Abstract
Background:
Hypertension in diabetes is a common and important problem, which aggravates diabetic macro- and microvascular complications. Since both diabetes and hypertension are common diseases, their follow up in primary health care centers should emphasize the early detection of hypertension in diabetes. This study aims at studying the magnitude of hypertension in diabetic subjects registered in primary health care centers.
Methods:
A sample of 1039 diabetic subjects registered at the primary health care in urban and rural Makkah region were interviewed. Information gathered included demographic and diabetes-related variables. Blood pressure and body mass index were determined for 1020 subjects.
Results:
Diabetic subjects who had high blood pressure readings amounted to 560 (54.9%), of whom with stage 1, 2, and 3 hypertension formed 25.5%, 7.0% and 2.5%, respectively. Subjects with undetected high blood pressure amounted to 225 (22.1%). There was significant association of high blood pressure with age, male gender, body mass index and low education.
Conclusion:
The problem of hypertension in diabetes could be sizeable. Many patients may remain undetected. A diligent search for diabetic subjects with elevated blood pressure should be made through an efficient system of follow up in the PHCC centers.
Keywords: Diabetes mellitus, Hypertension, Primary Health Care Centers
INTRODUCTION
Hypertension in diabetes is a common problem.1 In insulin dependent diabetes mellitus (IDDM) the condition is common in subjects with diabetic nephropathy.2 However, in non-insulin dependent diabetes (NIDDM) it is even more common, and is invariably associated with obesity.3 As in the case of essential hypertension, hypertension complicating diabetes mellitus represents a strong risk factor for cardiovascular complications, and aggravates the micro- and macrovascular complications of diabetes mellitus.4,5 Hypertension is also twice as common in diabetic than in non-diabetic subjects. Unlike the case of IDDM, hypertension associated with NIDDM may be present at the time of diagnosis of diabetes. This is because, in a considerable number of individuals, the two diseases may have common underlying mechanisms.6 Hypertension in diabetes is also associated with all the behavioral problems encountered with essential hypertension, such as unawareness, and non-compliance with drugs and non-drug management. Since both diabetes and hypertension are common problems in Saudi Arabia, it is important to shed some light on the problem of hypertension in diabetes. Both conditions are being mostly managed in the primary health care (PHCC) centers. This study aims to study the magnitude of the problem of hypertension in diabetes among diabetic subjects cared for in PHCC centers.
MATERIAL AND METHODS
The study population were adult diabetic subjects at the age of 15 years or more, who had had a confirmed diagnosis of diabetes mellitus for the last one year, and who were registered in the diabetic registries of the PHCC centers, in Makkah City, and in rural Makkah district during the year 1420H. (1999G.). There was a total of 11,614 diabetic subjects, 8,110 (70%), and 3504 (30%) of whom were registered in the urban and rural PHCC centers, respectively.
A two-stage stratified random sampling technique, with proportional allocation to choose about (10%) of diabetic subjects, from 9 urban and 12 rural PHCC, was adopted. In the first stage, simple random sampling technique was used to choose 9 urban and 12 rural PHCC. In the second stage, the sample of diabetic subjects from each chosen PHCC was also chosen, using simple random sampling.
Data were collected by pre-trained PHCC center physicians, using a structured questionnaire form. The questionnaire included socio-demographic data, such as age, sex, nationality, and educational level. Education level was categorized as low (primary and intermediate schooling), average (secondary schooling), and high (university and postgraduate). The questionnaire also included information regarding duration of diabetes mellitus, and the presence of hypertension. Diabetes mellitus was classified into type 1 and 2 according to whether the patient was being treated with insulin or oral hypoglycemic drugs, respectively. Measurement of weight in kilograms, and height in meters was done and body mass index (BMI) was calculated as weight in kilograms divided by the square of the height in meters. A BMI of more than 25 kilograms/ square meter was considered as high. Blood pressure measurement was done using a mercury sphygmomanometer with a suitable cuff size while the patient was seated and systolic (SBP), and diastolic blood pressure (DBP) were recorded at the onset and disappearance of Kortokoff's sounds, respectively. Blood pressure was classified as normal (SBP < 130, DBP < 85 mmHg), high normal (SBP = 130-139, DBP = 85-89 mmHg), stage 1 (SBP = 140-159, DBP = 90-99 mmHg), stage 2 (SBP = 160-179, DBP = 100-109 mmHG) and stage 3 hypertension (SBP > 180, DBP > 110 mmHg); in accordance with criteria adopted by the Joint National Committee on Detection, evaluation and Treatment of High Blood Pressure.7
Data was analyzed using the Statistical Package for Social Science (SPSS PC) version 7.0. Chi-squared test was used to assess the significance of differences between categories. A p-value of 0.05 or less was considered statistically significant.
RESULTS
The study sample consisted of 1039 diabetic subjects. Males and females constituted 66.7% and 33.3% of the sample, respectively. The overall mean age was 54.6±12.6 years (55.6±12.9 and 52±11.8 years for males and females, respectively). The majority of subjects (93.7%) were of Saudi nationality.
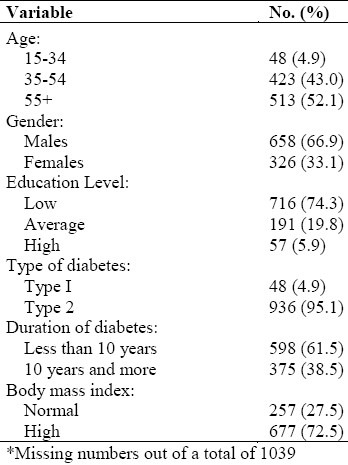
Subjects with type 2 diabetes mellitus constituted (95.1%), and almost two-thirds of these had had diabetes mellitus for less than 10 years. An abnormally high BMI was manifested by 72.4% of the sample (Table 1).
Table 1.
Demographic variables and disease pattern of diabetic subjects (N=984)*
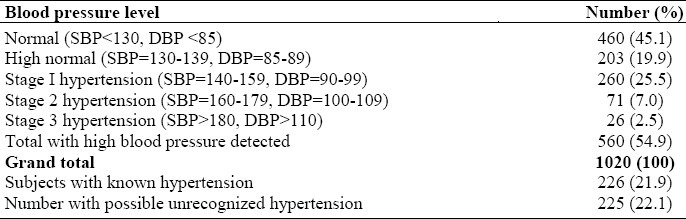
Blood pressure readings were obtained from 1020 subjects constituting 98.2% of the sample. A total of 560 (54.9%) subjects had high blood pressure readings, which were classified as high normal (19.9%), stage 1 hypertension (25.5%), stage 2 hypertension (7.0%), and stage 3 hypertension (2.5%). The number of subjects with unrecognized high blood pressure was 225 (22.1%) (Table 2)
Table 2.
Blood pressure level distribution among 1020 diabetic subjects
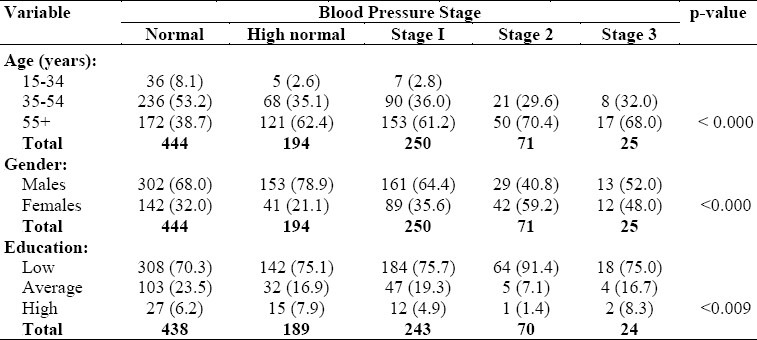
There were significant increases in the proportions of patients at all stages of high blood pressure, with increasing age (P < 0.0001), male gender (P < 0.0001), and with low educational level (P < 0.0001) (Table 3).
Table 3.
Blood pressure level distribution according to age, gender and education level
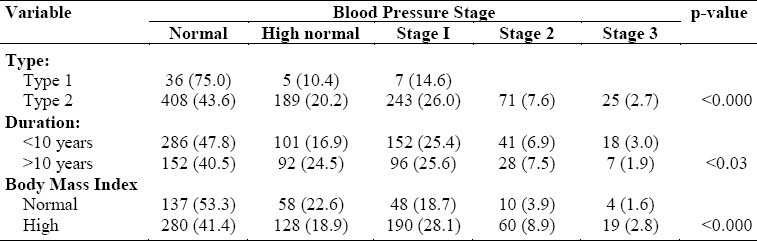
However, there was significantly higher incidence of all stages of high blood pressure (P < 0.0001, and P < 0.0001, respectively) in subjects with type 2 diabetes mellitus, and those with a high BMI. As regards the duration of diabetes, significantly more subjects who had had high blood pressure for less than 10 years at all stages of hypertension were observed (Table 4).
Table 4.
Blood pressure level distribution according to type, duration of diabetics and body mass index
DISCUSSION
Hypertension in diabetes implies a state of high risk of cardiovascular mortality;8 hence its detection, evaluation and effective management cannot be overemphasized. The prevalence of diabetes-related hypertension detected by this study amounts to 55% of the sample, with moderate to severe forms reaching 10%. This figure is high and is in agreement with similar figures cited in the literature.9,10 Moreover, the finding is significant in that both diabetes mellitus and hypertension are risk factors for cardiovascular diseases, and strong predisposing factors for renal disease. Consequently, no effort should be spared in the detection and management of hypertension associated with diabetes.11 It may be necessary to adopt the guidelines given by the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure which advocates that the management of patients with diabetes and hypertension should be carried out as if they were suffering from end-organ damage.12 The distribution of high blood pressure described by this study reveals that the majority of subjects have mild blood pressure elevation, together with high body mass index. This finding is significant since subjects with this degree of blood pressure remain asymptomatic. It is important, therefore, that effective methods be employed for their detection and evaluation, so that the modification of lifestyle could commence early.13
The figures shown in this study were based on casual blood pressure measurement, so it is expected that a proportion of the subjects affected might have White Coat Hypertension.14 A meticulous follow up is necessary, so that proper evaluation and further intervention could be undertaken.
Almost 50% of subjects with high blood pressure in this study were not aware of this. This figure is higher than that cited by other researchers,15 and reflects the quality of care that those subjects receive. Moreover, it again stresses the need for the employment of effective methods of early detection of high blood pressure. This could be achieved by training PHCC centers physicians on blood pressure audit.
The study also reveals an expected positive association of high blood pressure with age, gender and BMI, a finding that agrees with the results of other studies.16,17 The study which supports similar findings in the Arabian Gulf Region reveals an inverse relationship of high blood pressure with educational level18 This can be accounted for as a marker of early-life socioeconomic deprivation induced by environmental factors as has been suggested.18 It may also reflect the inadequate functional health literacy,19 on the one hand, and the lack of health education needed for control of diabetes and hypertension20 on the other hand.
In conclusion, this study reveals that the problem of hypertension in diabetes may be sizable, and that many patients may remain undetected. The findings call for a diligent search for diabetic subjects with elevated blood pressure, through an efficient system of follow up in the PHCC centers.
REFERENCES
- 1.Hypertension in Diabetes Study Group. Hypertension in diabetes study (HDS): 1. prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complications. J Hypertension. 1993;11:309–17. doi: 10.1097/00004872-199303000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Reavan GM, Lithell H, Landsberg L. Hypertension and associated metabolic abnormalities - the role of insulin resistance and the sympathoadrenal system. N Engl J Med. 1996;334:374–81. doi: 10.1056/NEJM199602083340607. [DOI] [PubMed] [Google Scholar]
- 3.Norgaard K, Rasmussen E, Jenssen T, Feldt-Rasmussen B. Nature of elevated blood pressure in normoalbuminuric type 1 diabetic patients. Essential hypertension? Am J Hypertens. 1993;6:830–6. doi: 10.1093/ajh/6.10.830. [DOI] [PubMed] [Google Scholar]
- 4.Sowers JR, Epstein M. Diabetes mellitus and associated hypertension, vascular disease, and nephropathy. Hypertension. 1995;26:869–79. doi: 10.1161/01.hyp.26.6.869. [DOI] [PubMed] [Google Scholar]
- 5.Cignarelli M, De Cicco ML, Damato A, et al. High systolic blood pressure increases prevalence and severity of retinopathy in NIDDM patients. Diabetes Care. 1992;15:1002–8. doi: 10.2337/diacare.15.8.1002. [DOI] [PubMed] [Google Scholar]
- 6.Zimmet P, Boyko EJ, Collier GR, de Courten M. Etiology of the metabolic syndrome: potential role of insulin resistance, leptin resistance, and other players. Ann N Y Acad Sci. 1999;892:25–44. doi: 10.1111/j.1749-6632.1999.tb07783.x. [DOI] [PubMed] [Google Scholar]
- 7.Joint National Committee. The sixth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI) Arch Intern Med. 1997;157(21):2413–24. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 8.Jamerson KA. Treating high-risk hypertensive patients. Am J Hypertens. 2000;13:68S–73S. doi: 10.1016/s0895-7061(00)00270-3. [DOI] [PubMed] [Google Scholar]
- 9.Sugarman JR. Prevalence of diagnosed hypertension among diabetic Navajo Indians. Arch Intern Med. 1990;150(2):359–62. [PubMed] [Google Scholar]
- 10.Le Floch JP, Thervet F, Desriac I, Boyer JF, Simon D. Management of diabetic patients by general practitioners in France 1997: an epidemiological study. Diabetes Metabol. 2000;26(1):43–9. [PubMed] [Google Scholar]
- 11.Bakris G, Sowers J, Epstein M, Williams M. Hypertension in patients with diabetes. Why is aggressive treatment essential? Postgrad Med. 2000;107(2):53–6. doi: 10.3810/pgm.2000.02.884. [DOI] [PubMed] [Google Scholar]
- 12.Elliot WJ, Weir DR, Black HR. Cost-effectiveness of the lower treatment goal (of JNC VI) for diabetic hypertensive patients. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 2000;160(9):1277–83. doi: 10.1001/archinte.160.9.1277. [DOI] [PubMed] [Google Scholar]
- 13.Julius S, Jamerson K, Mejia A, et al. The association of borderline hypertension with target organ changes and higher coronary risk. Tecumseh Blood Pressure study. JAMA. 1990;264:354–8. [PubMed] [Google Scholar]
- 14.Flores L, Recasens M, Gomis R, Esmatjes E. White coat hypertension in Type 1 diabetic patients without nephropathy. Am J hypertens. 2000;13:560–3. doi: 10.1016/s0895-7061(00)00232-6. [DOI] [PubMed] [Google Scholar]
- 15.Harris MI. Health care and health care status and outcomes for patients with type 2 diabetes. Diabetes Care. 2000;23(6):754–8. doi: 10.2337/diacare.23.6.754. [DOI] [PubMed] [Google Scholar]
- 16.Mason EE, Renquist K, Jiang D. Predictors of Two Obesity Complications: diabetes and hypertension. Obes Surg. 1992;2(3):231–7. doi: 10.1381/096089292765560105. [DOI] [PubMed] [Google Scholar]
- 17.Bone LR, Hill MN, Stallings R, Gelber AC, Barker A, Baylor I, et al. Community health survey in an urban African-American neighborhood: distribution and correlates of elevated blood pressure. Ethn Dis. 2000;10(1):87–95. [PubMed] [Google Scholar]
- 18.Al-Mahrous F, Al-Roomi K, McKeigue PM. Relation of high blood pressure to glucose intolerance, plasma lipids and educational status in an Arabian Gulf population. Int J Epidemiol. 2000;29(1):71–6. doi: 10.1093/ije/29.1.71. [DOI] [PubMed] [Google Scholar]
- 19.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 20.Bone LR, Renquist K, Jiang D. Predictors of Two Obesity Complications: diabetes and hypertension. Obes Surg. 1992;2(3):231–7. doi: 10.1381/096089292765560105. [DOI] [PubMed] [Google Scholar]


