Abstract
Background:
Alternative Medicine (AM) is gaining popularity worldwide.
Objectives:
This study was conducted to determine the prevalence and pattern of AM use in a military sector of the Saudi community.
Methods:
Three hundred and ten adult patients, visiting their family physicians over 6 weeks from the 1st of June 1998, were selected by systematic random sampling. They were asked to report worrying health problems and their use of modern medicine (MM) and AM.
Results:
Forty-six percent of the patients had used AM before and about 19% had used it in the past 12 months. Alternative medicine practitioners were visited by 16.5% of the study population. Herbal medicine users represented 8.7% of the study population, honey (4.5%), the black grain Nigella sative (3%) and cautery was used by one person only. Women, housewives and the illiterate were more likely to use AM. About 86% of all the study population preferred MM. The main source of information about AM was relatives (77%). A large proportion of patients who reported depression used AM (53%) or visited AM practitioners (33%). The average cost per visit to an AM pratitioner (166 Saudi Riyals) was higher than that in the USA ($27.60=100 Saudi Riyals).
Conclusion:
There is a need to educate the public through the media and health professionals on the appropriate use of AM; housewives and the illiterate should be targeted. A community-based household survey using interviewers not associated with the health system such as teachers (to avoid bias) is needed.
Keywords: Alternative medicine, Saudi Arabia, Media education
INTRODUCTION
Alternative medicine (AM) is widely practiced and is gaining popularity worldwide.1–4 The scope of AM is enormous and includes all therapeutic procedures and practices which fall outside the mainstream of medical practice.5 Different terms such as complementary, unconventional, unorthodox and others6 have been used to describe AM. Many reasons have been adduced to the huge upsurge and expenditure on AM; these include fear of iatrogenic illnesses, the demand for greater patient participation in treatment, the growth of awareness of health issues, and the failure of conventional treatment.5
AM practices in Saudi Arabia originate partly from the Islamic religion. The advice for Muslims to look for treatment for their illnesses comes from Prophet Mohammed, Peace be Upon Him (PBUH) Hadeeth. “Oh"! People take treatment and medication, as Allah did not put an illness without putting a treatment for it except one: senility (old age)”.7
AM practices include: (a) Reading the Quran and puffing over the affected part of the body: it was narrated that Prophet Mohammed (PBUH) had done this himself and for his companions. (b) Cautery, blood letting, honey and black grain stated in Hadeeths of Prophet Mohammed (PBUH).
A cross-sectional study of patients attending health centers found that 24% had used AM during the previous six months.8 In another study, 73% of patients admitted to hospital received oil and/or Ghee as folk medicine,9 and 72% of them did so because of the persistent advice from their relatives. At an outpatient pediatric orthopaedic clinic in a tertiary care hospital in Riyadh, it was found that 22% of the patients had cautery over the preceding 11 month period.10
Some forms of AM are well known but others are exotic, or mysterious, still others are dangerous.11 In Saudi Arabia, several studies have reported the serious side effects of some AM practices.9,11–14 Lamb bile was prescribed by a faith healer for 14 diabetic patients. Of these, 12 were hospitalized for gastrointestinal complaints.6 The use of some types of herbal medicine is known to cause liver toxicity.15
In spite of its importance, little is known about the overall prevalence, cost and pattern of AM use in different sectors of the Saudi population. Doctors’ understanding of the pattern of AM use, the characteristics of users and patients’ perception is important for a successful doctor - patient encounter. Studies in Saudi Arabia have been conducted in hospital in-patient settings,9,16 the use of a single type of AM,9,10,13,17 and AM practitioners through interviews18 or patients attending primary health care (PHC) centres in a small city,8 but there has been no community survey. To the best of the author's knowledge, this is the first study on the prevalence and pattern of AM use among patients in a military population in a large city in Saudi Arabia attending their health centres.
This study was conducted to increase our understanding of the pattern of use of AM in a sector of the Saudi community at the National Guard (NG) residential compound. The focus was on the following questions:- The extent of AM use among the study population? The types of AM commonly used? The sociodemographic factors that distinguish AM users from non-users? The perceived health problems for which AM is commonly used? The patients’ perception of the benefit and safety of AM vis a vis MM? The patients’ perception of the causes of their reported health problems?
SUBJECTS AND METHODS
Data Collection
The records of the study population including name, address, age and phone number were accessible through the computer. The initial plan was to collect the information through telephone interviews based on the assumption that it would be a better representation of the whole population. A few phone calls were made, but the response rate was poor. Some of the responders were suspicious of the research team's intentions especially when a female patient was to be interviewed. Therefore, face to face interviews were set up at the health centers.
Study Site
The NG residential compound, located at Kashm Alaan in the east part of Riyadh has a population of approximately 60,000 residents, all of whom are Saudi military personnel and their families. Of the total, 18000 (30%) persons were aged 18 years or above. PHC is provided through ten satellite clinics run by 30 physicians. Each clinic has a well-defined catchment area. Around 200,000 encounters took place during 1997 at the ten clinics.19
Subjects
The study population targeted was the adult patients, aged 18 years or more, attending the ten satellite clinics over a six-week period, from the first of June 1998.
The required sample size was estimated as 225. This was based on the assumption that 30% of the patients would have used AM over the past 12 months as shown in a previous Saudi study,8 with an estimated error of +6% within 95% level of confidence. Some adjustment was made in the sample size for an expected response rate of 80%. Therefore, a sample size of 300 patients was used. Patients were selected by a systematic random sample.20 Care was taken to make the sample size for each health center proportionate to the population size of its catchment area. The patients were asked about AM use during the 12 months before the interview. Therefore, the results were considered representative of the year from June 1997 to May 1998.
The Interview
Six trained social workers interviewed the selected patients using a pre-designed Arabic data collection form. Each of them interviewed 3 patients while being observed by the author as part of the training and to increase and safeguard reliability.
The interview was described to the respondents as a survey designed to assess their beliefs and practices when faced with health problems. No mention was made of AM while recruiting the respondents. Confidentiality was promised from the start. The initial sequence and wording of the questions was based on the study by Eisenberg.3 The interview, which averaged 15 minutes in length, started with questions on the respondent's health, health worries and his or her interaction with physicians during the past 12 months.
The interviewer then assessed the respondent's health problems by stating, “Have you suffered or are still suffering from the following health problems?. Twenty-three common health problems were named followed by the question, “What other important health complaints do you have?” The 23 health problems included common symptoms (such as back pain, digestive problems, headache and fatigue) as well as specific diagnoses such as diabetes, epilepsy, hypertension and cancer.
The respondents were then asked to identify the three (or fewer) “most bothersome or serious” health problems from the list they had just been given. These health problems are referred to here as “principal health conditions”. The respondents were asked whether they had seen their medical doctor for each principal health condition during the past 12 months and what their perception of these interactions had been.
At this point, they were asked about their use of unconventional therapy. The respondents were asked whether they had ever used one or more of 10 unconventional therapies for their principal health conditions and, if so, whether they had used any of them in the past 12 months. The 10 unconventional therapies included: (1) Cautery (2) Herbs (3) Water and oil (4) Quran (5) Honey (6) Black grain (7) Fracture fixation (8) Chemicals (9) Acupuncture (10) Jinni (Muslims believes in this as one of the supernatural beings able to assume human or animal form and often at the service of men: also spelled genie or Jinnee) removal from the patient body by sheik. For example, a respondent listing back problem as a principal health condition was asked whether he or she had used any of the ten unconventional therapies for this problem during the past 12 months. The respondents were next asked whether they had used “any other therapy not generally provided by most clinics and hospitals”.
When patients reported the use of AM during the past 12 months, the questions were asked to elicit the following information: The names of the unconventional therapies used or AM providers visited for each of the principal health problems, number of times used, the average charge per visit and opinion on the AM used, reasons for AM use, experience of side effects and the patients’ demographic characteristics. The patient was also asked if he/she had informed his or her doctor about AM use.
Data Analysis
The data were entered into a personal computer and both the chi-square and the odds ratio were used. The conventional < 0.05 level of statistical significance was used to determine the difference between groups.
RESULTS
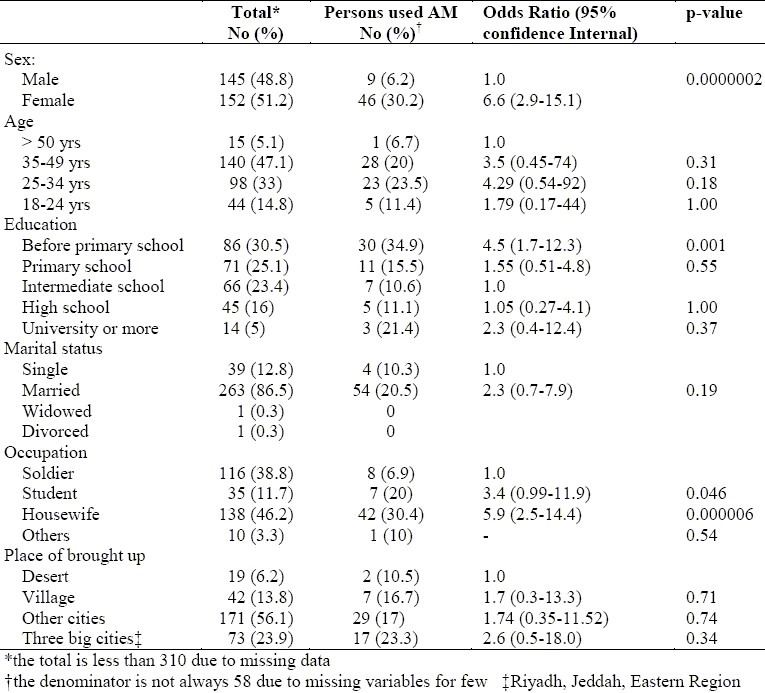
Out of a total of 320 patients targeted for the study, 310 agreed to participate (97%). All the patients included in the study are Saudi, (men 49% and women 51%). About half of them were below 35 years of age and one third had no formal education (Table 1). The majority of the study population were married and were either soldiers (for men) or housewives. Women, housewives and persons who had no formal education were found more likely to use AM.
Table 1.
Univariate associations between use of Alternative Medicine (AM) over the past 12 months and variables of interest
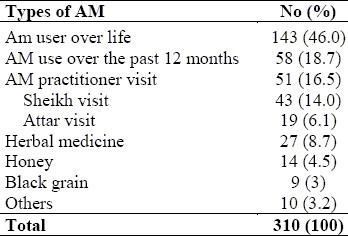
The proportion of patients who had ever used AM was 46%, 19% had used it during the past 12 months, (Table 2). About 17% of the patients visited one or more kinds of AM practitioners like a sheik for reading the Quran with oil and water (14%), or the attar (apothecary, herbalist: a person who prepares and sells crude drugs – herbs, roots and other ingredients – and practices healing) (6.1%). Herbal medicine users accounted for 8.7%, honey (4.5%) and the black grain Nigella sativa (3%) (Table 2). Although only one patient used cautery in the past year, 18 (5.8%) patients were cauterized before.
Table 2.
The proportion of users of different types of AM among the 310 study population during the past 12 months period and over life
Pattern of AM use
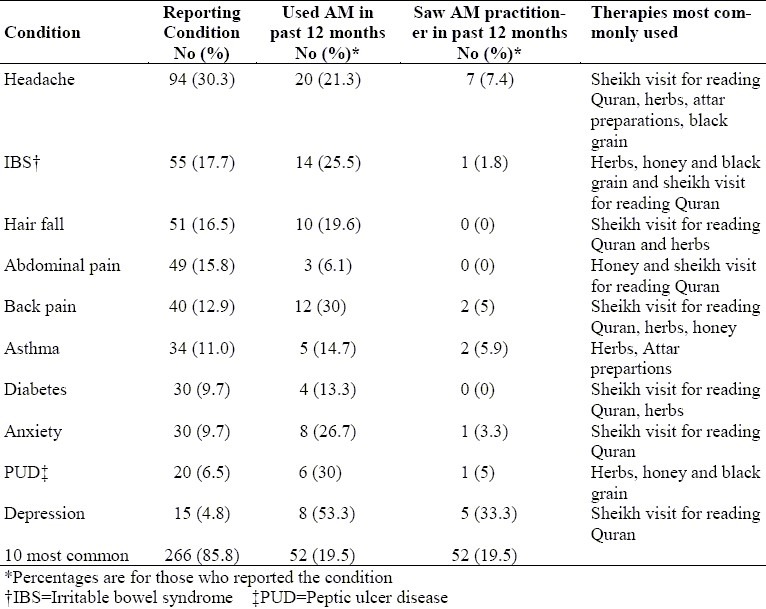
The vast majority of the patients (86%) reported a principal health problem over the past year. Table 3 summarizes the rate of AM use for the ten most common principal health problems. On the average, one in five respondents (19.5%) used AM for principal health problems (Table 3). Among all the conditions studied, the frequency of AM use was highest for headache (20), irritable bowel syndrome (IBS) (14) and backpain (12). The proportion of patients with depression who used AM (53%) was higher than that of patients with other conditions. The highest frequency of visits to AM practitioners’ was for headache (7 patients) and depression (5 patients). The average cost of any AM practitioner visit was 166 Saudi Riyals (SR), a visit to a sheik to read the Quran with oil and water (125 SR) and the average cost of buying herbs and black grain from the attar was 200 SR.
Table 3.
Use of AM for the 10 most frequently reported principal health conditions
For the study population, the perceived causes of health problems were destiny (64%), hereditary factors (7.4%), envy (7%) and acquired problems (5.5%). The main reasons for using AM were its success in treating previous health problems (28%) and unreliable doctor's diagnosis (21%), reliability of AM (17%) and inaccessibility of MM facilities (7%). Compared with AM, MM was perceived by a higher proportion of the total respondents as beneficial (96% vs 57%) and safe (95% vs 48%). Compared with patients who used MM only, a higher proportion of AM users perceived AM as beneficial, while a lower proportion perceived it as safe. Among the patients who had used AM over the past year, 50 (92%) had not had side effects at all, two had had minimal side effects, two had side effects for which medical advice was sought, but none needed admission in to hospital.
The patients were asked to name the three most important health problems and the type of treatment used for each, and their satisfaction with the treatment was explored. There was no statistically significant difference between AM and MM users in the rate of satisfaction. About 86% of all the study population preferred MM, while 1% preferred AM, and 12% preferred using both types. The main sources of information about AM were relatives (11%), neighbours (48%) and friends (39%). The media constituted only 8.3% of the information sources. Out of those who used AM, 40% said they would use it again. The majority would not volunteer any information to their doctors about AM use (72%) and those who would not advise their relatives or friend to use it constituted 70%.
DISCUSSION
The patients who participated in the present study were recruited from health facilities. Nevertheless, the sample could be considered representative of a significant proportion of the compound population, as statistics revealed that more than 90% of the residents visited their health centre annually19. Our discovery at the early stages of the study that it was socially unacceptable to discuss health matters on the phone necessitated our conduct of the study among patients attending their health facilities. Nevertheless, the data obtained revealed some trends in thinking, perception and practice of a significant number of the target population. The validity of the study results was raised by factors such as: the high response rate (97%), the appropriate sample size and the method used for data collection i.e interview rather than self-reported questionnaires, because of the high illiteracy rate (27% of the study population could not write).
The proportion of patients who had used AM over the last year was 19%. It was envisaged that the conduct of the study in a health facility run by persons associated with the health facility could introduce some unfairness or bias. Furthermore, the indication that 72% of the study subjects would not inform their doctors about AM use suggests that an underestimation of the rate of AM use was likely and patients would feign more favourable comments in favour of MM. The figure is lower than that reported from some developed countries, 34% in USA,3 48.5% in Australia,4 23% in Denmark, and 49% in France21. However, the percentage of patients who visited AM practitioners (16.5%) is more than the USA figure (11%)3 and the U.K. figure (10%),2 but less than in Australia (20.3%). The rate of herbal medicine use in the current study (8.7%) is higher than in the USA (3%), but less than the Australian study (9.9%). The finding of only one patient who was cauterized over the last year and that of 5.8% of the patients were cauterized before indicates either that cautery is becoming less popular among residents or that there is increased awareness of its dubious benefits and its possible side effects.
Women, housewives and individuals who had no formal eudcation were found more likely to use AM; these three characteristics are interrelated. In general, the females have less education than males in Saudi Arabia22,23. This agrees with Gupta's findings that most parents who decided to treat their children with AM were illiterate.9 The demographic characteristic associated with AM use in western studies are different from the findings in this study.4
There is a wide variation among countries in the types of AM practiced and the mode of practice. In Western studies, the common types include relaxation techniques, ginseng, chiropractic osteopathy, massage, image, mineral supplements and homeopathy.2–4 The types of AM practiced in Saudi Arabia are, however, quite different. A study of around 120 AM practitioners in different parts of the Kingdom of Saudi Arabia found that the majority were illiterate: 28% used cautery, 25% read the Quran and 45% used herbs as treatment modalities.18 In the present study, visiting a sheik to read the Quran and the use of herbs were found the most popular. In the Arar study, herbs constituted the main type of AM used (23.9%). Reading of the Quran (2.9%), visit to an attar (1.6%) and cautery (1.2%) were used by smaller proportions of patients.8
Compared with patients who reported other ailments, patients who reported depression were found more likely to use AM (53%) or visit AM practitioners (33%). In the perception of Saudis a doctors’ main job was to treat organic illnesses; there was stigma attached to psychological disorders.24,25 Therefore, when they have psychological illnesses the symptoms they present with are usually organic rather than psychological.24,26,27 This indicates that the proportion of psychological disorders could be more than is reported by patients.
Why do the majority of patients who use AM not inform their doctors? The patients probably surmise that AM is unacceptable to their doctors and would not be encouraged. The doctors are also probably not aware of the importance of obtaining information on AM use and would not ask about it. This needs to be investiged in future studies so that compaign for education on such practices would be better planned.
The perception of AM as dangerous by 70% of patients who used AM compared with 48% of those who used MM may be an indication of increased awareness of the AM users on the risks involved.
RECOMMENDATIONS
There is a great need for the education of the public through the media and by health professionals on the use of AM for the management of some health problems. Medical doctors should enquire about the history of AM use in the patients’ medical history. The adverse effects and benefits of both MM and AM should also be discussed. Certain groups e.g. housewives and the illiterate should be targeted in the education drive on AM. In addition to destiny (perceived by patients as the major cause of illness), the importance of preventing the known physical and psychological causes of these illnesses should not be underestimated. The establishment of channels of communication between physicians and faith healers should be considered. There is a need for a community-based household survey with trained interviewers, with no connection to the health system e.g. teachers or university students.
ACKNOWLEDGMENT
My sincere gratitude goes to the social workers who participated in the data collection.
REFERENCES
- 1.Ernst E. Researching complementary medicine. In: Brown J.S, Pereira Gray DJ, Horne RA, Reith W, editors. Royal College of General Practitioners Members’ Reference Book 1994. London: Sabrecrown Publishing; 1994. pp. 613–5. [Google Scholar]
- 2.Wood G, Dorozynski A, Lie LG, Zinn C, Josefson D, Ingram L. Complementary Medicine is booming worldwide. BMJ. 1996:131–3. [PMC free article] [PubMed] [Google Scholar]
- 3.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, and Delbanco TL. Unconventional medicine in the United States cost and pattern of use. N Engl J Med. 1993;328:246–52. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 4.MacLennan AH, Wilson DH, Tylor AW. Prevalence and cost of alternative medicine in Australia. Lancet. 1996;347:569–73. doi: 10.1016/s0140-6736(96)91271-4. [DOI] [PubMed] [Google Scholar]
- 5.Ginsburg M. Complementary Medicine. The practitioner. 1990;234:111. [Google Scholar]
- 6.Al-Qahtani MS. Hepatic and Renal toxicity among patients ingesting sheep bile as an unconventional remedy for diabetes mellitus in Saudi Arabia. Morbidity and Mortality Weekly Report. 1996;45:941–3. [PubMed] [Google Scholar]
- 7. Prophet Mohammed (PBUH) Hadeeth narrated by Ahmed in Al-Mosned and Abo Daood and Al-Tormedhi. [Google Scholar]
- 8.Ajaji N, Taha AZ, Al-Subier AG. Prevalence of utilization of native medicine among primary care consumers. Saudi Med J. 1998;19:551–4. [PubMed] [Google Scholar]
- 9.Gupta M, Chowdery MSA. A common practice of traditional medicine with oil and/or Ghee, as folk medicine in children of Southern Saudi Arabia. Ann Saudi Med. 1990;10:378–82. [Google Scholar]
- 10.Watt HG. Cutaneous cautery (Al Kowi): A study in pediatric orthopedic clinic in central Saudi Arabia. Ann Saudi Med. 1989;9:475–8. [Google Scholar]
- 11.Abdullatif HA. Medicinal plant in South Western Saudi Arabia. Economic Botany. 1987;41:354–60. [Google Scholar]
- 12.Abdullah MA. Traditional practices and other socio-cultural factors affecting the health of children in Saudi Arabia. Ann of Trop pediatrics. 1993;13:227–32. doi: 10.1080/02724936.1993.11747650. [DOI] [PubMed] [Google Scholar]
- 13.Al Awad ME, Vijaya kumar E, Malhotra RK. Native manual tonsillectomy: a dangerous practice in Asir. Ann Saudi Med. 1992;12:188–90. doi: 10.5144/0256-4947.1992.188. [DOI] [PubMed] [Google Scholar]
- 14.Rathi SK, Elzubier A, Srinivasan MA. Traditional healing methods prevalent in Zulfi Area. Ann Saudi Med. 1993;13:93–4. doi: 10.5144/0256-4947.1993.93. [DOI] [PubMed] [Google Scholar]
- 15.Larrey D, Vail T, Pauwels A, Castot A, Biour M, David M, Michel H. Hepatitis after Germander (Teucrium chamaedrys) Administration: Another Instance of Herbal Medicine Hepatotoxicity. Ann Int Med. 1992;117:129–132. doi: 10.7326/0003-4819-117-2-129. [DOI] [PubMed] [Google Scholar]
- 16.Sebai ZA. First Edition. Riyadh: Tihama Publications; 1984. Health in Saudi Arabia. [Google Scholar]
- 17.Tabbara K. Cautery, folk remedies and magic. Ann Saudi Med. 1989;9:433–34. [Google Scholar]
- 18.Al-Aska A, Al Khwaiter SA, Al-Jualie AA, Mufti MH, Al-Omair A, Al-Baaj T. A report of the results of 120 native healers interviews. Personal communication. (unpublished). A project sponsored by King Abdulaziz. City for Science and Technology [Google Scholar]
- 19.King Fahad National Guard Hospital – Department of Family Medicine Statistics 1997. 1998 [Google Scholar]
- 20.Dawson – Saunders B, Trapp RG, editors. Basic and clinical biostatistics. London: Prentice – Hall International Inc; 1997. Probability sampling and probability distributions; pp. 64–82. [Google Scholar]
- 21.Fisher P, Ward A. Complementary Medicine in Europe. BMJ. 1994;309:107–11. doi: 10.1136/bmj.309.6947.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexandria, Egypt: World health organization; 1996. World Health Organization. Regional office for the Eastern Mediterranean. Implementation of the Global Strategy for Health for all by the year 2000, Second evaluation, Eight report on the world health situation. [Google Scholar]
- 23.Khoja TA, Farid SM, editors. Riyadh: Ministry of Health; 1997. Saudi Arabia Family health Survey 1996. [Google Scholar]
- 24.Al-Faris EA, Al-Hamad A, Al-Shammari S. Hidden and conspicuous psychiatric morbidity in Saudi Primary Health Care (A pilot study) The Arab Journal of Psychiatry. 1995;6:262–75. [Google Scholar]
- 25.Al-Subaie A. Psychiatry in Saudi Arabia: an overview. Psychiatric Bulletin. 1990;14:298–300. [Google Scholar]
- 26.Racy J. Somatisation in Saudi Women: a Therapeutic Challenge. Br. J. Psychiatry. 1980;137:212–6. doi: 10.1192/bjp.137.3.212. [DOI] [PubMed] [Google Scholar]
- 27.Al-Faris E, Al-Subaie A, Khoja T, Abdulraheem F, Al-Hamdan N, Al-Mazrou Y, et al. Training primary health care physicians in Saudi Arabia to recognize psychiatric illness. Acta Psychiatr Scand. 1997;96:439–44. doi: 10.1111/j.1600-0447.1997.tb09945.x. [DOI] [PubMed] [Google Scholar]


