Abstract
We present a case of Loa loa infection in a patient, 21 years after visiting an endemic area for only 4 days. To our knowledge, this case represents the longest time for the diagnosis of loiasis to be made post-exposure in a traveler and emphasizes that even short exposures can place travelers at risk.
Case Report
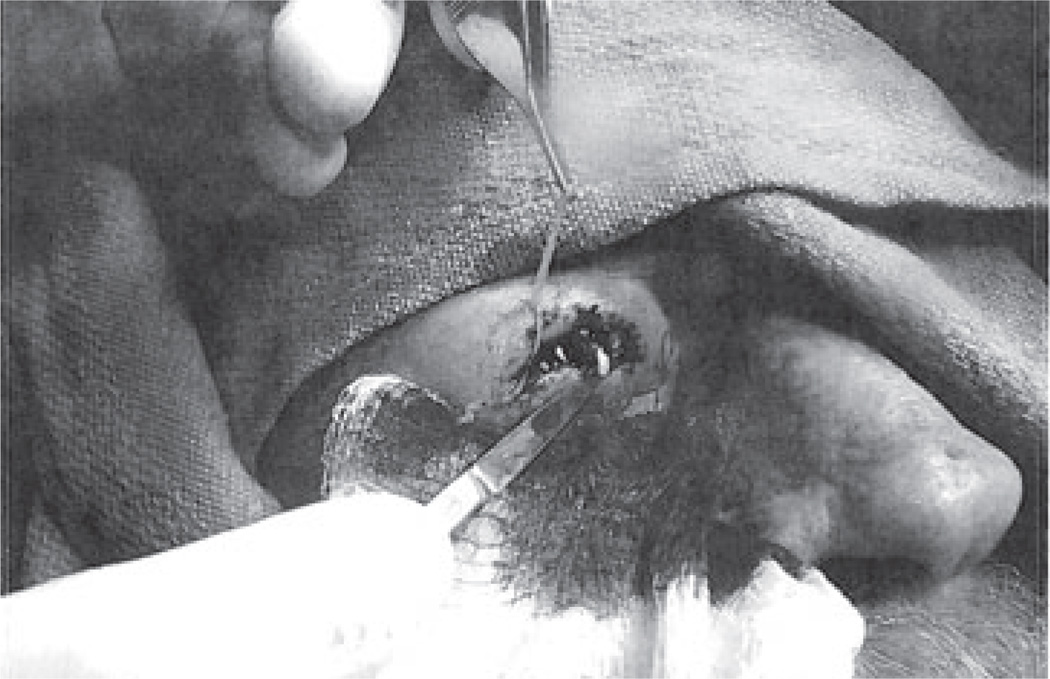
A 60-year-old man was referred to one of the authors (M. B.) after his dermatologist (J. K. G.) extracted a filamentous round worm from a right upper eyelid swelling (Figure 1). The patient had been experiencing migratory facial edema for the past 2 years. He had visited various physicians during that time period to evaluate transient swellings on the side of his nose, left eyebrow, and right cheek.Workup included a CT scan of the orbits, and an MRI brain—both of which were unrevealing except for a right lacrimal gland swelling on the MRI reported as “suspicious for lymphoma.” Three biopsies were performed prior to consultation, and no evidence of lymphoma or granulomatous disease was identified. The patient was told that these swellings could be a reaction to the facial surgery he had prior to becoming symptomatic.
Figure 1.
Extraction of worm.
The medical history was significant for hypertension, Gleason 6 prostate cancer, and a rhytidectomy (face lift) 10 years ago. Medications included an aspirin (81 mg) and olmesartan–hydrochlorothiazide. Social history was negative for alcohol abuse or tobacco. Although the patient had an extensive travel history throughout Europe, Asia, and South America, the case is notable in that he had only visited sub-Saharan Africa once: In 1989, he traveled to Lagos, Nigeria for a 3-day business trip. He did not recall any unusual bites at that time and was in an urban setting at all times during the travel.
The physical examination was unremarkable for further tissue swellings. In addition, there were no stigmata of chronic lymphedema or organomegaly. The rest of the examination was normal. The white blood cell count was 7,200 cells/microliter with 210 absolute eosinophils. Testing for peripheral blood microfilariae was negative. The IgE level was within the normal reference range, and the urinalysis was unremarkable. Serologies were not performed since we were able to send the worm for a definitive PCR diagnosis. Chest X-ray revealed pleural plaques and rounded multifocal opacities that were deemed on PET scan to be the sequelae of prior asbestos exposure.
Review of formalin-fixed, paraffin-embedded tissue sections from multiple biopsies from the patient’s neck, right inner cheek, forehead, and right eyelid between March 2009 and May 2010 demonstrated patchy lymphocytic infiltrates, sometimes extending into the subcutaneous fat with occasional multinucleated giant cells and areas of necrosis. No prominent eosinophilic infiltrates were seen on any of the biopsies.
A white roundworm measuring approximately 6.5 cm in length and 0.2 cm in diameter was removed from the right eyelid during an acute episode of periorbital edema (Figures 1 and 2). Real-time PCR for Loa loa was performed at the NIAID Laboratory of Parasitic Diseases, Bethesda, MD, using a recently described L loa-specific assay.1 The PCR assay is highly specific for L loa and fails to amplify DNA from Onchocerca volvulus, Mansonella perstans, Wuchereria bancrofti, and Brugia malayi. It can detect as little as 0.1 pg of L loa genomic DNA. Two duplicate reactions were performed, and both samples were positive.
Figure 2.
Worm identified as Loa loa.
The patient was treated with single-dose diethylcarbamazine (DEC; 6 mg/kg) due to his preference for single dose therapy over the traditional longer course of therapy. We were able to prescribe a full dose on the first day of treatment, as the patient had no detectable microfilaremia. He has been asymptomatic for nearly a year since the removal of the worm, and he had no post-treatment reactions to the single-dose DEC.
Discussion
L loa, also known as the African eye worm, is a filarial parasite that is transmitted through the bite of the deerfly, Chrysops; it is endemic to Central and West Africa. After a bite from an infected fly, larvae penetrate the skin of the host and develop into adult worms over a period of 4–6 months.2 Female worms produce thousands of microfilariae that circulate in the blood with a diurnal periodicity.2 The life cycle is completed when the microfilaria are taken up by the day-biting female Chrysops. Expatriates infected with this organism commonly develop pruritis, creeping dermatitis, and transient migratory facial and extremity angioedema known as Calabar swellings (named after the coastal Nigerian town where they were first recorded).3 These result from the migration of the worm through subcutaneous tissues.Other pathological manifestations include subconjunctival migration of worms, eosinophilia, elevated IgE, and, to a lesser extent, nephropathy, cardiomyopathy, retinopathy, arthritis, peripheral neuropathy, and lymphadenitis.4–7
The disease is a relatively rare entity in travelers in large part because of the restricted geographic niche L loa occupies and the oft-needed long-term exposure for acquisition.5,6 Most travel physicians do not consider short stays—even in endemic areas—to be high risk. Travelers that do become infected present with a greater predominance of allergic symptoms, frequently recurring episodes of angioedema, and striking peripheral eosinophilia. DEC is the treatment of choice for patients with loiasis; other options include albendazole and ivermectin. One must be cautious, however, in patients with high microfilarial burdens; treatment can precipitate encephalitis. Plasmapheresis and/or steroids are often considered in such cases.7
The patient’s presentation is notable for several reasons. First, the length of time between his probable inoculation and his becoming clinically symptomatic was ~20 years. (Much of the literature cites a maximum lifespan of around 15 y.)8 Secondly, loiasis is more common in individuals who have had extended exposure to infected Chrysops.9 Our patient recounted only a single 3-day visit to an endemic area. Thirdly, the patient’s lack of peripheral eosinophilia as well as a normal IgE level probably reflects the chronicity of the infection and the modulation of the acute responses that often occur early in infection. Lastly, the use of molecular approaches toward definitive speciation of a viable worm extracted from the patient 20 years after exposure suggests that in some cases L loa has an extremely extended lifespan. It is worth emphasizing that the molecular assay used to confirm the diagnosis is not cross-reactive with M perstans,1 which is endemic to areas in this patient’s travel history and may be associated with symptoms and periorbital migration similar to L loa.
The GeoSentinel Surveillance Network examined their database to identify demographic and travel characteristics associated with filarial species and L loa acquisition.6 From a total of 43,722 individual patient encounters over 7 years at travel clinics geographically dispersed, filarial infections were diagnosed in 269 (0.62%), of which ~25% were infected with L loa. Among the 16 travelers (not those born in Loa-endemic regions) with loiasis, only 2 (12.5%) had stays less than 30 days. This case is unusual and should remind the travel practitioner to take a detailed travel history in the setting of swelling and/or angioedema and not be dissuaded by the lack of eosinophilia on presentation or a prolonged interval between possible exposure and clinical presentation of L loa.
Acknowledgment
We would like to thank Ms Audrey Cantley for administrative assistance.
Footnotes
Declaration of Interests
The authors state they have no conflicts of interest to declare.
References
- 1.Fink DL, Kamgno J, Nutman TB. Rapid molecular assays for specific detection and quantitation of Loa loa microfilaremia. PLoS Negl Trop Dis. 2011;5:e1299. doi: 10.1371/journal.pntd.0001299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brumpt EJA. La Filaria loa, Guyot, est la forme adulte de la microfilaire désignée sous le nom de Filaria diurna Manson. Comp Rend Soc Biol Paris. 1904;56:630–632. [Google Scholar]
- 3.Manson P. On the nature and origin of Calabar swellings. Tr R Soc Trop Med Hyg Lond. 1910;3:244–256. [Google Scholar]
- 4.Rakita RM, White AC, Jr, Kielhofner MA. Loa loa infection as a cause of migratory angioedema: report of three cases from the Texas Medical Center. Clin Infect Dis. 1993;17:691–694. doi: 10.1093/clinids/17.4.691. [DOI] [PubMed] [Google Scholar]
- 5.Nutman TB, Miller KD, Mulligan M, Ottesen EA. Loa loa infection in temporary residents of endemic regions: recognition of a hyper-responsive syndrome with characteristic clinical manifestations. J Infect Dis. 1986;154:10–18. doi: 10.1093/infdis/154.1.10. [DOI] [PubMed] [Google Scholar]
- 6.Lipner EM, Law MA, Barnett E, et al. Filariasis in travelers presenting to theGeoSentinel Surveillance Network. PLoS Negl Trop Dis. 2007;1:e88. doi: 10.1371/journal.pntd.0000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boussinesq M. Loiasis. Ann Trop Med Parasitol. 2006;100:715–731. doi: 10.1179/136485906X112194. [DOI] [PubMed] [Google Scholar]
- 8.Gems D. Longevity and ageing in parasitic and free-living nematodes. Biogerontology. 2000;1:289–307. doi: 10.1023/a:1026546719091. [DOI] [PubMed] [Google Scholar]
- 9.Klion AD, Massougbodji A, Sadeler BC, et al. Loiasis in endemic and nonendemic populations: immunologically mediated differences in clinical presentation. J Infect Dis. 1991;163:1318–1325. doi: 10.1093/infdis/163.6.1318. [DOI] [PubMed] [Google Scholar]