Abstract
Pheochromocytoma during pregnancy is potentially disastrous to the mother and fetus. Its ambiguous presentation is often mistaken for pre-eclampsia, although it may imitate other problems during pregnancy. Early diagnosis and timely, appropriate management reduces possible maternal and fetal complications. We identified a case of pheochromocytoma during pregnancy; the condition was initially diagnosed as pre-eclampsia complicated with gestational diabetes. Surgical intervention via left adrenalectomy was successfully performed in the second trimester. After surgery, all of the patient’s medical problems nearly subsided and she did not require further treatment. However, her fetus displayed restricted intrauterine growth, and the patient eventually had premature delivery via a caesarean section. A multidisciplinary team to identify and treat pheochromocytoma is mandatory to ensure optimal conditions for tumour removal and to anticipate any possible catastrophic events.
Keywords: gestational diabetes, gynaecologic oncology, hypertension, pheochromocytoma, pregnancy, proteinuria
Introduction
Hypertension in pregnancy is a common condition, and pre-eclampsia is the most common problem in primigravidae. Severe cases of pre-eclampsia may be symptomatic and cause significant maternal and fetal complications that require delivery of the fetus and placenta as an ultimate treatment.
Pheochromocytoma is a catecholamine-secreting tumour that is rare during pregnancy, with the prevalence of 1 in 54 000 pregnancies (1). Recognising pheochromocytoma antenatally is difficult because it may mimic pre-eclampsia and other problems during pregnancy. Therefore, the management of pheochromocytoma is a great challenge to healthcare providers. Failure to diagnose the disease and delays in providing necessary treatments may cause fatality and life-threatening situations for the mother and the fetus (2). However, pheochromocytoma is curable by removing the tumour. The ability to accurately identify pheochromocytoma during the antenatal period with timely and appropriate management reduces maternal mortality and fetal loss (1,3,4). In the current report, we discussed a case of pheochromocytoma that was diagnosed during pregnancy and the complexity of its management.
Case Report
A 29-year-old Malay woman (gravida 2, para 0 + 1) presented at 21 weeks of amenorrhea (POA) with uncontrolled hypertension and proteinuria. She was newly diagnosed with gestational diabetes mellitus with no prior medical illnesses. She remained asymptomatic but had episodes of palpitations. Her blood pressure (BP) was labile with episodes of tachycardia during admission. The first impression of this case was a pregnancy with pre-eclampsia. However, the differential diagnosis of pheochromocytoma was suspected based on the evidence of labile BP and difficult-to-control hypertension that was associated with tachycardia.
Further physical examinations revealed a pale woman with BP ranging 100–203 mmHg (systolic BP) and 73–120 mmHg (diastolic BP) with episodes of tachycardia. Her weight and height were 37 kg and 161 cm, respectively. No goitre was detected. Her pregnancy was grossly normal, and ultrasound scan parameters corresponded to the estimated dates (approximately 20 weeks of gestation).
She developed acute renal failure with worsening complications that were associated with gestational diabetes requiring insulin treatment. The highest serum creatinine level was 148 μmol/L, and the renal failure was eventually resolved with rehydration. Although her haemoglobin level was 7 g/dL, there was no evidence of occult bleeding. Left ventricular hypertrophy with diastolic dysfunction was evident from echocardiogram. Her thyroid function tests were normal. The 24-hour urine catecholamine test revealed elevations of noradrenaline at 1075 μg (normal range 12.1–85.5 μg) and adrenaline at 196 μg (normal range 1.7–22.4 μg). The abdominal MRI confirmed the presence of a left adrenal tumour that was 4.9 × 5.7 × 7.5 cm (Figure 1).
Figure 1:
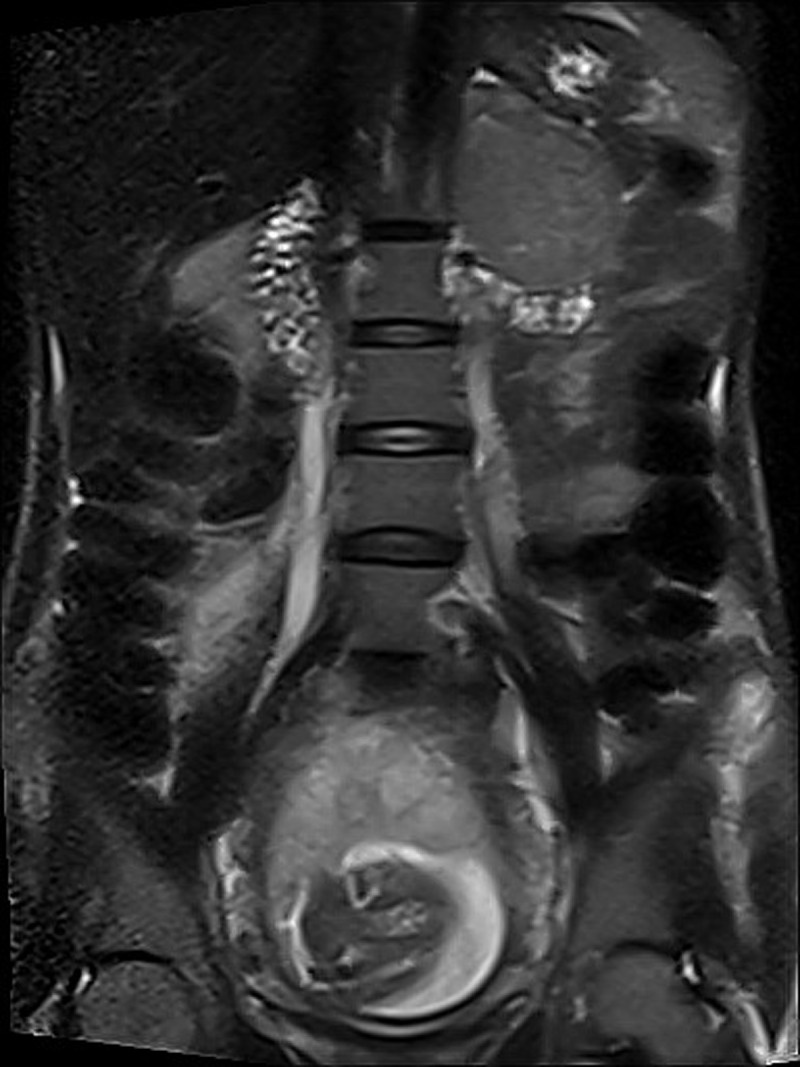
Sagittal section of T2-weighted magnetic resonance image showing the left adrenal pheochromocytoma and a fetus.
A multidisciplinary team consisting of obstetricians, endocrinologists, endocrine surgeons, and anaesthetists was involved in treatment management. Controlling the patient’s BP was difficult because the BP remained labile. The treatment consisted of numerous antihypertensives, such as prazosin (20 mg once daily), labetalol (300 mg thrice daily), metoprolol (200 mg twice daily), bisoprolol (10 mg twice daily), and felodipine (10 mg once daily). Magnesium sulphate and phenoxybenzamine at 40 mg once daily were used to prepare for surgery. Fluid replacement and blood transfusions were provided during the management of the patient’s labile BP and resulted in recurrent pulmonary oedema that required admission to the intensive care unit.
The patient’s condition was acceptable at 24 weeks POA to perform an open left adrenalectomy. While anaesthesia was provided, her BP surged to 340/230 mmHg, which was successfully controlled by infusing glyceryl trinitrate and sodium nitroprusside. After the removal of the tumour (Figure 2), the lowest recorded BP was 70/40 mmHg. The patient was normotensive after 2 hours of noradrenaline infusion
Figure 2:

A section of the dissected left pheochromocytoma (70 × 40 × 20 mm).
Post-operatively, the patient’s BP was controlled with low doses of an antihypertensive agent, with normalisation of urine catecholamine levels. The patient and her fetus were in good health, although the fetus experienced intrauterine restricted growth, which was most likely attributed to all of the patient’s complications. Her pregnancy was monitored through outpatient antenatal visits. After the surgery, she gained 11 kg. Her hypertension and diabetes had improved and required no medication. In the 27 weeks POA, the growth of her fetus was below the 5th centile. The Doppler study of the umbilical artery flow was normal until 37 weeks POA. Then, an emergency caesarean section due to fetal distress was performed.
The surgery was successful and a baby boy was delivered, weighing 1.86 kg. The neonatology review was satisfactory. Her post-partum period was uneventful, with normal results for the modified glucose tolerance test.
Discussion
The classical presentation of pheochromocytoma with paroxysmal hypertension, headaches, sweating, and palpitation (5,6) may not be simultaneously present, especially during pregnancy. Therefore, the initial diagnosis of hypertension during pregnancy is frequently attributed to pre-eclampsia rather than pheochromocytoma (5,7). Our patient presented with hypertension and proteinuria at 21 weeks POA. At this time, we made the most appropriate diagnosis, especially for a pseudo-primigravida. Excess weight and increased weight gain during pregnancy predisposed women to pre-eclampsia, although sudden weight gain is rarely seen in pheochromocytoma (5). This patient was underweight at the start of her pregnancy. However, her weight increased after the adrenalectomy. Weight loss in pheochromocytoma is due to catecholamineinduced hypermetabolism, which might be the reason for the patient’s low weight before surgery and subsequent weight gain after surgery with normalisation of catecholamine levels (6).
In addition to hypertension, altered renal function and proteinuria are caused by catecholamine-mediated renovascular abnormalities, which is common in pheochromocytoma (7). Some of the reported cases may display hyperglycaemia and had been treated as gestational diabetes (5,7,8), which was evident in this case. Episodic hyperglycaemia is most likely due to the effect of adrenalinesecreting pheochromocytoma. These data explained the initial misdiagnosis of this patient. Pheochromocytoma was suspected when the BP became labile and difficult to control, with episodic tachycardia. Pheochromocytomaassociated syndromes, such as medullary thyroid carcinoma, are currently being investigated in this patient, although she did not have any goitre. Further investigation for medullary thyroid carcinoma was not undertaken when she was initially admitted because her condition was not stable and she was pregnant.
Pregnancy itself would reveal the underlying pheochromocytoma through the enlarging uterus, changes of intra-abdominal pressure during fetal movements, compression of the growing tumour by pregnancy, stressful conditions related to delivery and anaesthesia that could have resulted in the release of catecholamines. The suspicion of pheochromocytoma in pregnancy, which was indicated by labile BP and difficulty in controlling hypertension, can direct the appropriate investigation to lead to an early diagnosis (7,8). Meanwhile, pulmonary oedema (6) may further complicate the management of this delicate hypertensive problem. The detection of high 24-hour urine catecholamine levels (2,9) and the imaging of the adrenal mass using magnetic resonance imaging (MRI), which is safe for the fetus as it requires no radiation, were used to diagnose pheochromocytoma in this patient and were the tools that were consistent with previous reports (2,5). Conversely, the ultrasound scan was reported to have poor sensitivity, especially during the 3rd trimester (2).
Because the disease was diagnosed at 22 weeks of gestation in this patient, the fetus was still developing. The fetal growth was restricted to lower than the 5th centile until 37 weeks. Similar cases of intrauterine restriction (8,10) have been reported and may be explained by the excessive production of catecholamines. Although catecholamines do not cross the placenta, the utero-placental insufficiency can occur through maternal vessels with the paroxysmal reduction and increment in blood pressure that may worsen intrauterine hypoxia.
The timing of the surgery is controversial and requires consideration on an individual basis. Surgery is less preferred during the 1st trimester due to the higher incidence of miscarriages. Adrenalectomy is recommended for 2nd-trimester cases. In the 3rd trimester, the surgery is delayed or often performed during caesarean section (6). General anaesthesia is preferred and recommended because most of the anaesthetic gases are safe for fetuses, except for halothane and desflurane (5). Although this is a definitive treatment, medical preparation is essential and can be achieved by using alpha-blockers (prazosin and phenoxybenzamine), beta-blockers, and other drugs, such as magnesium sulphate. Magnesium sulphate is beneficial in the management of pre-eclampsia and pheochromocytoma. In pre-eclampsia, magnesium sulphate reduces the BP and acts to prevent eclampsia. In pheochromocytoma, magnesium sulphate inhibits catecholamine release from the tumour, blocks peripheral catecholamine receptors, and is a direct vasodilator (7). Almost every report of pheochromocytoma in pregnancy has diligently stressed the importance of correctly balancing vasodilatation and vasoconstriction to optimise the mother’s condition and prevent fetal demise (5). Methyldopa, which is frequently used for hypertension during pregnancy, may worsen the symptoms of pheochromocytoma (5).
Diabetes, hypertension, and proteinuria in our patient were almost completely resolved after the adrenalectomy and are similar to the results that have been previously described (5,7). The ultimate aim was to prevent a hypertensive crisis (7) that is predictably disastrous to the mother and fetus. Utero-placental insufficiency affected the growth of fetus in this case. However, the fetus continued growing at the 5th centile. A caesarean section was performed due to fetal distress.
In conclusion, the commitment of a multidisciplinary team is of utmost importance, and individual patient consideration is essential during the management of this dangerous condition.
Footnotes
Authors’ Contribution
Conception and design, collection, assembly, analysis, and interpretation of the data, drafting of the article: MINA
Provision of patient, critical revision and final approval of the article: MINA, ARR, AWN, MR, NAK
References
- 1.Ahlawat SK, Jairi S, Kumari S, Varma S, Sharma BK. Pheochromocytoma associated with pregnancy: Case report and review of the literature. Obstet Gynecol Surv. 1999;54(11):728–737. doi: 10.1097/00006254-199911000-00025. [DOI] [PubMed] [Google Scholar]
- 2.Sarathi V, Lila AR, Bandgar TR, Menon PS, Shah NS. Pheochromocytoma and pregnancy: A rare but dangerous combination. Endocr Pract. 2010;16(2):300–309. doi: 10.4158/EP09191.RA. [DOI] [PubMed] [Google Scholar]
- 3.Wattanachanya L, Bunworasate U, Plengpanich W, Houngngam N, Buranasupkajorn P, Sunthornyothin S, et al. Bilateral pheochromocytoma during the postpartum period. Arch Gynecol Obstet. 2009;280(6):1055–1058. doi: 10.1007/s00404-009-1057-5. [DOI] [PubMed] [Google Scholar]
- 4.Mannelli M, Bemporad D. Diagnosis and management of pheochromocytoma during pregnancy. J Endocrinol Invest. 2002;25(6):567–571. doi: 10.1007/BF03345503. [DOI] [PubMed] [Google Scholar]
- 5.Oliva R, Angelos P, Kaplan E, Bakris G. Pheochromocytoma in pregnancy: A case series and review. Hypertension. 2010;55(3):600–606. doi: 10.1161/HYPERTENSIONAHA.109.147579. [DOI] [PubMed] [Google Scholar]
- 6.Grodski S, Jung C, Kertes P, Davies M, Banting S. Phaeochromocytoma in pregnancy. Intern Med J. 2006;36(9):604–606. doi: 10.1111/j.1445-5994.2006.01132.x. [DOI] [PubMed] [Google Scholar]
- 7.Huddle KR, Nagar A. Phaeochromocytoma in pregnancy. Aust N Z J Obstet Gynaecol. 1999;39(2):203–206. doi: 10.1111/j.1479-828x.1999.tb03374.x. [DOI] [PubMed] [Google Scholar]
- 8.George J, Sarathi V, Bandgar TR, Menon PS, Shah NS. Pregnancy and pheochromocytoma: A dangerous liaison. Endocrinologist. 2010;20(2):58–59. [Google Scholar]
- 9.Kondziella D, Lycke J, Szentgyorgyi E. A diagnosis not to miss: Pheochromocytoma during pregnancy. J Neurol. 2007;254(11):1612–1613. doi: 10.1007/s00415-007-0605-9. [DOI] [PubMed] [Google Scholar]
- 10.Kennelly MM, Ball SG, Robson V, Blott MJ. Difficult alpha-adrenergic blockade of a phaeochromocytoma in a twin pregnancy. J Obstet Gynaecol. 2007;27(7):729–730. doi: 10.1080/01443610701667049. [DOI] [PubMed] [Google Scholar]


