Abstract
AIM: To elucidate the colonoscopic features of serrated lesions of the colorectum using magnifying colonoscopy.
METHODS: Broad division of serrated lesions of the colorectum into hyperplastic polyps (HPs), traditional serrated adenomas (TSAs), and sessile serrated adenomas/polyps (SSA/Ps) has been proposed on the basis of recent molecular biological studies. However, few reports have examined the colonoscopic features of these divisions, including magnified colonoscopic findings. This study examined 118 lesions excised in our hospital as suspected serrated lesions after magnified observation between January 2008 and September 2011. Patient characteristics (sex, age), conventional colonoscopic findings (location, size, morphology, color, mucin) and magnified colonoscopic findings (pit pattern diagnosis) were interpreted by five colonoscopists with experience in over 1000 colonoscopies, and were compared with histopathological diagnoses. The pit patterns were categorized according to Kudo’s classification, but a more detailed investigation was also performed using the subclassification [type II-Open (type II-O), type II-Long (type II-L), or type IV-Serrated (type IV-S)] proposed by Kimura T and Yamano H.
RESULTS: Lesions comprised 23 HPs (23/118: 19.5%), 39 TSAs (39/118: 33.1%: with cancer in one case), 50 SSA/Ps (50/118: 42.4%: complicated with cancer in three cases), and six others (6/118: 5.1%). We excluded six others, including three regular adenomas, one hamartoma, one inflammatory polyp, and one juvenile polyp for further analysis. Conventional colonoscopy showed that SSA/Ps were characterized as larger in diameter than TSAs and HPs (SSA/P vs HP, 13.62 ± 8.62 mm vs 7.74 ± 3.24 mm, P < 0.001; SSA/Ps vs TSA, 13.62 ± 8.62 mm vs 9.89 ± 5.73 mm, P < 0.01); common in the right side of the colon [HPs, 30.4% (7/23): TSAs, 20.5% (8/39): SSA/P, 84.0% (42/50), P < 0.001]; flat-elevated lesion [HPs, 30.4% (7/23): TSAs, 5.1% (2/39): SSA/Ps, 90.0% (45/50), P < 0.001]; normal-colored or pale imucosa [HPs, 34.8% (8/23): TSAs, 10.3% (4/39): SSA/Ps, 80% (40/50), P < 0.001]; and with large amounts of mucin [HPs, 21.7% (5/23): TSAs, 17.9% (7/39): SSA/Ps, 72.0% (36/50), P < 0.001]. In magnified colonoscopic findings, 17 lesions showed either type II pit pattern alone or partial type II pit pattern as the basic architecture, with 14 HPs (14/17, 70.0%) and 3 SSA/Ps. Magnified colonoscopy showed the type II-O pit pattern as characteristic of SSA/Ps [sensitivity 83.7% (41/49), specificity 85.7% (54/63)]. Cancer was also present in three lesions, in all of which a type VI pit pattern was also present within the same lesion. There were four HPs and four TSAs each. The type IV-S pit pattern was characteristic of TSAs [sensitivity 96.7% (30/31), specificity 89.9% (72/81)]. Cancer was present in one lesion, in which a type VI pit pattern was also present within the same lesion. In our study, serrated lesions of the colorectum also possessed the features described in previous reports of conventional colonoscopic findings. The pit pattern diagnosis using magnifying colonoscopy, particularly magnified colonoscopic findings using subclassifications of surface architecture, reflected the pathological characteristics of SSA/Ps and TSAs, and will be useful for colonoscopic diagnosis.
CONCLUSION: We suggest that this system could be a good diagnostic tool for SSA/Ps using magnifying colonoscopy.
Keywords: Serrated adenoma, Sessile serrated adenoma/polyp, Hyperplastic polyps, Traditional serrated adenomas, Conventional colonoscopy, Magnifying colonoscopy, Pit patterns, Serrated lesions
INTRODUCTION
In addition to the previously known oncogenic pathways of adenoma-carcinoma sequence and de novo cancer[1], the so-called serrated neoplastic pathway has been proposed in recent years as a new oncogenic pathway from serrated lesions of the colorectum[2-6]. Sessile serrated adenomas/polyps (SSA/Ps) are a particular focus of attention as one type of precursor lesion for the microsatellite deficiency (MSI-H) cancers that comprise around 15% of sporadic colorectal cancers[7-11]. The low risk subtype of serrated adenocarcinomas is characterized by proximal location, BRAF-mutation, high CpG-island methylation with loss of MLH1 expression, and MSI-H phenotype[10,12-14]. Identifying serrated lesions of the colorectum during colorectal cancer surveillance is thus important, but few reports have described the colonoscopic characteristics of these lesions, particularly in terms of magnified colonoscopic findings, and a unified consensus has yet to be reached. We report herein our investigation of the colonoscopic characteristics of serrated lesions of the colorectum, using the surface architecture subclassification proposed by Kimura et al[15] in addition to conventional pit pattern diagnosis.
MATERIALS AND METHODS
Patient characteristics
From among all suspected serrated lesions that were endoscopically resected in our hospital between January 2008 and September 2011, this study examined the 118 lesions for which magnified colonoscopic findings and histopathological specimens could be compared. The study was conducted in accordance with all rules and regulations of the St. Marianna University School of Medicine Institutional Review Board, and informed consent was obtained from each patient.
Endoscopic resection and magnifying colonoscopy
All lesions were sprayed with indigo carmine and observed under endoscopic guidance with a CF-H260AZI endoscope using the EVIS LUCERA system (Olympus, Inc., Tokyo, Japan).
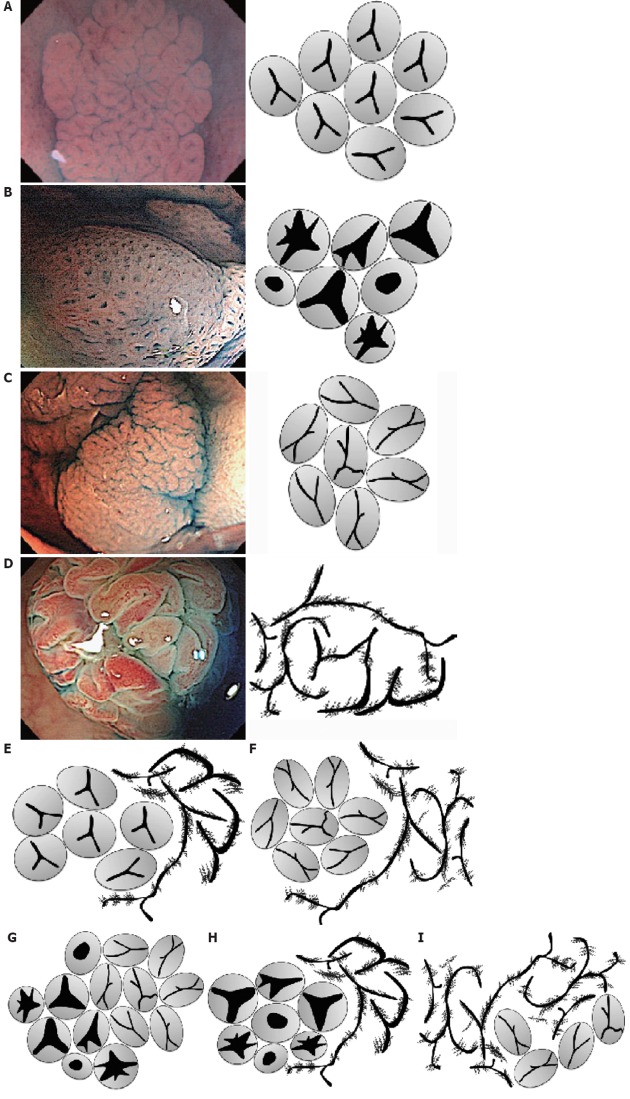
Five categories of conventional colonoscopic findings (location, size, shape, color, and presence or absence of mucin) and magnifying colonoscopic findings (pit pattern diagnosis) for these lesions were interpreted by five colonoscopists with experience in over 1000 colonoscopies, and compared with histopathological diagnoses. In addition to Kudo’s classification, the pit pattern was diagnosed in accordance with the subclassification proposed by Kimura et al[15] and Kudo et al[16] (Figure 1A-I). The endoscope was washed with an automatic washing machine and disinfectant (DISOPA Solution 0.55%, Johnson and Johnson, Langhorne, PA, United States) after each patient, according to the guidelines[17-19].
Figure 1.
Type II pit patterns and subclassification of surface architectures of serrated lesions of the colon and rectum. A: Conventional type II pit pattern. Regular array of star-shaped, uniform pits with serrated architecture; B: Type II-Open pit pattern. Star-shaped pits similar to conventional type II pits, but with dilated openings of the glandular crypts; C: Type II-Long pit pattern. Similar to type II pits, but elongated without dilation; D: Type IV-Serrated pit pattern. Also called “pine cone-shaped.” Villiform with a serrated architecture; E-I: Mixture of example pit patterns (E: Type II with IV-S; F: Type II-L with IV-S; G: Type II-O with II-L; H: Type II-O with IV-S; I: Type IV-S with II-L).
In addition to conventional type II pit pattern according to Kudo’s classification, surface architecture of the lesions was also broadly categorized as type II-Open (type II-O), type II-Long (type II-L), or type IV-Serrated (type IV-S) according to the provisional naming proposed by Kimura et al[15]. If several pit patterns were present in a single lesion, the pit pattern that occupied the greatest area was regarded as the basic architecture. We categorized into two groups as SSA/Ps or others on histopathological findings. Lesions that included a diagnosis other than that of serrated lesion of the colon are indicated as “others”, SSA/P, or SSA/P plus if adenoma was also present together with “SSA/Ps”.
Histopathological diagnosis
Histopathological diagnosis followed conventional diagnostic criteria for regular adenomas, the diagnostic criteria of Torlakovic et al[20] for hyperplastic polyps (HPs) and traditional serrated adenomas (TSAs). For practical purposes, according to the 2010 WHO classification, the diagnostic criteria for SSA/Ps was established by the research project “Potential of Cancerization of Colorectal Serrated Lesions” led by the Japanese Society for Cancer of the Colon and Rectum (JSCCR)[20,21].
According to these criteria, SSA/Ps are composed of serrated cryptal epithelium with aberrant compartmentalization, essentially characterized by the architectural abnormalities listed below. If the serrated lesions had more than two findings [crypt dilation; irregularly branching crypts; horizontally arranged basal crypts (inverted T- and/or L- shaped crypts)], it can be diagnosed as SSA/Ps[21].
Statistical analysis
Statistical testing comprised t tests, χ2 tests, and Fisher’s exact test, with values of P < 0.05 regarded as significant. All statistical analysis were performed using PRISM software for Windows, Version 4 (GraphPad Prism, Inc., San Diego, CA).
RESULTS
Patient characteristics
Lesions comprised 23 HPs, 39 TSAs (complicated with cancer in one case), 50 SSA/Ps (complicated with cancer in three cases), and six others, including regular adenomas and juvenile polyps. We excluded these six other lesions for further analysis. Patient characteristics and conventional colonoscopic findings are shown in Table 1 and Figure 2. Mean age and sex (percentage of females) were 58.9 years/13% for HPs, 61.9 years/33.3% for TSAs, and 63.7 years/32% for SSA/Ps. No characteristic trends were evident in patient backgrounds (Table 1).
Table 1.
Characteristics of the patients and conventional endoscopic findings n (%)
| HPs | TSAs | SSA/Ps | |
| Cases (n) | 23 | 39 | 50 |
| Age (yr), mean ± SD | 58.9 ± 12.8 | 61.9 ± 13.6 | 63.7 ± 10.6 |
| Location | |||
| Right side of colon | 7 (30.4) | 8 (20.5) | 42 (84.0) |
| Left side of colon | 16 (69.6) | 15 (79.5) | 8 (16.0) |
| Morphology | |||
| Flat type | 7 (30.4) | 2 (5.0) | 45 (90.0) |
| Protruded type | 16 (69.6) | 37 (95.0) | 5 (10.0) |
| Color | |||
| NC | 8 (34.8) | 4 (10.3) | 40 (80.0) |
| RC | 15 (65.2) | 35 (89.7) | 10 (20.0) |
| Mucin | |||
| With | 5 (21.7) | 7 (17.9) | 36 (72.0) |
| Without | 18 (78.3) | 32 (82.1) | 14 (28.0) |
| Size (mm), mean ± SD | 7.74 ± 3.24 | 9.89 ± 5.73 | 13.42 ± 8.62 |
HPs: Hyperplastic polyps; TSAs: Traditional serrated adenomas; SSA/Ps: Sessile serrated adenoma/polyps; NC: Normal-colored or pale in color of mucosa; RC: Reddish change in color.
Figure 2.
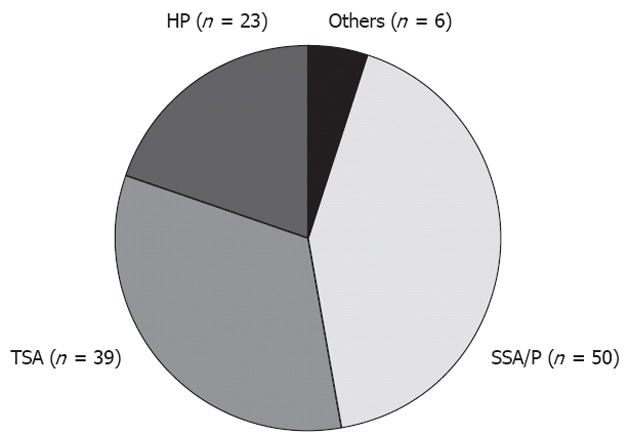
Classification of 118 subject lesions. Ratio of each lesions [traditional serrated adenomas (TSAs), and sessile serrated adenomas/polyps (SSA/Ps) and others].
Conventional colonoscopic findings
We categorized the location of lesions as either right side of the colon (on the oral side of the transverse colon) or left side of the colon (on the anal side of the transverse colon). Results showed that HPs tended to locate on the left side of the colon 69.6% (16/23) rather than the right side 30.4% (7/23). TSAs were more frequently located on the left side 79.5% (31/39) rather than the right side 20.5% (8/39). 84.0% (42/50) of SSA/Ps were on the right and 16% (8/50) were on the left (Table 1). SSA/Ps were found significantly more often on the right, compared with TSAs and HPs (P < 0.001) (Table 1).
Macroscopic morphology was categorized as either flat type (includes 0-IIa, superficial flat/elevated tumors: LST, lateral spreading tumor) or protruded type (0-Ip, protruded/pedunculated: 0-Isp, protruded/mixed sessile and pedunculated) based on JSCCR Guidelines 2010 for the treatment of colorectal cancer[22]. Results were as follows: 30.4% (7/23) of HPs were flat type and 69.6% (16/23) were protruded type; 5.1% (2/39) of TSAs were flat type and 94.9% (37/39) were protruded type; and 90.0% (45/50) of SSA/Ps were flat type and 10.0% (5/50) were protruded type. Significantly more SSA/Ps were identified as flat surface lesions compared with TSAs and HPs (P < 0.001) (Table 1).
We categorized as either reddish change (RC) or normal-colored (NC) or pale mucosa). The results were as follows: 65.2% (15/23) of HPs were RC and 34.8% (8/23) were NC; 89.7% (35/39) of TSAs were RC and 10.3% (4/39) were NC; and 20.0% (10/50) of SSA/Ps were RC and 80.0% (40/50) were NC. Significantly more SSA/Ps were same to whitish change in color compared with TSAs and HPs (P < 0.001) (Table 1).
We categorized lesions as without mucin if they could be observed without washing or with only regular washing, or with mucin if they required several repeated washings before they could be observed. Results were as follows: 78.3% (18/23) of HPs were without mucin and 21.7% (5/23) were with mucin; 82.1% (32/39) of TSAs were without mucin and 17.9% (7/39) were with mucin; and 28% (14/50) of SSA/Ps were without mucin and 72% (36/50) were with mucin. Significantly more SSA/Ps showed abundant mucin compared with TSAs and HPs (P < 0.001) (Table 1).
According to the tumor size, mean lesion size was 7.74 ± 3.24 mm for HPs, 9.89 ± 5.73 mm for TSAs, and 13.62 ± 8.62 mm for SSA/Ps. SSA/Ps were significantly larger in mean size compared with TSAs and HPs (SSA/P vs HP, P < 0.001; SSA/P vs TSA, P < 0.01) (Table 1).
Magnified colonoscopic findings
A comparison of magnified colonoscopic findings and histopathological diagnoses is given in Table 2. Seventeen lesions showed either type II pit pattern alone or partial type II pit pattern as the basic architecture, with 14 HPs (82.4%) and 3 SSA/Ps (Table 2).
Table 2.
Comparison of the magnified colonoscopic findings and pathological diagnoses
| Pit pattern | n | HPs (n = 23) | TSAs (n = 38) | TSAs + cancer (n = 1) | SSA/Ps + α (n = 47) | SSA/Ps + cancer (n = 3) |
| Type II | 17 | 14 | 3 | |||
| Alone | 16 | 13 | 3 | |||
| With IV-S | 1 | 1 | ||||
| Type II-L | 15 | 4 | 5 | 6 | ||
| Alone | 10 | 4 | 1 | 5 | ||
| With IV-S | 5 | 4 | 1 | |||
| Type II-O | 49 | 4 | 4 | 38 | 3 | |
| Alone | 30 | 3 | 27 | |||
| With II-L | 9 | 1 | 8 | |||
| With IV-S | 7 | 1 | 3 | 3 | ||
| With VI | 3 | 3 | ||||
| Type IV-S | 31 | 1 | 29 | 1 | ||
| Alone | 28 | 1 | 27 | |||
| With II-L | 2 | 2 | ||||
| With VI | 1 | 1 |
HPs: Hyperplastic polyp; TSAs: Traditional serrated adenoma; SSA/Ps: Sessile serrated adenoma/polyp; SSA/Ps + α: SSA/Ps or SSA/Ps + adenoma, others except serrated lesions.
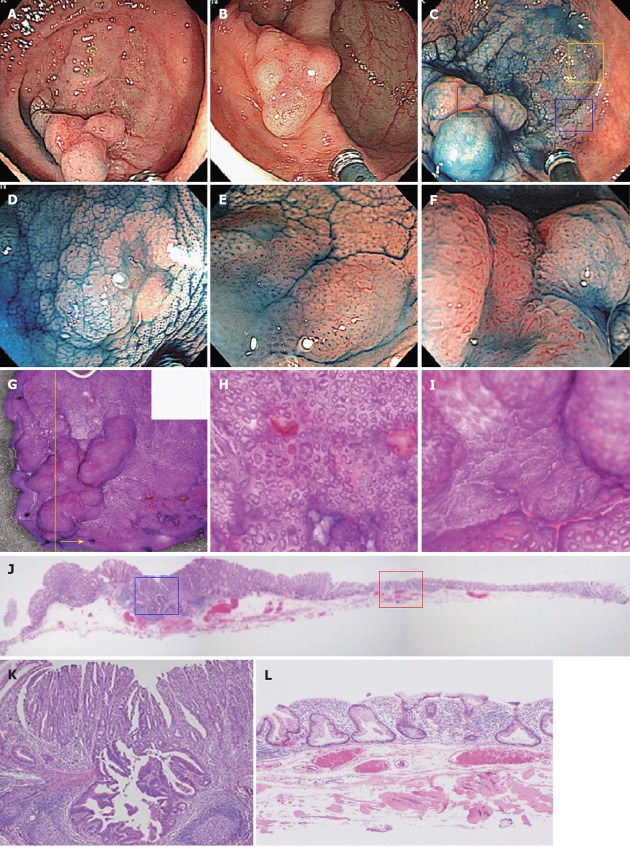
Fifteen lesions showed either type II-L alone or partial type II-L as the basic architecture, of which 6 were SSA/Ps, 5 were TSAs, 4 were HPs. Forty-nine lesions showed either type II-O alone or partial type II-O as the basic architecture, with SSA/Ps histology evident in 41 (83.7%) (Figure 1, Table 2). Cancer was also present in 3 lesions, in all of which a type VI pit pattern was also present within the same lesion (Figure 3C and F). There were 4 HPs and 4 TSAs.
Figure 3.
Adenocarcinoma (tub1) in sessile serrated adenomas/polyps case. A 60-year-old woman had a tumor lesion in the cecum, which was flat and elevated, that is a so-called lateral spreading tumor (LST), 45 mm in diameter. A, B: Standard view. A 45-mm LST lesion with large amounts of mucin is evident in the cecum. The flat portion is somewhat discolored compared with the surrounding mucosa. The protruded portion on the anal side is reddish in the center; C: Indigo carmine staining. The center of the protruded portion on the anal side is flat; D: Indigo carmine staining, enlarged image (yellow square in 3C). Type II-Long pit pattern is evident; E: Indigo carmine staining, enlarged image (blue square in 3C). Type II-Open pit pattern is evident; F: Indigo carmine staining, enlarged image (black square in 3C). We diagnosed as type VI pit pattern, because high density of crypts and irregular pit pattern were evident; G: Comparison of stereomicroscopic and colonoscopic images; H: Enlarged image of flat portion. Although basically type II, dilated duct openings are evident; I: Enlarged image of protruded portion on the anal side. An irregular surface architecture is evident; J: HE magnifying glass image (yellow line in Figure 3G). We examined HE staining (Figure 3J-L) using the yellow cutting line of endoscopically resected tissue (yellow arrow side tissue); K: Central part of the protrusion on the anal side (blue square in Figure 3J). Highly differentiated ductal cancer corresponding to type VI pits is evident; L: Dilatation of crypts and deformation in the horizontal direction at the bottom of the crypts are evident in the flat portion (red square in Figure 3J). Sessile serrated adenomas/polyps was diagnosed.
Thirty-one lesions showed either type IV-S alone or partial type IV-S as the basic architecture, including 30 TSAs (96.8%). Cancer was present in one lesion, in which a type VI pit pattern was also present within the same lesion.
DISCUSSION
Epithelial polyps, a serrated architecture without atypical cells, were previously called HPs. Such lesions were believed not to possess cancerous potential. In 1990, Longacre et al[23] proposed that lesions with a serrated architecture and atypicalities should be known as SAs. Torlakovic et al[20,24] subsequently suggested the existence of a subtype comprising atypia admixed within HPs, for which the name SSAs was proposed. Some, however, consider the term adenoma inappropriate, because these lesions cannot be recognized as tumorous. The latest 2010 WHO classification uses the term SSA/Ps, incorporating both adenoma and polyp[21,25]. The concept of serrated lesions, particularly SSA/Ps, is therefore comparatively new, with terminology and classifications that have only recently been standardized. Although this transition has yet to be fully adopted, the fact that it is widely recognized that there is no risk of cancer developing from HPs is one reason for the lack of detailed reports on the colonoscopic characteristics of these lesions.
Based on the WHO classification, serrated lesions of the colorectum can be broadly divided into HPs, TSAs, and SSA/Ps[25]. The present study investigated the characteristics of these three types from conventional colonoscopic findings and magnified colonoscopic findings (pit pattern diagnosis), which are routinely used in everyday colonoscopic evaluation[25]. To start with conventional colonoscopic findings, the characteristics of HPs are that they tend to occur in the left side of the colon, particularly in the rectum, are commonly less than 5 mm in size, and are NC or pale in color and flat[26]. In this study, HPs did not necessarily fit these characteristics. This may have been because the lesions investigated in the present study had been removed colonoscopically, and HPs that exhibited typical characteristics were not indicated for resection. HPs thus included many atypical lesions. The characteristics of TSAs are that they are Isp or Ip protruded lesions that tend to occur on the left side of the colon, vary in size from less than 5 mm to over 10 mm (although most are less than 10 mm)[23], and are often reddish in color. A further characteristic that was not included in this study is that some flat lesions show a surface architecture that can be described as highly protruding double elevation, pinecone-shaped, or coral-shaped[15,27,28]. In the present study, TSAs mostly satisfied these characteristics. SSA/Ps have been reported as a subclassification of HPs[20,24], and the colonoscopic findings are mostly similar. However, SSA/Ps tend to occur more often in the right colon compared with HPs; many are large, with a diameter exceeding 10 mm, and coloration may be yellowish due to mucin[29]. Our findings in the present study were similar.
In magnified colonoscopic findings, Rembacken et al[30] reported the value of SA diagnosis of lesions with serrated architecture with type IIIL tubiform pit pattern as type
IIIH pits, and type IV villiform pit pattern enlarged to resemble pine cones as type IVH pit pattern. These pits may be considered to correspond to the type IV-S pits of the present study. In this study, TSAs accounted for 76.9% (30/39) of lesions with a basic architecture of type IV-S pit pattern, and lesions without type IV-S pit pattern could be classified as non-TSAs with 96.7% sensitivity and 88.9% specificity. Lesions previously regarded as SAs are now considered to be TSAs, and type IV-S pit pattern can be considered a characteristic finding of TSAs.
Pit patterns reflect the pathological characteristics of lesions, and if the characteristics differ, different pit patterns should also be apparent. HPs are characterized histologically by serrated crypts, with straight crypts evenly distributed throughout[31]. There should thus be no argument that the type II pit pattern of Kudo’s classification reflect this characteristic. Diagnostic criteria for SSA/Ps, however, have yet to be standardized, and the classifications of Higuchi et al[32,33] have mainly been used in Japan. The JSCCR diagnostic criteria used in the present study have extracted three categories from among those defined by Higuchi et al[32,33] that can be regarded as important expressions of the nature of SSA/Ps. Figure 3 shows a typical case of SSA/Ps complicated with cancer treated in our hospital. In terms of serrated crypt, as in HPs, “dilatation of crypts” can be named as an observable colonoscopic finding. This finding may be considered to correspond to the type II-O pit pattern proposed by Kimura et al[15]. The present study also found SSA/P histology in 41 of 50 lesions (82.0%) with type II-O pit pattern as the basic architecture. Lesions without type II-O pit pattern could be classified as non-SSA/Ps with 83.7% sensitivity and 85.7% specificity. We could not deny that we diagnosed as HPs some lesions that even had a tiny SSA/P component at the glandular base. Although it is therefore not possible to diagnose all SSA/Ps solely on the basis of type II-O pit pattern, at least this finding is useful for the diagnosis of SSA/Ps with dilatation of crypts. Even if not diagnosed as SSA/Ps according to current diagnostic criteria, lesions with type II-O pit pattern reportedly possess molecular biological commonalities and regarding these as a single population may be preferable[9,15].
TSAs show a greater number of characteristic findings compared with HPs and SSA/Ps, facilitating colonoscopic diagnosis. Magnified colonoscopic assessment of the histological characteristics of SSA/Ps is difficult when they do not exhibit dilatation of the crypts, and distinguishing them from HPs is difficult at this point. Our findings suggest, however, that type II-O pit pattern may be of assistance in the colonoscopic diagnosis of lesions with dilatation of crypts.
The concept of serrated lesions of the colorectum is relatively recent, and criteria for pathological diagnosis have yet to be standardized. As TSAs and SSA/Ps are undoubtedly precursor lesions of colon cancer, however, colonoscopists are faced with the task of establishing colonoscopic diagnoses and elucidating lesions for which treatment is indicated. Identifying serrated lesions of the colorectum during colorectal cancer surveillance is thus important. Rex et al recommend that all serrated lesions proximal to the sigmoid colon and all serrated lesions in the rectosigmoid > 5 mm in size, be completely removed[34-37]. However, many issues still remain, including whether all TSAs and SSA/Ps should be indicated for treatment as precursor lesions for colon cancer and the probability of progression to a cancerous state. We hope that the present findings will be useful as a reference for the accumulation of larger numbers of cases in further studies to elucidate the oncogenic pathways in serrated lesions of the colon and rectum.
COMMENTS
Background
Broad division of serrated lesions of the colorectum into hyperplastic polyps, traditional serrated adenomas (TSAs), and sessile serrated adenomas/polyps (SSA/Ps) has been proposed on the basis of recent molecular biological studies. However, few reports have examined the colonoscopic features of these divisions, including magnified colonoscopic findings. In this article, the authors verified the diagnostic potency for SSA/Ps using the pit pattern classifications by magnifying colonoscopy.
Research frontiers
The pit patterns were categorized according to Kudo’s classification, but a more detailed investigation was also performed using the subclassification [type II-Open (type II-O), type II-Long (type II-L), or type IV-Serrated (type IV-S)] proposed by Kimura T and Yamano H. However, it has yet to be standardized. In this study, the authors performed herein the investigation of the colonoscopic characteristics of serrated lesions of the colorectum, using the surface architecture subclassification proposed by Kimura T and Yamano H in addition to conventional pit pattern diagnosis
Innovations and breakthroughs
The authors successfully confirmed that the pit pattern diagnosis using magnifying colonoscopy, particularly magnified colonoscopic findings using subclassifications of surface architecture, reflected the pathological characteristics of SSA/Ps and TSAs.
Applications
This study offers a better understanding of pathological characteristics of SSA/Ps and TSAs using subclassifications of surface architecture by magnified colonoscopy.
Terminology
Pit patterns reflect the pathological characteristics of lesions, and if the characteristics differ, different pit patterns should also be apparent. Hyperplastic polyps are characterized histologically by serrated crypts, with straight crypts evenly distributed throughout. There should thus be no argument that the type II pit pattern of Kudo’s classification reflect this characteristic.
Peer review
In magnified colonoscopic findings, lesions without type II-O pit pattern could be classified as non-SSA/Ps with high sensitivity and specificity. It is therefore not possible to diagnose all SSA/Ps solely on the basis of type II-O pit pattern, at least this finding is useful for the diagnosis of SSA/Ps with dilatation of crypts.
Footnotes
Supported by The Japanese Foundation for Research and Promotion of Endoscopy (JFE), in part; The Japanese Society of Gastroenterology (JSGE), to Watanabe Y; The Princess Takamatsu Cancer Research Fund; and A Generous Gift from both the JFE and the JSGE
Peer reviewers: William Dickey, Altnagelvin Hospital, Londonderry BT47 6SB, Northern Ireland, United Kingdom; Navneet K Ahluwalia, MD, FRCP, PhD, AGAF, MBA, Stepping Hill Hospital, Poplar Grove, Stockport Sk2 7JE, United Kingdom
S- Editor Gou SX L- Editor Kerr C E- Editor Xiong L
References
- 1.Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, Nakamura Y, White R, Smits AM, Bos JL. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319:525–532. doi: 10.1056/NEJM198809013190901. [DOI] [PubMed] [Google Scholar]
- 2.Hawkins NJ, Bariol C, Ward RL. The serrated neoplasia pathway. Pathology. 2002;34:548–555. [PubMed] [Google Scholar]
- 3.Jass JR, Young J, Leggett BA. Hyperplastic polyps and DNA microsatellite unstable cancers of the colorectum. Histopathology. 2000;37:295–301. doi: 10.1046/j.1365-2559.2000.01028.x. [DOI] [PubMed] [Google Scholar]
- 4.Jass JR. Serrated adenoma and colorectal cancer. J Pathol. 1999;187:499–502. doi: 10.1002/(SICI)1096-9896(199904)187:5<499::AID-PATH309>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 5.Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–2100. doi: 10.1053/j.gastro.2009.12.066. [DOI] [PubMed] [Google Scholar]
- 6.Shimoda T, Ikegami M, Fujisaki J, Matsui T, Aizawa S, Ishikawa E. Early colorectal carcinoma with special reference to its development de novo. Cancer. 1989;64:1138–1146. doi: 10.1002/1097-0142(19890901)64:5<1138::aid-cncr2820640529>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 7.Grady WM, Markowitz S. Genomic instability and colorectal cancer. Curr Opin Gastroenterol. 2000;16:62–67. doi: 10.1097/00001574-200001000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Issa JP. CpG island methylator phenotype in cancer. Nat Rev Cancer. 2004;4:988–993. doi: 10.1038/nrc1507. [DOI] [PubMed] [Google Scholar]
- 9.Issa JP. Colon cancer: it’s CIN or CIMP. Clin Cancer Res. 2008;14:5939–5940. doi: 10.1158/1078-0432.CCR-08-1596. [DOI] [PubMed] [Google Scholar]
- 10.Toyota M, Ho C, Ahuja N, Jair KW, Li Q, Ohe-Toyota M, Baylin SB, Issa JP. Identification of differentially methylated sequences in colorectal cancer by methylated CpG island amplification. Cancer Res. 1999;59:2307–2312. [PubMed] [Google Scholar]
- 11.Watanabe Y, Castoro RJ, Kim HS, North B, Oikawa R, Hiraishi T, Ahmed SS, Chung W, Cho MY, Toyota M, et al. Frequent alteration of MLL3 frameshift mutations in microsatellite deficient colorectal cancer. PLoS One. 2011;6:e23320. doi: 10.1371/journal.pone.0023320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brennetot C, Duval A, Hamelin R, Pinto M, Oliveira C, Seruca R, Schwartz S. Frequent Ki-ras mutations in gastric tumors of the MSI phenotype. Gastroenterology. 2003;125:1282. doi: 10.1016/j.gastro.2003.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Carvalho B, Pinto M, Cirnes L, Oliveira C, Machado JC, Suriano G, Hamelin R, Carneiro F, Seruca R. Concurrent hypermethylation of gene promoters is associated with a MSI-H phenotype and diploidy in gastric carcinomas. Eur J Cancer. 2003;39:1222–1227. doi: 10.1016/s0959-8049(03)00177-1. [DOI] [PubMed] [Google Scholar]
- 14.Pinto M, Oliveira C, Cirnes L, Carlos Machado J, Ramires M, Nogueira A, Carneiro F, Seruca R. Promoter methylation of TGFbeta receptor I and mutation of TGFbeta receptor II are frequent events in MSI sporadic gastric carcinomas. J Pathol. 2003;200:32–38. doi: 10.1002/path.1327. [DOI] [PubMed] [Google Scholar]
- 15.Kimura T, Yamamoto E, Yamano HO, Suzuki H, Kamimae S, Nojima M, Sawada T, Ashida M, Yoshikawa K, Takagi R, et al. A novel pit pattern identifies the precursor of colorectal cancer derived from sessile serrated adenoma. Am J Gastroenterol. 2012;107:460–469. doi: 10.1038/ajg.2011.457. [DOI] [PubMed] [Google Scholar]
- 16.Kudo S, Tamura S, Nakajima T, Yamano H, Kusaka H, Watanabe H. Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc. 1996;44:8–14. doi: 10.1016/s0016-5107(96)70222-5. [DOI] [PubMed] [Google Scholar]
- 17.Allen JI. Quality colonoscopy. Preface. Gastrointest Endosc Clin N Am. 2010;20:xv–xvi. doi: 10.1016/j.giec.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Allen JI. Quality assurance for gastrointestinal endoscopy. Curr Opin Gastroenterol. 2012;28:442–450. doi: 10.1097/MOG.0b013e3283561f0d. [DOI] [PubMed] [Google Scholar]
- 19.Valdastri P, Simi M, Webster RJ. Advanced technologies for gastrointestinal endoscopy. Annu Rev Biomed Eng. 2012;14:397–429. doi: 10.1146/annurev-bioeng-071811-150006. [DOI] [PubMed] [Google Scholar]
- 20.Torlakovic E, Skovlund E, Snover DC, Torlakovic G, Nesland JM. Morphologic reappraisal of serrated colorectal polyps. Am J Surg Pathol. 2003;27:65–81. doi: 10.1097/00000478-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Fujimori Y, Fujimori T, Imura J, Sugai T, Yao T, Wada R, Ajioka Y, Ohkura Y. An assessment of the diagnostic criteria for sessile serrated adenoma/polyps: SSA/Ps using image processing software analysis for Ki67 immunohistochemistry. Diagn Pathol. 2012;7:59. doi: 10.1186/1746-1596-7-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1–29. doi: 10.1007/s10147-011-0315-2. [DOI] [PubMed] [Google Scholar]
- 23.Longacre TA, Fenoglio-Preiser CM. Mixed hyperplastic adenomatous polyps/serrated adenomas. A distinct form of colorectal neoplasia. Am J Surg Pathol. 1990;14:524–537. doi: 10.1097/00000478-199006000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Torlakovic E, Snover DC. Serrated adenomatous polyposis in humans. Gastroenterology. 1996;110:748–755. doi: 10.1053/gast.1996.v110.pm8608884. [DOI] [PubMed] [Google Scholar]
- 25.Snover DC. Update on the serrated pathway to colorectal carcinoma. Hum Pathol. 2011;42:1–10. doi: 10.1016/j.humpath.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Waye JD, Bilotta JJ. Rectal hyperplastic polyps: now you see them, now you don’t--a differential point. Am J Gastroenterol. 1990;85:1557–1559. [PubMed] [Google Scholar]
- 27.Arao J, Sano Y, Fujii T, Kato S, Fu KI, Yoshino T, Ochiai A, Fujimori T, Yoshida S. Cyclooxygenase-2 is overexpressed in serrated adenoma of the colorectum. Dis Colon Rectum. 2001;44:1319–1323. doi: 10.1007/BF02234791. [DOI] [PubMed] [Google Scholar]
- 28.Oka S, Tanaka S, Hiyama T, Ito M, Kitadai Y, Yoshihara M, Haruma K, Chayama K. Clinicopathologic and endoscopic features of colorectal serrated adenoma: differences between polypoid and superficial types. Gastrointest Endosc. 2004;59:213–219. doi: 10.1016/s0016-5107(03)02693-2. [DOI] [PubMed] [Google Scholar]
- 29.Langdon DE. Large hyperplastic polyps of the right colon. Gastrointest Endosc. 1998;48:659. doi: 10.1016/s0016-5107(98)70081-1. [DOI] [PubMed] [Google Scholar]
- 30.Rembacken BJ, Trecca A, Fujii T. Serrated adenomas. Dig Liver Dis. 2001;33:305–312. doi: 10.1016/s1590-8658(01)80082-7. [DOI] [PubMed] [Google Scholar]
- 31.Jass JR, Whitehall VL, Young J, Leggett BA. Emerging concepts in colorectal neoplasia. Gastroenterology. 2002;123:862–876. doi: 10.1053/gast.2002.35392. [DOI] [PubMed] [Google Scholar]
- 32.Higuchi T, Jass JR. My approach to serrated polyps of the colorectum. J Clin Pathol. 2004;57:682–686. doi: 10.1136/jcp.2003.015230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Higuchi T, Sugihara K, Jass JR. Demographic and pathological characteristics of serrated polyps of colorectum. Histopathology. 2005;47:32–40. doi: 10.1111/j.1365-2559.2005.02180.x. [DOI] [PubMed] [Google Scholar]
- 34.Kahi CJ, Li X, Eckert GJ, Rex DK. High colonoscopic prevalence of proximal colon serrated polyps in average-risk men and women. Gastrointest Endosc. 2012;75:515–520. doi: 10.1016/j.gie.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 35.Kahi CJ, Hewett DG, Norton DL, Eckert GJ, Rex DK. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol. 2011;9:42–46. doi: 10.1016/j.cgh.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Lasisi F, Rex DK. Improving protection against proximal colon cancer by colonoscopy. Expert Rev Gastroenterol Hepatol. 2011;5:745–754. doi: 10.1586/egh.11.78. [DOI] [PubMed] [Google Scholar]
- 37.Rex DK, Ahnen DJ, Baron JA, Batts KP, Burke CA, Burt RW, Goldblum JR, Guillem JG, Kahi CJ, Kalady MF, et al. Serrated Lesions of the Colorectum: Review and Recommendations From an Expert Panel. Am J Gastroenterol. 2012:Jun 19; Epub ahead of print. doi: 10.1038/ajg.2012.161. [DOI] [PMC free article] [PubMed] [Google Scholar]