Abstract
Background.
In some older adults, higher blood pressure (BP) is associated with a lower risk of mortality. We hypothesized that higher BP would be associated with greater mortality in high-functioning elders and lower mortality in elders with lower functional status.
Methods.
Participants were 1,562 Latino adults aged 60–101 years in the Sacramento Area Latino Study on Aging. Functional status was measured by self-reported walking speed, and BP was measured by automatic sphygmomanometer. Death information was determined from vital statistics records.
Results.
There were 442 deaths from 1998 to 2010; 53% were cardiovascular. Mean BP levels (mmHg) varied across fast, medium, and slow walkers: 136, 139, and 140 mmHg (systolic), p = .02 and 75, 76, and 77 mmHg (diastolic), p = .08, respectively. The relationship between systolic BP and mortality varied by self-reported walking speed: The adjusted hazard ratio for mortality in slow walkers was 0.96 per 10 mmHg higher systolic BP (95% confidence interval: 0.89, 1.02) and 1.29 (95% confidence interval: 1.08, 1.55) in fast walkers (p value for interaction <.001). We found a similar pattern for diastolic BP, although the interaction did not reach statistical significance; the adjusted hazard ratio per 10 mmHg higher diastolic BP was 0.89 (95% confidence interval: 0.78, 1.02) in slow walkers and 1.20 (95% confidence interval: 0.82, 1.76) in fast walkers (p value for interaction = .06).
Conclusions.
In high-functioning older adults, elevated systolic BP is a risk factor for all-cause mortality. If confirmed in other studies, the assessment of functional status may help to identify persons who are most at-risk for adverse outcomes related to high BP.
Keywords: Blood pressure, Functional status, Latinos
There is substantial evidence that the association of blood pressure (BP) and mortality differs by age. Epidemiological evidence suggests a U-shaped relationship between BP and poor outcomes in older adults; both low and high levels of BP are associated with worse prognosis (1–4). In the oldest old, the relationship between higher BP levels and lower risk of mortality is even more pronounced. In addition, the effectiveness of BP lowering drugs also appears to be attenuated with age. A large recent meta-analysis of randomized controlled trials illustrated a decreased effect of BP lowering drugs on coronary heart disease and stroke events in older adults (5). Another meta-analysis of hypertension treatment trials limited to adults aged 80 years and older suggested that the benefit of antihypertensive therapy for stroke risk might be offset by an increase in the risk of death (6). In contrast, a recent large randomized controlled trial in adults aged 80 years and older, the Hypertension in the Very Elderly Trial, demonstrated a protective effect of antihypertensive therapy on stroke, cardiovascular events, heart failure, and all-cause mortality, after two years of treatment (7). Notably, the treatment target for systolic BP in this trial was higher (150 mmHg) than in most prior studies in younger people, and the study population included few poor-functioning elders (7).
The reasons for these differences in the associations between BP and outcomes in older adults remain unclear. One proposed explanation is that in poor-functioning older adults whom may have decrements in cardiovascular function, elevated BP may be a compensatory adaptation, necessary to maintain perfusion of vital organs, such as the brain or heart (8,9). In these poor-functioning elders, low BP may be an indicator of greater disease burden and a marker for worse prognosis. Because old age is a period of exceptional heterogeneity in health and functional status, it is possible that these differences may explain the apparent contradictory findings regarding the relationship between BP and mortality in older adults (8).
Even less is known about the relationship between BP, functional status, and outcomes in race/ethnic minorities, where the aging population is less well-studied. Latinos are the fastest growing ethnic group in the United States (10) and may be at higher risk for functional impairment due to risk factors such as diabetes, obesity, and the metabolic syndrome (11). In this study, we examined whether functional status, estimated by self-reported walking speed, modified the relationship between BP and mortality in Latino older adults. We hypothesized that higher systolic and diastolic BP will be associated with increased risk of mortality in elders, who reported faster walking speed; whereas, it would be associated with lower mortality in elders with slower self-reported walking speed. This analysis was conducted with data from the Sacramento Area Latino Study on Aging (SALSA), a cohort of 1,789 Mexican ancestry adults aged 60 years and older at baseline. This cohort had a wide range of physical function, which allowed us to examine the relationship between BP and mortality across a functionally diverse group of elders.
METHODS
Study Population
SALSA is a longitudinal cohort study of 1,789 community-dwelling Mexican Americans residing in California’s Sacramento Valley who were aged 60–101 years at baseline in 1998–1999. The participants were born in Mexico or another Latin American country (51%) or in the United States (49%). The study population and the recruitment of SALSA participants have been described in detail elsewhere (12). Participants were followed every 12–15 months via home visits that included clinical, cognitive, and functional assessments into 2008 for incident dementia and are still being followed for mortality. A semiannual phone call was made to obtain updates on medications, health events, and sociodemographic risk factors. SALSA was approved by the Institutional Review Boards at the University of Michigan and the University of California at San Francisco and Davis.
All-Cause and Cardiovascular Mortality
Mortality was ascertained through May, 2010, through online obituary surveillance, review of the Social Security death index and the National Death Index, review of vital statistics data files from California, and interviews with family members to track those participants who had moved. Death certificates were obtained for 84% (n = 375) of those known to be deceased. Information on cause of death was coded according to the Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems. Cardiovascular disease mortality was defined as deaths for which anywhere on the death certificate mentioned Tenth Revision codes for ischemic heart diseases (codes I20–125), heart failure (code 150), and stroke (codes I63, 164). If a death certificate was not located, the death was classified as all-cause mortality, with the cause unspecified. If the person was not known to be dead, they were coded as alive and censored at the date of last contact.
Blood Pressure
Sitting systolic and diastolic BP was measured at each home visit by automatic sphygmomanometer. Participants were asked to sit without talking for 10 minutes after which BP was measured twice with an interval of 5 minutes between the two measures. The two measures were averaged for this analysis.
Self-reported Walking Speed
Self-reported walking speed was used as a measure of functional status; this measure of walking activity was used to categorize walking ability. Participants were asked about their usual walking pace outdoors and were given six possible responses. Participants’ walking speed was classified as “slow” if they responded “easy/casual,” “never walks outdoors,” or “unable to walk”; “medium” if they responded “normal/average”; and “fast” if they responded “brisk pace” or “very brisk/striding.” Prior literature has demonstrated that self-reported walking measures correlate well with performance-based measures (13). This measure captures participants’ self-perceived functional status across a wide range of function. A recent study in this journal demonstrated that self-reported measures of physical capacity that include a broad range of function have greater reliability and validity compared with those that measure function over a more narrow range of function (eg, inability or ability)(14).
Other Variables
Age, sex, education, and insurance were assessed at baseline by self-report. Baseline body mass index was calculated as weight (in kilograms) divided by height (in meters) squared. Baseline depressive symptoms were measured with the Center for Epidemiologic Studies-Depression (15); the scale ranges from 0 to 60. Baseline cognitive function was assessed using the Modified Mini Mental State exam (16), a test of global cognition with a scale of 0–100 that has been validated and adapted for use in Mexican Americans. Total, high-density lipoprotein, and low-density lipoprotein cholesterol were measured in baseline serum samples as well as triglycerides, fasting glucose, creatinine, C-reactive protein, interleukin-6, and tumor necrosis factor-alpha. History of arthritis (in hands, shoulders, hips, or knees), myocardial infarction, stroke, heart failure, cancer, fracture, and hospitalization were assessed by self-report at baseline. Hypertension and diabetes medication use was assessed by medicine cabinet inventory at each annual visit and updated at the semiannual phone call. Classes of hypertension or diabetes medication were coded using the Centers for Disease Control and Prevention Ambulatory Care Drug Database System (http://www2.cdc.gov/drugs/index.asp).
Statistical Analysis
We first compared the mean values of baseline characteristics from Table 1 of participants across categories of self-reported walking speed, based on an analysis of variance test (or nonparametric equivalent) for continuous variables and a chi-squared test for categorical variables. We examined the adjusted association of systolic and diastolic BP with all-cause and cardiovascular mortality in Cox proportional hazards models with age as the index time. Blood pressure, self-reported walking speed, and all potential confounders were assessed at baseline. All-cause mortality was the primary outcome of interest, and systolic BP was the primary independent variable of interest. Sex was included as a potential confounder in all models; other candidate confounders included those variables listed above under other variables. A covariate was included in the adjusted model if it met the three following criteria: (a) associated with mortality at a significance level of p < .20, (b) associated with systolic BP at a significance level of p < .20, (c) its inclusion in a multivariable model changed the magnitude of the coefficient for systolic BP or the coefficient for the interaction between systolic BP and self-reported walking speed by more than 5%. Of all measures examined, only the Modified Mini Mental State exam, serum creatinine, interleukin-6, and diabetes medication use met all of these criteria. Multiplicative interaction terms between systolic and diastolic BP and self-reported walking speed were included in the multivariable models, and subsequently, models were stratified on self-reported walking speed. We used the Schoenfeld residuals to test if the proportional hazards assumption was met. In addition, we fit models with baseline and time-varying terms for systolic and diastolic BP. As sensitivity analyses, we included multiple comorbid conditions (myocardial infarction, stroke, heart failure, cancer, fracture, hospitalization) and antihypertensive medication use to test if the inclusion of these factors would attenuate the estimates of interest. In order to determine if the interaction between BP and self-reported walking speed was explained by an interaction between BP and age, we also tested whether inclusion of this interaction term would alter the relationship between BP and mortality across categories of self-reported walking speed. Finally, because falling BP levels can be an indicator of the end-of-life, we conducted a third sensitivity analysis, in which we excluded deaths in the first year of follow-up.
Table 1.
Baseline Characteristics of Participants, Stratified by Self-reported Walking Speed
| Slow Walkers (n = 465) | Medium Walkers (n = 816) | Fast Walkers (n = 281) | p Value | |
| Mean ± SD or N (%) | ||||
| Age (y) | 72 ± 8 | 70 ± 6 | 69 ± 6 | <.001 |
| Women | 298 (64) | 445 (55) | 170 (61) | .008 |
| Education (y) | 6.8 ± 5.1 | 7.3 ± 5.4 | 9.1 ± 5.4 | <.001 |
| No health insurance | 33 (7) | 86 (11) | 26 (9) | .13 |
| Depressive symptoms (CES-D) | 13.0 ± 12.0 | 9.1 ± 9.8 | 7.6 ± 9.2 | <.001 |
| Cognitive function (3MSE) | 84 ± 12 | 86 ± 11 | 89 ± 10 | <.001 |
| Systolic blood pressure (mmHg) | 140 ± 21 | 139 ± 19 | 136 ± 18 | .02 |
| Diastolic blood pressure (mmHg) | 75 ± 11 | 76 ± 11 | 77 ± 9 | .02 |
| Body mass index (kg weight/m2) | 30.5 ± 6.8 | 29.9 ± 5.5 | 28.4 ± 5.5 | <.001 |
| Total cholesterol (mg/dL) | 210 ± 40 | 213 ± 39 | 215 ± 39 | .20 |
| Glucose (mg/dL) | 119 ± 51 | 114 ± 45 | 109 ± 39 | .01 |
| Serum creatinine (mg/dL) | 0.93 ± 0.64 | 0.88 ± 0.55 | 0.83 ± 0.32 | .04 |
| C-reactive protein (mg/L) | 7.5 ± 10.4 | 5.4 ± 7.6 | 4.3 ± 7.6 | <.001 |
| Interleukin-6 (pg/mL) | 6.4 ± 10.2 | 4.9 ± 5.1 | 4.1 ± 4.0 | <.001 |
| History of arthritis* | 259 (56) | 371 (46) | 122 (43) | <.001 |
| History of cardiovascular event† | 116 (25) | 116 (14) | 24 (9) | <.001 |
| History of cancer | 53 (11) | 58 (7) | 23 (8) | .03 |
| History of hospitalization | 383 (83) | 562 (69) | 194 (69) | <.001 |
| Diabetes medication use | 141 (30) | 163 (20) | 38 (14) | <.001 |
| Antihypertensive use | 259 (56) | 357 (44) | 102 (36) | <.001 |
Notes: CES-D = Center for Epidemiologic Studies-Depression; 3MSE = Modified Mini Mental State exam.
In hands, shoulders, hips, or knees.
Stroke, myocardial infarction, heart failure.
For an alternative analysis, we classified systolic BP as a binary variable. In order to identify a cutpoint for systolic BP which could be used to group participants based on their risk of mortality, we conducted a regression tree analysis of failure time to all-cause mortality (17). Regression tree analysis is a commonly used data-mining tool that can be used to identify cutpoints for one or more predictor variables (ie, systolic BP and self-reported walking speed) that best distinguish between populations based on an outcome of interest (ie, time to death). We included the same adjustment variables included in the Cox proportional hazards models. We classified high systolic BP based on the cutpoint identified in this analysis (>160 mmHg) and conducted a Cox proportional hazards model to estimate the association of high systolic BP and mortality across categories of self-reported walking speed.
All analyses were conducted with Stata 10.0 (StataCorp, College Station, TX).
RESULTS
Of 1,789 total participants, 1,562 had measured BP and reported walking speed at baseline and were included in this analysis; 465 were classified slow walkers, 816 were medium-speed walkers, and 281 were fast walkers. On average, self-reported slow walkers were older, more likely to be women, have completed fewer years of education, were less likely to have insurance, and had higher depression scores and lower cognitive function compared with faster walkers. Slow walkers had higher body mass index and glucose compared with fast walkers. In addition, creatinine, C-reactive protein, and interleukin-6 levels were higher in slow walkers. Slow walkers also had higher prevalence of a history of arthritis, cardiovascular events, cancer, hospitalization, use of diabetes, and antihypertensive medications. Mean BP levels varied modestly across slow, medium, and fast walkers: 140, 139, and 136 mmHg (systolic), p value = .02, and 77, 76, and 75 mmHg (diastolic), p value = .02, respectively (Table 1).
Blood Pressure and Self-reported Walking Speed
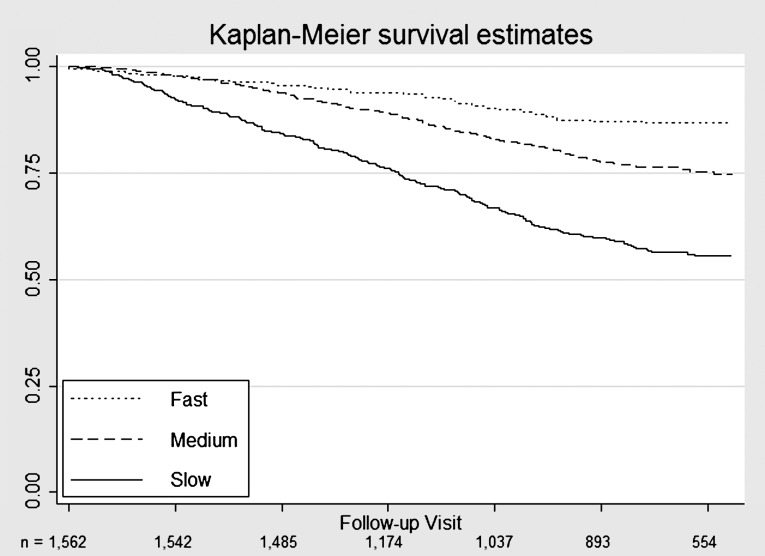
There were 442 deaths from 1998 to 2009; 375 were confirmed by death certificate, and 53% (198/375) of confirmed deaths were reported as from cardiovascular causes. Persons who were identified as slower walkers had a greater risk of mortality compared with faster walkers over the follow-up period (Figure 1). The relationship between systolic BP and mortality varied across self-reported walking speed (p value for interaction = .004). There was no relationship between higher systolic BP and mortality in participants who reported slow or medium speed walking. In contrast, higher systolic BP was associated with a 30% elevated risk of all-cause mortality in the fast walkers (p = .005; Table 2). We observed similar relationships between diastolic BP and all-cause mortality across participants with varying self-reported walking speed. The point estimates for higher BP were in the protective direction in the slower walkers, and harmful in the faster walkers, although the estimates were highly variable, and none reached statistical significance. As a secondary outcome, we examined the relationship between BP and cardiovascular mortality and observed a similar pattern (Table 3). However, the statistical power was limited in this subgroup, and none of the estimates reached statistical significance.
Figure 1.
Kaplan–Meier plot of all-cause mortality, stratified by self-reported walking speed. Study visits were conducted every 12–15 months.
Table 2.
Association of Blood Pressure and Mortality, Stratified by Self-reported Walking Speed
| Slow Walkers (n = 465) | Medium Walkers (n = 816) | Fast Walkers (n = 281) | p Value for interaction* | p Value for pairwise interaction | ||||
| HR† (95% CI) | p Value | HR† (95% CI) | p Value | HR† (95% CI) | p Value | |||
| Systolic blood pressure (10 mmHg‡) | 0.96 (0.89, 1.02) | .18 | 1.00 (0.93, 1.08) | .95 | 1.29 (1.08, 1.55) | .005 | .004 | Ref (slow) |
| .50 (med) | ||||||||
| <.001 (fast) | ||||||||
| Diastolic blood pressure (10 mmHg‡) | 0.89 (0.78, 1.02) | .09 | 1.00 (0.88, 1.15) | .97 | 1.20 (0.82, 1.76) | .35 | .11 | Ref (slow) |
| .16 (med) | ||||||||
| .06 (fast) | ||||||||
Notes: CI = confidence interval; HR = hazard ratio.
For blood pressure by walking speed.
Adjusted for age, gender, cognitive function, creatinine, interleukin-6, diabetes medication use.
HRs are modeled per 10 mmHg higher blood pressure.
Table 3.
Association of Blood Pressure and Cardiovascular Mortality, Stratified by Self-Reported Walking Speed
| Slow Walkers (n = 465) | Medium Walkers (n = 816) | Fast Walkers (n = 281) | p Value for interaction* | p Value for pairwise interaction | ||||
| HR† (95% CI) | p Value | HR† (95% CI) | p Value | HR† (95% CI) | p Value | |||
| Systolic blood pressure (10 mmHg‡) | 0.95 (0.87, 1.05) | .31 | 1.11 (0.98, 1.25) | .09 | 1.28 (0.95, 1.71) | .11 | .11 | Ref (slow) |
| .13 (med) | ||||||||
| .07 (fast) | ||||||||
| Diastolic blood pressure (10 mmHg‡) | 0.85 (0.70, 1.03) | .09 | 1.05 (0.85, 1.29) | .66 | 1.16 (0.59, 2.26) | .67 | .24 | Ref (slow) |
| .18 (med) | ||||||||
| .21 (fast) | ||||||||
Notes: CI = confidence interval; HR = hazard ratio.
For blood pressure by walking speed.
Adjusted for age, gender, cognitive function, creatinine, interleukin-6, diabetes medication use.
HRs are modeled per 10 mmHg higher blood pressure.
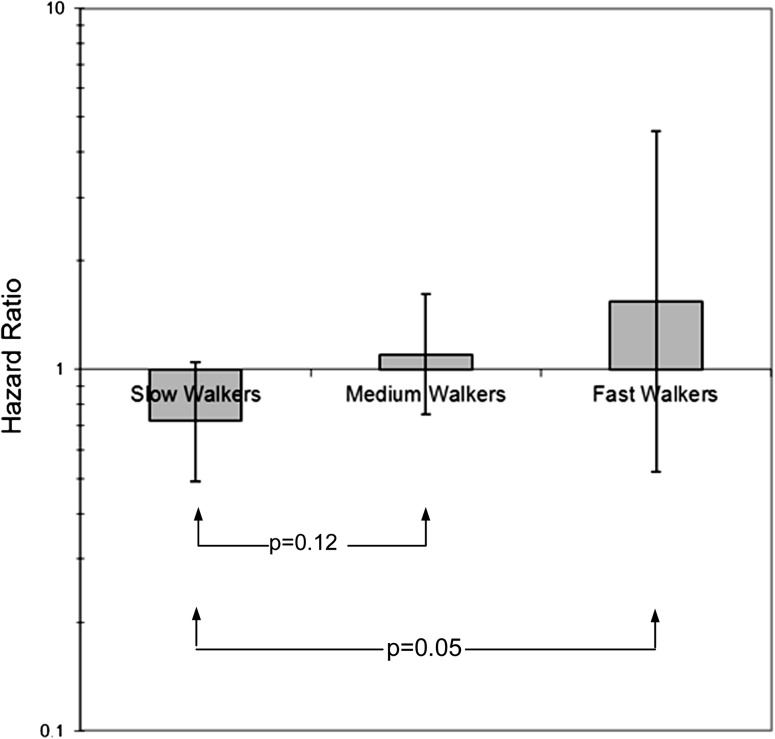
Figure 2.
The association of high systolic blood pressure (>160 mmHg) with all-cause mortality differs in older Latino adults with self-reported slow, medium, and fast walking speed. This association was assessed in a Cox proportional hazards model, adjusted for age, gender, cognitive function, creatinine, interleukin-6, and diabetes medication use. The overall p value for interaction between high systolic blood pressure and walking speed was .10.
The estimates for the associations of systolic BP and all-cause mortality did not change appreciably when we included history of myocardial infarction, stroke, heart failure, cancer, fracture, and hospitalization in the model; the hazard ratios (HRs) per 10 mmHg higher systolic BP were 0.96 (p = .26), 1.01 (p = .78), and 1.30 (p = .004) for slow, medium, and fast walkers, respectively. The inclusion of antihypertensive medication as an adjustment variable also did not change the estimates; the HRs were 0.95 (p = .13), 1.00 (p = .90), and 1.29 (p = .005) for slow, medium, and fast walkers, respectively. The addition of a BP and age interaction term had a minor impact on the estimates; the HRs were 0.95 (p = .45), 1.09 (p = .10), 1.39 (p = .002). Finally, the estimates were robust against the exclusion of deaths in the first year; the HRs were 0.95 (p = .17), 1.00 (p = .99), and 1.31 (p = .005) for slow, medium, and fast walkers, respectively.
Based on the regression tree analysis of systolic BP and self-reported walking speed and time to death, a cutpoint of 160 mmHg best distinguished between survival time in the fast and slow walkers. Systolic BP more than 160 mmHg was associated with a lower HR of death in slow walkers, 0.72 (95% confidence interval: 0.49, 1.05), compared with fast walkers, 1.52 (0.52, 4.58), p value for interaction = .05 (Figure 2).
DISCUSSION
We observed that the association of BP and mortality differs between low- and high-functioning older Latino adults. In participants with fast self-reported walking speed, higher systolic BP was associated with an elevated risk of mortality. This association was not observed among slow walkers. Latino elders have an elevated risk of functional decline because of the high prevalence of risk factors, including diabetes and obesity (18,19). The study of this population with diverse physical functioning may allow us to gain insight into the relationship between BP, mortality, and functional status. Our findings suggest that the functional status of elderly persons is an important factor to consider when studying the association between BP and the risk of mortality. If confirmed in other racial/ethnic populations, measures of functional status may help clinicians to identify older adults who may benefit the most from treatment of high BP. Our finding that higher systolic BP is associated with increased risk of death among fast walkers but not slow or medium walkers may be of particular clinical importance due to the high prevalence of isolated systolic hypertension in elderly adults (20).
One of the earliest studies to suggest an impact of age on the relation between BP and survival in the United States was the Rancho Bernardo Study (1). In a study population of 2,270 predominantly white adults, investigators reported a paradoxical association of higher diastolic BP and lower mortality (p = .04 for trend) in men older than 75 years of age. They did not observe a similar relation in women or younger men, and the relation between systolic BP and mortality was inconclusive. Satish and colleagues (4) investigated the relationship between BP and 6-year mortality in the Established Populations for Epidemiological Studies of the Elderly, a cohort study of 12,802 community-dwelling elderly adults aged 65 years and older. The authors found a strong relationship between higher BP and lower mortality in adults aged 85 years and older; the lowest risk of mortality was at 182 ± 22 mmHg systolic BP. In adults aged 65–84 years, there was a U-shaped relation between systolic BP and mortality; the systolic BP associated with the lowest risk of mortality was 134 ± 3.3 mmHg; mortality risk was elevated at higher and lower BP levels. In older adults, elevated BP has been suggested as a compensatory mechanism to offset reductions in function in the cardiovascular system and a loss of elasticity in vasculature (8,9). Higher BP may be necessary in frail elders to maintain perfusion of the vital organs, such as the brain and heart.
Whereas these prior studies have examined chronologic age as a potential modifier of the relation between BP and mortality, functional status may be a better measure of physiologic aging. Walking speed is strongly associated with mortality, and slower walking speed may identify those individuals who have low reserves in any of a number of organ systems including the cardiovascular, respiratory, musculoskeletal, and nervous systems (21). Self-reported walking speed is a subjective measure and may also be influenced by an individual’s mood, motivation, and self-perception. In addition, the measure of self-perceived walking speed also likely partially captures a participant’s physical activity. Prior research has demonstrated that self-reported measures of health and functional status are strongly associated with mortality and other outcomes (22–25).
Some have suggested that differences in the estimate of the association of BP and survival in older adults in observational studies are due to the conditions associated with lower BP, such as cancer, myocardial infarction, and heart failure; however, in the present study, adjustment for these factors did not influence our estimates. In addition, the differential relationship of BP and mortality in high- and low-functioning elders was present even after the exclusion of persons dying in the first year of follow-up. Both systolic and diastolic BP were slightly higher in the slow walkers compared with the fast walkers, so the paradoxical relation of higher BP and lower mortality in slow walkers is not a result of abnormally low BP levels in these individuals.
The SALSA cohort provided an opportunity to examine a relatively homogenous study population, with a wide range of functional status. The ethnic homogeneity of the study population is an advantage of the study because it reduces the potential for confounding by this factor. However, our study also has limitations, which should be considered. The primary limitation was the limited precision of the estimates; the identification of statistically significant interaction terms typically require larger sample sizes than comparable main effects and may be subject to a higher likelihood of Type II error. Therefore, we used other criteria to interpret the relevance of our findings, namely the consistency of our results across BP measures, all-cause and cardiovascular disease mortality, and sensitivity analyses. However, we interpret the nonstatistically significant findings with caution because of the increase in risk of a Type I error. An additional limitation was that many of the health status variables were determined by self-report, and there may be measurement error or misclassification of these variables. Furthermore, death certificate data may be inaccurate in older adults with multiple comorbid conditions, so our ability to identify cause-specific mortality was limited. Self-perceptions of walking speed may vary across populations and over time. We chose to use baseline measures of BP as our primary predictor of interest in order to compare our findings with those studies that have examined the interaction between BP and age. The current research will inform future work that aims to better unravel the complex relationship between BP, functional status, and mortality over time. Finally, because this study was only conducted in Latino adults, the findings should be confirmed in a more ethnically diverse study population.
In conclusion, across levels of self-reported walking speed, we identified a differential association of BP and mortality in this cohort of older Latino adults. If confirmed in other studies, these findings may help explain the paradoxical association between higher BP and lower mortality in some older populations. This could have important implications regarding the treatment of hypertension; assessment of functional status may help to identify patients who may benefit the most from treatment of high BP.
FUNDING
This work was supported by the National Institute on Aging (R01AG12975 and R01AG033751) and the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK60753). Dr. Odden was supported by a Ruth L. Kirschstein National Research Service Award from the Health Resources and Services Administration (T32HP19025).
References
- 1.Langer RD, Criqui MH, Barrett-Connor EL, Klauber MR, Ganiats TG. Blood pressure change and survival after age 75. Hypertension. 1993;22(4):551–559. doi: 10.1161/01.hyp.22.4.551. [DOI] [PubMed] [Google Scholar]
- 2.Mattila K, Haavisto M, Rajala S, Heikinheimo R. Blood pressure and five year survival in the very old. Br Med J (Clin Res Ed) 1988;296(6626):887–889. doi: 10.1136/bmj.296.6626.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rastas S, Pirttila T, Viramo P, et al. Association between blood pressure and survival over 9 years in a general population aged 85 and older. J Am Geriatr Soc. 2006;54(6):912–918. doi: 10.1111/j.1532-5415.2006.00742.x. [DOI] [PubMed] [Google Scholar]
- 4.Satish S, Freeman DH, Jr, Ray L, Goodwin JS. The relationship between blood pressure and mortality in the oldest old. J Am Geriatr Soc. 2001;49(4):367–374. doi: 10.1046/j.1532-5415.2001.49078.x. [DOI] [PubMed] [Google Scholar]
- 5.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gueyffier F, Bulpitt C, Boissel JP, et al. Antihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. INDANA Group. Lancet. 1999;353(9155):793–796. doi: 10.1016/s0140-6736(98)08127-6. [DOI] [PubMed] [Google Scholar]
- 7.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin JS. Embracing complexity: a consideration of hypertension in the very old. J Gerontol A Biol Sci Med Sci. 2003;58(7):653–658. doi: 10.1093/gerona/58.7.m653. [DOI] [PubMed] [Google Scholar]
- 9.Rigaud AS, Forette B. Hypertension in older adults. J Gerontol A Med Sci. 2001;56(4):M217–M225. doi: 10.1093/gerona/56.4.m217. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Census Bureau. U.S. Interim Projections by Age, Sex, Race, and Hispanic Origin 2008. 2008. [Google Scholar]
- 11.Ottenbacher KJ, Graham JE, Al Snih S, et al. Mexican Americans and frailty: findings from the Hispanic established populations epidemiologic studies of the elderly. Am J Public Health. 2009;99(4):673–679. doi: 10.2105/AJPH.2008.143958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51(2):169–177. doi: 10.1046/j.1532-5415.2003.51054.x. [DOI] [PubMed] [Google Scholar]
- 13.Alexander NB, Guire KE, Thelen DG, et al. Self-reported walking ability predicts functional mobility performance in frail older adults. J Am Geriatr Soc. 2000;48(11):1408–1413. doi: 10.1111/j.1532-5415.2000.tb02630.x. [DOI] [PubMed] [Google Scholar]
- 14.Freedman VA, Kasper JD, Cornman JC, et al. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J Gerontol A Biol Sci Med Sci. 2011;66(9):1013–1021. doi: 10.1093/gerona/glr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:45–50. [Google Scholar]
- 16.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 17.Segal MR. Regression trees for censored data. Biometrics. 1988;44:35–47. [Google Scholar]
- 18.Warner DF, Brown TH. Understanding how race/ethnicity and gender define age-trajectories of disability: an intersectionality approach. Soc Sci Med. 72(8):1236–1248. doi: 10.1016/j.socscimed.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al Snih S, Fisher MN, Raji MA, Markides KS, Ostir GV, Goodwin JS. Diabetes mellitus and incidence of lower body disability among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2005;60(9):1152–1156. doi: 10.1093/gerona/60.9.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franklin SS, Jacobs MJ, Wong ND, L’Italien GJ, Lapuerta P. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension. 2001;37(3):869–874. doi: 10.1161/01.hyp.37.3.869. [DOI] [PubMed] [Google Scholar]
- 21.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 305(1):50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. Am J Epidemiol. 1999;149(1):41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- 23.Khokhar SR, Stern Y, Bell K, et al. Persistent mobility deficit in the absence of deficits in activities of daily living: a risk factor for mortality. J Am Geriatr Soc. 2001;49(11):1539–1543. doi: 10.1046/j.1532-5415.2001.4911251.x. [DOI] [PubMed] [Google Scholar]
- 24.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C, Satariano WA. Self-rated current and future health independently predict subsequent mortality in an aging population. J Gerontol A Biol Sci Med Sci. 2007;62(12):1428–1434. doi: 10.1093/gerona/62.12.1428. [DOI] [PubMed] [Google Scholar]