Abstract
Background:
Referral between primary care and hospitals is of great importance for patient care and follow-up. This study was conducted because of the importance of the quality of referral letters and feedback reports.
Objectives:
To evaluate the quality of referrals from primary health care (PHC) centers to general hospital in four regions in Saudi Arabia.
Methods:
This was a cross-sectional study of a random sample of referrals from the PHC centers. The first sampling unit was the general hospitals to which the health centers refer. A random sample of health centers was then selected based on their distance from the hospitals. This was followed by randomly selecting 30 referrals from each health center. The referral letters and the corresponding feedback reports were then studied for quality by scoring the components of each. The data was entered in a personal computer using the Stat Pack Gold Statistical Package. The chi-square was used to compare the different scores across the regions and T-test was used to compare the cumulative scores.
Main outcome measures:
The quality of referral letters and feedback reports was defined according to the standardized components using a scoring system.
Results:
The most frequently mentioned items in the referrals were demographic data (100%), specialty referred to (93.3%) and reason for referral (82.7%). Other important items in the feedback reports including the name of the treating physician (81.8%), diagnosis (86.0%), and decision on follow-up (80%) were missing. The quality of referral letters was poor in 23%, with 81% as the corresponding figure for the feedback reports with some variation between the different regions.
Conclusions:
The quality of referral letters and feedback reports is poor and needs to be improved. This can be achieved through implementing the quality assurance programme.
Keywords: Referral letters, feedback reports, quality, primary care, Saudi Arabia
INTRODUCTION
Referral from primary care to hospitals is an important daily activity that safeguards good medical care to patients. The main objective of building and improving a referral system is to improve the quality of patient care.
Referral is a two-way communication process between primary care physicians and specialists in hospitals, both of whom have an important role to play. It is the responsibility of the primary care physician to convey a clear message about the need and reason(s) for referring a patient. On the other hand, the specialist in a hospital is responsible for conveying a clear feedback on his evaluation of the patient's condition and a plan of management. However, problems in the referral process arise from primary care or hospitals when the primary care physician fails to clarify the reason(s) for referral,1 or conveys inappropriate or incomplete information.2 The specialist may also not address the physician's reason for referral or may fail to communicate his finding to the referring physician.3
Several authors have stressed the importance of good referral letters as the best mode of transmitting information to promote the understanding of a problem or patient. This not only improves management, but also aids the appropriate use of resources.4–9
In Saudi Arabia, the referral system given to primary care physicians is based on clear guidelines detailing the referral process. This includes the use of a pre-designed standardized referral form with important relevant clinical and social information. However, a small scale study on referral letters in two health centers in Riyadh have shown the inadequacy of both referral letters as well as the feedback received from specialists.10 Thus, there is a need to explore further the practices within the referral system in Saudi Arabia further.
The current study is part of a national project undertaken to evaluate the quality of the referral system in Saudi Arabia. In this paper, we report the quality of referrals in four regions of the Kingdom.
METHODS
The study was conducted in four regions in Saudi Arabia (namely Riyadh, Gazan, Northern Region and Hail). These regions were chosen because of the assumed variation in many health service characteristics such as the total population served, the number of health centers and hospitals, geographic characteristics, and other facilities.
Sampling Procedures
The sampling units for the study were the general hospitals in the region. These hospitals were first listed in a stratified sampling frame based on bed capacity, as follows: large hospitals – more than 150 beds, medium hospitals – from 100-150 beds, small hospitals – less than 100 beds. A random sample from each stratum was chosen, using a lottery method. The final number of hospitals was: 3 hospitals each from Riyadh and Gazan, and 2 hospitals each from the Northern Region and Hail (there were no hospitals of 100-150 beds in these two regions).
The next step was the sampling of the health centers. First, the health centers referring patients to these hospitals were identified and numbered, and the distance from hospitals (in kilometers) specified. The health centers were stratified according to the distance from hospitals to study the effect of this on the process of referral. A sample of two health centers that were near and two distant health centers was taken randomly using the random tables after pre-pointing a random start. The total number of selected health centers was 39 centers (one health center from Hail was excluded because there was no record of referrals for the whole year).
Sampling of the referral letters
The selected health centers were visited and the referral records of one year were identified and numbered. Thirty referrals from each health center were then randomly selected using random tables, and the information gathered was recorded on pre-designed and tested data sheets. The data sheets included demographic data of the patient referred, place of referral, specialty to which he was referred and other items that reflect the quality of the referral letters.
Scoring of the referrals
The important items in the referral letter were identified and the investigator and two other experienced family physicians undertook the scoring for referrals from the health centers. The team assessed the quality of referral letters on the basis of the following scoring system: patient's age (not present=0, present=1), patient's sex (not present=0, present=1), present complaint (not specified=0, specified=1), duration of complaint (not mentioned=0, mentioned=1), physical examination (not present=0, present but not clear=0, present and clear=1), differential diagnosis (not mentioned=0, mentioned but not clear=0, mentioned and clear=1), name of the referring physician (not mentioned=0, mentioned but not clear=0, mentioned and clear=1), reason for referral (not specified=0, specified=1), specialty to which the patient was referred (not specified=0, specified=2), and date, file number, health center and hospital in the same way and legibility of writing (not legible=0, legible=1). This gave a total score of 14.
Scoring was also done for the feedback from hospitals according to the following manner: result of evaluation (not available=0, available and not clear=0, available and clear=1), name of the attending physician (not written=0, written and not clear=1, written and clear=2), decision on follow-up (not clear=0, clear=1), plan of management (not clear=0, clear=1), and recommendations to the referring physician (not clear=0, clear=1) final diagnosis, response to the questions of the PHC physician, physical examination and file number were scored in the same way. This gave a total score of 9 for the feedback from specialists.
Data analysis
The data were entered in a personal computer using the Statpack Gold Statistical Package. Chi-square test was used to compare the variables and the different scores of quality of referral letters in the different regions.
RESULTS
Of the 1060 referral letters with feedback reports studied, 1026 (97%) were suitable for the final analysis, 34 forms were found to be difficult to evaluate and were excluded.
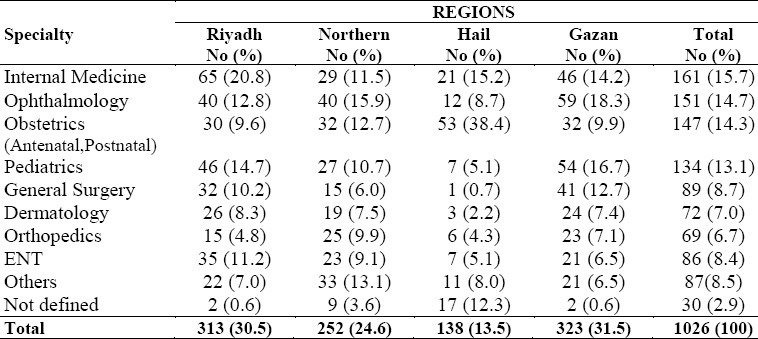
The specialists to whom the patients were referred from the primary care centers are presented in Table 1. The majority of patients were referred to General Medicine (15.7%), Ophthalmology (14.7%), Obstetrics and Gynecology (14.3%), and Pediatrics (13.1%). In a few of the referrals (2.9%) the specialty was not defined.
Table 1.
Specialties to which patients were referred in the different regions
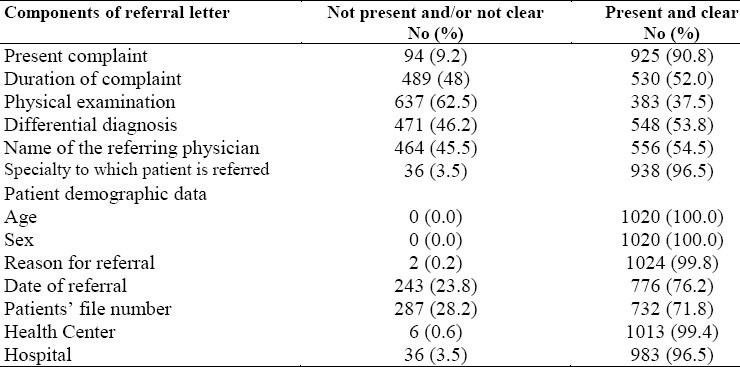
The frequency of important and relevant components of the referral letter is shown in Table 2. The most frequently mentioned items were age and sex (100%), the specialty to which the patient was referred (96.5%), the present complaint (90.8%) and reason for referral (99.8%). Important and relevant items such as duration of complaint, physical examination, name of the referring physician, and differential diagnosis were not mentioned or specified in 46% of the referral letters.
Table 2.
Frequency distribution of referral letters from health centers according to relevant items
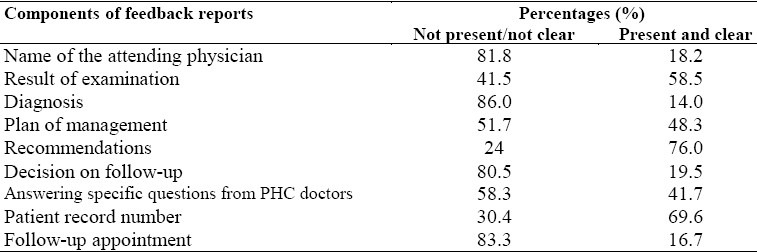
The most frequently mentioned components of the feedback report (from hospitals) were patient's record number (69.6%), recommendations to PHC physicians (76.0%), and result of examination (58.5%) (Table 3). Response to specific questions from PHC doctors was mentioned in only 41.7%. Other important items such as the name of the treating physician, diagnosis, decision on follow-up and arrangement for follow-up were mentioned in less than 20% of the reports.
Table 3.
Frequency of components of referral feedback reports
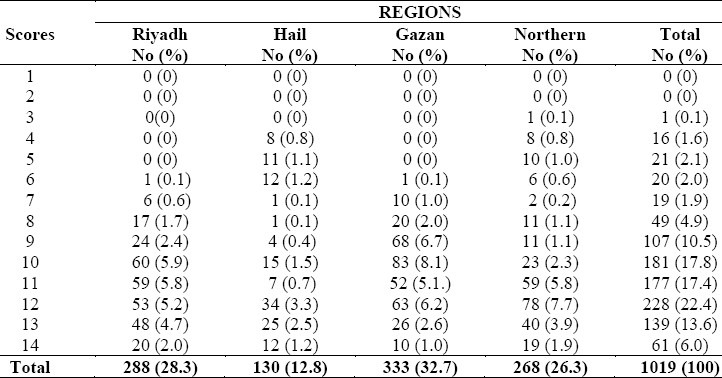
The frequency of scoring for the relevant items as components of referral letters is shown in Table 4. The mean score was 10.7 ± SD 2.2 and the majority were in the higher scores (more than 70% scored 10 or more).
Table 4.
Frequency of scores for the contents of referral letters by region (n=1019)
In Table 5, the scores for the relevant items of the feedback reports are shown. Only about half of the reports scored 5 or more of the scale (the mean score ± SD was 3.9 ± 2.1).
Table 5.
Frequency of scores for the components of feedback reports (n=896)
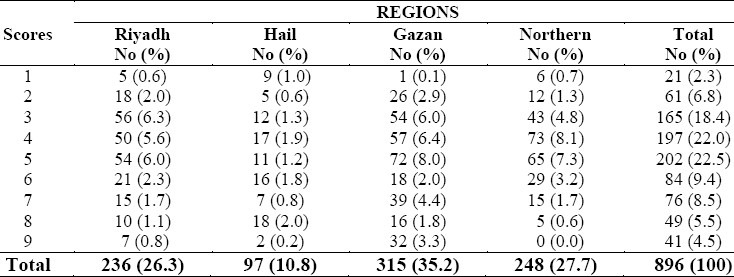
Assessment of the quality of referral letters and feedback reports based on the scores in different regions is shown in Table 6. The majority of letters (77.1%) were found to be of good quality (scored 10 or more). There was a significant difference between the regions. Riyadh and Northern regions were the best and Gazan was the worst (chi-square for trend = 18.95, p=0.0000).
Table 6.
Assessment of referral letters and feedback report according to the scores in different regions
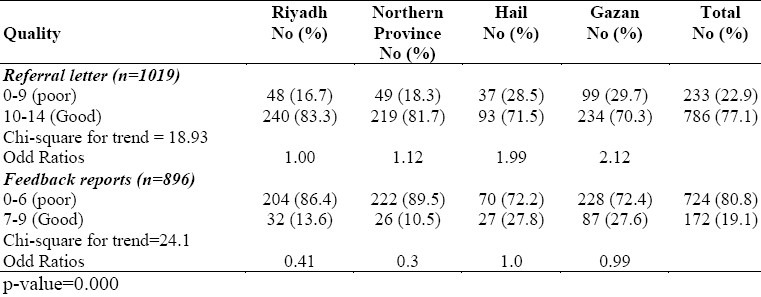
However, the quality of a vast majority (80.8%) of feedback reports was poor. There was a significant difference between the regions. Hail and Gazan were the best and the Northern region was the worst (chi-square for trend = 24.1, p=0.000).
DISCUSSION
The results of this study as reflected by the quality of the referral letters and feedback reports show that communication between the primary care physicians and specialists in hospitals is poor. The lack of basic clinical information such as duration of complaints, findings on clinical examination, and the like in the referral letter, is worrying. This observation which was documented in previous international8,11,12 and local studies,10,13 was found to be a major determinant of the quality of the process of referral and the feedback from the specialist.14 Taking into consideration the costly hospital consultations as compared to PHC, the “gate keeping” provided by primary health care should be efficient and cost-effective. This certainly should include providing the specialist in hospital with adequate clinical information about the patient, the initial evaluation of his condition, and the specific questions which need to be addressed.
The feedback from specialists to PHC doctors was found to be deficient in some respects. For example, there should be responses to the referring physician's questions and an indication of a clear and complete management plan to be followed. In this study, the specialists in hospitals did not address nearby 60% of the questions. Ignoring such questions widens the gap between the PHC physician and the specialist, and may endanger patient care.
It seems regrettable that a significant proportion (62%) of the letters and reports were not legible. Hardly any benefit can be derived from letters or reports that are illegible. Such letters will be ignored and new information about the patient's problem will be sought and workup done resulting in unnecessary waste of resources and time of both the PHC physician and the specialists in hospitals.
Both the PHC physicians and the specialists should recognize that referral is a bi-directional process which does not imply permanent transfer of responsibility for patient care to either party. It is obvious that inadequate or unclear information will affect the decision and the attitude of the recipient. Byrd and Moskwitz have reported that the overall satisfaction of the referring physician was dependent on the clarity and promptness of the consultant's reply, and on the clarity of his responses to specific questions.2
The educational benefits to the referring physician from referral needs some emphasis. The additional useful information provided to him helps him to improve the management of the referred patients, and improves the continuity of care. Poor quality feedback reports leaves the PHC physician with limited options on how to evaluate and manage the patient. The results of the referral also enable him to draw up an effective management plan. Not communicating these results to the PHC physician, has a negative effect on decision in future referrals. The referral threshold may increase to the detriment of the patient.
The very high rate of poor feedback reports (80%) is striking. Despite the fact that the facilities in hospitals are expected to be better than those in PHC, and the fact that the referral system has reduced the workload in hospitals,14 the specialists still do not seem to be aware of the importance of providing adequate information to PHC doctors, and the effect of this formation on patient care and its continuity. It is also possible that specialists consider referral as a permanent transfer of patient care and, consequently do not find it necessary to provide detailed information to the referring physicians. The referral system and the patient's care at large would benefit if this situation is clarified in formal administrative meetings in the hope of opening up communication channels between PHC doctors and hospital staff. Standardization of the referral forms was recommended by a group of general practitioners in a previous study.15 It is interesting to note that although the referral forms in the present study were standardized, this did not guarantee good quality of the contents of the letters and reports. The problem faced may reflect the attitude of the physicians rather than their knowledge about the components of a standard referral letter or feedback report.
The variation between the regions as regards the overall quality of referral letters is noteworthy. There were fewer letters and reports suitable for analysis from Hail region, and there were more poor quality letters from Hail and Gazan than from other regions. Gazan is remote, densely populated and has the highest workload (consultation load) among the regions under study but Hail is the reverse, which means that little effort is done to maintain quality referrals in Hail region.
One possible solution for this is to build a system of individual feedback on referrals and feedback reports to physicians involved, within the referral system in Saudi Arabia. Moreover, the involvement of the hospital and its staff in PHC tasks and activities might help in understanding the role of PHC and encourage the specialists in hospitals to respond more appropriately to the PHC doctor's requests.
The implementation of the quality assurance program for referrals established by the national committee of quality assurance16 would guarantee better monitoring and quality of the referrals. However, this should go hand in hand with better provision of relevant diagnostic and therapeutic facilities in health centers and more importantly, communication facilities in both health centers and hospitals. Both hospitals and PHC facilities should have adequate resources to maintain referral support functions.
In conclusion, the quality of referral based on quality of referral letters and feedback reports is poor and needs to be improved. This can be achieved by making the PHC physicians and specialists in hospitals aware of the problem, and understand their role in the process. The implementation of the quality assurance programme on referral will improve the situation and is highly recommended.
ACKNOWLEDGMENT
I would like to thank the Ministry of Health, Saudi Arabia for sponsoring this work, the primary health care personnel in all the regions, and the family physicians who helped in scoring the referral letters. The editorial comments of Prof. A. Gader are highly appreciated and my gratitude to Mr. Ejaz for his secretarial assistance.
REFERENCES
- 1.Lee T, Pappius EM, Goldman L. Impact of inter-physician communication on the effectiveness of medical consultations. Am J Med. 1983;74:109–12. doi: 10.1016/0002-9343(83)91126-9. [DOI] [PubMed] [Google Scholar]
- 2.Byrd JC, Moskowitz AM. Outpatient consultation: Interaction between the general internist and the specialists. J Gen Intern Med. 1987;2(2):93–8. doi: 10.1007/BF02596304. [DOI] [PubMed] [Google Scholar]
- 3.Sears CL, Charlson ME. The effectiveness of a consultation: compliance with initial recommendations. Am J Med. 1983;74:870–6. doi: 10.1016/0002-9343(83)91079-3. [DOI] [PubMed] [Google Scholar]
- 4.Epstein O. The transformation of letter writing with information technology. Br J Hosp Med. 1989;41:177–81. [Google Scholar]
- 5.Hart JT. What sort of letters do GPs want to receive from hospital specialists? Br J Hosp Med. 1989;41:175–6. [PubMed] [Google Scholar]
- 6.Blaney D, Pullen I. Communication between psychiatrists and general practitioners: what style of letters do psychiatrists prefer? J R Coll Gen Pract. 1989;39:67. [PMC free article] [PubMed] [Google Scholar]
- 7.Marinker M, Wilkin D, Metcalfe DH. Referral to hospital: can we do better? BMJ. 1988;297:461–4. doi: 10.1136/bmj.297.6646.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scaffardi RA. Study of written communication between general practitioners and a community physiotherapist. J R Coll Gen Pract. 1989;39:375–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Kentish R, Jenkins P, Lask B. Study of written communication between general practitioners and departments of child psychiatry. J R Coll Gen Pract. 1987;37:162–3. [PMC free article] [PubMed] [Google Scholar]
- 10.Jarallah JS. The quality of referral letters in two health centers in Riyadh. Annals of Saudi Medicine. 1990;10(5):585. doi: 10.5144/0256-4947.1991.658. [DOI] [PubMed] [Google Scholar]
- 11.Cumminus RO, Smith RW, Inui TS. Communication failure in primary care failure of consultants to provide follow up information. JAMA. 1980;24(16):1650–2. [PubMed] [Google Scholar]
- 12.Hansen JP, Brown SE, Sullivan RJ, Muhlabaier LH. Factors related to an effective referral and consultation process. J Fam Pract. 1982;15(4):651–6. [PubMed] [Google Scholar]
- 13.Al-Kashif Mr. Evaluation of efficiency of the referral system in rural primary health care. Annals of Saudi Medicine. 1990;10(5):585. [Google Scholar]
- 14.Al Mazroa YY, Al-Shammari SA, Siddique M, Jarallah JS. A preliminary report on the effect of referral system in four areas in the Kingdom of Saudi Arabia. Ann Saudi Med. 1991;11:663–8. doi: 10.5144/0256-4947.1991.663. [DOI] [PubMed] [Google Scholar]
- 15.Newton J, Eccles M, Hutchinson A. Communication between general practitioners and consultants: What should their letter include. BMJ. 1992;304:821–4. doi: 10.1136/bmj.304.6830.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jarallah JS. Referral system. National Committee for Quality Assurance (ed.) Quality Assurance in PHC, MOH. 1994 [Google Scholar]


