Abstract
Background
The role of time management in safe and efficient medicine is important but poorly incorporated into the taxonomies of error in primary care. This paper addresses the lack of time management, presenting a framework integrating five time scales termed ‘Tempos’ requiring parallel processing by GPs: the disease's tempo (unexpected rapid evolutions, slow reaction to treatment); the office's tempo (day-to-day agenda and interruptions); the patient's tempo (time to express symptoms, compliance, emotion); the system's tempo (time for appointments, exams, and feedback); and the time to access to knowledge. The art of medicine is to control all of these tempos in parallel and simultaneously.
Method
Two qualified physicians reviewed a sample of 1046 malpractice claims from one liability insurer to determine whether a medical injury had occurred and, if so, whether it was due to one or more tempo-related problems. 623 of these reports were analysed in greater detail to identify the prevalence and characteristics of claims and related time management errors.
Results
The percentages of contributing factors were as follows: disease tempo, 37.9%; office tempo, 13.2%; patient tempo, 13.8%; out-of-office coordination tempo, 22.6%; and GP's access to knowledge tempo, 33.2%.
Conclusion
Although not conceptualised in most error taxonomies, the disease and patient tempos are cornerstones in risk management in primary care. Traditional taxonomies describe events from an analytical perspective of care at the system level and offer opportunities to improve organisation, process, and evidence-based medicine. The suggested classification describes events in terms of (unsafe) dynamic control of parallel constraints from the carer's perspective, namely the GP, and offers improvement on how to self manage and coordinate different contradictory tempos and day-to-day activities. Further work is needed to test the validity and usefulness of this approach.
Keywords: Primary care; adverse event; taxonomy, human error
Introduction
There is a lack of information about the rate of adverse events in primary care compared with those occurring in hospital. Estimates of patient safety incidents in primary care vary considerably from 0.004 to 240 per 1000 primary care consultations; 45–76% of all patient safety incidents are considered preventable.1 Initiatives and methods to collect data on quality and safety in primary care are still being discussed.2
The nature and causes of errors vary significantly between in-hospital and out-of-hospital settings.3 In an out-of-hospital setting, GPs are likely to work with limited direct visual and oral contact with their colleagues and other medical professionals. In addition, patients have greater freedom. They can choose their medical professionals, see and tell their doctors about any problem they consider important or not, choose the time for this disclosure, and the time of the next visit. Moreover, there are few complaints about GPs' suggestions (examinations, drugs).4
Of the available taxonomies used to classify ambulatory medical errors, most use Reason's framework of contributive and causative factors to make the distinction between human errors (knowledge deficiencies) and system errors (communication, process and organisational problems).5 6 Some classifications have attempted to go beyond linking the causes with the impact (outcome),7 preferring to assess the type (of activity) and the domain (setting, staff, patient, target).8 However, the design of a unique and consensual international tool, that is readily usable and reliable for end users (GPs), providing them with comprehensive opportunities for improvement, is still a challenge, especially in primary care.9
There is, however, a consensus in these taxonomies and in the literature that show three recurrent categories of errors and vulnerabilities, relatively specific to primary care, and all related to time control:
First, missed and delayed diagnoses10 are considered to be the main cause of claims and allegations in primary care, especially for cancer and cardiac diseases. Although the calculation of the delay is a matter of debate, diagnostic delays may occur at any point during disease progression and can be divided into pre-symptomatic delays, patient delays, primary care delays, referral delays, and secondary care delays.11 These problems are clearly prevalent in primary care because patients often present with early manifestations of illness, more or less often, with a background of existing psychosocial problems and physical co-morbidities.12 Diagnosis of these conditions, and moreover, during a short consultation, is never easy.
Second, failure in access and availability of GPs on call, especially when calling GPs after hours or during consultations.13 14
Third, communication breakdown in the clinic/office (wrong appointment, wrong chart, missing information15) and between the office and an outside entity (referrals not done, incorrect discharge16).
The core characteristic of all of these sources of failure is an improper dynamic control of the process (care strategy and surveillance of progression of the disease) figure 1.
Figure 1.
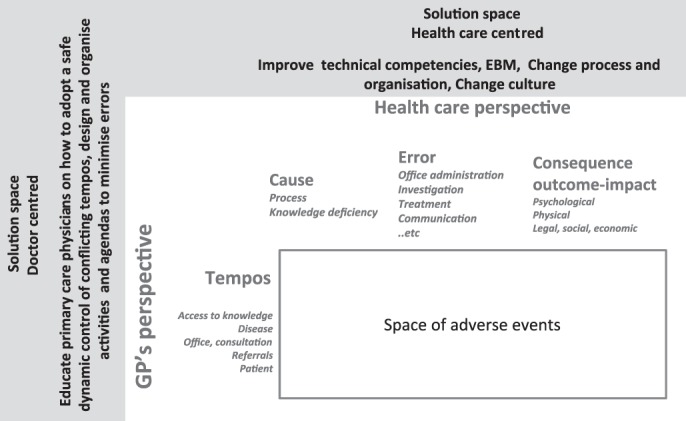
Healthcare-centred taxonomies of medical adverse events and related space of improvement versus doctor-centred taxonomy of unsafe dynamic control of medical tempos (leading to medical adverse events) and related space of improvement. EBM, evidence-based medicine.
Dynamic situations, such as industrial, aviation, or traffic process control, in uncertain environments, have long been one of the major study targets for safety improvements.17–20
In these situations, the human operator only partially controls the technical process or the environment. For example, the actions of a ship's helmsman do not fully determine the route taken by that ship. The combined effects of the steering of the ship, the current, the wind, and the inertia of the ship must also be taken into account. Operators are confronted with uncertainties, in particular because of their partial control of the situation.21
Time can assist cognition and lead to errors in two ways. First, time is encoded in the representation of the activity, and is used as an internal clock to organise tasks. De Keyser22 introduces the notion of time reference systems to demonstrate the existence of different time scales in human and professional tasks requiring parallel processing. Some tasks are managed on a time scale measured in seconds, others are measured in months. For example, the time to get a referral in primary care is measured in days, the time to educate a patient is measured in minutes, and certain therapeutic effects are measured in seconds while others are in months. The operator generally uses deadlines as milestones around which shared activities can be organised. The large number of these deadlines is sometimes misleading, but in most cases, operators manage parallel time scales extremely well, and use them as natural markers to distribute their activity throughout the day.
Second, time is what drives transformation in the world; it has its own problem and error solving potential. Situations are dynamic and, therefore, a problem encountered at one moment in time will not be the same as another encountered later. Sometimes, not doing anything is the best way to solve difficulties. Furthermore, time changes situations. As information stacks up over time, this can sometimes turn a complex problem into a much simpler one. Human beings are well aware of the fact, and often use this property of time. Waiting sometimes becomes the best decision to make, including decisions in terms of workload management. Renewed theories on natural decision-making23 provide numerous inputs into the idea of ‘suffisance’ in the control of time.24 This school of thought has collected data in a great number of high-risk situations (aviation, military and industry). The authors have shown that most biases found in the classical theories on decision-making25 are in fact irrelevant and unimportant in complex and dynamic real-life situations. Decision-making is an ongoing process, linked to the environment. This process is made up of a flow of more or less relevant partial decisions, which eventually lead to an acceptable result, given the margins available in real situations. Operators often have an adequate knowledge of the ‘worlds’ to which their decisions will be applied. For better or worse, operators have an in-depth expertise of what gaps they can fill, therefore they can afford to make decisions already known as being hardly valid, as long as they believe that this decision will not place them in a situation exceeding their level of expertise. It is self evident that GPs use waiting strategies when symptoms are unclear. For example, a young and busy patient voicing a recent, severe but isolated fatigue would probably be prescribed a symptom-relief medication, with the suggestion that a new appointment be made in case of persistence of the fatigue.
Error control usually follows this route. Time is a precious error detection instrument and often helps to alleviate the consequences of errors, but it is also the source of many errors in dynamic situation control.
All taxonomies cite time as a type of error (delays in diagnosis, therapy, referral, admission to hospital7–9) and/or as a cause of errors (time pressure, etc).9 They describe the events from an analytical perspective of the care at the system level and offer opportunities to improve organisation, process and evidence-based medicine (‘The judicious use of the best current evidence in making decisions about the care of the individual patient’, Webster Dictionary). Time is one of the identified problems, and remedies are usually given by recommending new protocols and new organisational tools.
However, these taxonomies are less effective in addressing the events in terms of (unsafe) dynamic control of parallel dimensions of the patient journey from the perspective of the carer. Learning to read medical case stories from this actor-centred point of view may offer additional remedies to reduce adverse events, aiding doctors to adopt a safe personal idea of the patient pathway to complement the recommended technical and systemic organisation of care (figure 1).
This paper attempts to address the lack of time management, describing the failure to control the various times in which doctors must manage to deliver safe care. This complementary contribution to existing taxonomies will hopefully lead to a comprehensive and causative framework of failures in the day-to-day practice of GPs with direct implications for additional learning and improvements.
Method
Material
We reviewed a sample of malpractice claims from one liability insurance company to determine whether a medical injury had occurred and, if so, whether it was due to one or more time-related problems. A total of 1046 files were reviewed, which represents the total number of claims for general practice submitted to this insurance company during the period 2004–2006. This insurance company provides cover for about 60% of all French GPs.
We considered all claims during this 3-year-period, whether they were closed or not (we considered that working with only closed claims meant selecting only old files with lesser relevance for present practice; moreover the correlation between preliminary assessment and final litigation outcome was over 90%). All claims included a thorough medical analysis, and the findings of one or two independent medical appraisals. They also contained an extended summary (3 to 4 pages) of the medical observations written by the insurance medical committee.
Analysis
The reviews were conducted at the insurance company's office by the two authors. The reviews lasted 15 min per file on average and were conducted by one reviewer. The reviewers were made aware of the litigation outcomes but were instructed to ignore them and rely on their own clinical judgement in making decisions about errors. To test the reliability of the process, the first expert's judgement on a case was systematically submitted to the second expert, to check for consensus in the scoring.
The reviews included independent assessments of whether the claim involved injury caused by time-related problems. On the basis of the literature review and preliminary work on a random selection of claims, five types of time-related problems were considered — access to knowledge, office, patient, disease, and out-of-office coordination — and a uniform definition of each type was applied in all cases.
Each problem amounts to a specific time-related aspect of risk that can be termed a ‘tempo’. The Webster dictionary defines tempo as ‘primarily a musical term describing the rate of speed of a musical piece’. By extension, it is a pace of an action, a rate of performance or delivery. The skill of the doctor is to control the tempo of each situation and to manage the five tempos simultaneously, in a consistent manner. Poor control of one or more of these tempos may result in poor quality of care and adverse events. Based on these observations, a draft taxonomy is presented in box 1.
Box 1. A preliminary draft taxonomy of tempos.
-
Disease tempo
– Time estimate of disease evolution
– Time estimate of drug effects
-
Office tempo
– Consultation management
– Interruption management
– Telephone consultation management
– Private agenda management, competitive duties
-
Patient tempo
– Time and opportunity to express symptoms
– Non-compliance with time-related aspects of care
-
Out-office coordination/referral tempo
– Time to get referrals and examination
-
Access to knowledge
– Priming of salient and frequent symptoms
– Inability to access the right knowledge during consultation
The five tempos can be described as follows:
The disease tempo: GPs have an idea of average disease evolution times. For instance, they know that, in a healthy adult, standard flu will last about 10 days and an upper respiratory infection with cough about 7 days (although the total duration may exceed 13 days).26 They also have estimates of the time it takes for drugs to show their expected effects. However, these estimates of time may lead to errors. The disease can escalate, the patient may respond to drugs slowly, and elements can easily combine to produce an unexpected situation. We have encoded this tempo as being at risk any time the evolution of the disease does not follow the usual standard evolution of equivalent pathologies, whether it is too fast, has unanticipated complications or is atypically slow.
The office tempo: physicians, as is the case for any professionals, must organise consultations, visits and administration in a consistent manner, manage interruptions and calls, and make all these activities fit in with other personal, family and private needs. In this paper's analysis, this tempo is considered as being at risk any time the availability of a GP to take care of a patient (whether directly or by telephone) has been reduced or made impossible because of other duties.
The patient's tempo: patients are often emotionally impacted by their symptoms; they may fear describing them. They can be chatty, demanding, silent or aggressive, easing or slowing interactions and doctors' search for relevant history. They can be rapid or slow to comply with doctors' requests for exams or future appointments. We have encoded this tempo as being at risk anytime patients have contributed, by their behaviour, to delay the access to diagnosis and treatment.
The out-of-office coordination tempo: the medical system outside the hospital is difficult to coordinate. Doctors prescribe examinations, radiology/imaging or specialist consultations, but there is no guarantee that the results will be available in a fixed period of time. This tempo is coded as being at risk any time referrals with other medical professionals and feedback of information have exceeded standard delays.
The time to access knowledge is the last category of tempo, clearly different from previous tempos because it relates to biases in cognitive access to memory. External peer judgements and most error taxonomies6–9 consider that errors in patient examination, deficiency in investigation, or undertaking procedures signal a deficiency in knowledge and skills. Such situations, however, are not that simple. Ergonomics18 makes a distinction between competence and performance models. The competence model refers to the knowledge the professionals have; the performance model refers to the contextual activation of such knowledge, required to carry out the job. The cognitive and medical literature on diagnosis27 28 abounds with situations in which operators or doctors have been contextually attracted by a set of apparently obvious or misleading symptoms and jumped to an incorrect diagnosis, although they prove that they have the knowledge of the right diagnosis. This tempo is coded as being at risk whenever the GP has misinterpreted the initial situation and symptoms, or was unable to access the right knowledge during consultation, but showed consistent recovery actions in subsequent events, indicating that the knowledge was not lacking. Conversely, when knowledge was clearly lacking, the report was excluded from the analysis.
For each case, either one tempo was coded when it was considered to be the main source of the problem, or two tempos were coded when two or more tempos were thought to contribute to the problem (only the two most important tempos were coded) (box 2).
Box 2. Case example: a mix of patient tempo (attitude) and office tempo (workload).
Dr B's Office, 14:30, full waiting room, holiday period. Dr ZH on duty, locum of Dr B.
Mrs Simone P, 56 years, usual patient of the office, very talkative, hard to control, asking for prescription replacement for non-severe angina pectoris, type 2 diabetes, and hypercholesterolaemia.
Simone says that she had multiple events from the last visit, some diarrhoea (her husband also), she felt tired many times, with back pain, now going better … She just put on the table a package of old x-rays and biological results … and starts discussing the past.
The patient's file is quite laconic. The three last visits are traced only with mention to treatment replacements.
The locum hesitates, records the patient queries in her file, and tries to regain control and conclude the visit…
Entries in the patient file mention blood pressure and the renewal of prescriptions. The patient was prescribed yeast powder (not mentioned in the file) 2 months later, diagnosis of a sigmoid cancer. Simone confirms having had black stools for 3 months with episodes of diarrhoea and constipation.
Results
Exclusion
Of the 1046 claims initially reviewed, 623 reports were included in the final review. The main reasons for exclusion were as follows: 174 claims had no independent expert review (having been notified because of potential rather than actual claims); and 249 claims were found to be unrelated to problems associated with GPs (legal certificates, pure technical errors or unambiguous knowledge deficiency, per operative complications, etc). A summary of the errors associated with these 249 cases is given in table 1.
Table 1.
Contribution of tempo-related and non-tempo-related incidents to the five main classes of adverse events
| Nature of adverse events | Series of 249 files of non-tempo-related incidents for GPs | Series of 623 files of tempo-related incidents (at least one tempo concerned with the issue) |
| Missed or delayed diagnosis | 7.2% (18) | 25.6% (160) |
| Adverse drug events | 21.7% (54) | 24.1% (150) |
| Poor strategy of care, inadequate treatment, surveillance | 20.1% (50) | 20.7% (129) |
| Ethics, conflict management, and miscellaneous | 39.8% (99) | 17.2% (107) |
| Falls/device and care-induced traumas | 11.2% (28) | 12.4% (77) |
| Total | 100% (249) | 100% (623) |
Percentages are calculated separately for the series of non-tempo-related problems (N=249) and for tempo-related problems (N=623). The total of 1046 files also included 174 claims that had no data or no independent expert review and were excluded from the review (raw data are in brackets).
Global results
The 623 patient files included 318 women and 306 men. The mean age was 48.5 years and the median age was 50 years. The typology of adverse events in our database has already been published.29 It shows that the top three categories of claims were missed and delayed diagnosis (25.6%), errors managing care (non-medication) (20.7%), and adverse drug events (ADEs) (24.1%). The other categories of errors were ethics and patient–doctor conflicts (10.4%), delay or refusal to visit the patient's home (7.2%), device-induced traumas (injections, infiltrations, manipulations) (7.6%), falls in the office (3%) and miscellaneous (1.4%).
The following sections only focus on the five main tempos cited above, which are considered to be potential causes of these adverse events.
Coder agreement
The concordance among coders was measured using the kappa test. Only one principal tempo per report was included for the test. The initial agreement was fair (0.68). The spontaneous convergence was very high for in-office, disease, out-of-office and patient tempos; and a little less for GP's access to knowledge. Complete disagreement after common re-examination by the two coders fell from over 18% to less than 2% of cases.
Results from the database
The tempos assigned to the 623 reports were used to create a three-tiered distribution (table 2). The GP's access to knowledge tempo represents the first third, the disease tempo represents the second third, and the office, patient and out-of-office coordination tempos together represent the last third.
Table 2.
Raw count of tempos in the 623 reports
| Tempos | Non-contributive | Contributive | Decisive | Contributive + decisive (%) |
| Access to knowledge | 416 | 124 | 83 | 33.2 |
| Tempo of the disease | 387 | 132 | 104 | 37.9 |
| Tempo of the office | 541 | 48 | 34 | 13.2 |
| Tempo of the patient | 537 | 57 | 29 | 13.8 |
| Tempo of the out-office coordination | 482 | 58 | 83 | 22.6 |
| 419 | 333 | |||
The causal implication of GP's access to knowledge echoes the literature on GPs' knowledge deficiencies (cited in a third of reports). This indicates that, in most cases, knowledge deficiencies coded in the existing publications are in fact contextual traps in the access to knowledge, rather than complete absence of knowledge.
The other tempos are not coded in existing taxonomies and relate to doctors' ability to cognitively control the various time pressures.
The estimate of the disease tempo is the cornerstone of the time-management process because it determines the margins of regulation available for other tempos. For instance, a 50-year-old man with episodes of diarrhoea lasting for 2 months, with no past history, will trigger a series of routine schemas based on the expectation that the most threatening diagnosis to eliminate is cancer. With that idea in mind, the GP will estimate the safest available time for the first examinations (probably about a month for colonoscopy and blood levels) and a trimester for planning surgery if needed. The GP will therefore class this patient as ‘semi-urgent’ priority, who can tolerate some small delays in out-of-office tempo but not much, and will be ready to accept this patient at the office at short notice. Of course, the reality can follow a different path, with either unexpected complications (disease-related or organisational) or side effects (accepting all interruptions from this patient during a consultation with another patient may ironically induce distraction and generate risk for the other patient present in the office). Typically a cascade effect of time constraints and time-management arbitrations are faced. These can feed and enrich the paradigm of cascade analysis.30
The relation between tempos and errors
In this section we consider the association between the immediate cause of adverse events and the most frequently uncontrolled tempos. We have grouped all the incidents into five main categories: missed or delayed diagnosis, ADEs, poor strategic care, ethics, and care-induced traumas (see table 3).
Table 3.
Relative contribution of each tempo to the five main classes of adverse events
| Nature of adverse events | Series of 623 files of tempo-related events | |||||
| GPs' access to knowledge (%) | Disease tempo (%) | Office tempo (%) | Patient tempo (%) | Out-office coordination tempo (%) | Total | |
| Missed or delayed diagnosis | 30.7 | 51.9 | 4.2 | 6.8 | 19.7 | 113.3 |
| Adverse drug events | 57.1 | 33.3 | 6.0 | 19.0 | 31.0 | 146.4 |
| Poor strategic of care, inadequate treatment, surveillance | 29.9 | 43.3 | 7.5 | 17.2 | 27.6 | 125.4 |
| Ethics, conflict management, and miscellaneous | 4.1 | 6.8 | 50.0 | 20.3 | 23.0 | 104.1 |
| Falls/device and care-induced traumas | 52.2 | 11.9 | 28.4 | 20.9 | 4.5 | 117.9 |
Since the coding scheme was permitting the combination of two contributive tempos, the sum of tempos for a given class of adverse event is always more than 100%. The closer the total to 100%, the more the considered adverse event has resulted from only one tempo (for instance the missed or delayed diagnosis). Conversely, the greater the sum, the more the adverse event has resulted from associations of tempos.
Missed or delayed diagnoses are primarily associated with the disease tempo (52%). There is a clear indication of a repetitive conflicting pattern of tempos for making diagnosis. Although the taxonomies usually consider missed or delayed diagnoses as pointing to knowledge deficiencies,3 31 5 the roles of disease and external triggering factors appear to be even more important. Most errors come from incorrect estimates by GPs of the safe window of time for the critical evolution of the disease, during which GPs consider they can ask for further information and safely wait for the results.
ADEs are most commonly associated with access to knowledge and out-of-office coordination tempos (88% in total). Fifty-six per cent of ADEs are related to the incorrect mistimed administration of anticoagulants before or after discharge from hospital, and poor communication between the in-hospital specialist, the GP and the patient.
Falls relate mainly to the office tempo. For example, doctors rush to write prescriptions just after they have examined patients, leaving patients to stand up from the examination table without assistance.
Ethics and conflict management are typical issues of the office tempo. Doctors are interrupted, give imprudent answers on the telephone, refuse or delay home visits.
Discussion
From this study there are four main results. First, the unsafe control of tempos is present in 71% of the total files (623 out of 872 records containing relevant data). Second, although not cited frequently in taxonomies, the unsafe control of disease tempos is present in 37.9% of the files, while patient tempos account for 13.8%. Third, difficult access to knowledge is present in 33.2% of the files. Fourth, poor control of competing tempos (at least two tempos contributing to the event) is present in 67.2% of the total files (419 out of 623).
The disease tempo appears to be a cornerstone in managing risk. This is also the case for the patient tempo, which may lead to numerous GP errors.32 For both tempos, the reasons under consideration are probably related to the emphasis given to the search for competence and technical causes in adverse event analysis to the detriment of more general and loosely coupled elements of care (workload, personal time to devote to the patient, outside pressures, patients' time, spontaneous evolution of the pathology).
The suggested draft taxonomy highlights overlaps with current taxonomies, although this does not include non-identical parts of the safety problem and, as such, seems to offer new opportunities for improvement. Classic taxonomies classify events according to error, causes, and consequences and lead to opportunities for improvement in terms of organisation, process and evidence-based medicine. The suggested classification describes events in terms of unsafe dynamic control of care from the point of view of the carer, namely the GP, and therefore, may lead to specific education and design improvements. At present, it appears that education provided to primary care physicians on time management of encounters is highly variable across the world. Emphasis on tracking time-sensitive events, such as referrals, test results or disease progression, also varies greatly from setting to setting both in educational venues and clinical practice. This framework may help to standardise training and provide a safer agenda for day-to-day activities. It may even inspire GPs to carry out their own safety audits on personal strategies to cope with risk when reporting and analysing adverse events.
Limitations
We acknowledge there are some limitations to this study. First, the data were limited to insurance claims and research based on other data (reported incidents, chart audits, etc) is needed. Second, there were only two judges who are the co-authors of this paper, and there was limited or no capacity to obtain further medical information other than what was included on the reviewers' reports.
The problem of potentially divergent coding by the reviewers for the access to knowledge tempo requires further comment. Reports are factual, describing visible actions and poorly reflecting the context and any hesitation by GPs. Moreover, the specific context of an insurance claim gives emphasis to non-compliance with evidence-based medicine, which is cited in over 80% of the reports and may lead to some causes being overvalued.
A final issue is generalisation, which may be limited by the focus on French GPs, but has the potential to have a broader focus than in France or in general practice. This study could prove to be relevant for all non-acute healthcare settings, not just general practice but also outpatient care in hospitals. At this stage, therefore, this can be considered only as a promising preliminary tool requiring further tests to determine validity and usefulness in different settings.
Conclusion
The process control industry has long invested in the role of time, as well as success or failure. Training courses have been developed in the aviation and nuclear industries, with explicit recommendations and guidelines on good practice. Conversely, in medicine, with some exceptions,5 6 time has not usually been conceptualised as a main component of error analysis, nor has it been considered in safety culture, quality approaches, or even WHO curricula for patient safety.33 However, there is mounting evidence that tempos are at the core of successful and safe medical practice, especially in primary care.
We therefore recommend four main strategic skills to be taught to GPs to help with time control:
learning how to develop safe control of time during the consultation
learning coping strategies when dealing with multiple parallel activities, especially telephone calls: how to answer, what to say, how to deal with a range of issues
learning about realistic margins when arranging diagnostic tests and examinations, or requesting referrals: making sure expected delays are compatible with disease evolution
learning about instructions to give to patients about the expected time effects of medications, and what to do if they are not working as expected.
Acknowledgments
We thank Bronwyn Shumack from CEC (Sydney), Aisling Tierney and Maxime Brami for helpful comments and proofreading.
Footnotes
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Makeham M, Dovey S, Runciman W, et al. Methods and measures used in primary care patient safety research. Results of a literature review on behalf of the Methods & Measures Working Group of the WHO World Alliance for Patient Safety. 2007. http://www.who.int/patientsafety/research/methods_measures/makeham_dovey_full.pdf(accessed 16 Aug 2011). [Google Scholar]
- 2.Wetzels R, Wolters R, van Weel C, et al. Mix of methods is needed to identify adverse events in general practice: a prospective observational study. BMC Fam Pract 2008;9:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makeham MA, Stromer S, Bridges-Webb C, et al. Patient safety events reported in general practice: a taxonomy. Qual Saf Health Care 2008;17:53–7 [DOI] [PubMed] [Google Scholar]
- 4.Barber N. Should we consider non-compliance a medical error? Qual Saf Health Care 2002;11:81–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dovey SM, Meyers DS, Phillips RL, Jr, et al. A preliminary taxonomy of medical errors in family practice. Qual Saf Health Care 2002;11:233–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makeham MA, Dovey SM, County M, et al. An international taxonomy for errors in general practice: a pilot study. Med J Aust 2002;177:68–72 [DOI] [PubMed] [Google Scholar]
- 7.Pace WD, Fernald DH, Harris DM, et al. Developing a taxonomy for coding ambulatory medical errors: a report from the ASIPS Collaborative. Advances in patient safety: from research to implementation (Volume 2: Concepts and methodology). Rockville (MD): Agency for Healthcare Research and Quality (US), 2005. http://www.ahrq.gov/downloads/pub/advances/vol2/pace.pdf (accessed 16 Aug 2011). [PubMed] [Google Scholar]
- 8.Chang A, Schyve PM, Croteau RJ, et al. The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care 2005;17:95–105 [DOI] [PubMed] [Google Scholar]
- 9.Weingart SN. Beyond Babel: prospects for a universal patient safety taxonomy. Int J Qual Health Care 2005;17:93–4 [DOI] [PubMed] [Google Scholar]
- 10.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med 2006;145:488–96 [DOI] [PubMed] [Google Scholar]
- 11.Neal RD, Pasterfield D, Wilkinson C, et al. Determining patient and primary care delay in the diagnosis of cancer—lessons from a pilot study of patients referred for suspected cancer. BMC Fam Pract 2008;9:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobson L, Elwyn G, Robling M, et al. Error and safety in primary care: no clear boundaries. Fam Pract 2003;20:237–41 [DOI] [PubMed] [Google Scholar]
- 13.Hildebrandt DE, Westfall JM, Fernald DH, et al. Harm resulting from inappropriate telephone triage in primary care. J Am Board Fam Med 2006;19:437–42 [DOI] [PubMed] [Google Scholar]
- 14.Derkx HP, Rethans JJ, Muijtjens AM, et al. Quality of clinical aspects of call handling at Dutch out of hours centres: cross sectional national study. BMJ 2008;337:a1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA 2005;293:565–71 [DOI] [PubMed] [Google Scholar]
- 16.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831–41 [DOI] [PubMed] [Google Scholar]
- 17.Woods D, Hollnagel E. Mapping cognitive demands in complex problem solving worlds. Int J Man Mach Stud 1987;26:257–75 [Google Scholar]
- 18.Amalberti R, Deblon F. Cognitive modelling of fighter aircraft's control process: a step towards intelligent onboard assistance system. Int J Man Mach Stud 1992;36:639–71 [Google Scholar]
- 19.Cellier JM, De Keyser V, Valot C, eds. La gestion du temps dans les environnements dynamiques 1996. Paris: PUF [Time management in dynamic environments], 1996 [Google Scholar]
- 20.Hollnagel E. Time and time again. Theor Issues Ergon Sci 2002;3:143–58 [Google Scholar]
- 21.Hoc JM, Amalberti R. Cognitive control dynamics for reaching a satisficing performance in complex dynamic situations. J Cogn Eng Decision making 2007;1:22–55 [Google Scholar]
- 22.De Keyser V. Time in ergonomics research. Ergonomics 1995;38:1639–60 [Google Scholar]
- 23.Klein GA, Orasanu J, Calderwood R, et al. Decision making in action: models and methods. Norwood, NJ: Ablex, 1993 [Google Scholar]
- 24.Amalberti R. La conduite de systèmes à risques [Controlling risky systems]. Paris: Presses Universitaires de France, 2001. (First published 1996). [Google Scholar]
- 25.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science 1974;185:1124–31 [DOI] [PubMed] [Google Scholar]
- 26.Jackson LA, Cherry JD, Wang SP, et al. Frequency of serological evidence of Bordetella infections and mixed infections with other respiratory pathogens in university students with cough illnesses. Clin Infect Dis 2000;31:3–6 [DOI] [PubMed] [Google Scholar]
- 27.Wachter RM. Why diagnostic errors don't get any respect—and what can be done about them. Health Aff (Millwood) 2010;29:1605–10 [DOI] [PubMed] [Google Scholar]
- 28.Kostopoulou O, Devereaux-Walsh C, Delaney BC. Missing celiac disease in family medicine: the importance of hypothesis generation. Med Decis Making 2009;29:282–90 [DOI] [PubMed] [Google Scholar]
- 29.Brami J, Amalberti R. La sécurité du patient en médecine générale [Patient safety in primary care]. Paris: Springer, 2009 [Google Scholar]
- 30.Woolf SH, Kuzel AJ, Dovey SM, et al. A string of mistakes: the importance of cascade analysis in describing, counting, and preventing medical errors. Ann Fam Med 2004;2:317–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jacobs S, O'Beirne M, Derfiingher LP, et al. Errors and adverse events in family medicine: developing and validating a Canadian taxonomy of errors. Can Fam Physician 2007;53:271–6, 270. [PMC free article] [PubMed] [Google Scholar]
- 32.Buetow S, Kiata L, Liew T, et al. Patient error: a preliminary taxonomy. Ann Fam Med 2009;7:223–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Alliance for Patient Safety WHO Patient safety curriculum guide for medical schools. http://www.who.int/patientsafety/activities/technical/who_ps_curriculum.pdf (accessed 16 Aug 2011).


