [Google Scholar]
- 25. Festa A, Mulieri PJ, Newman JS, Spitz DJ, Leslie BM. Effectiveness of magnetic resonance imaging in detecting partial and complete distal biceps tendon rupture. J Hand Surg Am. 2010;35(1):77-83 [DOI] [PubMed] [Google Scholar]
- 26. Frazier MS, Boardman MJ, Westland M, Imbriglia JE. Surgical treatment of partial distal biceps tendon ruptures. J Hand Surg Am. 2010;35(7):1111-1114 [DOI] [PubMed] [Google Scholar]
- 27. Freeman CR, McCormick KR, Mahoney D, Baratz M, Lubahn JD. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am. 2009;91(10):2329-2334 [DOI] [PubMed] [Google Scholar]
- 28. Gabel GT. Acute and chronic tendinopathies at the elbow. Curr Opin Rheumatol. 1999;11(2):138-143 [DOI] [PubMed] [Google Scholar]
- 29. Gabel GT, Morrey BF. Operative treatment of medical epicondylitis: influence of concomitant ulnar neuropathy at the elbow. J Bone Joint Surg Am. 1995;77(7):1065-1069 [DOI] [PubMed] [Google Scholar]
- 30. Gabel GT, Zwahlen B, Morrey BF. Surgical management of the extensor mechanism of the elbow. Instr Course Lect. 1998;47:151-156 [PubMed] [Google Scholar]
- 31. Gaines ST, Durbin RA, Marsalka DS. The use of magnetic resonance imaging in the diagnosis of triceps tendon ruptures. Contemp Orthop. 1990;20(6):607-611 [PubMed] [Google Scholar]
- 32. Gardner RC. Tennis elbow: diagnosis, pathology and treatment. Nine severe cases treated by a new reconstructive operation. Clin Orthop Relat Res. 1970;72:248-253 [PubMed] [Google Scholar]
- 33. Garg R, Adamson GJ, Dawson PA, Shankwiler JA, Pink MM. A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(4):508-512 [DOI] [PubMed] [Google Scholar]
- 34. Giangarra CE, Conroy B, Jobe FW, Pink M, Perry J. Electromyographic and cinematographic analysis of elbow function in tennis players using single- and double-handed backhand strokes. Am J Sports Med. 1993;21(3):394-399 [DOI] [PubMed] [Google Scholar]
- 35. Gosens T, Peerbooms JC, van Laar W, den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011;39(6):1200-1208 [DOI] [PubMed] [Google Scholar]
- 36. Grana W. Medial epicondylitis and cubital tunnel syndrome in the throwing athlete. Clin Sports Med. 2001;20(3):541-548 [DOI] [PubMed] [Google Scholar]
- 37. Green JB, Skaife TL, Leslie BM. Bilateral distal biceps tendon ruptures. J Hand Surg Am. 2012;37(1):120-123 [DOI] [PubMed] [Google Scholar]
- 38. Groppel JL, Nirschl RP. A mechanical and electromyographical analysis of the effects of various joint counterforce braces on the tennis player. Am J Sports Med. 1986;14(3):195-200 [DOI] [PubMed] [Google Scholar]
- 39. Grundberg AB, Dobson JF. Percutaneous release of the common extensor origin for tennis elbow. Clin Orthop Relat Res. 2000;376:137-140 [DOI] [PubMed] [Google Scholar]
- 40. Haake M, Konig IR, Decker T, et al. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: a randomized multicenter trial. J Bone Joint Surg Am. 2002;84(11):1982-1991 [DOI] [PubMed] [Google Scholar]
- 41. Hamilton PG. The prevalence of humeral epicondylitis: a survey in general practice. J R Coll Gen Pract. 1986;36(291):464-465 [PMC free article] [PubMed] [Google Scholar]
- 42. Hay EM, Paterson SM, Lewis M, Hosie G, Croft P. Pragmatic randomised controlled trial of local corticosteroid injection and naproxen for treatment of lateral epicondylitis of elbow in primary care. BMJ. 1999;319(7215):964-968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hechtman KS, Uribe JW, Botto-vanDemden A, Kiebzak GM. Platelet-rich plasma injection reduces pain in patients with recalcitrant epicondylitis. Orthopedics. 2011;34(2):92. [DOI] [PubMed] [Google Scholar]
- 44. Herrick RT, Herrick S. Ruptured triceps in a powerlifter presenting as cubital tunnel syndrome: a case report. Am J Sports Med. 1987;15(5):514-516 [DOI] [PubMed] [Google Scholar]
- 45. Hume PA, Reid D, Edwards T. Epicondylar injury in sport: epidemiology, type, mechanisms, assessment, management and prevention. Sports Med. 2006;36(2):151-170 [DOI] [PubMed] [Google Scholar]
- 46. Jockel CR, Mulieri PJ, Belsky MR, Leslie BM. Distal biceps tendon tears in women. J Shoulder Elbow Surg. 2010;19(5):645-650 [DOI] [PubMed] [Google Scholar]
- 47. Jorgensen F, Solgaard S. Bilateral rupture of the triceps tendon in a patient receiving long-term hemodialysis. Ugeskr Laeger. 1982;144(37):2723 [PubMed] [Google Scholar]
- 48. Kaleli T, Ozturk C, Temiz A, Tirelioglu O. Surgical treatment of tennis elbow: percutaneous release of the common extensor origin. Acta Orthop Belg. 2004;70(2):131-133 [PubMed] [Google Scholar]
- 49. Kijowski R, De Smet AA. Magnetic resonance imaging findings in patients with medial epicondylitis. Skeletal Radiol. 2005;34(4):196-202 [DOI] [PubMed] [Google Scholar]
- 50. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow): clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81(2):259-278 [PubMed] [Google Scholar]
- 51. Kuklo TR, Taylor KF, Murphy KP, Islinger RB, Heekin RD, Baker CL. Arthroscopic release for lateral epicondylitis: a cadaveric model. Arthroscopy. 1999;15(3):259-264 [DOI] [PubMed] [Google Scholar]
- 52. Kurppa K, Viikari-Juntura E, Kuosma E, Huuskonen M, Kivi P. Incidence of tenosynovitis or peritendinitis and epicondylitis in a meat-processing factory. Scand J Work Environ Health. 1991;17(1):32-37 [DOI] [PubMed] [Google Scholar]
- 53. Kurvers H, Verhaar J. The results of operative treatment of medial epicondylitis. J Bone Joint Surg Am. 1995;77(9):1374-1379 [DOI] [PubMed] [Google Scholar]
- 54. Labelle H, Guibert R. Efficacy of diclofenac in lateral epicondylitis of the elbow also treated with immobilization: the University of Montreal Orthopaedic Research Group. Arch Fam Med. 1997;6(3):257-262 [DOI] [PubMed] [Google Scholar]
- 55. Lattermann C, Romeo AA, Anbari A, et al. Arthroscopic debridement of the extensor carpi radialis brevis for recalcitrant lateral epicondylitis. J Shoulder Elbow Surg. 2010;19(5):651-656 [DOI] [PubMed] [Google Scholar]
- 56. Mackay D, Rangan A, Hide G, Hughes T, Latimer J. The objective diagnosis of early tennis elbow by magnetic resonance imaging. Occup Med (Lond). 2003;53(5):309-312 [PubMed] [Google Scholar]
- 57. Mair SD, Isbell WM, Gill TJ, Schlegel TF, Hawkins RJ. Triceps tendon ruptures in professional football players. Am J Sports Med. 2004;32(2):431-434 [DOI] [PubMed] [Google Scholar]
- 58. Martin CE, Schweitzer ME. MR imaging of epicondylitis. Skeletal Radiol. 1998;27(3):133-138 [DOI] [PubMed] [Google Scholar]
- 59. Martinez-Silvestrini JA, Newcomer KL, Gay RE, Schaefer MP, Kortebein P, Arendt KW. Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther. 2005;18(4):411-419 [DOI] [PubMed] [Google Scholar]
- 60. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34(11):1774-1778 [DOI] [PubMed] [Google Scholar]
- 61. Nirschl RP. Prevention and treatment of elbow and shoulder injuries in the tennis player. Clin Sports Med. 1988;7(2):289-308 [PubMed] [Google Scholar]
- 62. Nirschl RP. Tennis elbow. Orthop Clin North Am. 1973;4(3):787-800 [PubMed] [Google Scholar]
- 63. Ollivierre CO, Nirschl RP, Pettrone FA. Resection and repair for medial tennis elbow: a prospective analysis. Am J Sports Med. 1995;23(2):214-221 [DOI] [PubMed] [Google Scholar]
- 64. Ono Y, Nakamura R, Shimaoka M, et al. Epicondylitis among cooks in nursery schools. Occup Environ Med. 1998;55(3):172-179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Othman AM. Arthroscopic versus percutaneous release of common extensor origin for treatment of chronic tennis elbow. Arch Orthop Trauma Surg. 2011;131(3):383-388 [DOI] [PubMed] [Google Scholar]
- 66. Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255-262 [DOI] [PubMed] [Google Scholar]
- 67. Pettrone FA, McCall BR. Extracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitis. J Bone Joint Surg Am. 2005;87(6):1297-1304 [DOI] [PubMed] [Google Scholar]
- 68. Pienimaki T, Siira P, Vanharanta H. Widespread pain in chronic epicondylitis. Eur J Pain. 2011;15(9):921-927 [DOI] [PubMed] [Google Scholar]
- 69. Pienimaki TT, Siira PT, Vanharanta H. Chronic medial and lateral epicondylitis: a comparison of pain, disability, and function. Arch Phys Med Rehabil. 2002;83(3):317-321 [DOI] [PubMed] [Google Scholar]
- 70. Pina A, Garcia I, Sabater M. Traumatic avulsion of the triceps brachii. J Orthop Trauma. 2002;16(4):273-276 [DOI] [PubMed] [Google Scholar]
- 71. Potter HG, Hannafin JA, Morwessel RM, DiCarlo EF, O’Brien SJ, Altchek DW. Lateral epicondylitis: correlation of MR imaging, surgical, and histopathologic findings. Radiology. 1995;196(1):43-46 [DOI] [PubMed] [Google Scholar]
- 72. Ritz BR. Humeral epicondylitis among gas- and waterworks employees. Scand J Work Environ Health. 1995;21(6):478-486 [DOI] [PubMed] [Google Scholar]
- 73. Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275-283 [PubMed] [Google Scholar]
- 74. Savnik A, Jensen B, Norregaard J, Egund N, Danneskiold-Samsoe B, Bliddal H. Magnetic resonance imaging in the evaluation of treatment response of lateral epicondylitis of the elbow. Eur Radiol. 2004;14(6):964-969 [DOI] [PubMed] [Google Scholar]
- 75. Schamblin ML, Safran MR. Injury of the distal biceps at the musculotendinous junction. J Shoulder Elbow Surg. 2007;16(2):208-212 [DOI] [PubMed] [Google Scholar]
- 76. Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164(11):1065-1074 [DOI] [PubMed] [Google Scholar]
- 77. Sierra RJ, Weiss NG, Shrader MW, Steinmann SP. Acute triceps ruptures: case report and retrospective chart review. J Shoulder Elbow Surg. 2006;15(1):130-134 [DOI] [PubMed] [Google Scholar]
- 78. Silverstein B, Welp E, Nelson N, Kalat J. Claims incidence of work-related disorders of the upper extremities: Washington state, 1987 through 1995. Am J Public Health. 1998;88(12):1827-1833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Smith AM, Castle JA, Ruch DS. Arthroscopic resection of the common extensor origin: anatomic considerations. J Shoulder Elbow Surg. 2003;12(4):375-379 [DOI] [PubMed] [Google Scholar]
- 80. Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. J Shoulder Elbow Surg. 1998;7(2):151-153 [DOI] [PubMed] [Google Scholar]
- 81. Stahl S, Kaufman T. The efficacy of an injection of steroids for medial epicondylitis: a prospective study of sixty elbows. J Bone Joint Surg Am. 1997;79(11):1648-1652 [DOI] [PubMed] [Google Scholar]
- 82. Stahl S, Kaufman T. Ulnar nerve injury at the elbow after steroid injection for medial epicondylitis. J Hand Surg Br. 1997;22(1):69-70 [DOI] [PubMed] [Google Scholar]
- 83. Stanley J. Radial tunnel syndrome: a surgeon’s perspective. J Hand Ther. 2006;19(2):180-184 [DOI] [PubMed] [Google Scholar]
- 84. Tagliafico A, Gandolfo N, Michaud J, Perez MM, Palmieri F, Martinoli C. Ultrasound demonstration of distal triceps tendon tears. Eur J Radiol. 2012;81(6):1207-1210 [DOI] [PubMed] [Google Scholar]
- 85. Thanasas C, Papadimitriou G, Charalambidis C, Paraskevopoulos I, Papanikolaou A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med. 2011;39(10):2130-2134 [DOI] [PubMed] [Google Scholar]
- 86. Thornton SJ, Rogers JR, Prickett WD, Dunn WR, Allen AA, Hannafin JA. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33(10):1558-1564 [DOI] [PubMed] [Google Scholar]
- 87. van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am. 2003;85(10):1961-1967 [DOI] [PubMed] [Google Scholar]
- 88. van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). 2009;48(5):528-536 [DOI] [PubMed] [Google Scholar]
- 89. Viegas SF. Avulsion of the triceps tendon. Orthop Rev. 1990;19(6):533-536 [PubMed] [Google Scholar]
- 90. Wagner JR, Cooney WP. Rupture of the triceps muscle at the musculotendinous junction: a case report. J Hand Surg Am. 1997;22(2):341-343 [DOI] [PubMed] [Google Scholar]
- 91. Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Occupation and epicondylitis: a population-based study. Rheumatology (Oxford). 2012;51(2):305-310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Whaley AL, Baker CL. Lateral epicondylitis. Clin Sports Med. 2004;23(4):677-691 [DOI] [PubMed] [Google Scholar]
- 93. Yeh PC, Dodds SD, Smart LR, Mazzocca AD, Sethi PM. Distal triceps rupture. J Am Acad Orthop Surg. 2010;18(1):31-40 [DOI] [PubMed] [Google Scholar]
- 94. Yerger B, Turner T. Percutaneous extensor tenotomy for chronic tennis elbow: an office procedure. Orthopedics. 1985;8(10):1261-1263 [DOI] [PubMed] [Google Scholar]


