Abstract
The optimal administration of 5-fluorouracil (5-FU)/leucovorin (LV) for colorectal cancer (CRC) has yet to be fully defined although evidence of the combination has already been established. In a multicentre phase II study, pharmacokinetic modulating chemotherapy (PMC), which is based on the concept that continuous intravenous 5-FU infusion can be enhanced by low-dose oral uracil/tegafur, was combined with LV and administered. Thirty-seven patients were enrolled. The objective response rate was 31.4% and the tumour stabilization rate was 85.7%. The most common toxic effects were neutropenia and hand-foot skin reactions although no life-threatening grade 3–4 toxicities were noted. Grade 3 toxicities such as neutropenia, nausea, diarrhoea and oesophagitis occurred in one patient each. We identified the usefulness of a new type of infusional 5-FU combined with LV for the treatment of CRC. The combination of PMC and LV is active with an acceptable rate of toxicity as a first-line treatment of advanced CRC.
Keywords: pharmacokinetic modulating chemotherapy, 5-fluorouracil, leucovorin, colorectal cancer
Introduction
Surgery is the mainstay of treatment in colorectal cancer (CRC). However, during the past decade the role of chemotherapy has expanded considerably. Previously dominated by bolus injections of 5-fluorouracil (5-FU), chemotherapy has made considerable progress in CRC by biochemical modulation of the 5-FU effect by leucovorin (LV) (1), the development of infused 5-FU/LV regimens (2,3) and the introduction of two new cytotoxic drugs, irinotecan and oxaliplatin (4–6). Particularly, 5-FU has played a central role in the treatment of CRC, and many attempts have been made to improve its efficacy and potentiate its action over the last 50 years.
One approach was the biochemical modulation with compounds such as methotrexate (7) and LV (8). Another approach was the attempt to influence the mode of administration on the mechanism of action and pharmacology of 5-FU. Many studies have compared the protracted venous infusion method, also known as continuous infusion, to the bolus infusion of 5-FU alone or in combination with LV (9). Since publication of the meta-analysis, several other randomized trials have been performed to compare infusional 5-FU to bolus 5-FU regimens. A number of infusional 5-FU regimens that were developed have been useful in the treatment of patients with CRC. De Gramont et al developed a regimen that contained a 400 mg/m2 5-FU bolus, 200 mg/m2/2 h LV, followed by 600 mg/m2 5-FU over 22 h on days 1 and 2 per week. A randomized trial demonstrated that this regimen was associated with significantly higher response rates and a longer time to progression compared with bolus 5-FU/LV (10). Furthermore, the clinical effect of chemotherapy for CRC has made rapid progress with the development of the combination regimens, 5-FU/LV/CPT-11 and 5-FU/LV/oxaliplatin. In these triplet regimens, infusional 5-FU, derived from the De Gramont regimen, showed a better outcome than bolus 5-FU (11). The De Gramont-based regimen of combining a bolus and infusional administration of 5-FU, has currently taken on a central role in CRC chemotherapy, especially in triplet regimens.
On the other hand, our attempt was to modify the pharmacology of 5-FU. We reported the efficacy of pharmacokinetic modulating chemotherapy (PMC), which is based on the concept that the benefit of a continuous intravenous 5-FU infusion can be potentiated by low-dose oral uracil/tegafur (UFT). PMC consists of the continuous infusion of 5-FU over 24 h for 1 day a week at 600 mg/m2/day, and an oral dose of UFT, a 5-FU derivative at 400 mg/day for 5–7 days per week, repeated every week (12–14). Interestingly, PMC resulted in low recurrence and a high-survival rate even in p53 mutant colorectal cancer, which is generally chemoresistant (12). Moreover, we experimentally revealed the potential mechanism of PMC efficacy in CRC (15). In PMC, the infusion of higher amounts of 5-FU once a week in combination with lower amounts of 5-FU taken orally resulted in two different cytotoxic effects, depending on the dose: G1-S arrest and apoptosis with higher 5-FU concentrations, and G2-M arrest and mitotic catastrophe with lower 5-FU concentrations. Thus, PMC is characteristic in that efficacy is obtained from a new type of infusional 5-FU, and potentiation of 5-FU via cell-cycle regulation may play an additional role in multi-drug regimens as well as FOLFIRI or FOLFOX. Theoretically, it is also conceivable that LV plus PMC constitute an ideal 5-FU/LV treatment, since LV is a reduced folate that is easily metabolized to an essential cofactor in the inhibition of thymidylate synthase by FdUMP, an active form of 5-FU (16). On the basis of these results, we therefore conducted a phase II study to assess the efficacy and safety of LV plus PMC as a front-line chemotherapy in patients with metastatic CRC.
Patients and methods
Patient eligibility
Patients with metastatic CRC were eligible for enrollment in the study. Other eligibility criteria were: histologically or cytologically confirmed advanced CRC or postoperative recurrent cancer with metastasis to other organs (liver, lung and lymph nodes); at least one measurable lesion to Response Evaluation Criteria in Solid Tumours (RECIST) criteria (17); no prior chemotherapy (patients receiving postoperative chemotherapy with oral fluoropyrimidines or 5-FU/LV were acceptable if recurrence occurred at least 24 weeks after the completion of such therapy) or radiotherapy; age between 20 and 79 years; an Eastern Cooperative Oncology Group performance status of 0–2; a life expectancy >12 weeks from the start of treatment; acceptable major organ function (white blood cell count between 4,000 and 12,000 mm3, platelet count >100,000 mm3, haemoglobin >9.5 g/dl, serum AST/ALT <2.5 times the institutional upper limit of normal (ULN), serum total bilirubin <1.5 times the ULN, serum creatinine < ULN and normal electrocardiogram). Written informed consent was required and the study was approved by the ethics boards of the participating centres.
Chemotherapy schedule
Patients received PMC, which consists of continuous infusion of 5-FU over 24 h for 1 day/week at 600 mg/m2/day and an oral dose of UFT at 400 mg/day for 5 days/week, repeated every week. On days 1, 8 and 15, l-LV (250 mg/m2) was administered as a 2-h infusion with PMC. One treatment course consists of 3 cycles of l-LV plus PMC, followed by 2 cycles of PMC alone. Treatment courses were repeated every 5 weeks until evidence of disease progression, unacceptable toxicity or patient refusal. Patients then received second-line chemotherapy based on the preference of their attending physician.
Treatment criteria
Prior to receiving treatment on days 8, 15, 22 and 29, each patient was screened to ensure that the white blood cell count was >3,000 mm3; neutrophil count was >1,500 mm3; platelet count was >100,000 mm3; temperature was <38°C and that no detectable infection nor diarrhoea, or other toxicities more than grade 2, assessed according to the National Cancer Institute Common Toxicity Criteria (NCI-CTC) version 2 were apparent (18). The scheduled dose was not administered when any of the criteria described above was not fulfilled. Treatment was suspended until the patient recovered. However, if administration criteria were not fulfilled for 5 weeks, the patient was removed from the study.
Dose modification criteria
Patients were checked for toxicity during each cycle and the doses of 5-FU were reduced according to the dose modification criteria. 5-FU was reduced by 25% of the previous dose in the case of more than grade 3 haematologic (leukopenia, neutropenia and thrombocytopenia) and non-haematologic toxicity (excluding nausea, vomiting, anorexia and alopecia). If performance status was >3 after chemotherapy was administered, the patient was removed from the study.
Endpoints and evaluation criteria
The primary object of the study was response rate (RR), with toxicity and overall survival (OS) being secondary. Responses were classified according to RECIST criteria (18). Tumour measurement was independently reviewed by a radiologist, who was blinded from the tumour assessments carried out by the investigators. Patients who received at least one treatment course were considered assessable for response and toxicity. OS was calculated from the first day of the treatment to the date patients succumbed to the disease or last follow-up. Toxicity was monitored according to the NCI-CTC version 2.
Sample size
The study comprised a meta-analysis of 6 randomized trials involving 1,219 patients with CRC compared to bolus and infusional 5-FU. The response rate was significantly higher with infusional 5-FU (22 vs. 14%) (1). Our PMC revealed the response rate of <30% in our experiences, while 5-FU/LV achieved response rates of 20–30% in patients receiving initial chemotherapy (1,8). Accordingly, 30% was considered to be the expected response rate and ±15% as the 95% confidence interval. Thus, the required number of patients was estimated to be 35 patients. Therefore, the target number of patients was set at 37 to allow for some exclusions from analysis.
Results
Patient characteristics
From April 2002 to April 2005, 37 patients were enrolled. The baseline characteristics are listed in Table I. The median age was 63 years (range, 38–77). Patients had a histologically proven adenocarcinoma of the colon and rectum. Nineteen (51.4%) had liver metastasis and 6 (16.2%) had lung metastasis. Three (8.1%) patients had both liver and lung metastasis. Six (16.2%) had peritoneal metastasis including ovarian. Three (8.1%) had lymph node metastasis and 2 (5.4%) had local recurrence. The patients had metastatic disease at the time of study entry.
Table I.
Clinical characteristics of the patients.
| No. of patients | 37 |
| Gender | |
| Male | 21 |
| Female | 16 |
| Median age (range) | 65 (38–77) |
| PS | |
| 0 | 27 |
| 1 | 10 |
| Prior treatment | |
| None | 12 |
| Surgery | 25 |
| Tumour | |
| Primary | 25 |
| Recurrent | 12 |
| Histology | |
| Well-differentiated | 10 |
| Moderately differentiated | 13 |
| Poorly differentiated | 2 |
| Mucinous | 2 |
| Sites of metastasis | |
| Liver | 19 (51.4%) |
| Lung | 6 (16.2%) |
| Peritoneal dissemination | 6 (16.2%) |
| Lymph nodes | 3 (8.1%) |
| Local | 2 (5.4%) |
PS, performance status.
Treatment and drug delivery
In total, 595 cycles were administered with a median of 15 cycles per patient (range, 3–48 cycles). The delivered relative dose intensities were 91% for 5-FU.
Tumour response and survival
Thirty-five patients were assessable for tumour response. The objective response rate was 31.4% (95% CI, 23.3–38.7%). There was complete response (CR) in 2 patients, partial response (PR) in 9, stable disease (SD) in 19 and progressive disease (PD) in 5 patients (according to RECIST). The tumour stabilization rate (including SD) was 85.7% (95% CI, 73.6–96.5%).
The median survival time (MST) was 24.7 months and the median follow-up time was 21.9 months (range, 4.5–84.6; Fig. 1). Furthermore, the 1-year survival rate was 78.3% and the 2-year survival rate was 52.8%.
Figure 1.
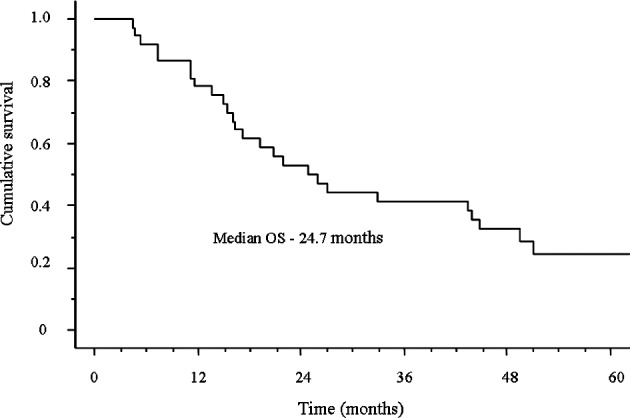
Overall survival (OS) of all patients.
Toxicity
Patients were assessable for safety. Toxic effects observed during the study are listed in Table II. The most common toxic effects were neutropenia and hand-foot skin reaction. Eight patients (21.6%) experienced neutropenia during their course of therapy, although more than grade 3 neutropenia was detected in only 1 patient (2.7%). Nine patients (24.3%) experienced hand-foot skin reactions, of which 7 had grade 1, while 2 had grade 2. There was no treatment-related death or life-threatening toxicity at grades 3–4. Grade 3 nausea, diarrhoea and oesophagitis occurred in 1 patient each (2.7%). Only 1 patient was admitted to the emergency room for paralysis of the lower body due to cervical metastasis.
Table II.
Toxic profile.
| Toxicity | Grade | ≥Grade 3 | Total | |||
|---|---|---|---|---|---|---|
|
|
||||||
| 1 | 2 | 3 | 4 | |||
| Haematological | ||||||
| Neutropenia | 6 | 1 | 1 | 0 | 1 (2.7%) | 8 (21.6%) |
| Non-haematological | ||||||
| Hand-foot skin reaction | 7 | 2 | 0 | 0 | 0 (0.0%) | 9 (24.3%) |
| Fatigue | 1 | 2 | 0 | 0 | 0 (0.0%) | 3 (8.1%) |
| Anorexia | 6 | 0 | 0 | 0 | 0 (0.0%) | 6 (16.2%) |
| Nausea | 0 | 0 | 1 | 0 | 1 (2.7%) | 1 (2.7%) |
| Vomiting | 1 | 0 | 0 | 0 | 0 (0.0%) | 1 (2.7%) |
| Diarrhoea | 3 | 3 | 1 | 0 | 1 (2.7%) | 7 (18.9%) |
| Oesophagitis | 0 | 0 | 1 | 0 | 1 (2.7%) | 1 (2.7%) |
Discussion
The pharmacokinetics of 5-FU are influenced by the dose and schedule of administration. Particularly, a number of infusional 5-FU regimens have been developed that are useful in the treatment of patients with CRC. In general, these regimens have a more favourable toxicity profile compared with bolus 5-FU/LV. However, the principal mechanism of action of 5-FU with various clinical schedules has yet to be clearly defined. Both 5-FU concentration and duration of exposure influence the mechanism of cytotoxicity. Short-term, high-concentration exposures are thought to favour RNA-directed 5-FU toxicity, whereas DNA-directed effects are felt to be more prominent with longer exposures to lower drug concentration (19–21). These pathways are not mutually exclusive, and more than one mechanism of action may contribute to cytotoxicity. Therefore, bolus and infusional 5-FU represents another strategy to improve outcomes by potentially allowing more than one cytotoxic mechanism to occur (10,21). This may support recent standard intravenous 5-FU regimens consisting of the bolus and infusional 5-FU in combination with LV, derived from the De Gramont regimen.
We attempted to produce another effective chemotherapy using a 5-FU-based combination, since the Japanese national insurance did not allow the use of LV in the treatment of CRC until 1999. Kusunoki et al designed a regimen of PMC in 1989, involving continuous the intravenous. infusion of 5-FU for 24 h/week and oral administration of UFT twice a day for 5–7 days/week (12,13), based on experiments using rat models by Fujii et al (22). UFT is a combination of tegafur, a prodrug of 5-FU, and uracil at a molar ratio of 1:4. Dihydropyrimidine dehydrogenase, a key enzyme that degrades 5-FU into therapeutically inactive metabolites, catalyzes the reduction of 60–90% of administered 5-FU, and its catalytic activity correlates with the rate of 5-FU clearance. Uracil inhibits hepatic dihydropyrimidine dehydrogenase, and thus enhances the plasma 5-FU level and antitumour activity of 5-FU (23). Our PMC regimen has improved the prognosis of patients with CRC over the past 10 years (12–15,24). PMC showed an improved prognosis of irradiated rectal cancer with p53 overexpression (12). This result suggested that the antitumour property of 5-FU is enhanced by rectal tumours with a loss of the p53-related apoptotic pathway. In addition, an in vitro study showed that efficacy of the PMC regimen is based on targeting at least two different phases of the cell cycle, regardless of the status of the p53 gene. Surgical specimens after PMC suggested the coexistence of mitotic catastrophe and apoptosis in these specimens (15).
The current study identified the efficacy and safety of LV plus PMC as a front-line chemotherapy in patients with metastatic CRC. Although the response rate of LV plus PMC appeared to be similar to conventional 5-FU/LV, a high tumour stabilization rate was obtained (85.7%) and the OS was 24.7 months. OS in excess of 20 months may be the result of treatments following LV plus PMC. Nineteen of the 37 patients (51.4%) received LV plus PMC, combined with CPT-11 as the second-line chemotherapy. Since Japanese national insurance only allowed the use of oxaliplatin in the treatment of CRC in 2005, we also used the FOLFOX regimen as second- or third-line chemotherapy. Furthermore, we attempted secondary surgery or radiofrequency thermal ablation to remove metastases in 4 patients who obtained tumour stabilization after second-line chemotherapy. Thus, many factors, as well as LV plus PMC, affect the survival of patients with CRC. However, it is conceivable that LV augments the original PMC characteristics with an enhanced efficacy from a new type of infusional 5-FU and potentiation of 5-FU via cell cycle regulation.
In a recent comparative study, we revealed that the use of chemotherapeutic agents or regimens against CRC differed among countries (25). Regional characteristics as to the administration of standard 5-FU were actually identified as factors favouring the use of infused 5-FU/LV in the EU, and oral fluoropyrimidines in Japan. The study concluded that an increasing mutual understanding of regional characteristics along with global evidence could result in standardized treatments suited for regional characteristics, thereby prolonging patient survival. This suggests that the conventional 5-FU/LV regimen is open to further improvement. In addition, recent reports also suggested that 5-FU pharmacokinetics remain an important factor for prognosis in patients with CRC, even after progression of modern chemotherapy (26,27). Therefore, we anticipate that the De Gramont-based regimen is not necessarily going to be the standard 5-FU/LV regimen in the future. The concept of pharmacokinetic modulation for either the PMC or De Gramont regimen resemble each other, and our study suggested that the optimal administration of 5-FU/LV has yet to be defined.
In conclusion, we identified the usefulness of a new type of infusional 5-FU combined with LV for the treatment of CRC. The combination of PMC and LV could be a baseline 5-FU/LV with an acceptable rate of toxicity in the first-line treatment of advanced CRC.
Acknowledgements
This study was conducted by the Mie Colorectal Cancer Chemotherapy Study Group. Study investigators: Yoshiyuki Ito and Toshio Kato (Toyama Hospital, Mie, Japan); Toru Masuda and Eiki Ojima (Mie Prefecture General Medical Centre, Mie, Japan); Kazuo Matsumoto (Shingu Municipal Medical Centre, Wakayama, Japan); Tatsushi Kitagawa and Koichi Matsumoto (Yokkaichi Social Insurance Hospital, Mie, Japan); Tsuneki Kinoshita and Keiji Iriyama (Kuwana Municipal Hospital, Mie, Japan); Hisashi Urata and Kenji Takeuchi (Nabari Municipal Hospital, Mie, Japan).
References
- 1.Meta-analysis Group in Cancer. Efficacy of intravenous continuous infusion of fluorouracil compared with bolus administration in advanced colorectal cancer. J Clin Oncol. 1998;16:301–308. doi: 10.1200/JCO.1998.16.1.301. [DOI] [PubMed] [Google Scholar]
- 2.Saltz LB, Cox JV, Blanke C, et al. Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study Group. N Engl J Med. 2000;343:905–914. doi: 10.1056/NEJM200009283431302. [DOI] [PubMed] [Google Scholar]
- 3.Douillard JY, Cunningham D, Roth AD, et al. Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trial. Lancet. 2000;355:1041–1047. doi: 10.1016/s0140-6736(00)02034-1. [DOI] [PubMed] [Google Scholar]
- 4.De Gramont A, Figer A, Seymour M, et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000;18:2938–2947. doi: 10.1200/JCO.2000.18.16.2938. [DOI] [PubMed] [Google Scholar]
- 5.Giacchetti S, Perpoint B, Zidani R, et al. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2000;18:136–147. doi: 10.1200/JCO.2000.18.1.136. [DOI] [PubMed] [Google Scholar]
- 6.Wagner JS, Adson MA, van Heerden JA. The natural history of hepatic metastases from colorectal cancer: a comparison with resective treatment. Ann Surg. 1984;199:502–508. doi: 10.1097/00000658-198405000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Advanced Colorectal Cancer Meta-Analysis Project. Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: evidence in terms of response rate. Advanced Colorectal Cancer Meta-Analysis Project. J Clin Oncol. 1992;10:896–903. doi: 10.1200/JCO.1992.10.6.896. [DOI] [PubMed] [Google Scholar]
- 8.Thirion P, Michiels S, Pignon JP, et al. Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: an updated meta-analysis. J Clin Oncol. 2004;22:3766–3775. doi: 10.1200/JCO.2004.03.104. [DOI] [PubMed] [Google Scholar]
- 9.Hansen RM, Quebbeman E, Anderson T. 5-Fluorouracil by protracted venous infusion. A review of current progress. Oncology. 1989;46:245–250. doi: 10.1159/000226725. [DOI] [PubMed] [Google Scholar]
- 10.DeGramont A, Bosset JF, Milan C, et al. Randomized trial comparing monthly low-dose leucovorin and fluorouracil bolus with bimonthly high-dose leucovorin and fluorouracil bolus plus continuous infusion for advanced colorectal cancer: a French intergroup study. J Clin Oncol. 1997;15:808–815. doi: 10.1200/JCO.1997.15.2.808. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RM, Sargent DJ, Morton RF, et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004;22:23–30. doi: 10.1200/JCO.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 12.Kusunoki M, Yanagi H, Kotera H, Noda M, Yamamura T. Effects of pharmacokinetic modulating chemotherapy using oral UFT and continuous venous 5FU infusion on the prognosis of irradiated rectal carcinomas with p53 overexpression. Int J Oncol. 1998;13:653–657. doi: 10.3892/ijo.13.4.653. [DOI] [PubMed] [Google Scholar]
- 13.Kusunoki M, Yanagi H, Noda M, Yamamura T. The usefulness of pharmacokinetic modulating chemotherapy (UFT plus 5FU) in the treatment of unresectable colorectal carcinomas. Oncol Rep. 1998;6:547–552. doi: 10.3892/or.6.3.547. [DOI] [PubMed] [Google Scholar]
- 14.Kusunoki M, Yanagi H, Noda M, Yoshikawa R, Yamamura T. Results of pharmacokinetic modulating chemotherapy in combination with hepatic arterial 5-fluorouracil infusion and oral UFT after resection of hepatic colorectal metastases. Cancer. 2000;15:1228–1235. doi: 10.1002/1097-0142(20000915)89:6<1228::aid-cncr6>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 15.Yoshikawa R, Kusunoki M, Yanagi H, et al. Dual antitumor effects of 5-fluorouracil on the cell cycle in colorectal carcinoma cells: a novel target mechanism concept for pharmacokinetic modulating chemotherapy. Cancer Res. 2001;1:1029–1037. [PubMed] [Google Scholar]
- 16.Kubota T, Fujita S, Kodaira S, et al. Antitumor activity of fluoropyrimidines and thymidylate synthetase inhibition. Jpn J Cancer Res. 1991;82:476–482. doi: 10.1111/j.1349-7006.1991.tb01873.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 18.NCI Common Toxicity Criteria Version 2.0. Bethesda: National Cancer Institute, Division of Cancer Treatment; 1999. [Google Scholar]
- 19.Aschele C, Sobrero A, Faderan MA, Bertino JR. Novel mechanism(s) of resistance to 5-fluorouracil in human colon cancer (HCT-8) sublines following exposure to two different clinically relevant dose schedules. Cancer Res. 1992;52:1855–1864. [PubMed] [Google Scholar]
- 20.Sobrero AF, Aschele C, Guglielmi AP, et al. Synergism and lack of cross-resistance between short-term and continuous exposure to fluorouracil in human colon adenocarcinoma cells. J Natl Cancer Inst. 1993;85:1937–1944. doi: 10.1093/jnci/85.23.1937. [DOI] [PubMed] [Google Scholar]
- 21.Sobrero AF, Aschele C, Bertino JR. Fluorouracil in colorectal cancer - a tale of two drugs: implications for biochemical modulation. J Clin Oncol. 1997;15:368–381. doi: 10.1200/JCO.1997.15.1.368. [DOI] [PubMed] [Google Scholar]
- 22.Fujii S, Ikenaka K, Fukushima M, Shirasaka T. Effect of uracil and its derivatives on antitumor activity of 5-fluorouracil and 1-(2-tetrahydrofuryl)-5-fluorouracil. Gann. 1978;69:763–772. [PubMed] [Google Scholar]
- 23.Fujii S, Kitano S, Ikenaka K, Shirasaka T. Effect of co-administration of uracil or cytosine on the anti-tumor activity of clinical doses of 1-(2-tetrahydrofuryl)-5-fluorouracil and level of 5-fluorouracil in rodents. Gann. 1979;70:209–214. [PubMed] [Google Scholar]
- 24.Inoue Y, Miki C, Hiro J, et al. Improved survival using multi-modality therapy in patients with lung metastases from colorectal cancer: A preliminary study. Oncol Rep. 2005;14:1571–1576. [PubMed] [Google Scholar]
- 25.Inoue Y, Toiyama Y, Tanaka K, Miki C, Kusunoki M. A comprehensive comparative study on the characteristics of colorectal cancer chemotherapy. Jpn J Clin Oncol. 2009;39:367–375. doi: 10.1093/jjco/hyp031. [DOI] [PubMed] [Google Scholar]
- 26.Gamelin E, Delva R, Jacob J, et al. Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: results of a multicenter randomized trial of patients with metastatic colorectal cancer. J Clin Oncol. 2008;26:2099–2105. doi: 10.1200/JCO.2007.13.3934. [DOI] [PubMed] [Google Scholar]
- 27.Di Paolo A, Lencioni M, Amatori F, et al. 5-fluorouracil pharmacokinetics predicts disease-free survival in patients administered adjuvant chemotherapy for colorectal cancer. Clin Cancer Res. 2008;14:2749–2755. doi: 10.1158/1078-0432.CCR-07-1529. [DOI] [PubMed] [Google Scholar]


